Acute Myeloid Leukaemia Dr Soheir Adam MRCPath Assistant

- Slides: 14
Acute Myeloid Leukaemia Dr. Soheir Adam, MRCPath Assistant Professor Department of Haematology, KAUH
Acute Myeloid Leukaemia n Definition - It is a clonal malignant disease, in which there is maturation arrest of the haemopoietic precursors at an early stage of development - It is characterized by the presence of > 20% blasts in the bone marrow
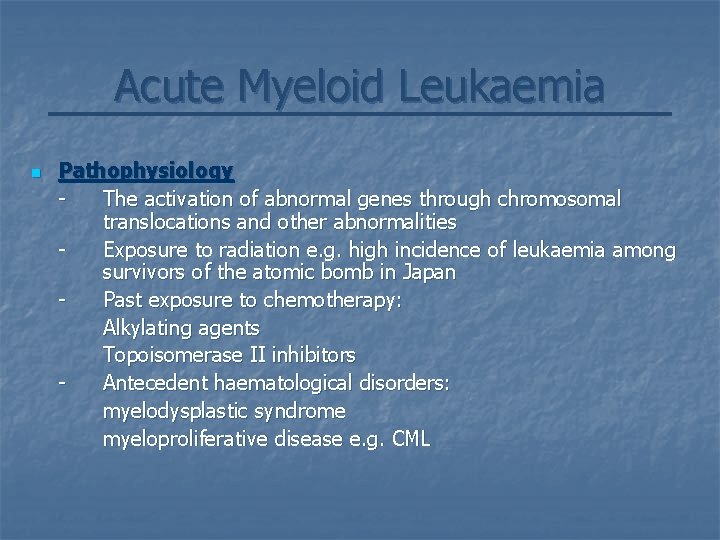
Acute Myeloid Leukaemia n Pathophysiology The activation of abnormal genes through chromosomal translocations and other abnormalities Exposure to radiation e. g. high incidence of leukaemia among survivors of the atomic bomb in Japan Past exposure to chemotherapy: Alkylating agents Topoisomerase II inhibitors Antecedent haematological disorders: myelodysplastic syndrome myeloproliferative disease e. g. CML
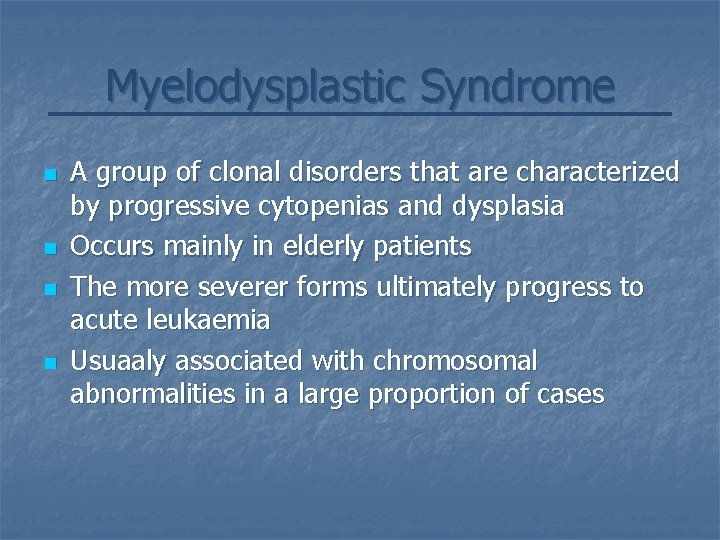
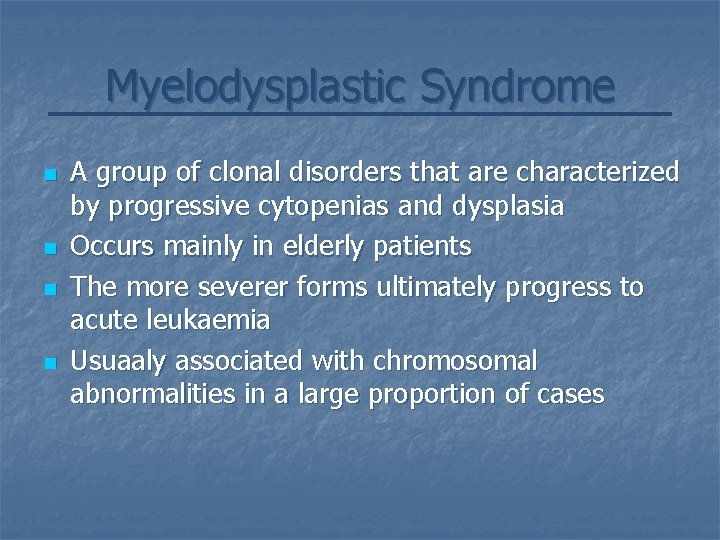
Myelodysplastic Syndrome n n A group of clonal disorders that are characterized by progressive cytopenias and dysplasia Occurs mainly in elderly patients The more severer forms ultimately progress to acute leukaemia Usuaaly associated with chromosomal abnormalities in a large proportion of cases
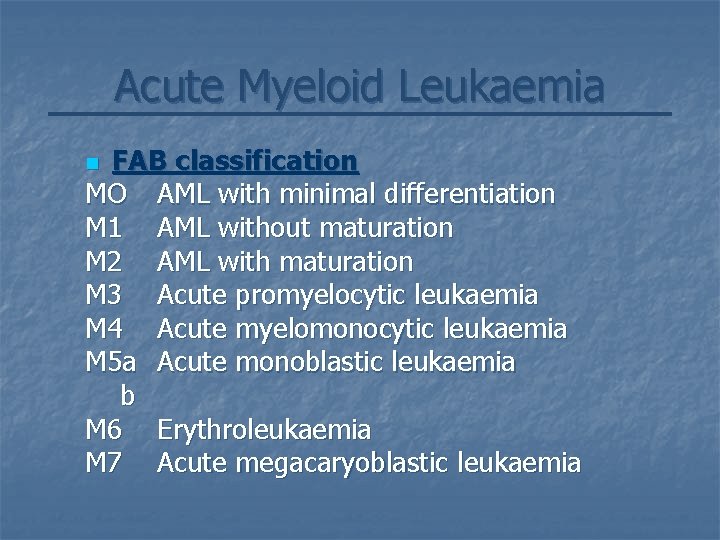
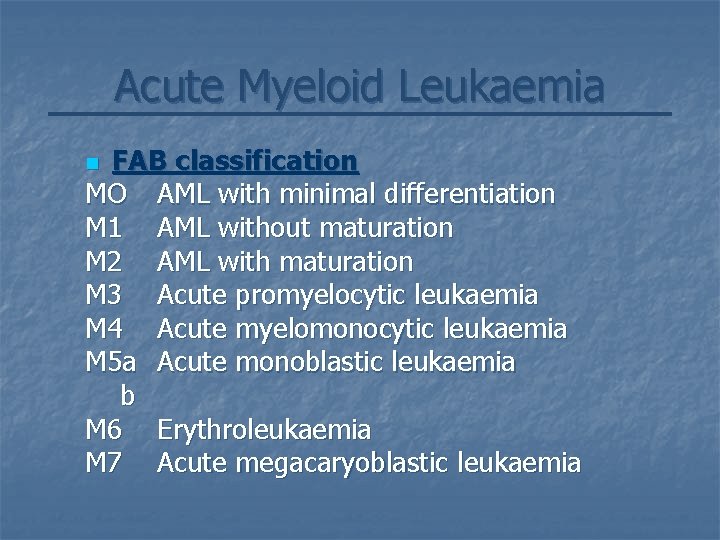
Acute Myeloid Leukaemia FAB classification MO AML with minimal differentiation M 1 AML without maturation M 2 AML with maturation M 3 Acute promyelocytic leukaemia M 4 Acute myelomonocytic leukaemia M 5 a Acute monoblastic leukaemia b M 6 Erythroleukaemia M 7 Acute megacaryoblastic leukaemia n
