Allergy Wise anaphylaxis training for primary care staff






- Slides: 22
Allergy. Wise anaphylaxis training for primary care staff YOUR NAME
Learning objectives Improved and updated knowledge in managing severe allergies • Early recognition of symptoms • Allergen avoidance • Crisis management which can be used to teach patients and their families, carers and friends • Enhanced skills in the use of adrenaline auto injectors

Key principles of good management ALLERGEN AVOIDANCE EARLY RECOGNITION OF SYMPTOMS CRISIS MANAGEMENT
What is anaphylaxis? Anaphylaxis is a severe life threatening, generalised or systemic hypersensitivity reaction This is characterised by; • Rapidly developing airway and/or • Breathing and/or • Circulation problems • Usually associated with skin or mucosal changes.
Symptoms of anaphylaxis • • Airway swelling, hoarse voice, stridor Difficulty in swallowing or speaking Shortness of breath/ wheeze Signs of shock - pale, clammy Tachycardia and hypotension Urticaria and angioedema Gastro-intestinal symptoms Collapse and unconsciousness

What exactly is going on? • An anaphylaxis reaction is caused by the sudden release of chemical substances, including histamine, from cells in the blood and tissues where they are stored • The release is triggered by the reaction between allergic antibodies (Ig. E) and the allergen
Types of reactions Uni-phasic • Rapidly developing severe reaction involving the airway or circulation Bi-phasic • Early symptoms as above, then a symptom-free period of 1 hour, then increasing symptoms involving breathing and circulation
Common causes Food allergens • Peanuts, treenuts, milk, egg, sesame, fish, shellfish, kiwi, lupin Non-food allergens • Wasp sting, bee sting, latex, penicillin, drugs
Treatments Adrenaline is the mainstay of treatment because it; • Reverses swelling • Relieves asthma • Constricts the blood vessels • Stimulates the heartbeats Antihistamines and asthma inhalers may be helpful
Emerade® auto injector How to use • Remove needle shield About Emerade® • Press the device firmly against the upper, outer thigh • Three doses available; Adult dose 0. 5 mgs & 0. 3 mgs, Child dose 0. 15 mgs • Hold for 5 seconds • 18 month shelf life • Massage the injection site
Epi. Pen® auto injector How to use • Remove blue safety cap • Hold device a few cm away from upper, outer thigh and jab firmly • Listen for click • Hold for 3 seconds About Epi. Pen® • Two doses available; Adult dose 0. 3 mgs, Child dose 0. 15 mgs • 18 month shelf life

