1 NATIONAL PHARMACEUTICAL UNIVERSITY Department of Pharmacology MEDICINES

- Slides: 33
1 NATIONAL PHARMACEUTICAL UNIVERSITY Department of Pharmacology MEDICINES AFFECTING EFFERENT INNERVATION 1
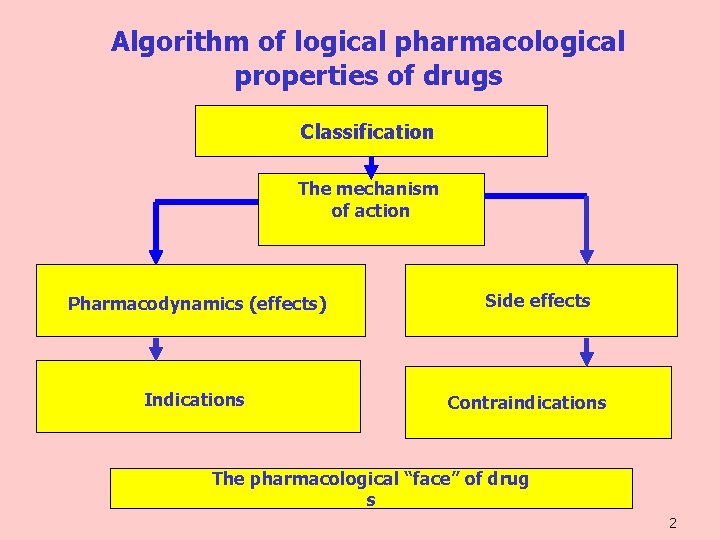
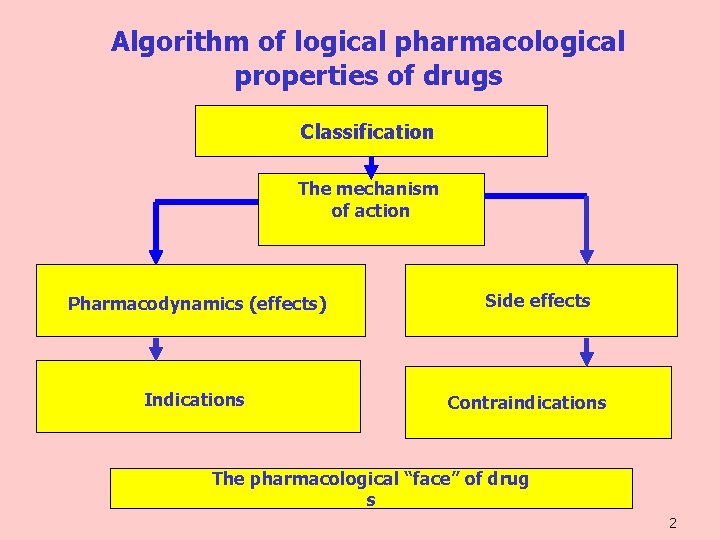
Algorithm of logical pharmacological properties of drugs Classification The mechanism of action Pharmacodynamics (effects) Indications Side effects Contraindications The pharmacological “face” of drug s 2
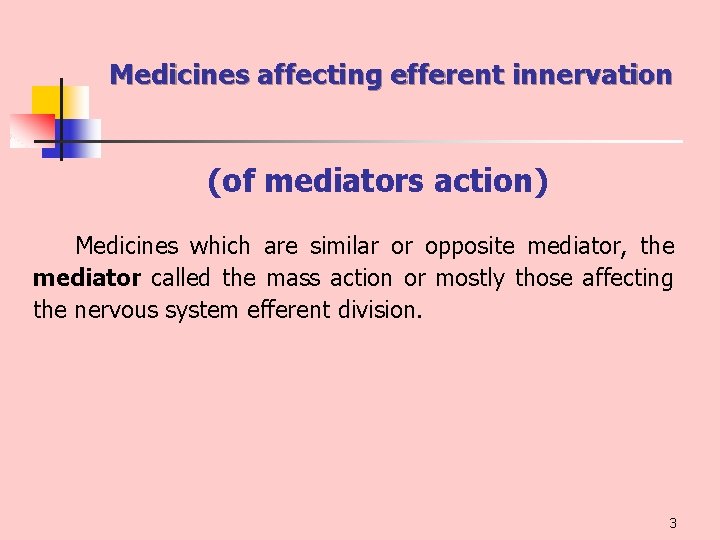
Medicines affecting efferent innervation (of mediators action) Medicines which are similar or opposite mediator, the mediator called the mass action or mostly those affecting the nervous system efferent division. 3
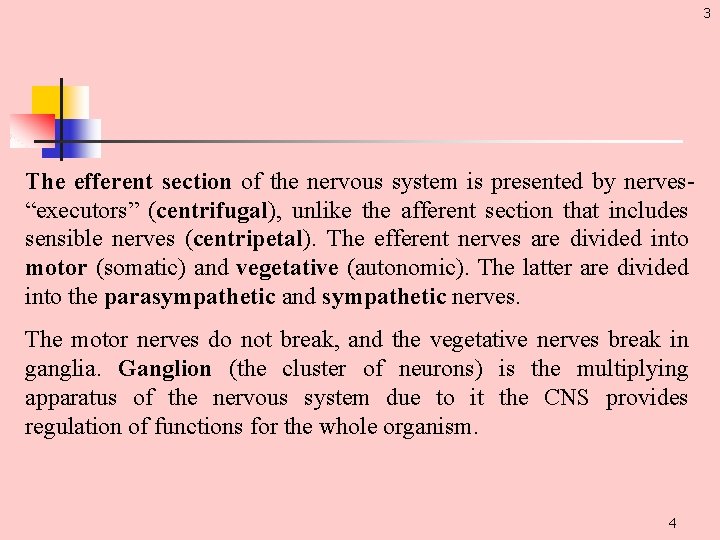
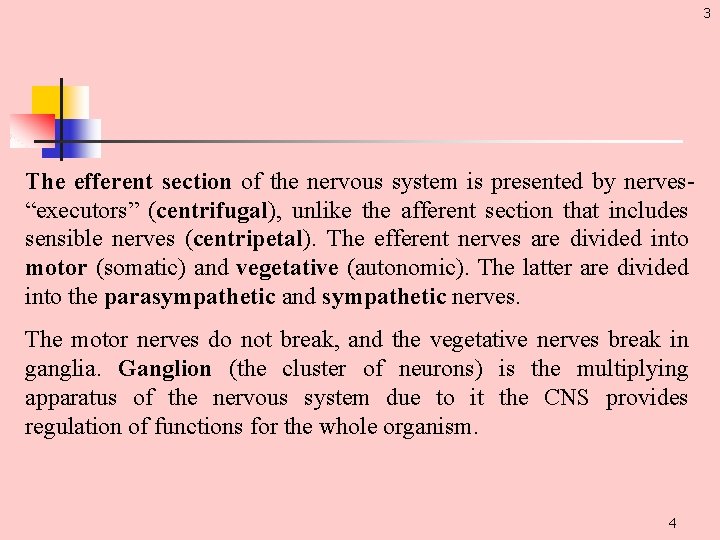
3 The efferent section of the nervous system is presented by nerves “executors” (centrifugal), unlike the afferent section that includes sensible nerves (centripetal). The efferent nerves are divided into motor (somatic) and vegetative (autonomic). The latter are divided into the parasympathetic and sympathetic nerves. The motor nerves do not break, and the