Chapter 5 Diarrhoea Case I Case study Sarah



- Slides: 19
Chapter 5 Diarrhoea Case I
Case study: Sarah, a 9 months old girl was brought to the hospital with diarrhoea for 5 days. She was restless and irritable.
What are the stages in the management of Sarah?
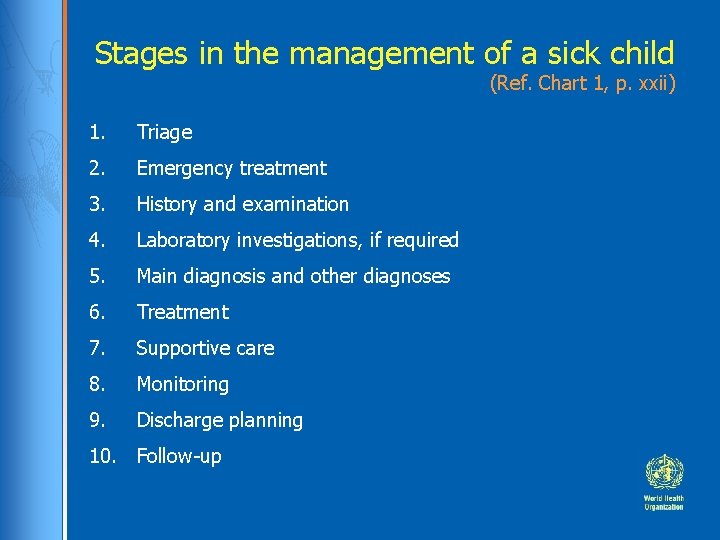
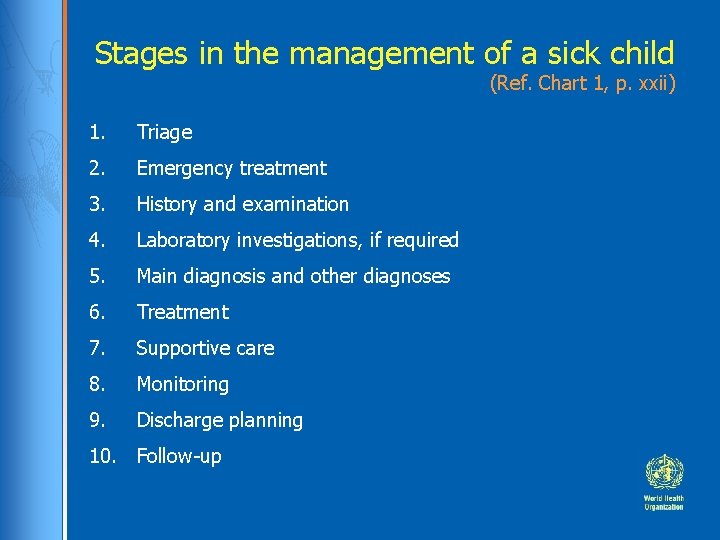
Stages in the management of a sick child (Ref. Chart 1, p. xxii) 1. Triage 2. Emergency treatment 3. History and examination 4. Laboratory investigations, if required 5. Main diagnosis and other diagnoses 6. Treatment 7. Supportive care 8. Monitoring 9. Discharge planning 10. Follow-up
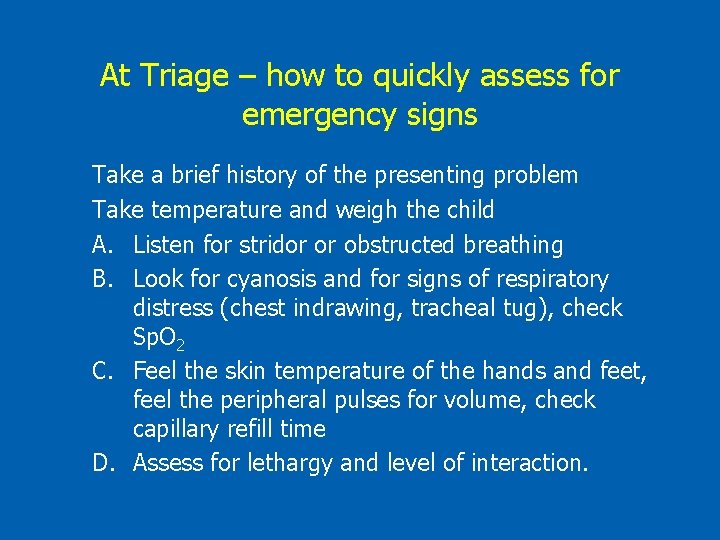
At Triage – how to quickly assess for emergency signs Take a brief history of the presenting problem Take temperature and weigh the child A. Listen for stridor or obstructed breathing B. Look for cyanosis and for signs of respiratory distress (chest indrawing, tracheal tug), check Sp. O 2 C. Feel the skin temperature of the hands and feet, feel the peripheral pulses for volume, check capillary refill time D. Assess for lethargy and level of interaction.