Jext® auto injector How to use • Remove yellow safety cap • Place the black injector tip against upper, outer thigh and push firmly • Listen for click • Hold for 10 seconds • Massage the injection site About Jext® • Two doses available; Adult dose 0. 3 mgs, Child dose 0. 15 mgs • 18 month shelf life
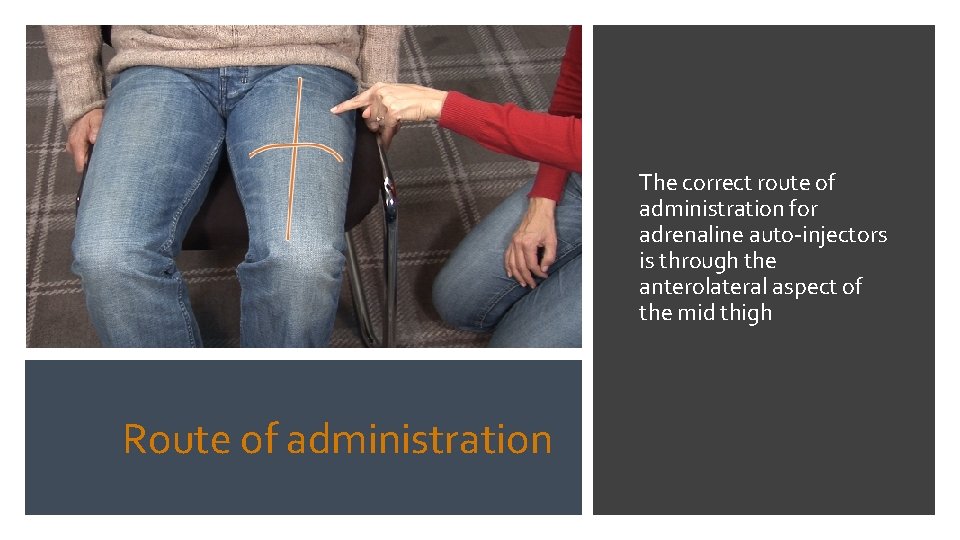
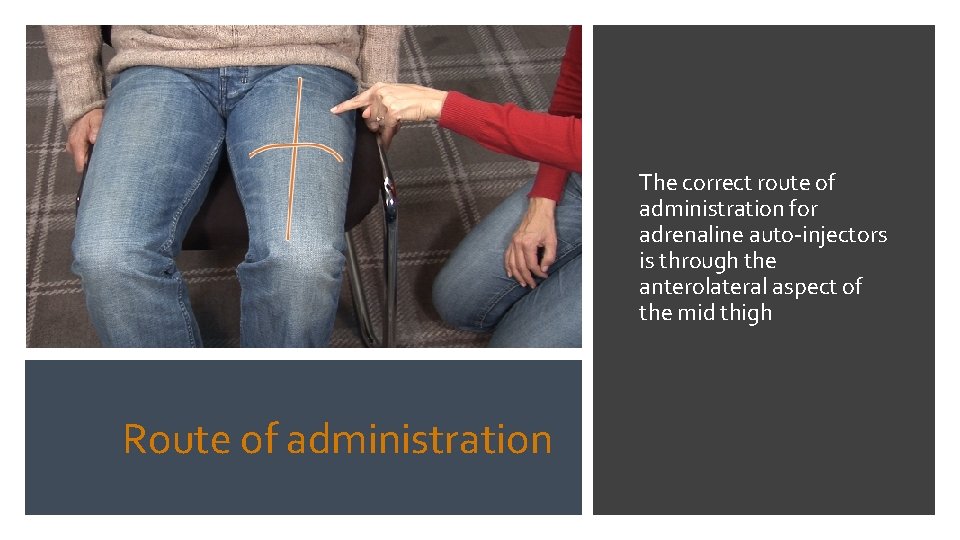
The correct route of administration for adrenaline auto-injectors is through the anterolateral aspect of the mid thigh Route of administration

Personal carrying cases • Accessible • Avoid extremes of temperature • Clearly labelled • In date

Know all about the allergen Know all the names that apply to it Allergen Avoidance – Food Understand the food labelling laws Learn about the high risk foods Think about the high risk situations Be allergy aware and risk assess Factsheets
Ask about any known allergies Allergen Avoidance – non food Record in patients records Check before giving any medications or injections Drug allergy factsheet Insect sting avoidance factsheet
Crisis Management • • • Stay calm and call for help Assess the reaction using the ABCDE approach Ensure the patient is lying down Give IM adrenaline Give high flow oxygen
What to do in an allergic reaction • Continue to monitor blood pressure, oxygen saturation levels and ECG if available • Commence IV fluids if cardiovascular compromise • Further dose of adrenaline can be given after 5 minutes if needed • Transfer to hospital by ambulance

Long term management • Check weight of children to ensure the correct adrenaline dose is prescribed • Ensure good asthma control in your severely allergic patients • Make sure adrenaline injector technique is checked at least annually • Prescribe the adrenaline injector by name to prevent confusion and training concerns.
Want more information? Contact the Anaphylaxis Campaign Helpline • Tel: 01252 542029 • Email: info@anaphylaxis. org. uk • Website: www. anaphylaxis. org. uk