vegetative nerves break in ganglia. Ganglion (the cluster of neurons) is the multiplying apparatus of the nervous system due to it the CNS provides regulation of functions for the whole organism. 4
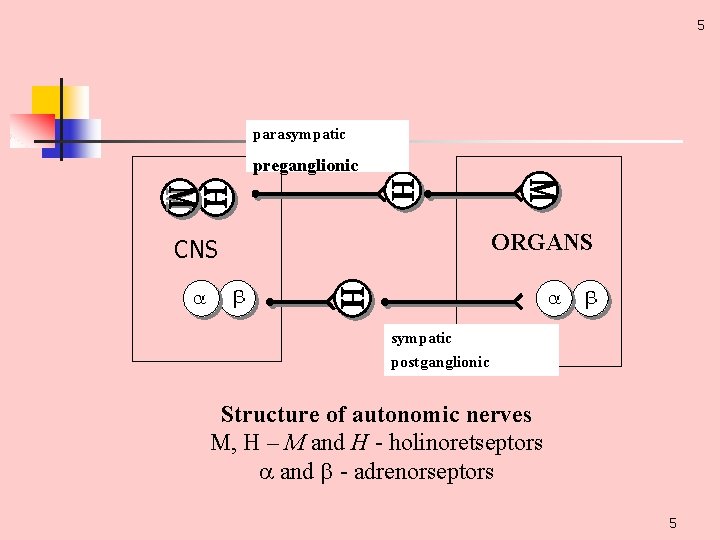
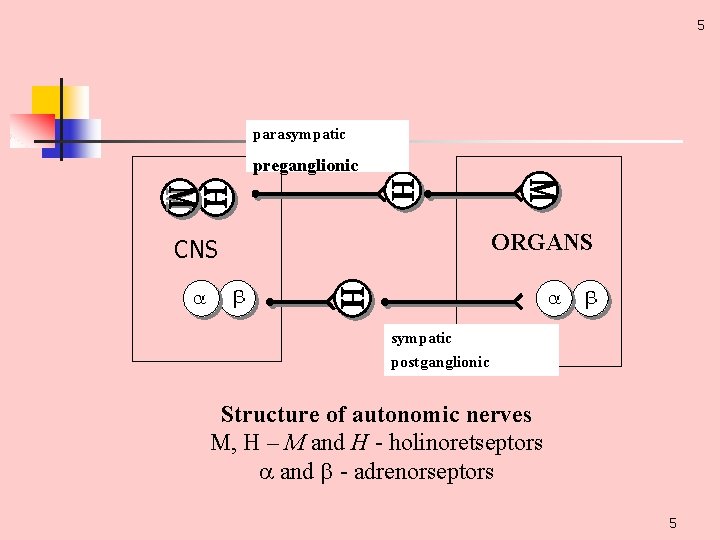
5 parasympatic preganglionic ORGANS CNS sympatic postganglionic Structure of autonomic nerves М, Н – М and Н holinoretseptors and adrenorseptors 5
6 As these medicines change the rate of the nervous impulse conductivity in synapse, they are also called synaptic acting medicines. Synapse is the place of action for the drugs primary influencing on the peripheral processes of neurotransmission (the efferent section of the nervous system). 6
11 Classification of medicines affecting efferent innervation I. Cholinergic – the action is similar to acetylcholine functions. II. Anticholinergic – the action is opposite to acetylcholine functions , medicines block Ch. R and make them insensitive to a neurotransmitter. III. Adrenergic – their action is similar to NA and A functions. IV. Anti-adrenergic – opposite to adrenergic agents. Comparing the classification and the effects of these medicines it can