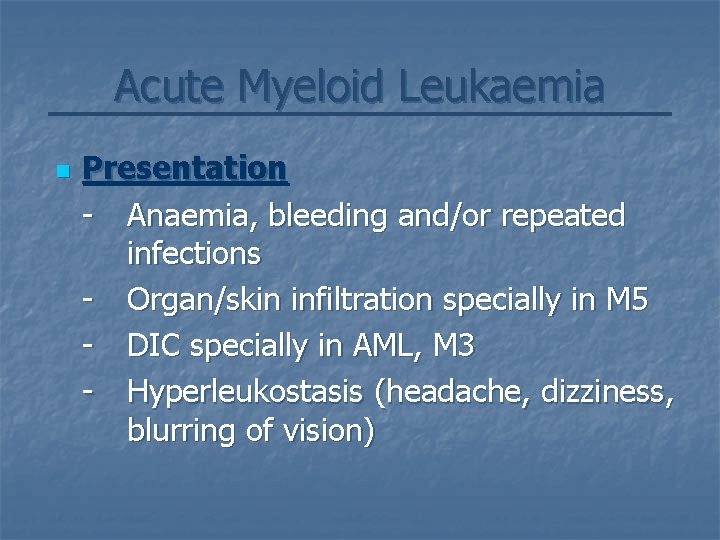
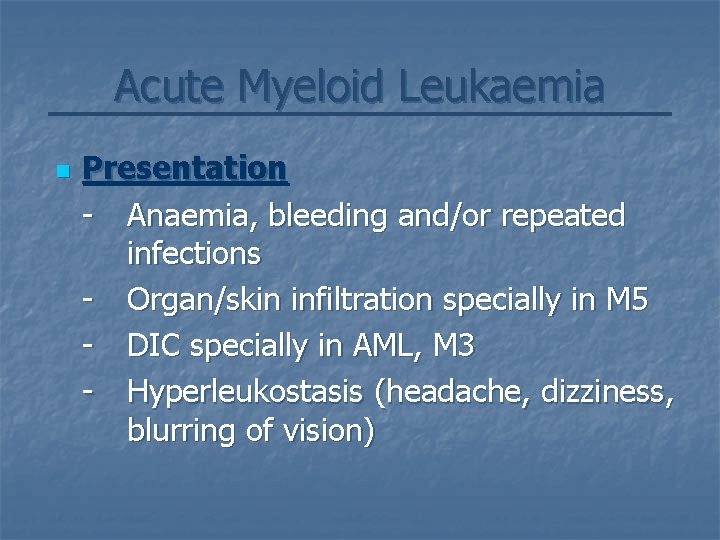
Acute Myeloid Leukaemia n Presentation - Anaemia, bleeding and/or repeated infections - Organ/skin infiltration specially in M 5 - DIC specially in AML, M 3 - Hyperleukostasis (headache, dizziness, blurring of vision)
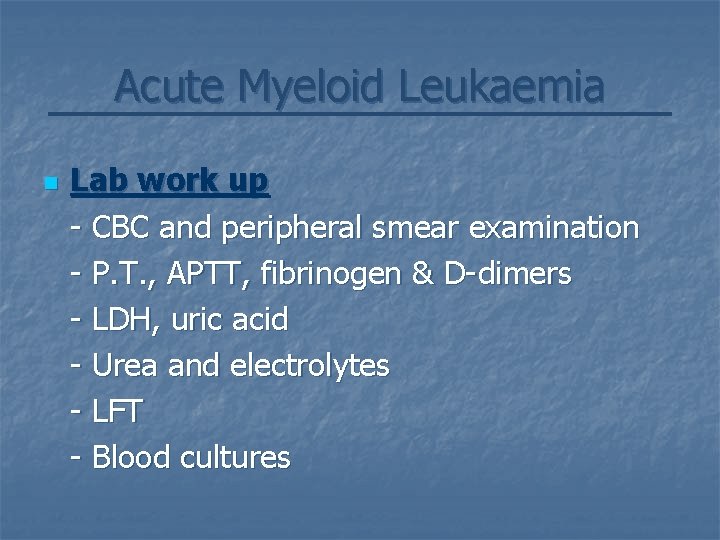
Acute Myeloid Leukaemia n Lab work up - CBC and peripheral smear examination - P. T. , APTT, fibrinogen & D-dimers - LDH, uric acid - Urea and electrolytes - LFT - Blood cultures
Acute Myeloid Leukaemia Lab work up Bone marrow aspiration and trephine biopsy for: - Morphology - Cytochemical stains - Immunophenotyping - Cytogenetic analysis n
Acute Myeloid Leukaemia n Other investigations - Chest X-ray - ECG - MGA scan (cardiac toxicity of anthracycline chemotherapeutics)
Acute Myeloid Leukaemia n. Prognostic criteria Cytogenetic abnormalities are the single most important prognostic factors in AML. - Good prognostic abnormalities: M 3 t(15, 17) M 2 t(8, 21) M 3 inv(16) - Poor prognostic abnormalities Monosomy 7 Monosomy 5
Acute Myeloid Leukaemia Management n n Induction and consolidation - Combination of Anthracycline & Ara-C - A total of 3 to 5 courses Late intensification - High dose Ara-C in young good risk group - Matched All-BMT in fit, bad risk fit - Mini-allo BMT or autologus BMT in older patients