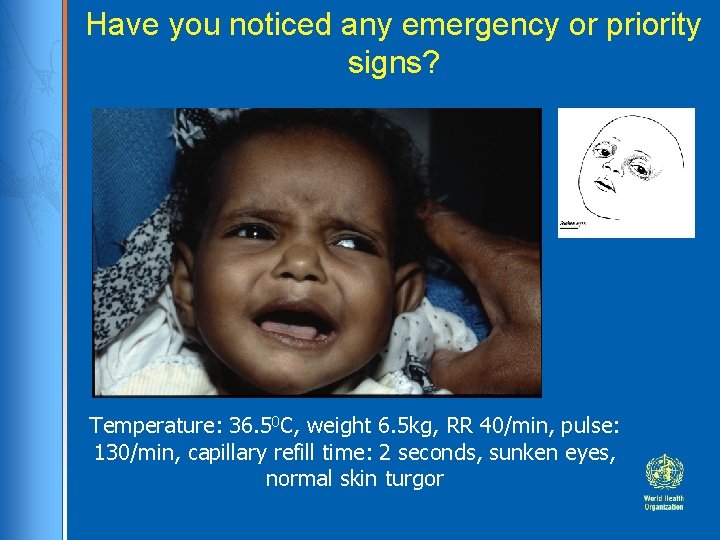
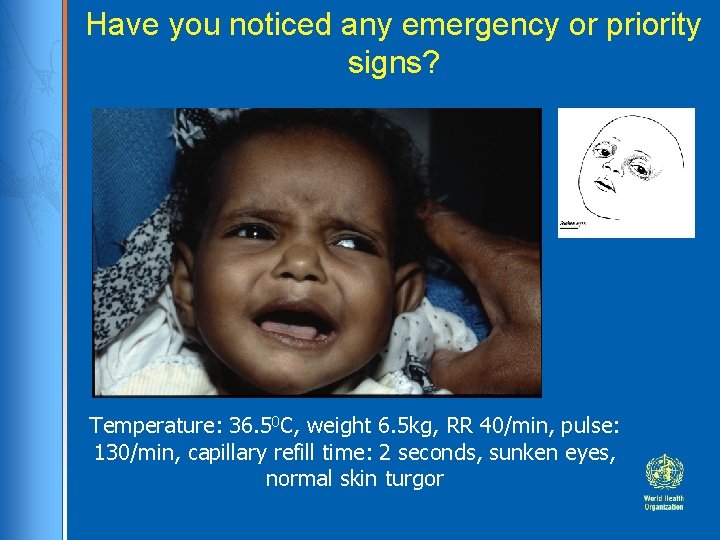
Have you noticed any emergency or priority signs? Temperature: 36. 50 C, weight 6. 5 kg, RR 40/min, pulse: 130/min, capillary refill time: 2 seconds, sunken eyes, normal skin turgor
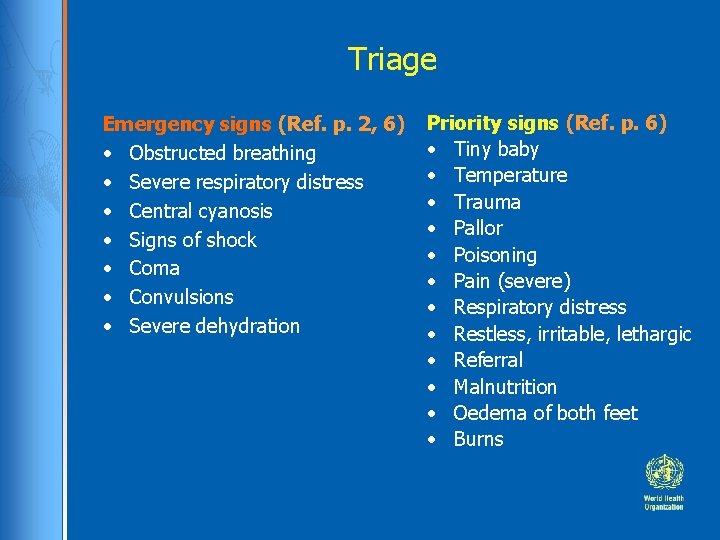
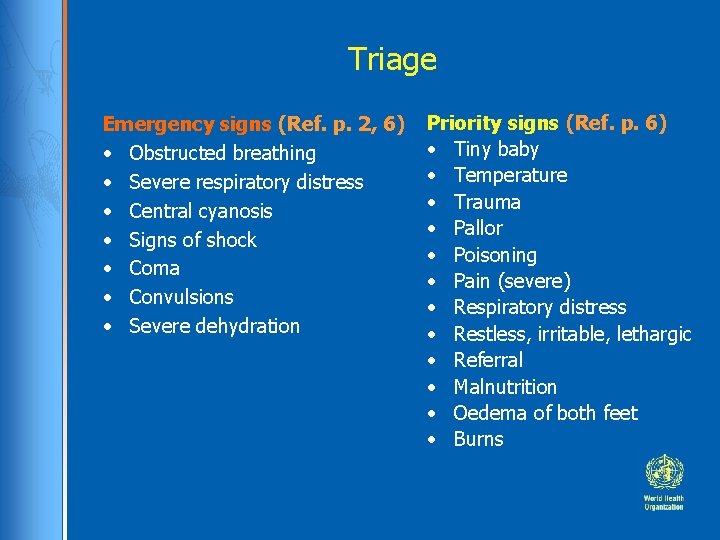
Triage Emergency signs (Ref. p. 2, 6) • Obstructed breathing • Severe respiratory distress • Central cyanosis • Signs of shock • Coma • Convulsions • Severe dehydration Priority signs (Ref. p. 6) • Tiny baby • Temperature • Trauma • Pallor • Poisoning • Pain (severe) • Respiratory distress • Restless, irritable, lethargic • Referral • Malnutrition • Oedema of both feet • Burns
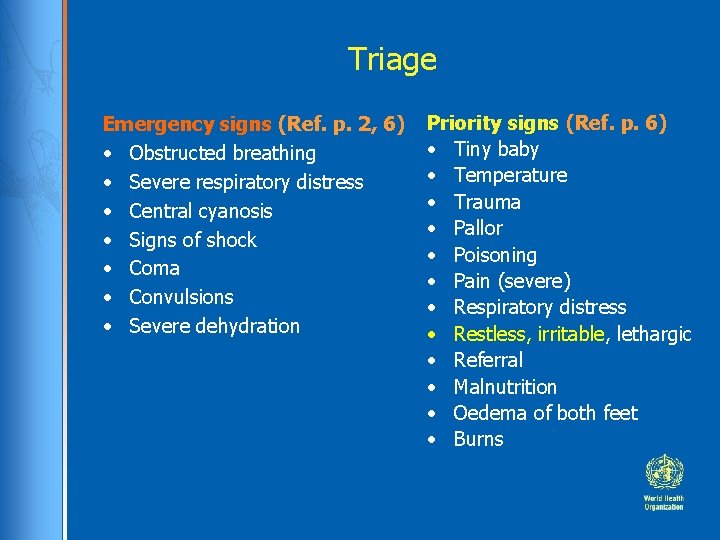
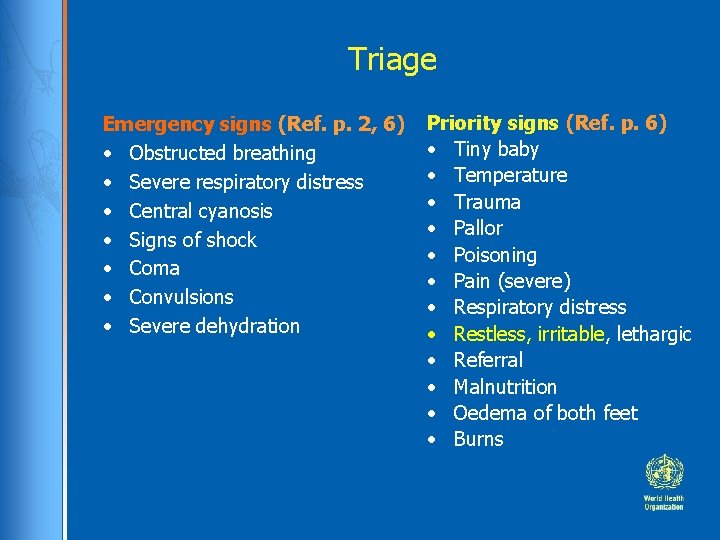