be conditionally considered that when using of cholinergic medicines the effects connected with the stimulation of parasympathetic nerves dominate in the organism, while with adrenergic medicines sympathetic nerves are stimulated 7
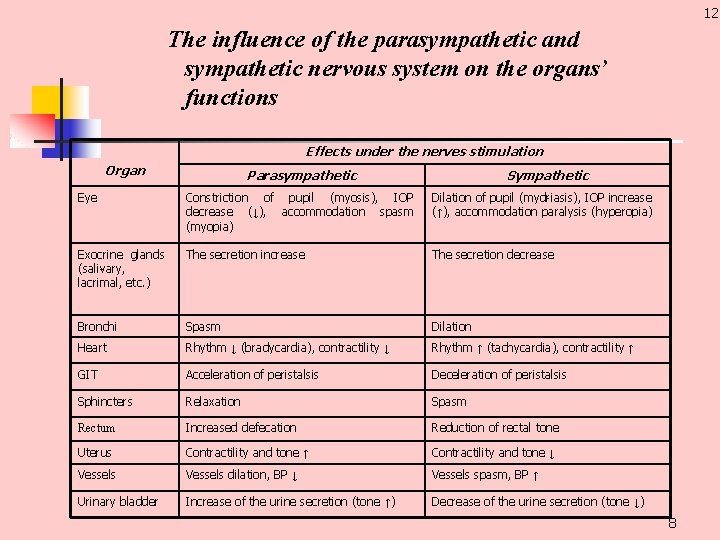
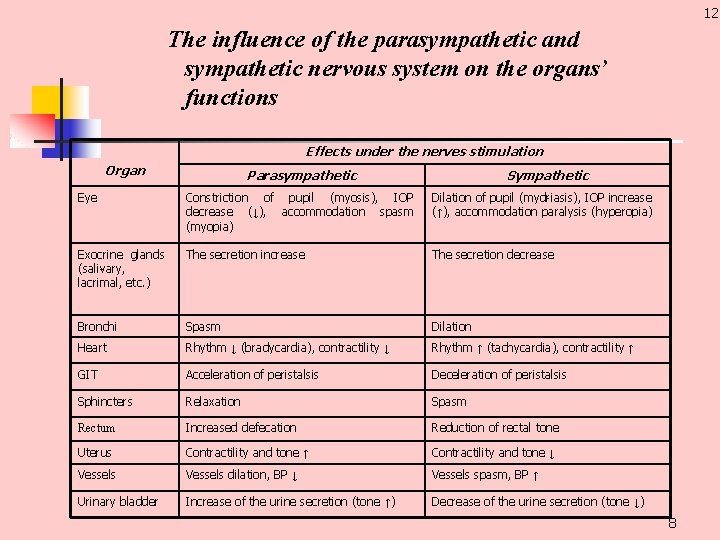
12 The influence of the parasympathetic and sympathetic nervous system on the organs’ functions Effects under the nerves stimulation Organ Parasympathetic Sympathetic Eye Constriction of pupil (myosis), IOP decrease (↓), accommodation spasm (myopia) Dilation of pupil (myd riasis), IOP increase (↑), accommodation paralysis (hyperopia) Exocrine glands (sali vary, lacrimal, etc. ) The secretion increase The secretion decrease Bronchi Spasm Dilation Heart Rhythm ↓ (bradycardia), contractility ↓ Rhythm ↑ (tachycardia), contractility ↑ GIT Acceleration of peristalsis Deceleration of peristalsis Sphincters Relaxation Spasm Rectum Increased defecation Reduction of rectal tone Uterus Contractility and tone ↑ Contractility and tone ↓ Vessels dilation, BP ↓ Vessels spasm, BP ↑ Urinary bladder Increase of the urine secretion (tone ↑) Decrease of the urine secretion (tone ↓) 8
