April 26 2018 Scottsdale AZ Otology Workshop Advanced


- Slides: 37
April 26, 2018 Scottsdale AZ Otology Workshop; Advanced Ryan Marovich, MPAS, PA-C J. Andrew Clark, PA-C Updated 2018 Eighth Annual ENT for the PA-C | April 25 – 29, 2018| Scottsdale, AZ
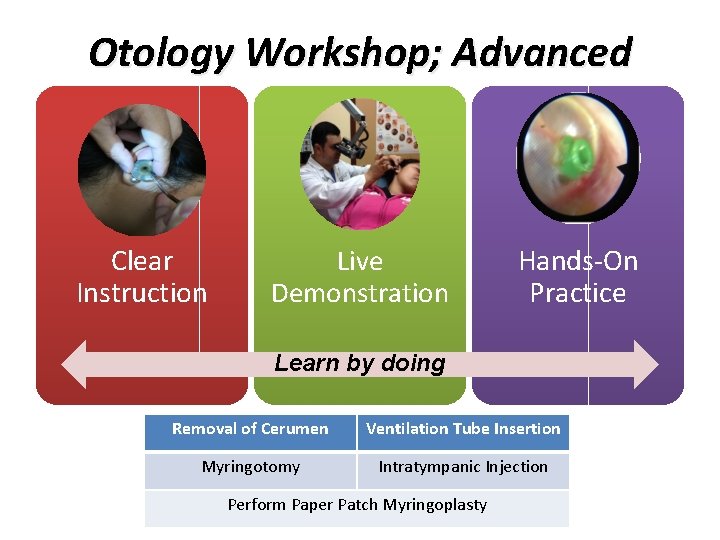
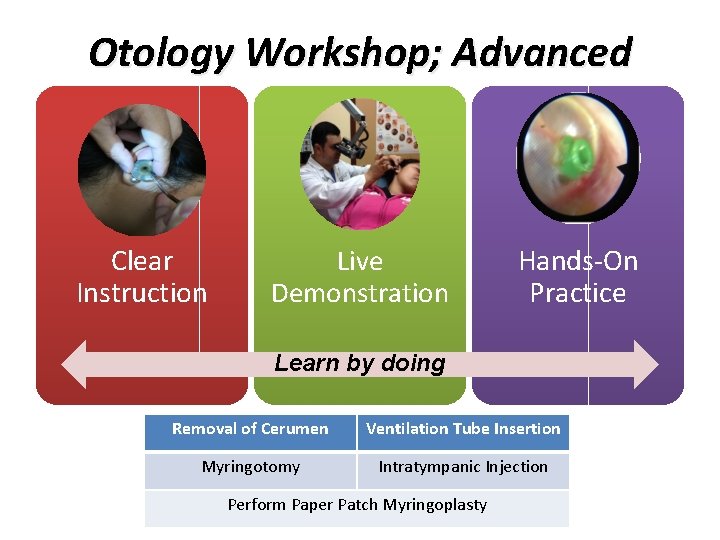
Otology Workshop; Advanced Clear Instruction Live Demonstration Hands-On Practice Learn by doing Removal of Cerumen Ventilation Tube Insertion Myringotomy Intratympanic Injection Perform Paper Patch Myringoplasty
Introduction There are multiple methods and techniques available to successfully complete all the topics presented in this workshop. Some are based on patient request, available equipment or supervising physician’s preference. The goal of this workshop is to correctly demonstrate the most common methods and give participants time for hands on training. Eighth Annual ENT for the PA-C | April 25 – 29, 2018| Scottsdale, AZ
Otology Workshop: Advanced • • • Learning Objectives Practice removing cerumen impaction under microscope Practice myringotomy Practice ventilation tube insertion Practice intra-tympanic membrane injection Practice Paper Patch Myringoplasty Eighth Annual ENT for the PA-C | April 25 – 29, 2018| Scottsdale, AZ
Practice Mannequin(s) • Practice removal of cerumen and FB • Simulated tympanic membrane to practice • Intratympanic steroid injection • Myringotomy and ventilation tube insertion • Paper patch myringoplasty Eighth Annual ENT for the PA-C | April 25 – 29, 2018| Scottsdale, AZ
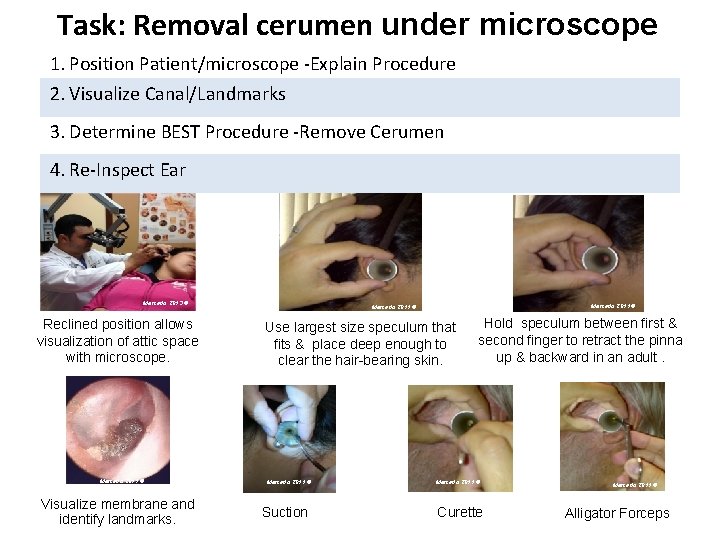
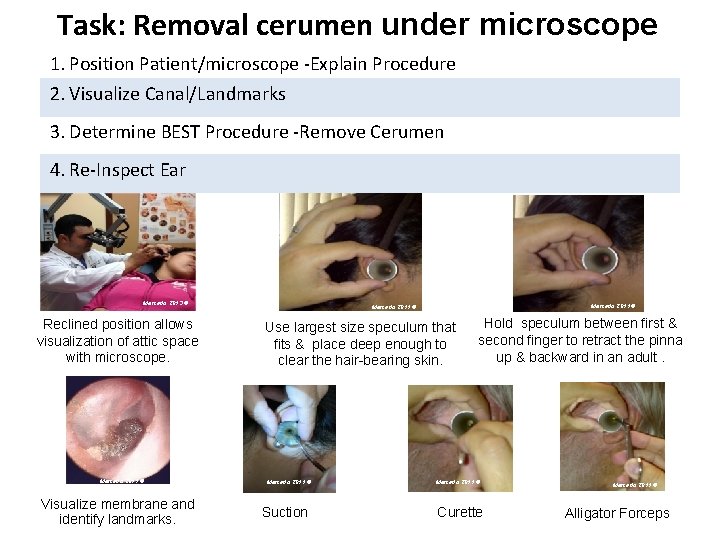