Triage Emergency signs (Ref. p. 2, 6) • Obstructed breathing • Severe respiratory distress • Central cyanosis • Signs of shock • Coma • Convulsions • Severe dehydration Priority signs (Ref. p. 6) • Tiny baby • Temperature • Trauma • Pallor • Poisoning • Pain (severe) • Respiratory distress • Restless, irritable, lethargic • Referral • Malnutrition • Oedema of both feet • Burns
History Sarah was well until 5 days ago, then she started having loose watery stools 6 -10 times per day. • Vomited the last 2 days, 2 times each day • There was no blood or pus in the stool. • Past medical history: previously well, no significant past history • Immunization: up to date according to vaccine schedule, measles vaccine due at 9 months • Social history: lives with her mother and sister, 4 years old • Medications: none
Examination Sarah was crying continuously, she only stopped briefly when her mother put her to her breast. When she was offered ORS she drank eagerly. Vital signs: temperature: 36. 5 °C, RR: 40/min, pulse: 130/min Weight: 6. 5 kg Eyes: sunken Skin: normal skin turgor (skin pinch goes back immediately) Chest: air entry was good bilaterally and there were no added sounds Cardiovascular: both heart sounds were audible and there was no murmur Abdomen: soft and doughy, bowel sounds active and there was no organomegaly Neurology: restless and irritable; no neck stiffness
Differential diagnoses List possible causes of the illness, in order they are likely, use clinical features to say which are most and least likely (Ref. p. 127)
Differential diagnoses What clinical features make these diagnoses most or less likely? • Acute watery diarrhoea • Cholera • Dysentery • Persistent diarrhoea • Diarrhoea with severe malnutrition • Diarrhoea associated with recent antibiotic use • Intussusception
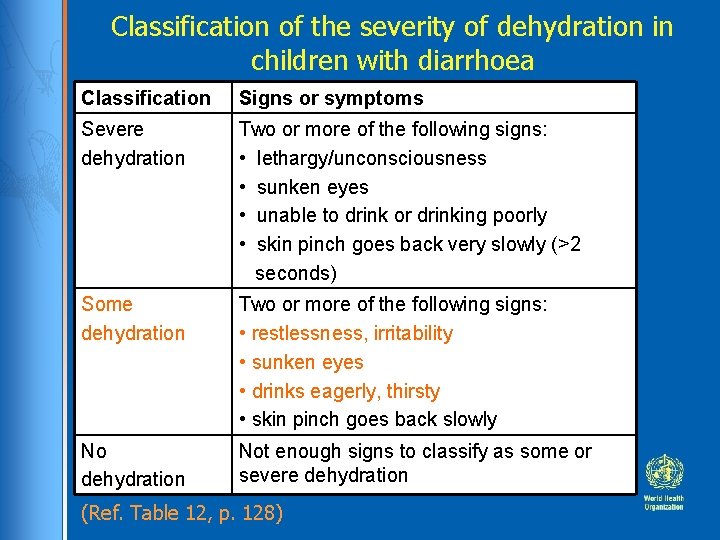
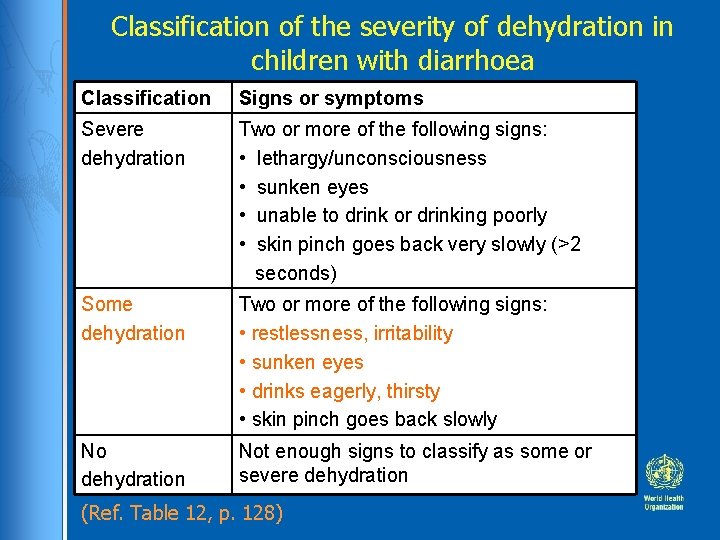