Acute Myeloid Leukaemia n Management - About 50% of patients achieve CR after first course - Another 10% enter remission after 2 nd course
Acute Promyelocytic Leukaemia n Clinical presentation - Younger age on presentation as compared to other AML subtypes - Often patients have low counts on presentation - Bone marrow has >30% promyelocytes - It is commonly associated with DIC which is the main reason for early deaths - Aggressive replacement with platelets and cryoprecipitate is the mainstay of early management

Acute Promyelocytic Leukaemia n n n T(15, 17) is a good prognostic indicator and is present in 95% of cases This translocation involves the retinoic acid receptor gene rendering the tumor cells susceptible to all-trans retinoic acid (ATRA) CR achieved in >90% of cases with ATRA and chemotherapy
 Aspiration biopsy
Aspiration biopsy Mrcpath
Mrcpath Mrcpath
Mrcpath Myeloid tissue is a type of
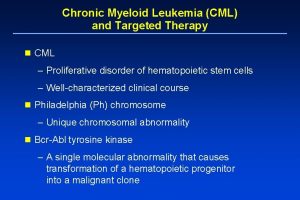
Myeloid tissue is a type of Chronic myeloid leukemia
Chronic myeloid leukemia Myelopoiesis
Myelopoiesis Mark juckett md
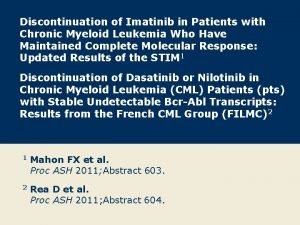
Mark juckett md Chronic myeloid leukemia treatment
Chronic myeloid leukemia treatment Chronic myeloid leukemia
Chronic myeloid leukemia Adam white speaks
Adam white speaks Where to listen for apical pulse
Where to listen for apical pulse Describe the care team and the chain of command
Describe the care team and the chain of command Lingual pit
Lingual pit Hacheur réversible en courant
Hacheur réversible en courant Personal writing assistant
Personal writing assistant