Task: Removal cerumen under microscope 1. Position Patient/microscope -Explain Procedure 2. Visualize Canal/Landmarks 3. Determine BEST Procedure -Remove Cerumen 4. Re-Inspect Ear Mercado 2013 © Reclined position allows visualization of attic space with microscope. Mercado 2011 © Visualize membrane and identify landmarks. Mercado 2011 © Use largest size speculum that fits & place deep enough to clear the hair-bearing skin. Mercado 2011 © Suction Hold speculum between first & second finger to retract the pinna up & backward in an adult. Mercado 2011 © Curette Mercado 2011 © Alligator Forceps
Myringotomy with Ventilation Tube Insertion Eighth Annual ENT for the PA-C | April 25 – 29, 2018| Scottsdale, AZ
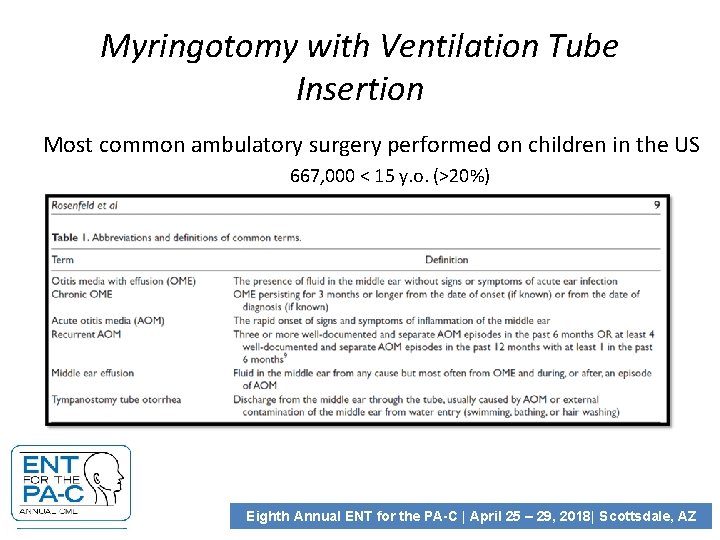
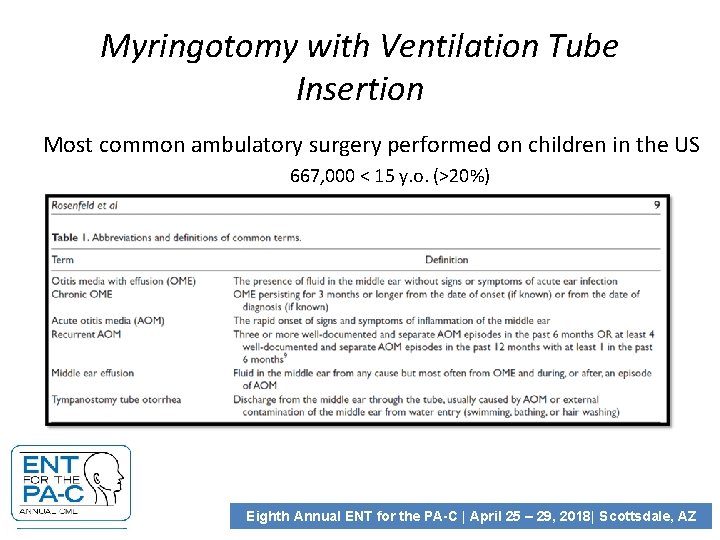
Myringotomy with Ventilation Tube Insertion Most common ambulatory surgery performed on children in the US 667, 000 < 15 y. o. (>20%) Eighth Annual ENT for the PA-C | April 25 – 29, 2018| Scottsdale, AZ
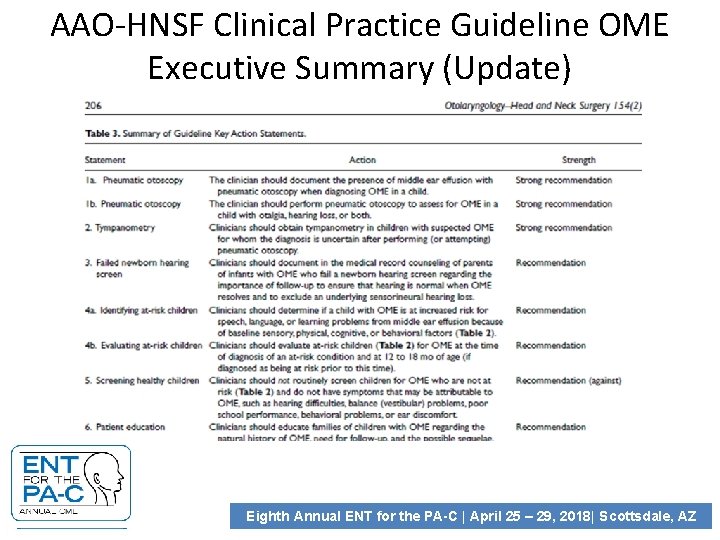
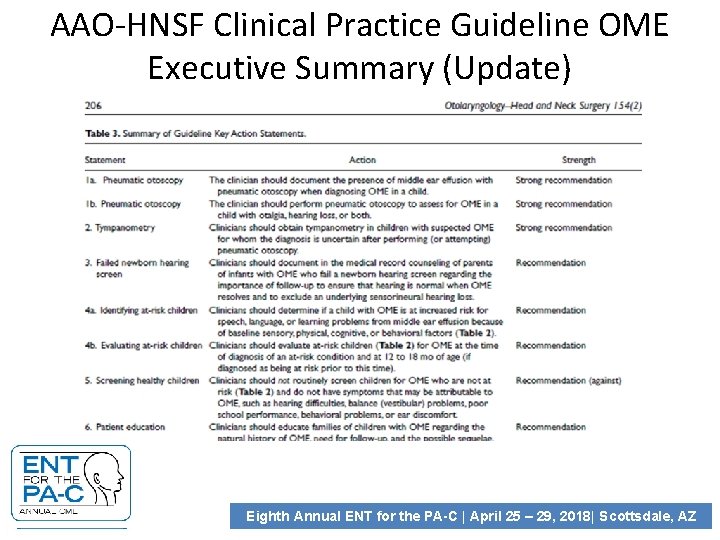
AAO-HNSF Clinical Practice Guideline OME Executive Summary (Update) Eighth Annual ENT for the PA-C | April 25 – 29, 2018| Scottsdale, AZ
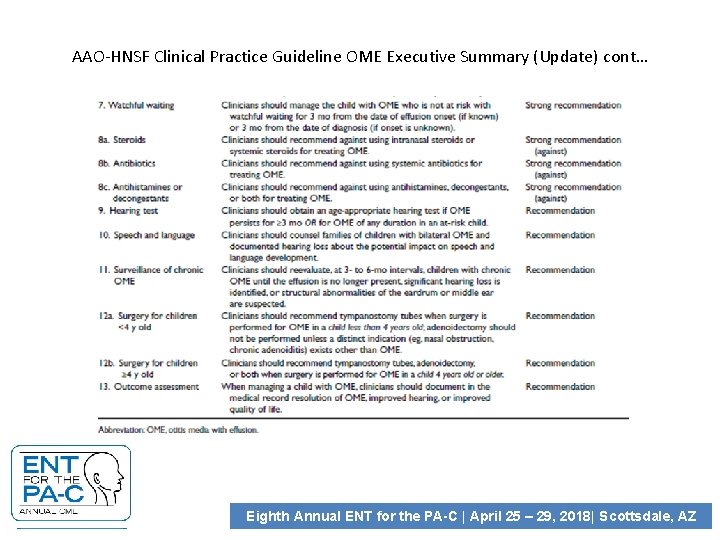
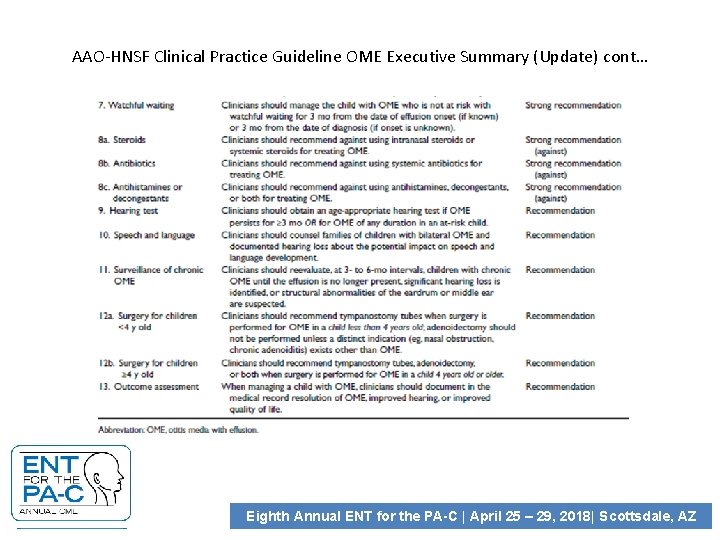
AAO-HNSF Clinical Practice Guideline OME Executive Summary (Update) cont… Eighth Annual ENT for the PA-C | April 25 – 29, 2018| Scottsdale, AZ
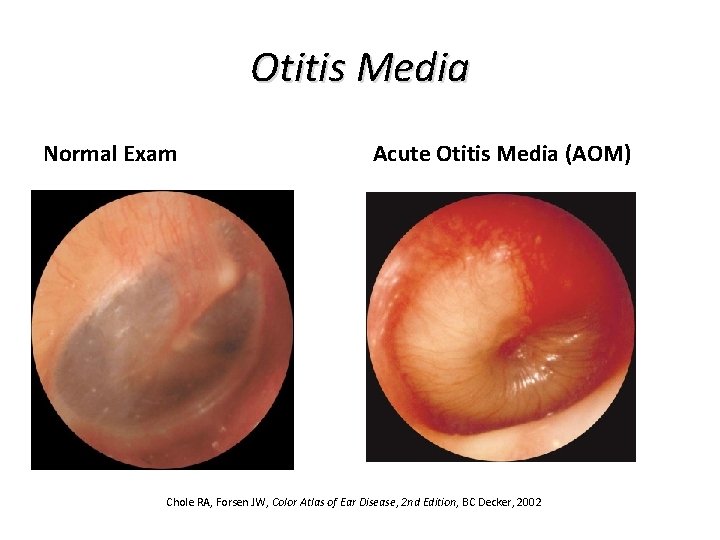
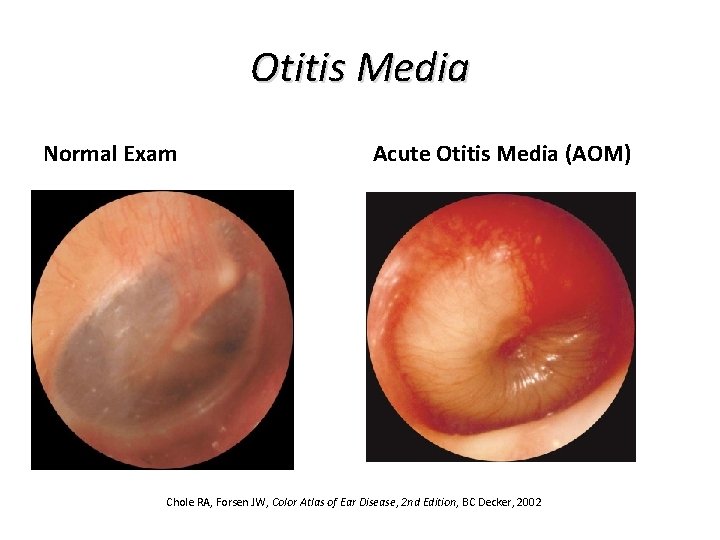
Otitis Media Normal Exam Acute Otitis Media (AOM) Chole RA, Forsen JW, Color Atlas of Ear Disease, 2 nd Edition, BC Decker, 2002
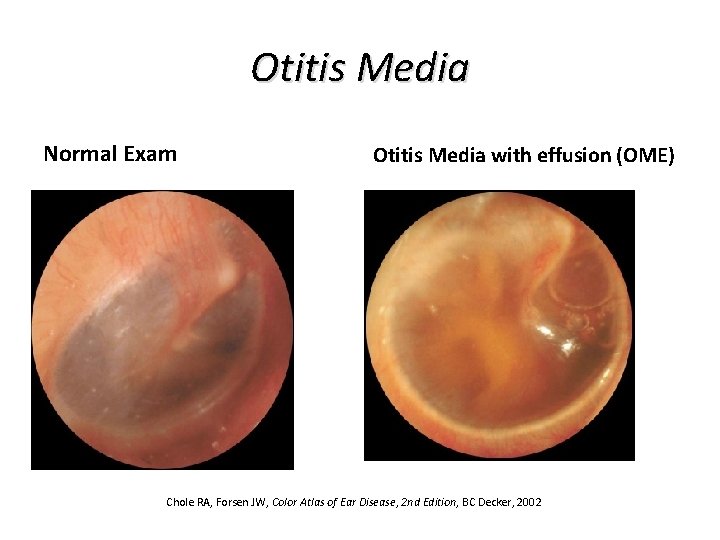
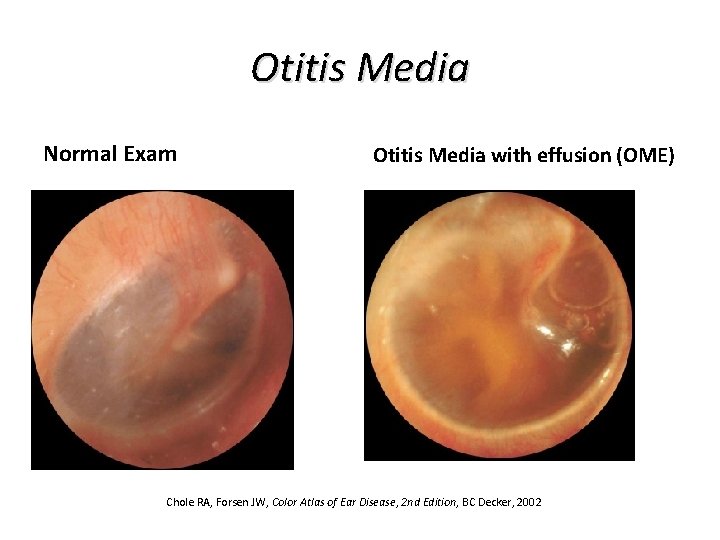
Otitis Media Normal Exam Otitis Media with effusion (OME) Chole RA, Forsen JW, Color Atlas of Ear Disease, 2 nd Edition, BC Decker, 2002
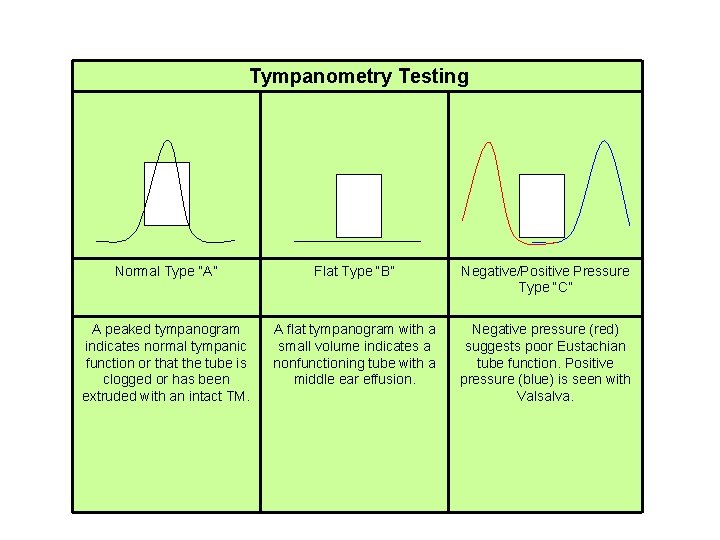
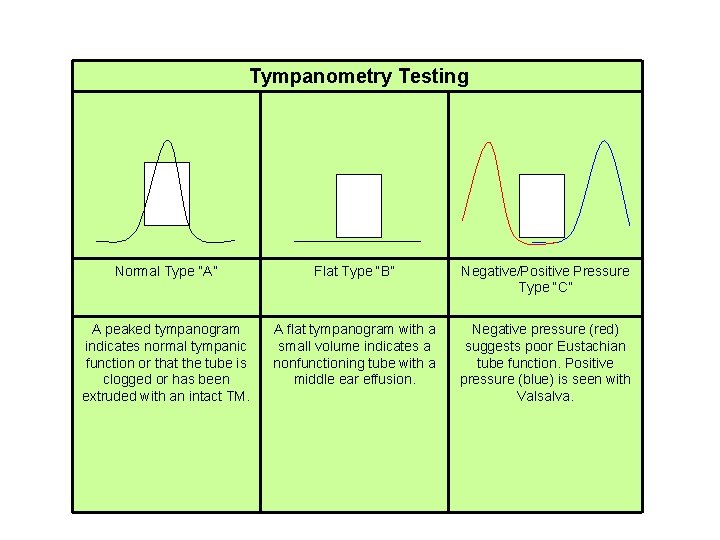
