AN UNUSUAL CASE OF CHRONIC DIARRHOEA Dr Shivam







- Slides: 16
AN UNUSUAL CASE OF CHRONIC DIARRHOEA Dr. Shivam Sharma Dept. of General Medicine

Presentation A 28 year old male presented with Ø Diarrhoea and weight loss of 5 Kg over a period of 6 months refractory to standard treatment Ø Frequent episodes of abdominal pain since 2 months. Clinical examination was normal. Routine hematology and biochemistry was normal. Serology for HBV, HIV was negative. Stool routine microscopy was normal. Ultrasonography of abdomen & pelvis was normal.
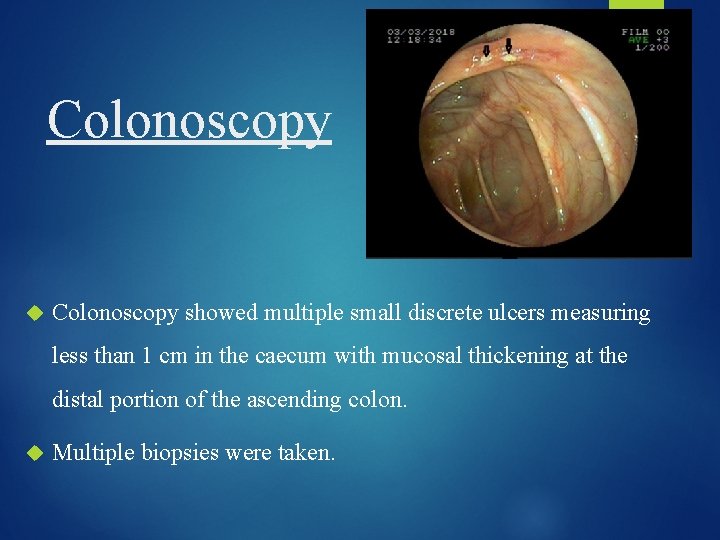
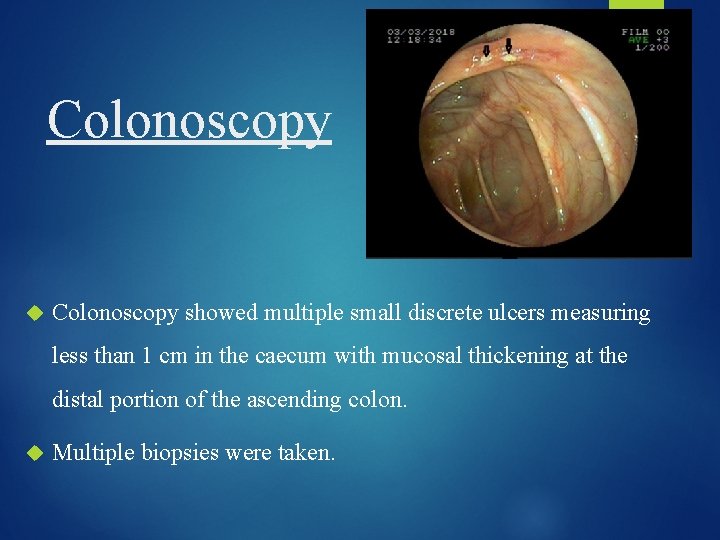
Colonoscopy showed multiple small discrete ulcers measuring less than 1 cm in the caecum with mucosal thickening at the distal portion of the ascending colon. Multiple biopsies were taken.