Classification of the severity of dehydration in children with diarrhoea Classification Signs or symptoms Severe dehydration Two or more of the following signs: • lethargy/unconsciousness • sunken eyes • unable to drink or drinking poorly • skin pinch goes back very slowly (>2 seconds) Some dehydration Two or more of the following signs: • restlessness, irritability • sunken eyes • drinks eagerly, thirsty • skin pinch goes back slowly No dehydration Not enough signs to classify as some or severe dehydration (Ref. Table 12, p. 128)

Are any investigations needed to make a diagnosis ?

How would you treat Sarah?
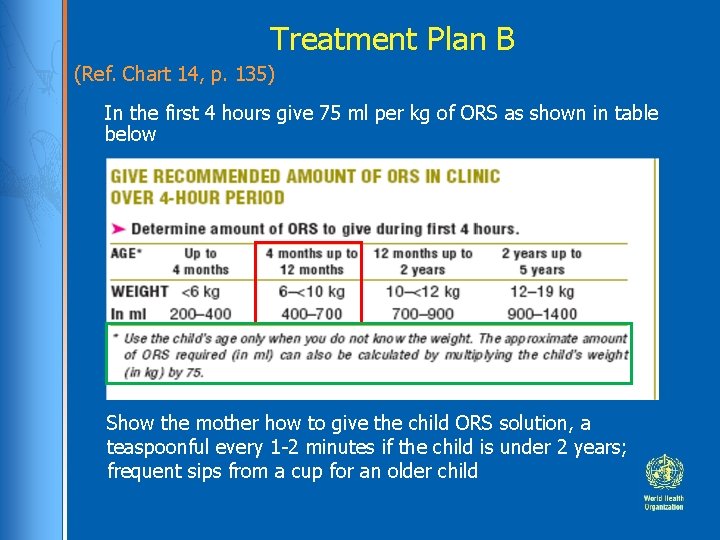
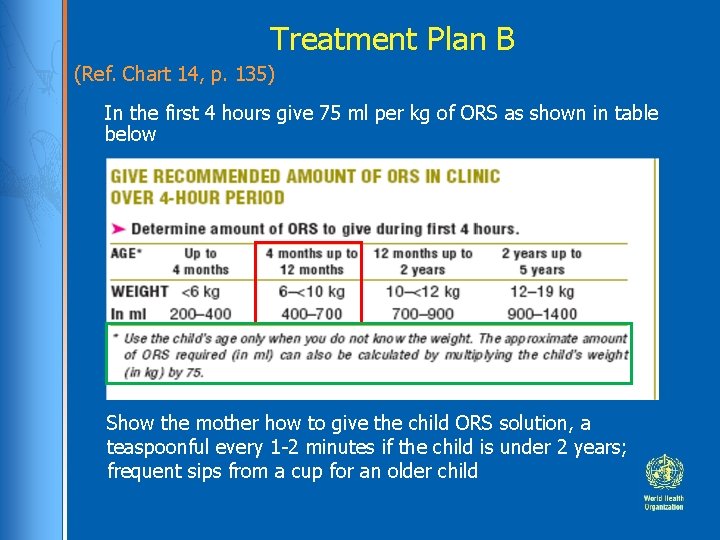
Treatment Plan B (Ref. Chart 14, p. 135) In the first 4 hours give 75 ml per kg of ORS as shown in table below Show the mother how to give the child ORS solution, a teaspoonful every 1 -2 minutes if the child is under 2 years; frequent sips from a cup for an older child

Supportive Care • Check to see if there are problems (Ref. p. 132 -136 ) • Advise mother to continue to breastfeed whenever Sarah wants to feed • Infection control: hand washing