Tympanometry Testing Normal Type “A” Flat Type “B” Negative/Positive Pressure Type “C” A peaked tympanogram indicates normal tympanic function or that the tube is clogged or has been extruded with an intact TM. A flat tympanogram with a small volume indicates a nonfunctioning tube with a middle ear effusion. Negative pressure (red) suggests poor Eustachian tube function. Positive pressure (blue) is seen with Valsalva. AAO and AAP recommend the use of tympanometry to confirm tympanic membrane mobility.
Operating Microscope Eighth Annual ENT for the PA-C | April 25 – 29, 2018| Scottsdale, AZ
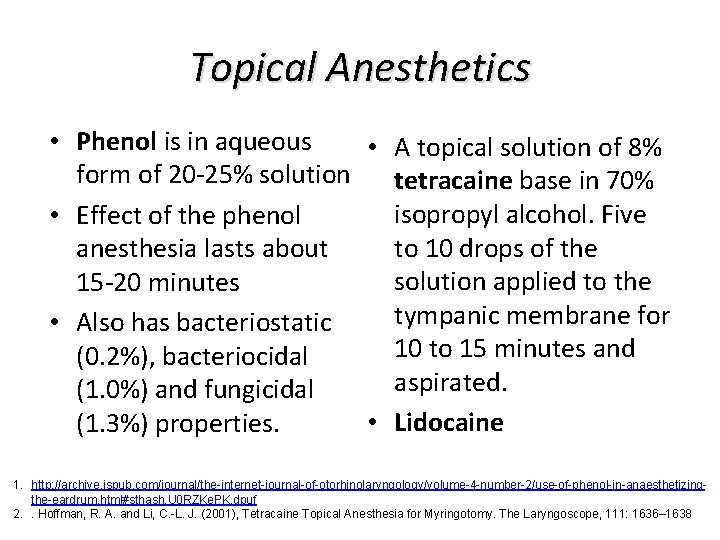
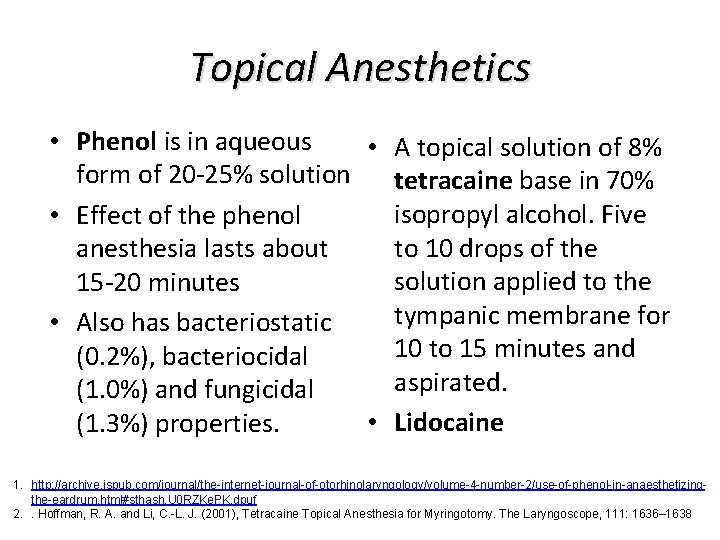
Topical Anesthetics • Phenol is in aqueous • A topical solution of 8% form of 20 -25% solution tetracaine base in 70% isopropyl alcohol. Five • Effect of the phenol to 10 drops of the anesthesia lasts about solution applied to the 15 -20 minutes tympanic membrane for • Also has bacteriostatic 10 to 15 minutes and (0. 2%), bacteriocidal aspirated. (1. 0%) and fungicidal • Lidocaine (1. 3%) properties. 1. http: //archive. ispub. com/journal/the-internet-journal-of-otorhinolaryngology/volume-4 -number-2/use-of-phenol-in-anaesthetizingthe-eardrum. html#sthash. U 0 RZKe. PK. dpuf 2. . Hoffman, R. A. and Li, C. -L. J. (2001), Tetracaine Topical Anesthesia for Myringotomy. The Laryngoscope, 111: 1636– 1638
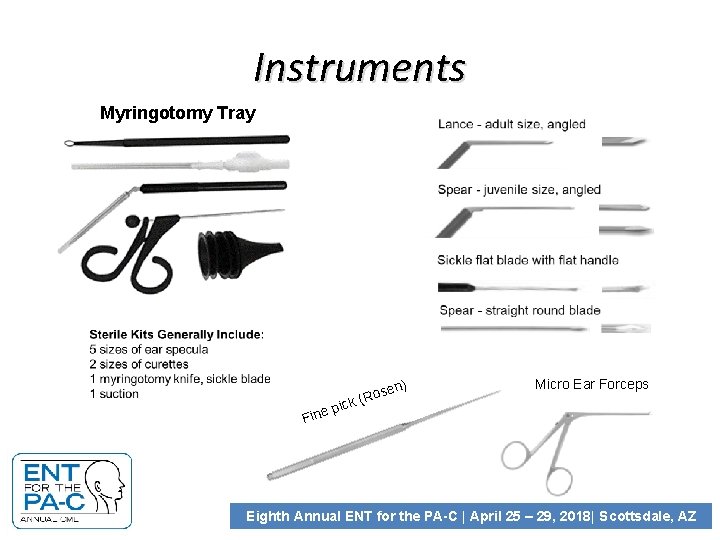
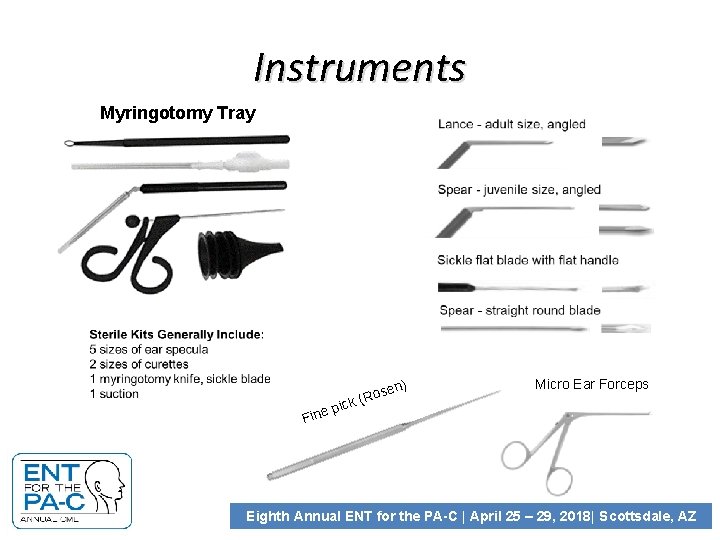
Instruments Myringotomy Tray en) Fine s (Ro k c i p Micro Ear Forceps Eighth Annual ENT for the PA-C | April 25 – 29, 2018| Scottsdale, AZ
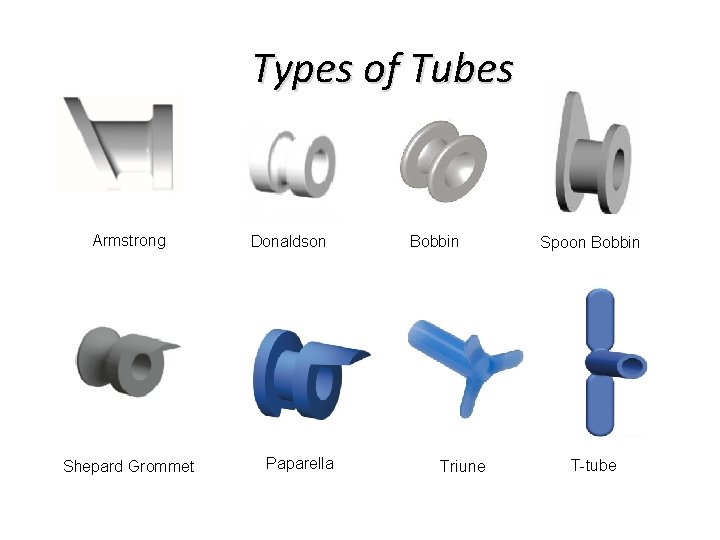
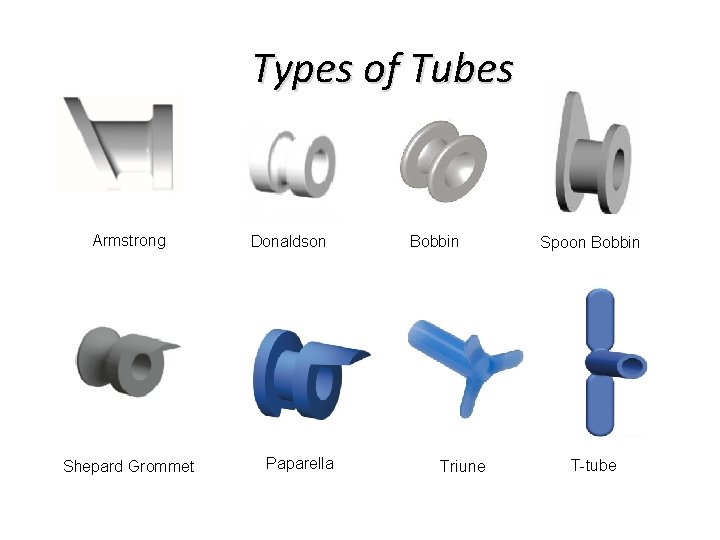
Types of Tubes Armstrong Shepard Grommet Donaldson Paparella Bobbin Triune Spoon Bobbin T-tube
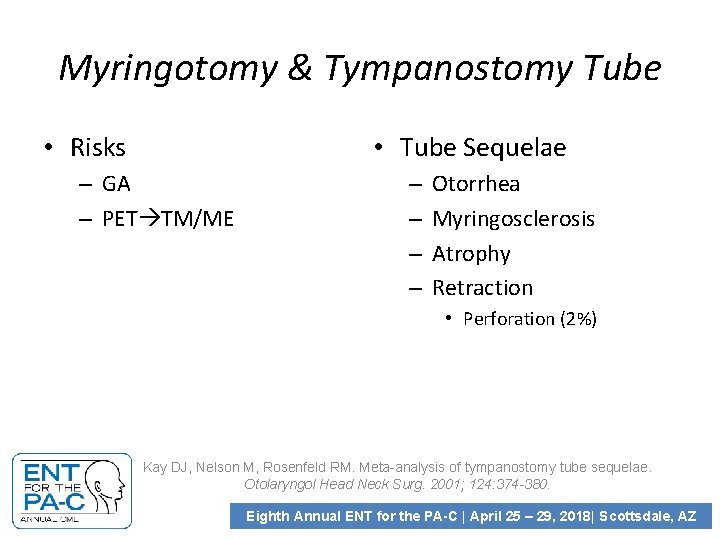
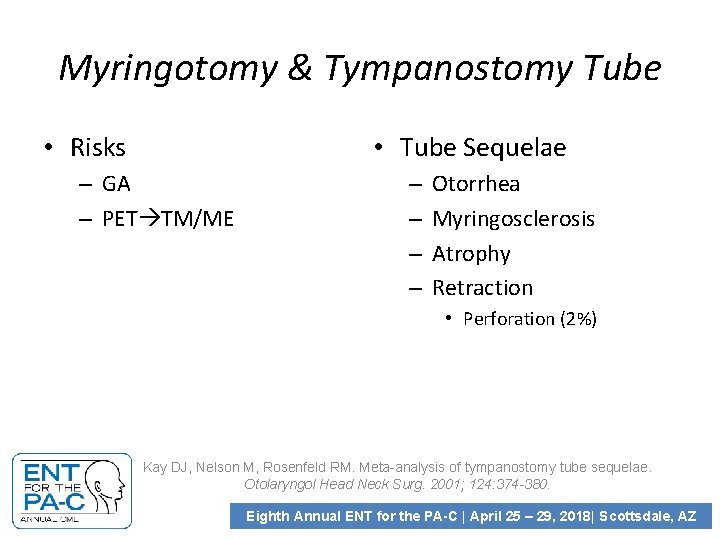
Myringotomy & Tympanostomy Tube • Risks • Tube Sequelae – GA – PET TM/ME – – Otorrhea Myringosclerosis Atrophy Retraction • Perforation (2%) Kay DJ, Nelson M, Rosenfeld RM. Meta-analysis of tympanostomy tube sequelae. Otolaryngol Head Neck Surg. 2001; 124: 374 -380. Eighth Annual ENT for the PA-C | April 25 – 29, 2018| Scottsdale, AZ