CECT Abdomen CECT abdomen showed asymmetrical thickening (maximum 11 mm) of the caecal wall with moderate thickening of ileocaecal valve. Other organs were normal.
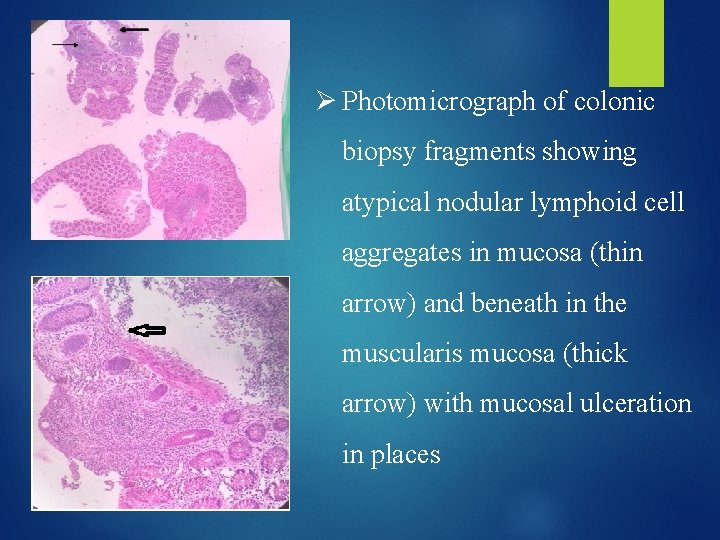
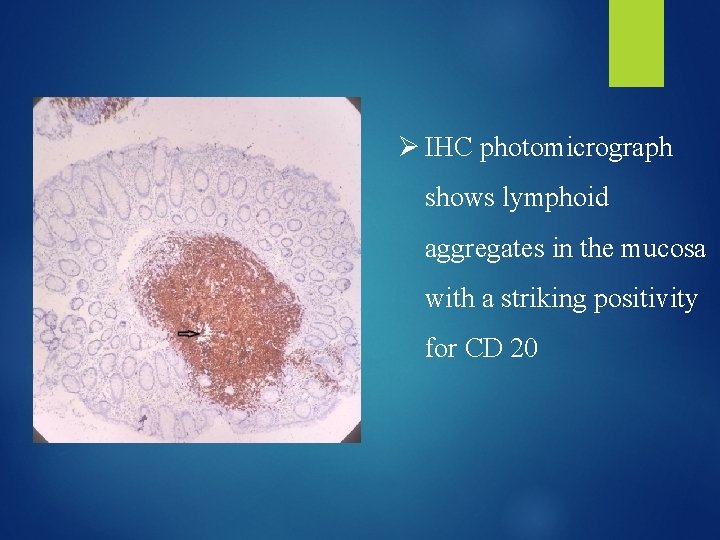
Histopathology We received multiple fragmented biopsy bits from colon HPE revealed large bowel mucosa with ulceration and atypical nodular lymphoid cell aggregates involving the submucosa and muscularis propria.
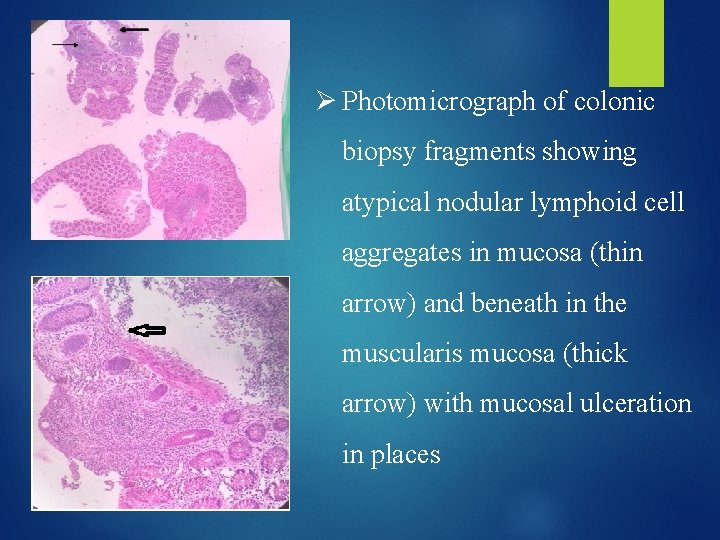
Ø Photomicrograph of colonic biopsy fragments showing atypical nodular lymphoid cell aggregates in mucosa (thin arrow) and beneath in the muscularis mucosa (thick arrow) with mucosal ulceration in places