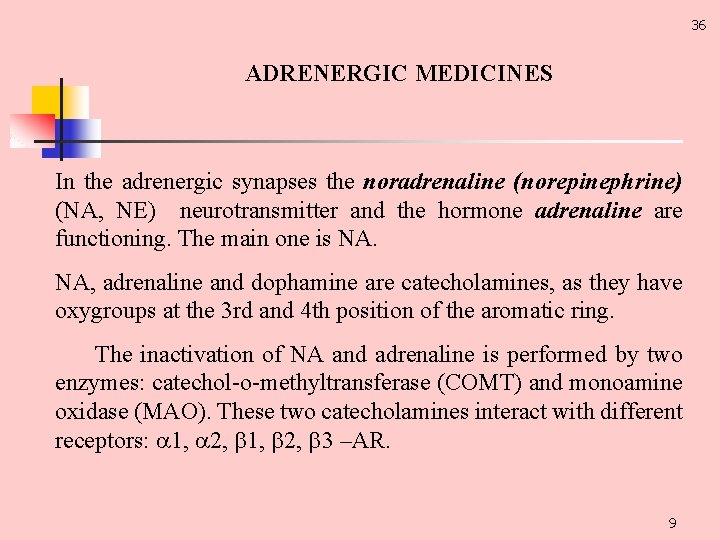
36 ADRENERGIC MEDICINES In the adrenergic synapses the noradrenaline (norepinephrine) (NA, NE) neurotransmitter and the hormone adrenaline are functioning. The main one is NA. NA, adrenaline and dophamine are catecholamines, as they have oxygroups at the 3 rd and 4 th position of the aromatic ring. The inactivation of NA and adrenaline is performed by two enzymes: catechol o methyltransferase (COMT) and monoamine oxidase (MAO). These two catecholamines interact with different receptors: 1, 2, 3 –AR. 9
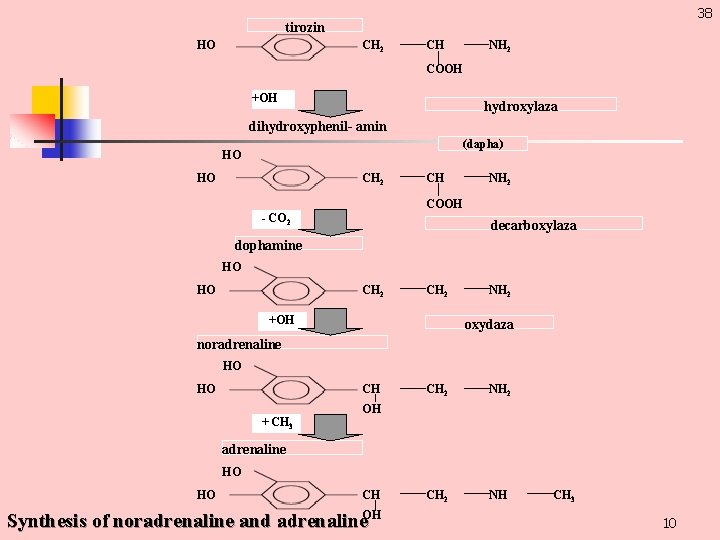
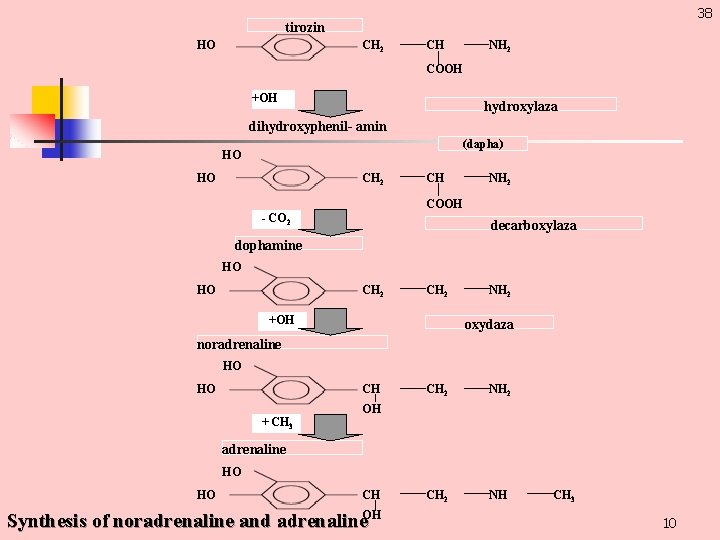
38 tirozin НО СН 2 СН NН 2 СOOН +OН hydroxylaza dihydroxyphenil- amin (dapha) НО НО СН 2 СН NН 2 СOOН - СO 2 decarboxylaza dophamine НО НО СН 2 +OН NН 2 oxydaza noradrenaline НО НО СН + СН 3 СН 2 NН 2 СН 2 NН ОН adrenaline НО НО СН Synthesis of noradrenaline and adrenaline. ОН СН 3 10
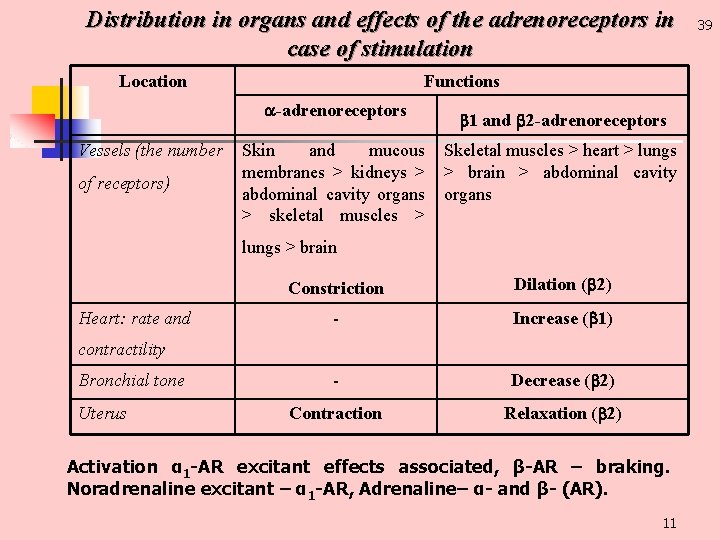
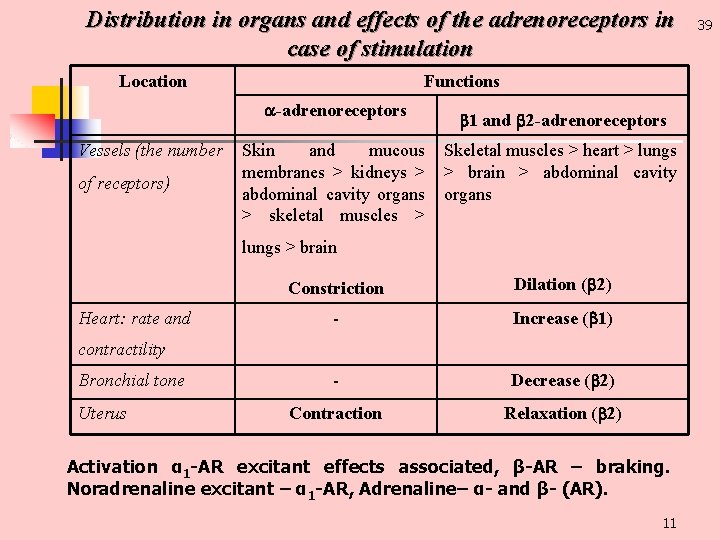
Distribution in organs and effects of the adrenoreceptors in case of stimulation Location Functions -adrenoreceptors Vessels (the number of receptors) Skin and mucous membranes > kidneys > abdominal cavity organs > skeletal muscles > 1 and 2 -adrenoreceptors Skeletal muscles > heart > lungs > brain > abdominal cavity organs lungs > brain Heart: rate and Constriction Dilation ( 2) Increase ( 1) Decrease ( 2) Contraction Relaxation ( 2) contractility Bronchial tone Uterus Activation α 1 -АR excitant effects associated, β-АR – braking. Noradrenaline excitant – α 1 -АR, Adrenaline– α- and β- (АR). 11 39
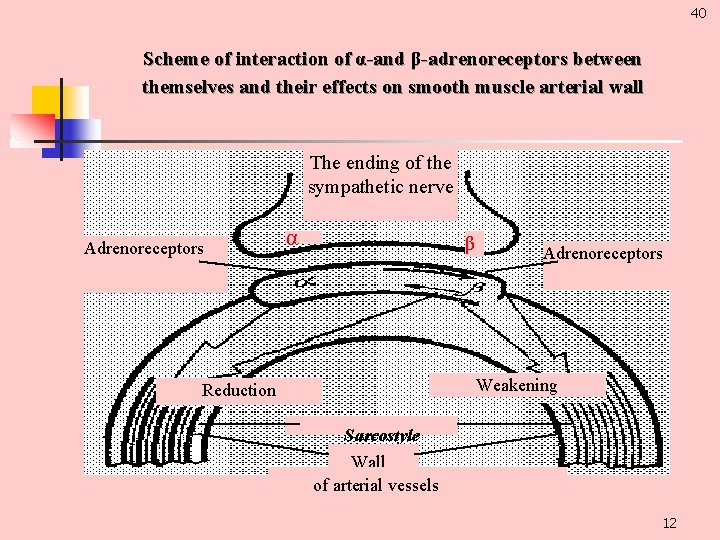
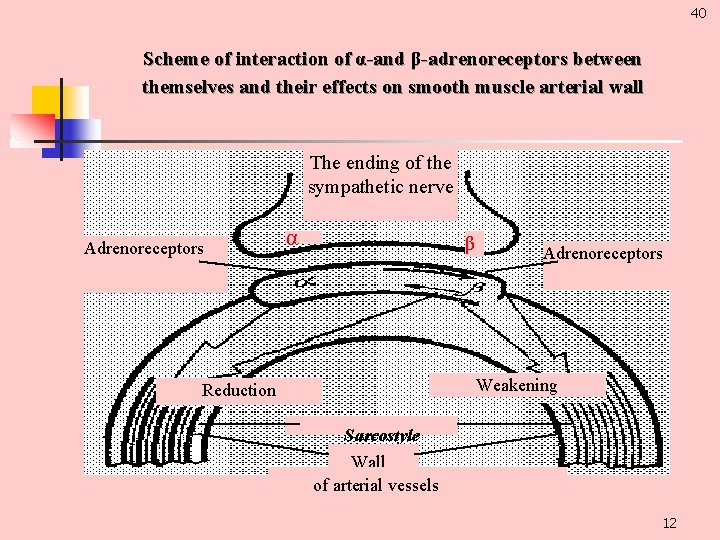
40 Scheme of interaction of α-and β-adrenoreceptors between themselves and their effects on smooth muscle arterial wall The ending of the sympathetic nerve Adrenoreceptors α β Adrenoreceptors Weakening Reduction Sarcostyle Wall of arterial vessels 12
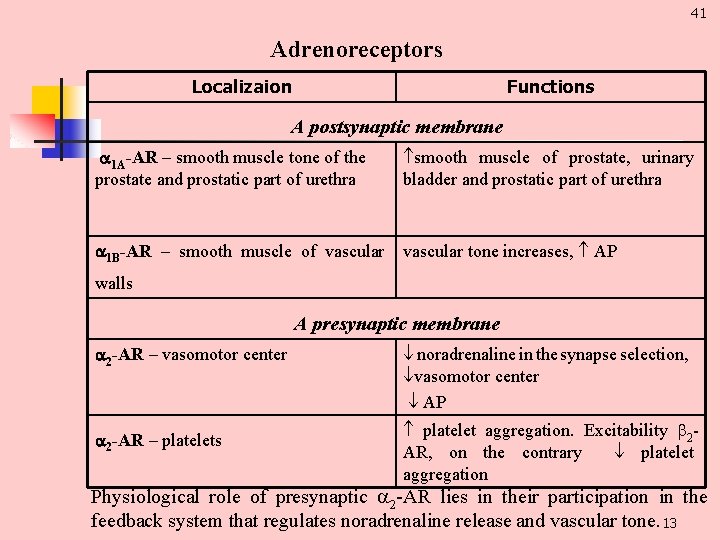
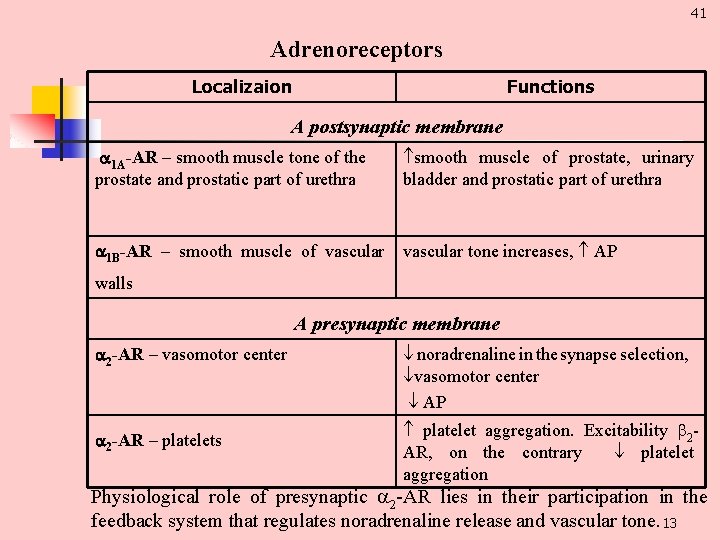
41 Adrenoreceptors Localizaion Functions A postsynaptic membrane 1 А-АR – smooth muscle tone of the prostate and prostatic part of urethra smooth muscle of prostate, urinary bladder and prostatic part of urethra 1 В-АR – smooth muscle of vascular tone increases, AP walls A presynaptic membrane 2 -АR – vasomotor center 2 -АR – platelets