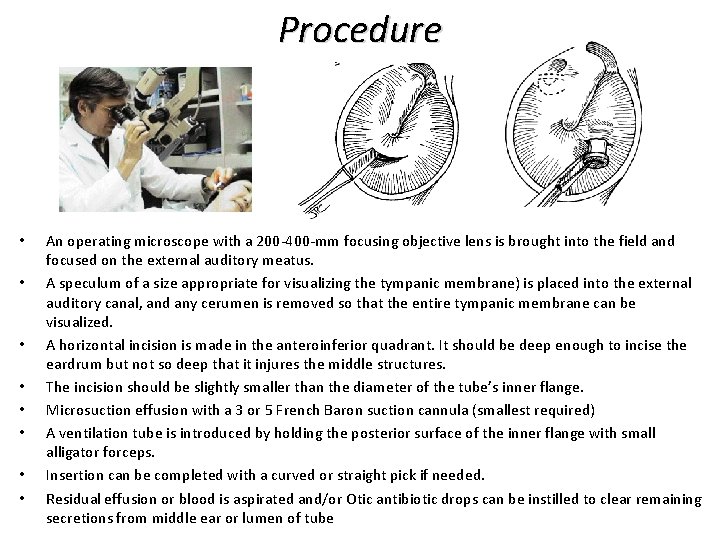
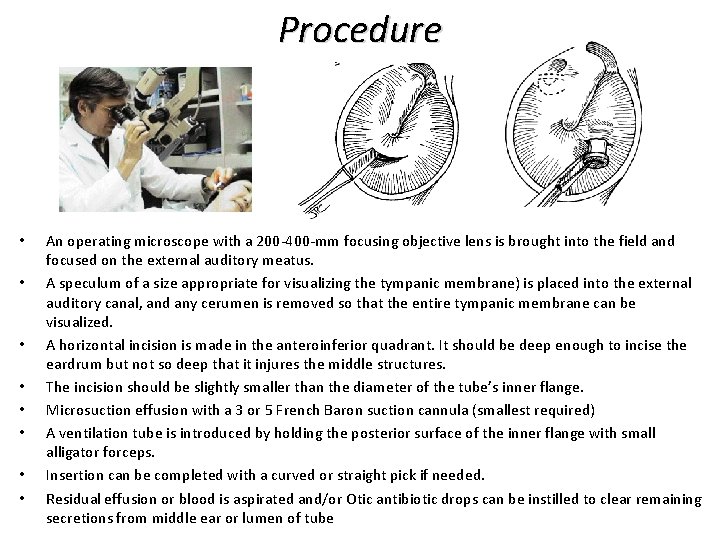
Procedure • • An operating microscope with a 200 -400 -mm focusing objective lens is brought into the field and focused on the external auditory meatus. A speculum of a size appropriate for visualizing the tympanic membrane) is placed into the external auditory canal, and any cerumen is removed so that the entire tympanic membrane can be visualized. A horizontal incision is made in the anteroinferior quadrant. It should be deep enough to incise the eardrum but not so deep that it injures the middle structures. The incision should be slightly smaller than the diameter of the tube’s inner flange. Microsuction effusion with a 3 or 5 French Baron suction cannula (smallest required) A ventilation tube is introduced by holding the posterior surface of the inner flange with small alligator forceps. Insertion can be completed with a curved or straight pick if needed. Residual effusion or blood is aspirated and/or Otic antibiotic drops can be instilled to clear remaining secretions from middle ear or lumen of tube

Myringotomy & Tympanostomy Tube Myringotomy Mercado 2011 © Tympanostomy Tube Mercado 2011 ©
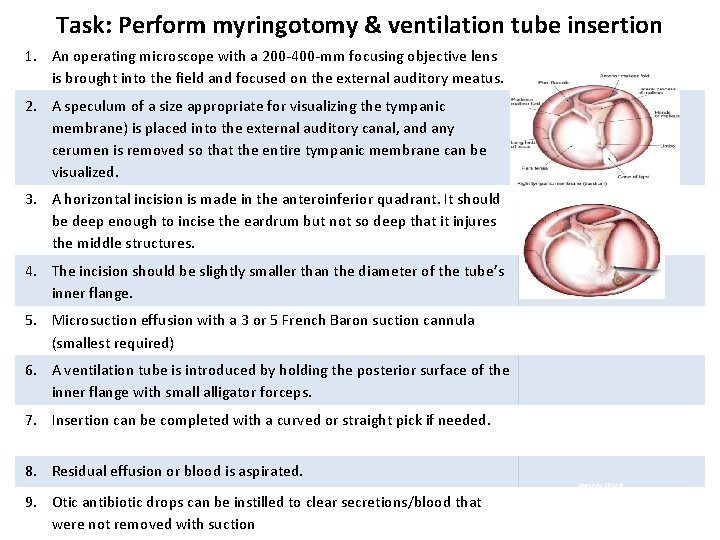
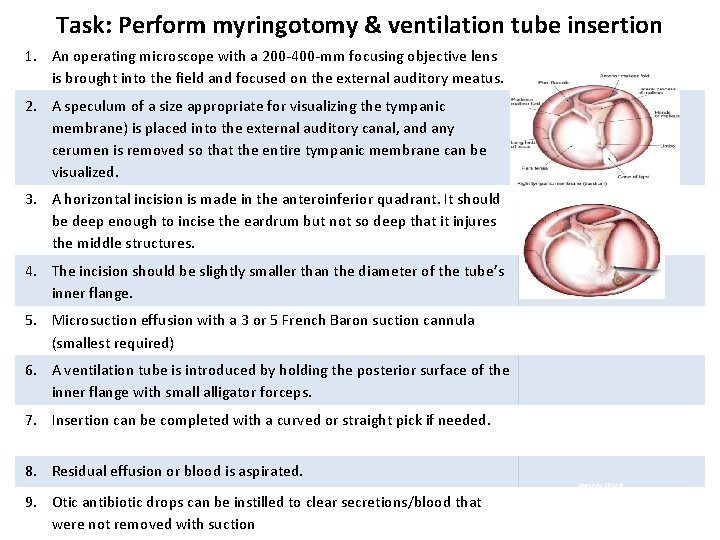
Task: Perform myringotomy & ventilation tube insertion 1. An operating microscope with a 200 -400 -mm focusing objective lens is brought into the field and focused on the external auditory meatus. 2. A speculum of a size appropriate for visualizing the tympanic membrane) is placed into the external auditory canal, and any cerumen is removed so that the entire tympanic membrane can be visualized. 3. A horizontal incision is made in the anteroinferior quadrant. It should be deep enough to incise the eardrum but not so deep that it injures the middle structures. 