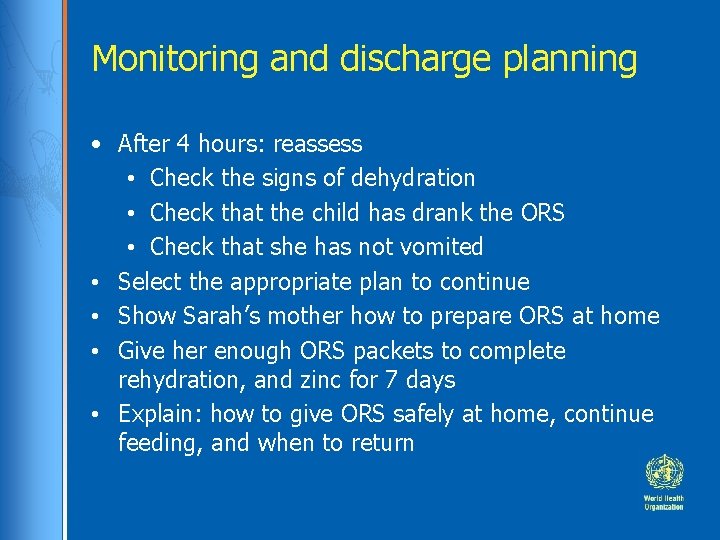
Monitoring and discharge planning • After 4 hours: reassess • Check the signs of dehydration • Check that the child has drank the ORS • Check that she has not vomited • Select the appropriate plan to continue • Show Sarah’s mother how to prepare ORS at home • Give her enough ORS packets to complete rehydration, and zinc for 7 days • Explain: how to give ORS safely at home, continue feeding, and when to return
Summary • Sarah had acute watery diarrhoea and some dehydration • She was rehydrated with ORS and continued breast feeding • She was discharged on the same day after taking ORS for 4 hours (75 ml/kg), without vomiting • At discharge she was alert, and able to drink and eat. • Her mother was given advice on how to give extra fluid, to continue feeding and to return to be checked the following day.