noradrenaline in the synapse selection, vasomotor center AP platelet aggregation. Excitability 2 АR, on the contrary platelet aggregation Physiological role of presynaptic 2 AR lies in their participation in the feedback system that regulates noradrenaline release and vascular tone. 13
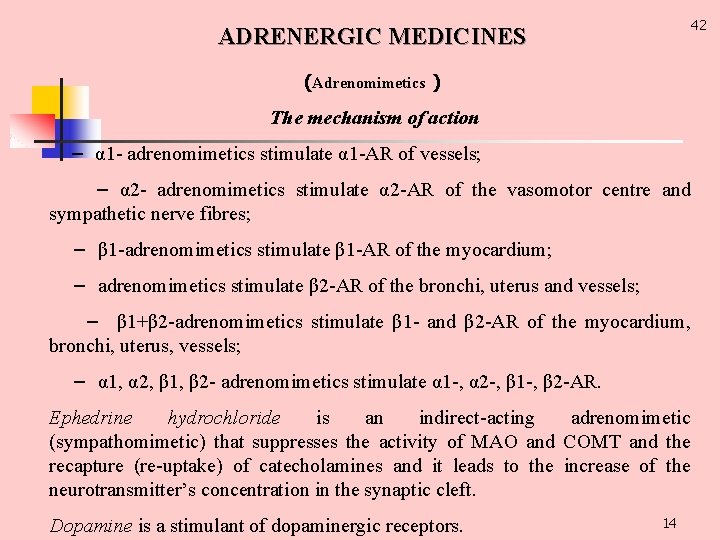
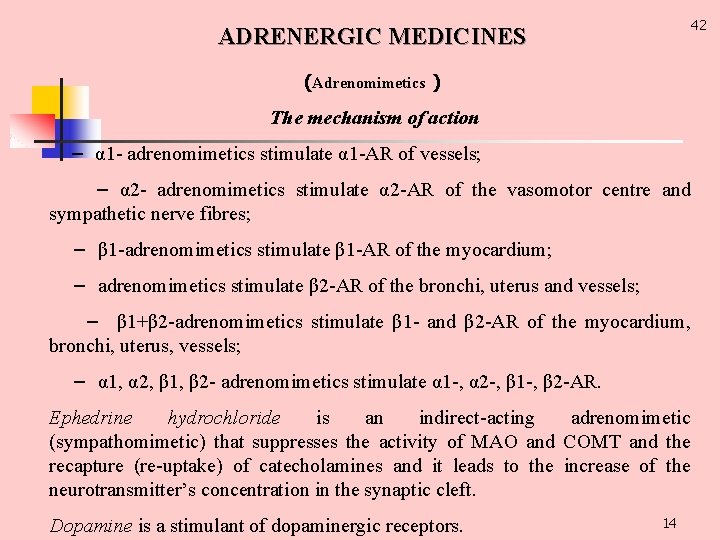
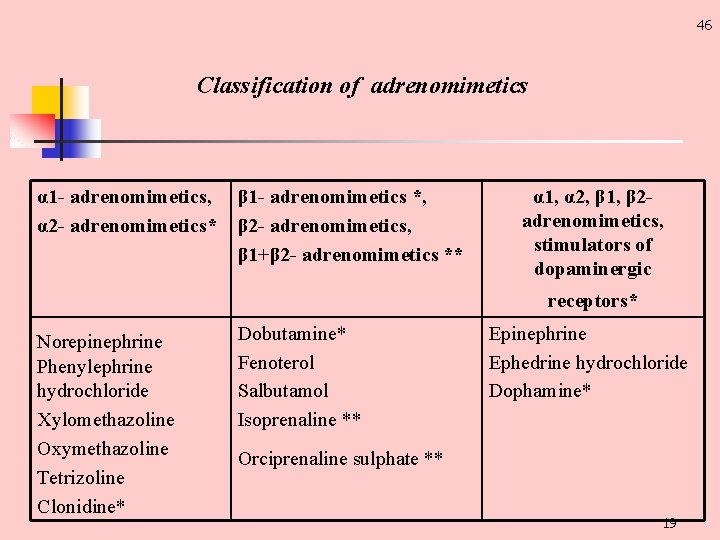
42 ADRENERGIC MEDICINES (Adrenomimetics ) The mechanism of action – α 1 adrenomimetics stimulate α 1 AR of vessels; – α 2 adrenomimetics stimulate α 2 AR of the vasomotor centre and sympathetic nerve fibres; – β 1 adrenomimetics stimulate β 1 AR of the myocardium; – adrenomimetics stimulate β 2 AR of the bronchi, uterus and vessels; – β 1+β 2 adrenomimetics stimulate β 1 and β 2 AR of the myocardium, bronchi, uterus, vessels; – α 1, α 2, β 1, β 2 adrenomimetics stimulate α 1 , α 2 , β 1 , β 2 AR. Ephedrine hydrochloride is an indirect acting adrenomimetic (sympathomimetic) that suppresses the activity of MAO and COMT and the recapture (re uptake) of catecholamines and it leads to the increase of the neurotransmitter’s concentration in the synaptic cleft. Dopamine is a stimulant of dopaminergic receptors. 14