4. The incision should be slightly smaller than the diameter of the tube’s inner flange. 5. Microsuction effusion with a 3 or 5 French Baron suction cannula (smallest required) 6. A ventilation tube is introduced by holding the posterior surface of the inner flange with small alligator forceps. 7. Insertion can be completed with a curved or straight pick if needed. 8. Residual effusion or blood is aspirated. Mercado 2011 © 9. Otic antibiotic drops can be instilled to clear secretions/blood that were not removed with suction
Myringotomy & Tympanostomy Tube Demonstration Eighth Annual ENT for the PA-C | April 25 – 29, 2018| Scottsdale, AZ
Intratympanic Injection Eighth Annual ENT for the PA-C | April 25 – 29, 2018| Scottsdale, AZ
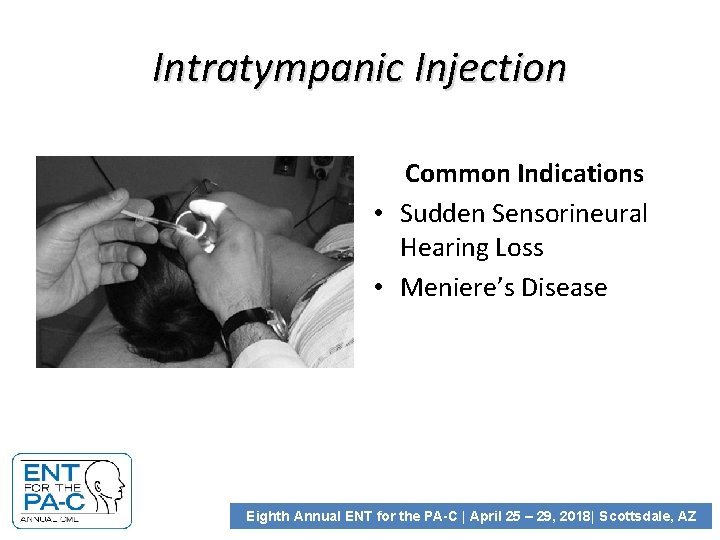
Intratympanic Injection Common Indications • Sudden Sensorineural Hearing Loss • Meniere’s Disease Eighth Annual ENT for the PA-C | April 25 – 29, 2018| Scottsdale, AZ
Sudden Hearing Loss: Definition Eighth Annual ENT for the PA-C | April 25 – 29, 2018| Scottsdale, AZ
AAO CLINICAL PRACTICE GUIDELINES 2012 Eighth Annual ENT for the PA-C | April 25 – 29, 2018| Scottsdale, AZ
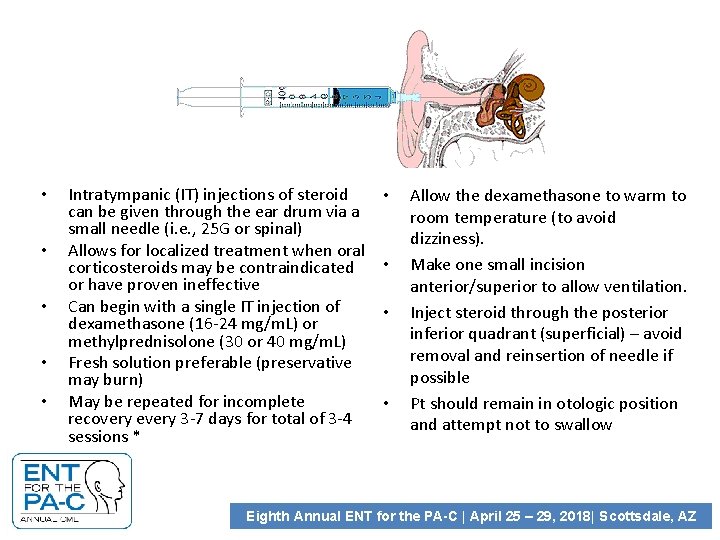
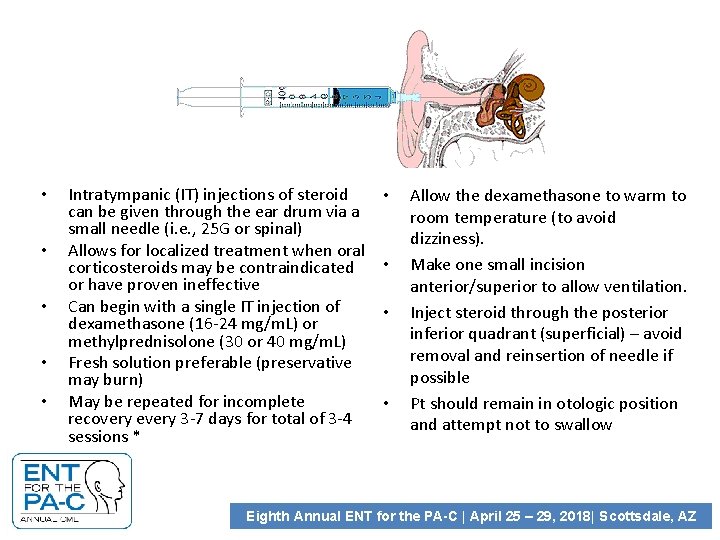
• • • Intratympanic (IT) injections of steroid can be given through the ear drum via a small needle (i. e. , 25 G or spinal) Allows for localized treatment when oral corticosteroids may be contraindicated or have proven ineffective Can begin with a single IT injection of dexamethasone (16 -24 mg/m. L) or methylprednisolone (30 or 40 mg/m. L) Fresh solution preferable (preservative may burn) May be repeated for incomplete recovery every 3 -7 days for total of 3 -4 sessions * • • Allow the dexamethasone to warm to room temperature (to avoid dizziness). Make one small incision