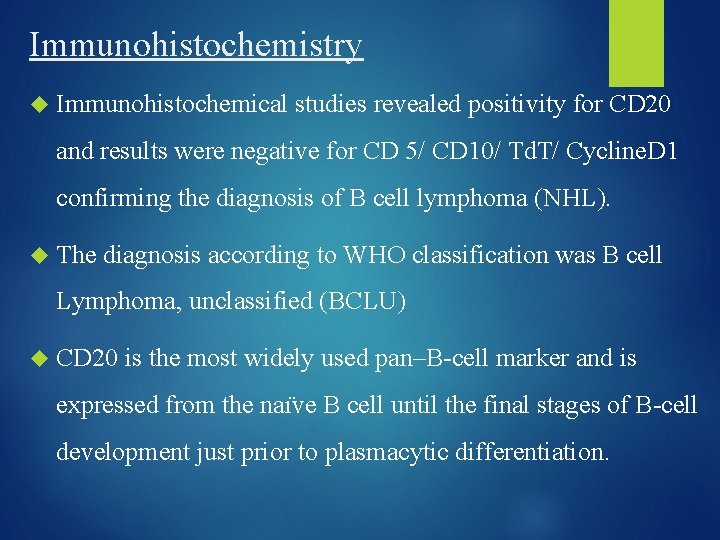
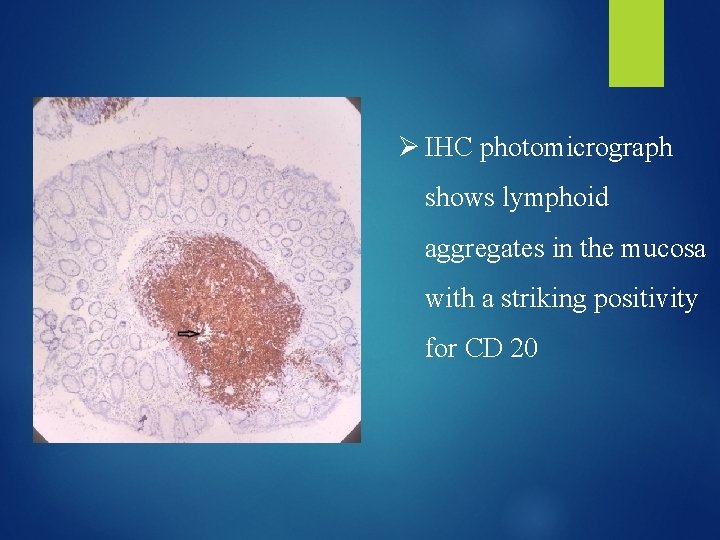
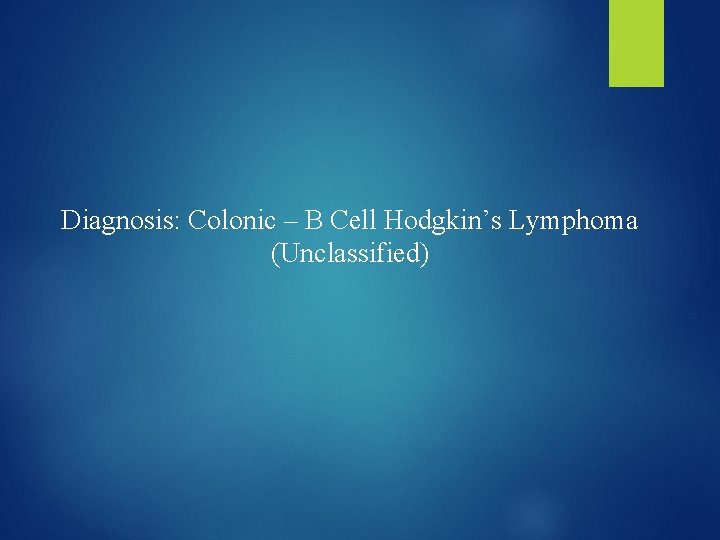
Immunohistochemistry Immunohistochemical studies revealed positivity for CD 20 and results were negative for CD 5/ CD 10/ Td. T/ Cycline. D 1 confirming the diagnosis of B cell lymphoma (NHL). The diagnosis according to WHO classification was B cell Lymphoma, unclassified (BCLU) CD 20 is the most widely used pan–B-cell marker and is expressed from the naı ve B cell until the final stages of B-cell development just prior to plasmacytic differentiation.
Ø IHC photomicrograph shows lymphoid aggregates in the mucosa with a striking positivity for CD 20
Diagnosis: Colonic – B Cell Hodgkin’s Lymphoma (Unclassified)