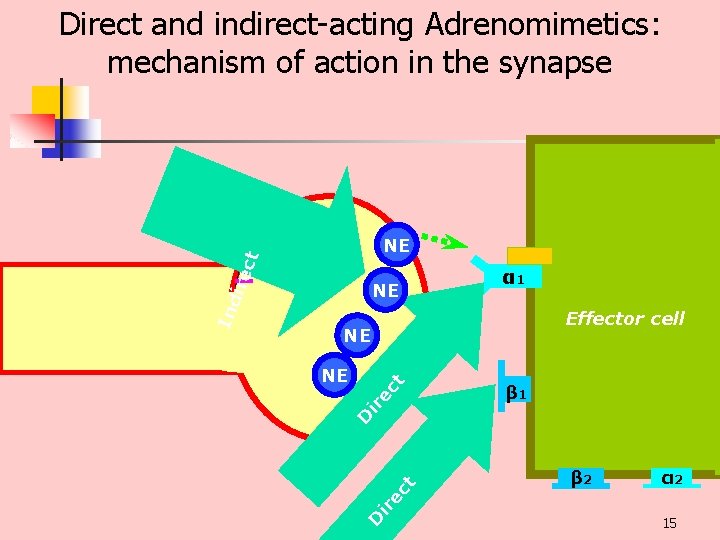
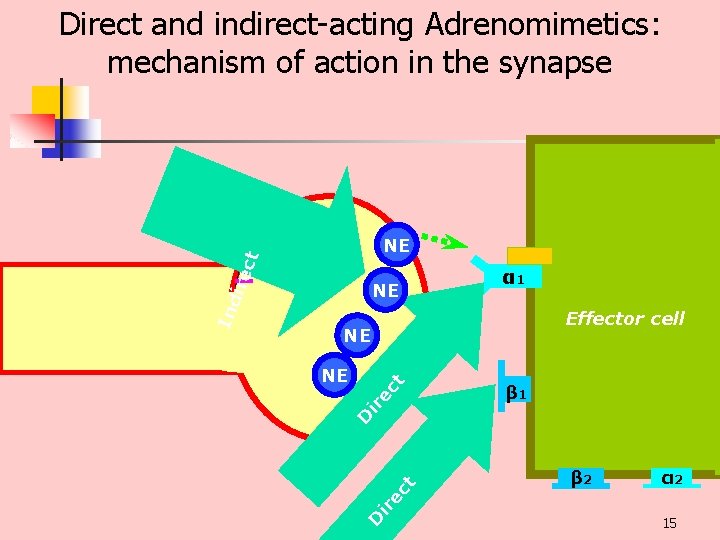
Direct and indirect acting Adrenomimetics: mechanism of action in the synapse NE α 1 Effector cell NE β 1 β 2 α 2 ir ec t D ir ec t NE D Ind ire ct NE 15
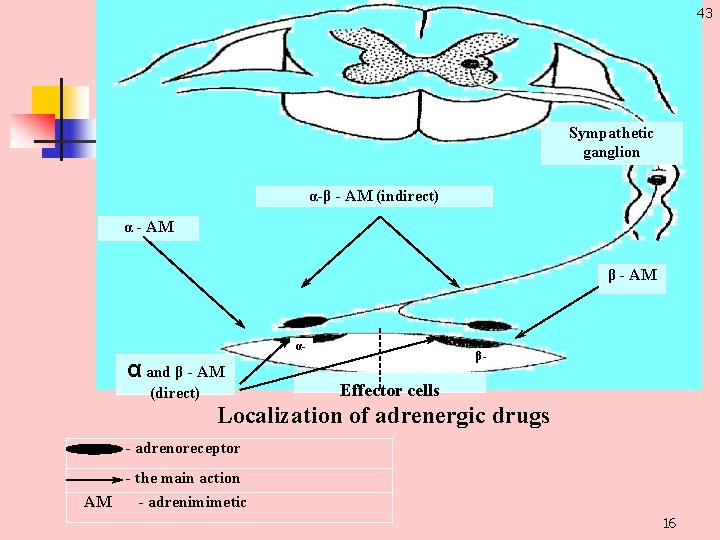
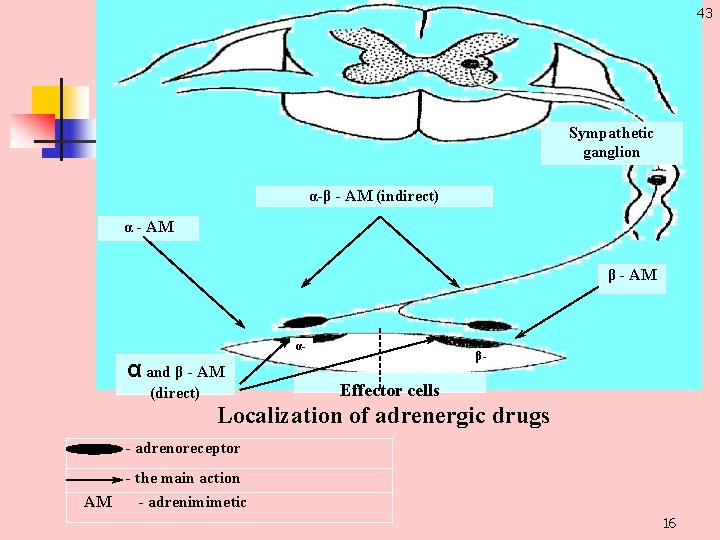
43 Sympathetic ganglion α-β - АМ (indirect) α - АМ β - АМ α- α and β - АМ (direct) β- Effector cells Localization of adrenergic drugs - adrenoreceptor - the main action АМ - adrenimimetic 16
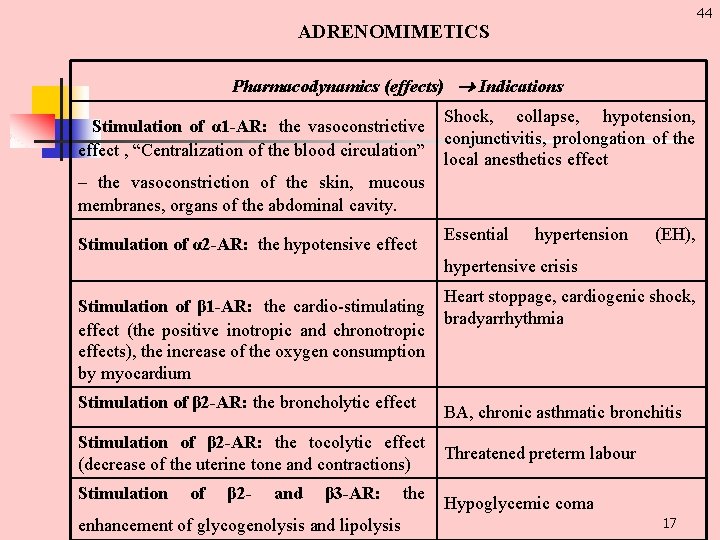
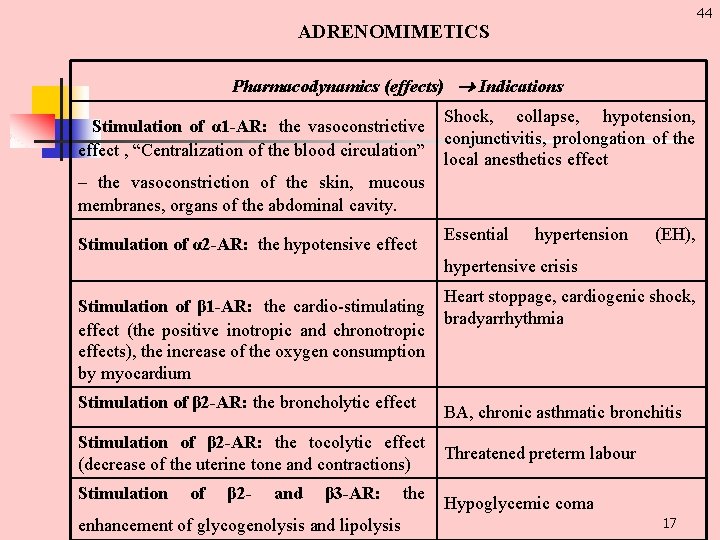
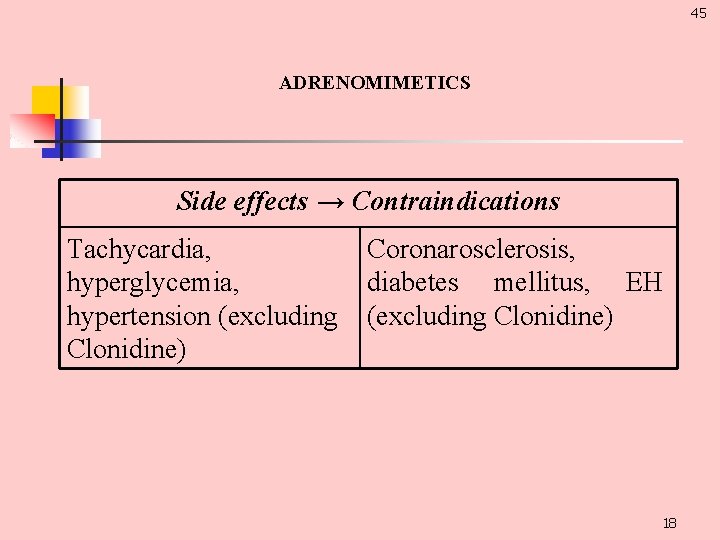
44 ADRENOMIMETICS Pharmacodynamics (effects) Indications Stimulation of α 1 -AR: the vasoconstrictive effect , “Centralization of the blood circulation” Shock, collapse, hypotension, conjunctivitis, prolongation of the local anesthetics effect – the vasoconstriction of the skin, mucous membranes, organs of the abdominal cavity. Stimulation of α 2 -AR: the hypotensive effect Essential hypertension (EH), hypertensive crisis Stimulation of β 1 -AR: the cardio stimulating effect (the positive inotropic and