anterior/superior to allow ventilation. Inject steroid through the posterior inferior quadrant (superficial) – avoid removal and reinsertion of needle if possible Pt should remain in otologic position and attempt not to swallow Eighth Annual ENT for the PA-C | April 25 – 29, 2018| Scottsdale, AZ

Task: Perform Intratympanic injection 1. Explain Procedure. Prepare supplies. Allow the dexamethasone to warm to room temperature (to limit caloric response). 2. Position patient 3. Apply anesthetic Mercado 2013 © 4. Make ventilation incision- usually anterosuperior 5. Inject the steroid slowly once a very superficial myringotomy site has been established posteriorly with careful attention to avoid contact with the ossicular chain or any middle ear structure
Intratympanic Injection Demonstration of intratympanic injection procedure Eighth Annual ENT for the PA-C | April 25 – 29, 2018| Scottsdale, AZ
Paper Patch Myringoplasty • Small chronic perforations – Overall closure rate 62. 8%, perforations < 5% at 78. 3%, >5% at 45%. • Topical phenol or trichloroacetic acid is applied to the edges of the perforation with a wisp of cotton on an applicator. • A sharp pick is then used to freshen the margins of the tympanic membrane perforation to allow removal of the edges of the perforation. • This technique removes any squamous epithelium that may have migrated under the medial surface of the tympanic membrane at the edge of the perforation and stimulates bleeding and healing from the local vascular supply
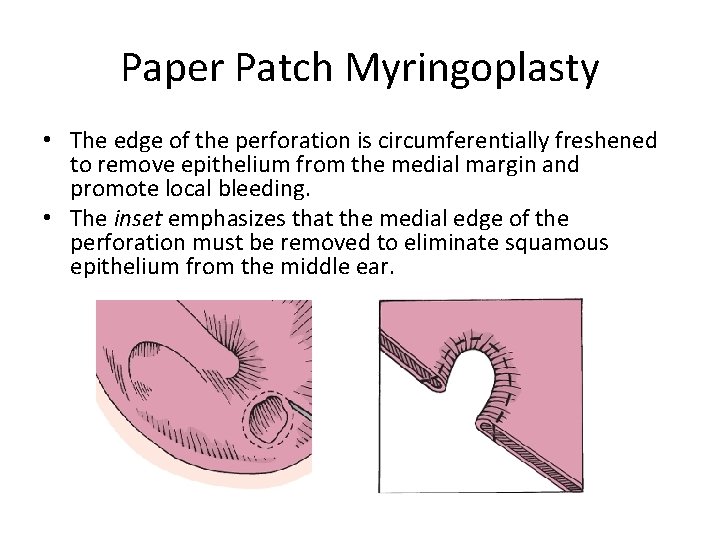
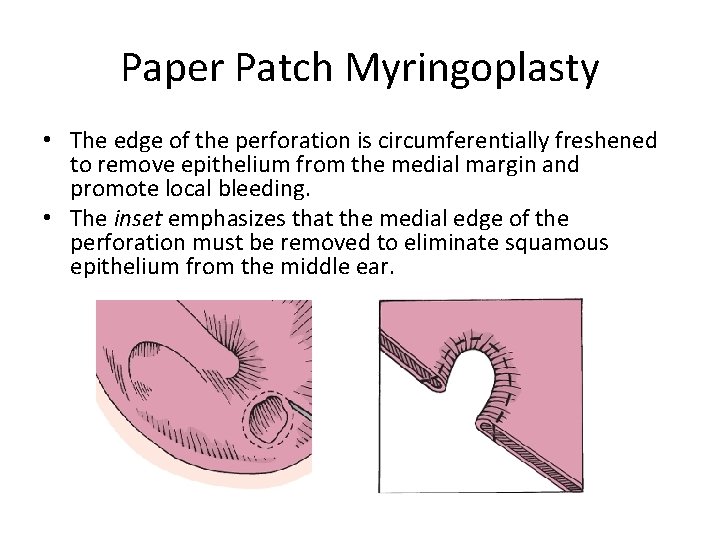
Paper Patch Myringoplasty • The edge of the perforation is circumferentially freshened to remove epithelium from the medial margin and promote local bleeding. • The inset emphasizes that the medial edge of the perforation must be removed to eliminate squamous epithelium from the middle ear.