Ø PET scan was performed with 7. 5 m. Ci of 18 FDG, it showed circumferential thickening of caecum. Ø FDG uptake was seen in multiple mesenteric nodes measuring 1. 5 x 1. 2 cm, sub-centric aortocaval node, mildly enhancing mesenteric thickening along the SMV.
Diagnosis Ø To conclude, the patient had a metabolically active caecal wall thickening consistent with histological diagnosis of lymphoma. Ø The presence of metabolically active mesenteric and aortocaval lymph nodes were noted. Ø The staging of this case was BCLU T 3 N 3 M 0 B 0 according to Paris Staging system which is specifically meant for primary gastrointestinal lymphomas. Ø Final Diagnosis - Primary B cell Lymphoma of Caecum and Colon presenting as an ulcerative lesion in a young male.

Treatment Patient was advised R-CHOP regimen (Rituximab, Cyclophosphamide, Doxorubicin, Vincristine, Prednisolone) as treatment option.

Discussion Non-Hodgkin lymphomas (NHLs) commonly present as lymphadenopathy. Primary NHL accounts for 0. 1%-0. 5% of all colorectal malignant disease, with most common being the Diffuse Large B cell Lymphoma. [1] The most common symptoms of colonic lymphoma are abdominal pain and weight loss, with a palpable abdominal mass[2]
Tumour was considered to be primary because: No palpable superficial lymphadenopathy at the first examination No obvious enlargement of the mediastinal nodes on chest x ray Normal TLC, DLC and normal bone marrow examination SPECT scan showed no focal lesions in the liver, spleen, and bone marrow No FDG uptake in liver and spleen

On endoscopic examination, primary B-cell lymphomas of gut usually present as exophytic lesions, which also provides specimen for histologic diagnosis. [3] Primary intestinal lymphoma is mostly seen in the ileocaecal region, probably due to presence of high lymphoid tissue. Involvement of regional lymph nodes has a bad prognosis[4] BCLU Hence, is curable with surgery and or chemotherapy. lymphoma should also be considered as a differential diagnosis in patients presenting with colonic ulcers even though it is an uncommon manifestation.

REFERENCES 1) Kumar KM, Indira V, Reddy CK, Swetha K, Vujhini SK. Diffuse Large B-Cell Lymphoma of the Caecum in a Non-HIV Patient - A Rare Occurrence: Case Report. Sch. Acad. J. Biosci. , 2014; 2(9): 613 -617 2) Bairey O, Ruchlemer R, Shpilberg O. Non-Hodgkin’s Lymphomas of the Colon. IMAJ 2006; 8: 832– 835 3) Wu PH, Chu KE, Lina YM, Huang SH , Wu CC T-Cell Lymphomas Presenting as Colon Ulcers and Eosinophilia. Case Rep Gastroenterol. 2015 May-Aug; 9(2): 246– 252. 4) Jayabackthan L, Murgi SB, Graham S, Kini RG. A rare case of primary lymphoma of the caecum presenting as intussusception. J Lab Physicians 2013; 5: 118 -20.
 Shivam ispat
Shivam ispat Among the four students of class 5 radha , meera
Among the four students of class 5 radha , meera Imnci guidelines for diarrhoea
Imnci guidelines for diarrhoea Spluttering diarrhoea
Spluttering diarrhoea Diarrhea types
Diarrhea types Prevention of diarrhoea
Prevention of diarrhoea Nursing management of diarrhoea
Nursing management of diarrhoea Dr sudhanshu mishra
Dr sudhanshu mishra Hyperkalemia symptoms and signs
Hyperkalemia symptoms and signs Imnci color coding
Imnci color coding Nice guidelines diarrhoea and vomiting in adults
Nice guidelines diarrhoea and vomiting in adults Bell's diarrhoea
Bell's diarrhoea Flora git drop
Flora git drop Imnci guidelines for diarrhoea
Imnci guidelines for diarrhoea Bell's diarrhoea repertory
Bell's diarrhoea repertory Monilial diarrhoea
Monilial diarrhoea Prevention of diarrhoea
Prevention of diarrhoea