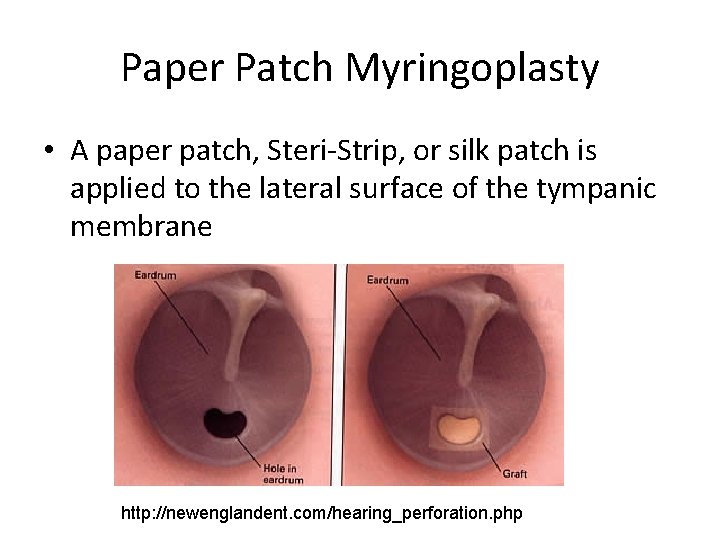
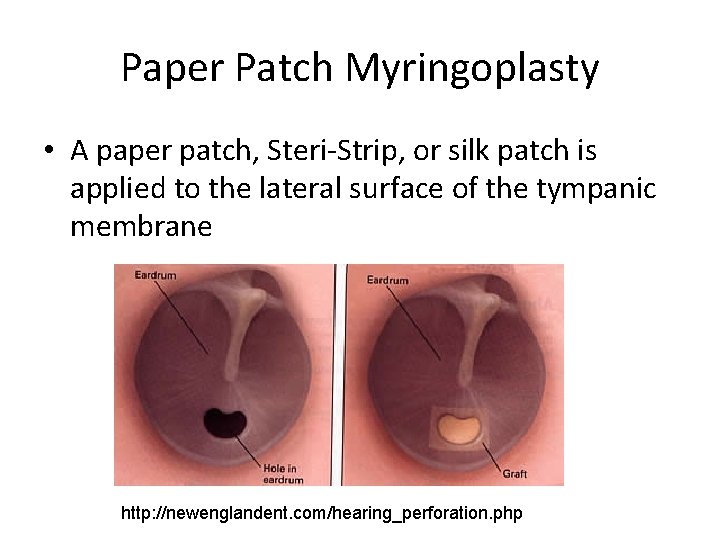
Paper Patch Myringoplasty • A paper patch, Steri-Strip, or silk patch is applied to the lateral surface of the tympanic membrane http: //newenglandent. com/hearing_perforation. php
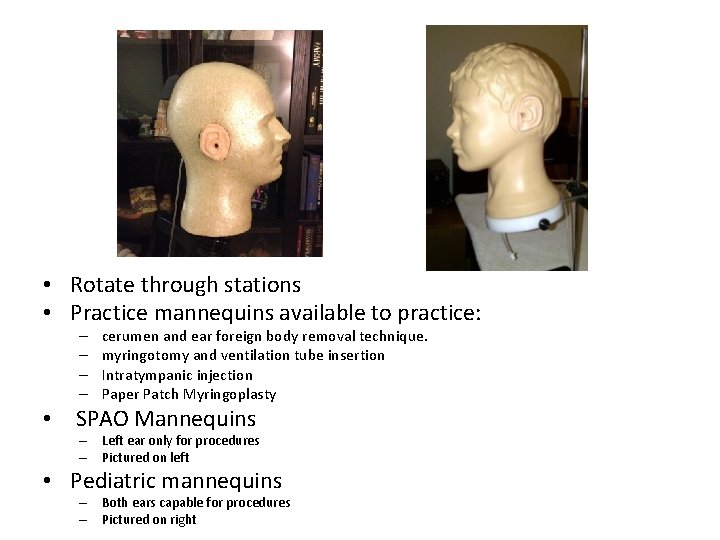
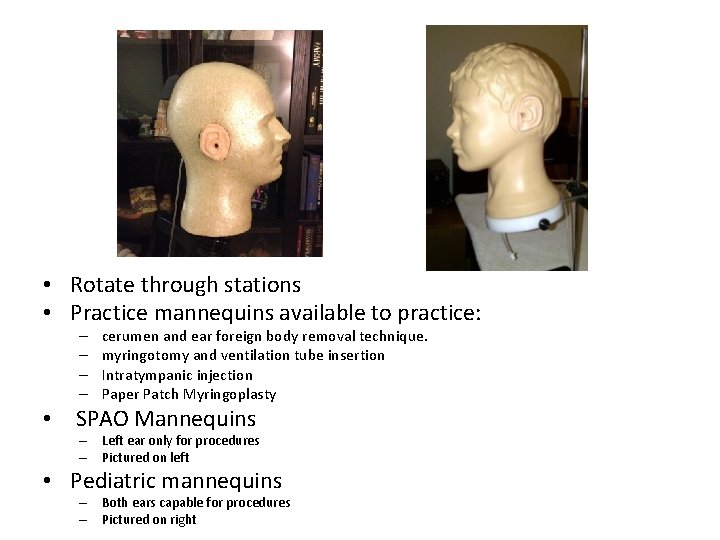
• Rotate through stations • Practice mannequins available to practice: – – cerumen and ear foreign body removal technique. myringotomy and ventilation tube insertion Intratympanic injection Paper Patch Myringoplasty • SPAO Mannequins – Left ear only for procedures – Pictured on left • Pediatric mannequins – Both ears capable for procedures – Pictured on right
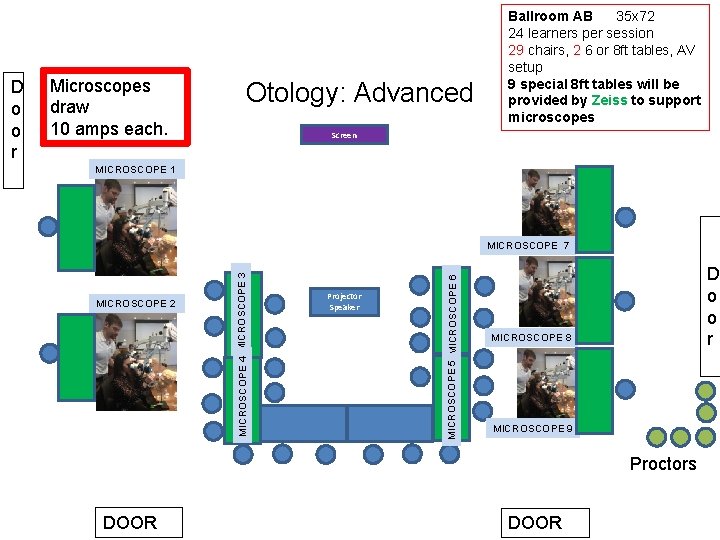
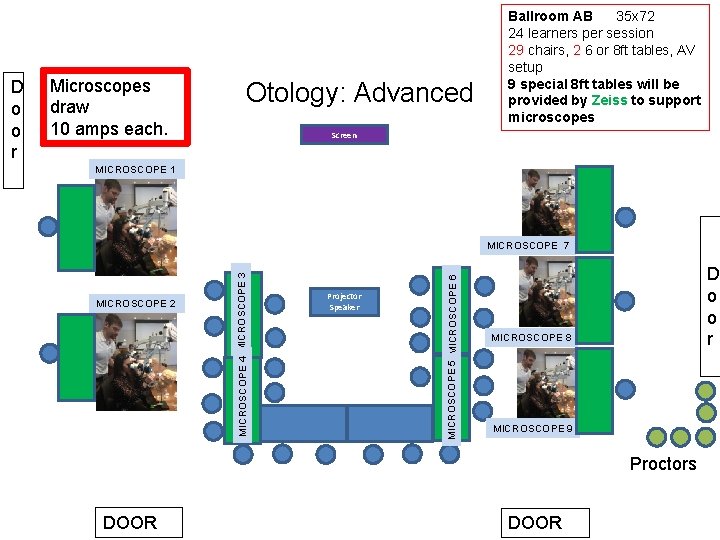
Microscopes draw 10 amps each. Otology: Advanced Screen MICROSCOPE 1 MICROSCOPE 2 Projector Speaker MICROSCOPE 5 MICROSCOPE 6 MICROSCOPE 7 MICROSCOPE 4 MICROSCOPE 3 D o o r Ballroom AB 35 x 72 24 learners per session 29 chairs, 2 6 or 8 ft tables, AV setup 9 special 8 ft tables will be provided by Zeiss to support microscopes D o o r MICROSCOPE 8 MICROSCOPE 9 Proctors DOOR
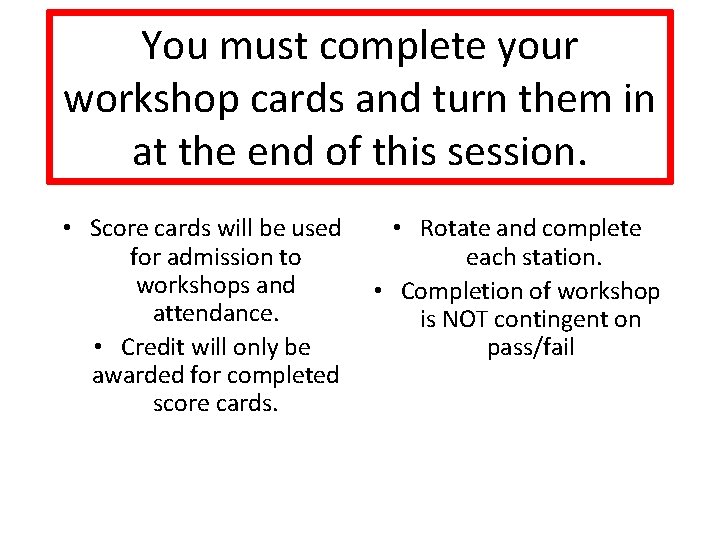
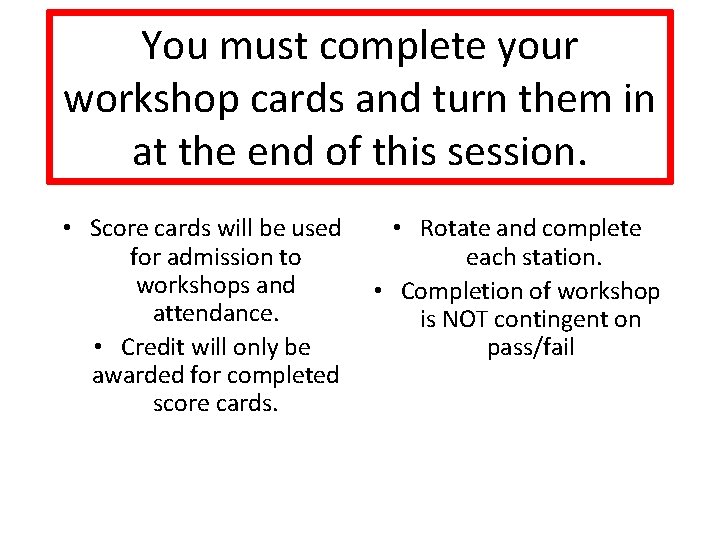
You must complete your workshop cards and turn them in at the end of this session. • Score cards will be used for admission to workshops and attendance. • Credit will only be awarded for completed score cards. • Rotate and complete each station. • Completion of workshop is NOT contingent on pass/fail
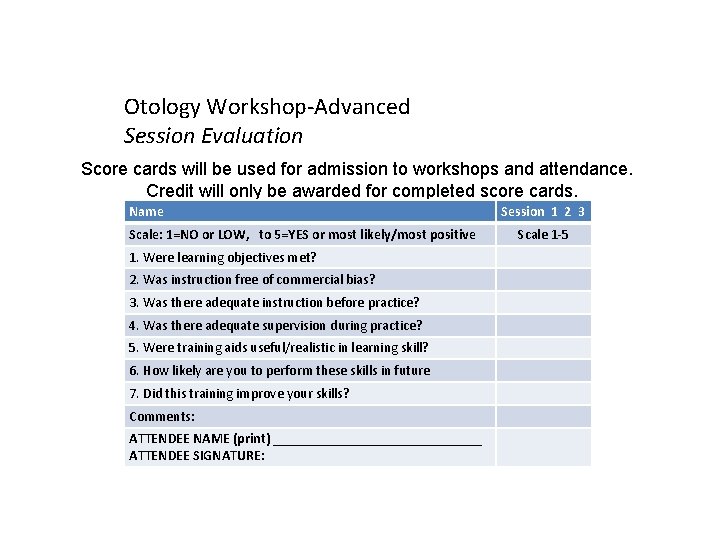
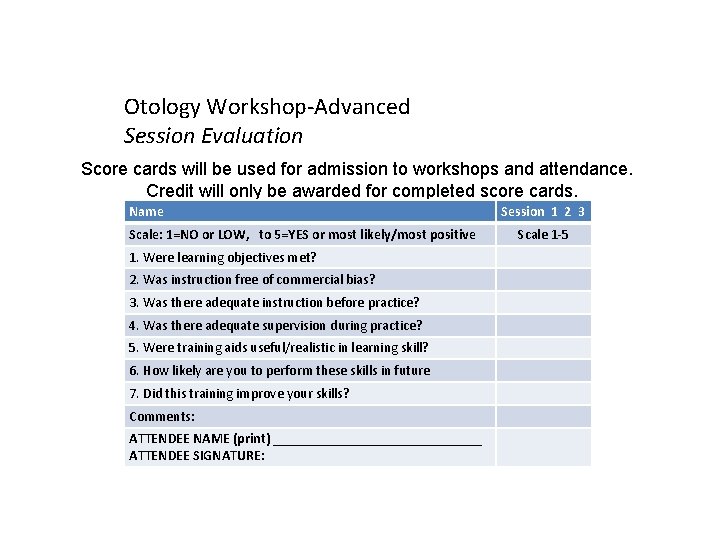
Otology Workshop-Advanced Session Evaluation Score cards will be used for admission to workshops and attendance. Credit will only be awarded for completed score cards. Name Scale: 1=NO or LOW, to 5=YES or most likely/most positive 1. Were learning objectives met? 2. Was instruction free of commercial bias? 3. Was there adequate instruction before practice? 4. Was there adequate supervision during practice? 5. Were training aids useful/realistic in learning skill? 6. How likely are you to perform these skills in future 7. Did this training improve your skills? Comments: ATTENDEE NAME (print) _______________ ATTENDEE SIGNATURE: Session 1 2 3 Scale 1 -5
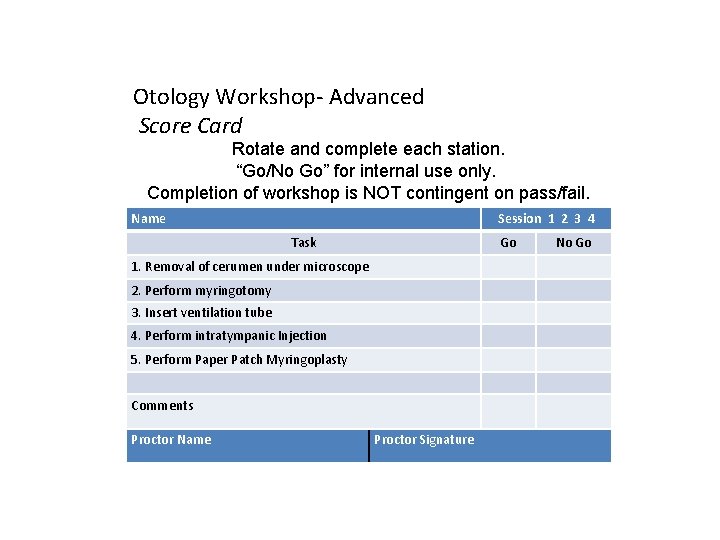
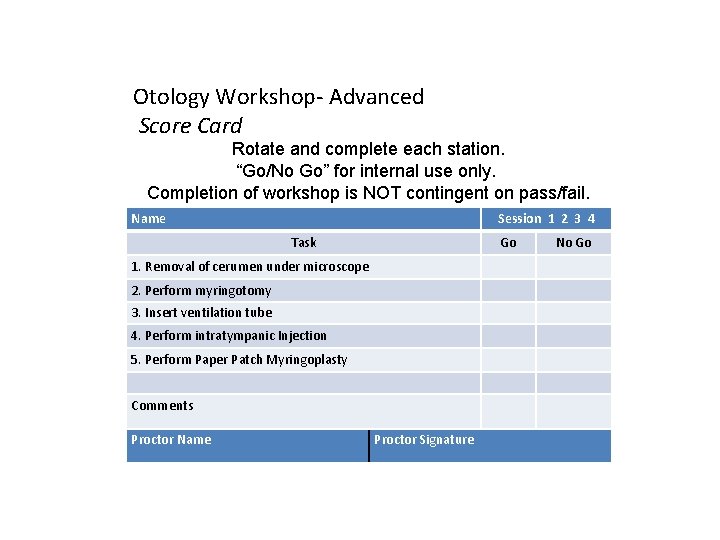
Otology Workshop- Advanced Score Card Rotate and complete each station. “Go/No Go” for internal use only. Completion of workshop is NOT contingent on pass/fail. Name Session 1 2 3 4 Task Go 1. Removal of cerumen under microscope 2. Perform myringotomy 3. Insert ventilation tube 4. Perform intratympanic Injection 5. Perform Paper Patch Myringoplasty Comments Proctor Name Proctor Signature No Go
 Scottsdale fire station
Scottsdale fire station Scottsdale explantation
Scottsdale explantation Scottsdale preparatory academy
Scottsdale preparatory academy Senior center scottsdale
Senior center scottsdale Hindu temples in arizona
Hindu temples in arizona Dada la siguiente secuencia rusia 2018 rusia 2018
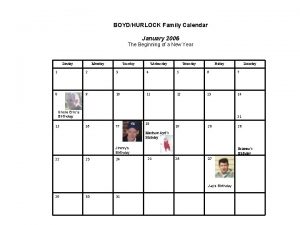
Dada la siguiente secuencia rusia 2018 rusia 2018 Paula hurlock birthday
Paula hurlock birthday 30 days has september april june and november
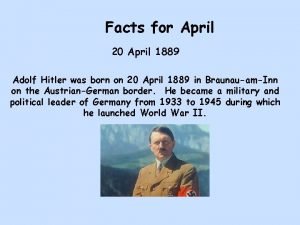
30 days has september april june and november 20.april 1889
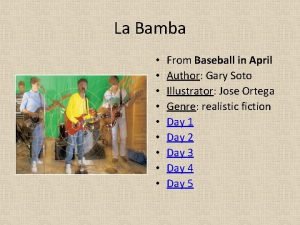
20.april 1889 La bamba by gary soto
La bamba by gary soto April bjornsen
April bjornsen April 8th in history
April 8th in history April 1958
April 1958 Play in a day
Play in a day Amsterdam 27 april
Amsterdam 27 april Tiffany scroggins
Tiffany scroggins Apod nasa calendar 26 april 2004
Apod nasa calendar 26 april 2004 International day april 4
International day april 4 April piscids
April piscids 8 day week
8 day week April 23 1564
April 23 1564 What is april dedicated to
What is april dedicated to 30 tage hat september april juni und november
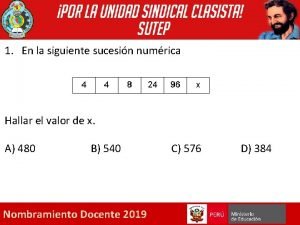
30 tage hat september april juni und november Berikut ini merupakan definisi pajak kecuali
Berikut ini merupakan definisi pajak kecuali April 23 1564
April 23 1564 27 april 2003
27 april 2003 January february march april may
January february march april may Sonnet 64
Sonnet 64 April raintree summary
April raintree summary How to read p
How to read p April school activities
April school activities Falske computer timeshare company
Falske computer timeshare company April kindergarten newsletter
April kindergarten newsletter 1889 april 20
1889 april 20 Morning night april
Morning night april 3 april 2008
3 april 2008 When in april the sweet showers fall
When in april the sweet showers fall Meaning
Meaning