chronotropic effects), the increase of the oxygen consumption by myocardium Stimulation of β 2 -AR: the broncholytic effect Stimulation of β 2 -AR: the tocolytic effect (decrease of the uterine tone and contractions) Stimulation of β 2 - and β 3 -AR: enhancement of glycogenolysis and lipolysis the Heart stoppage, cardiogenic shock, bradyarrhythmia BA, chronic asthmatic bronchitis Threatened preterm labour Hypoglycemic coma 17
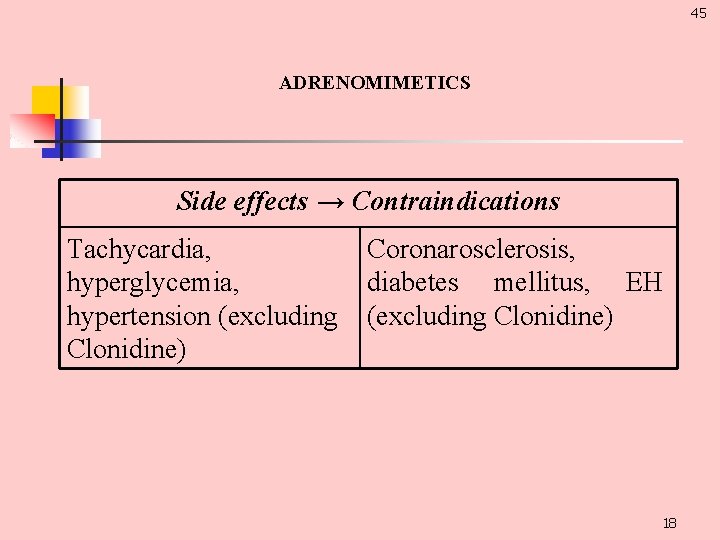
45 ADRENOMIMETICS Side effects → Contraindications Tachycardia, hyperglycemia, hypertension (excluding Clonidine) Coronarosclerosis, diabetes mellitus, EH (excluding Clonidine) 18
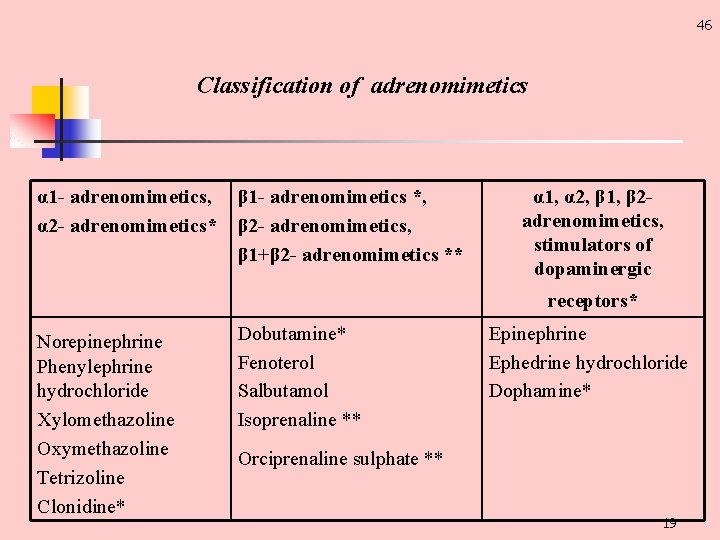
46 Classification of adrenomimetics α 1 - adrenomimetics, α 2 - adrenomimetics* β 1 - adrenomimetics *, β 2 - adrenomimetics, β 1+β 2 - adrenomimetics ** α 1, α 2, β 1, β 2 adrenomimetics, stimulators of dopaminergic receptors* Norepinephrine Phenylephrine hydrochloride Xylomethazoline Oxymethazoline Tetrizoline Clonidine* Dobutamine* Fenoterol Salbutamol Isoprenaline ** Epinephrine Ephedrine hydrochloride Dophamine* Orciprenaline sulphate ** 19
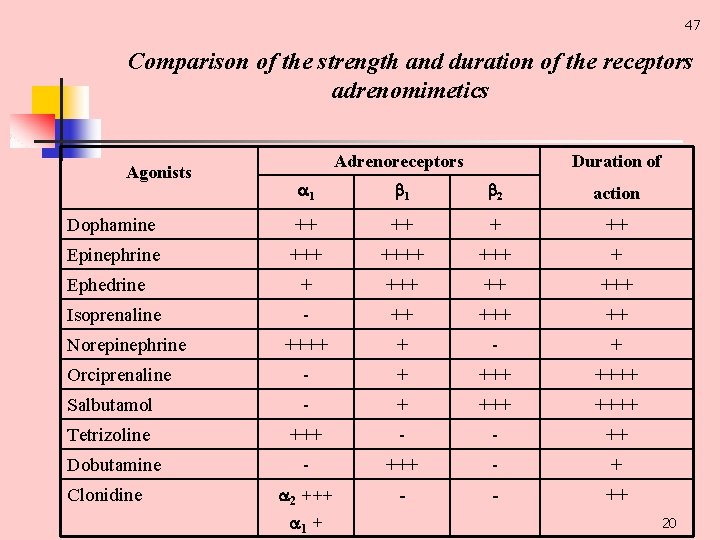
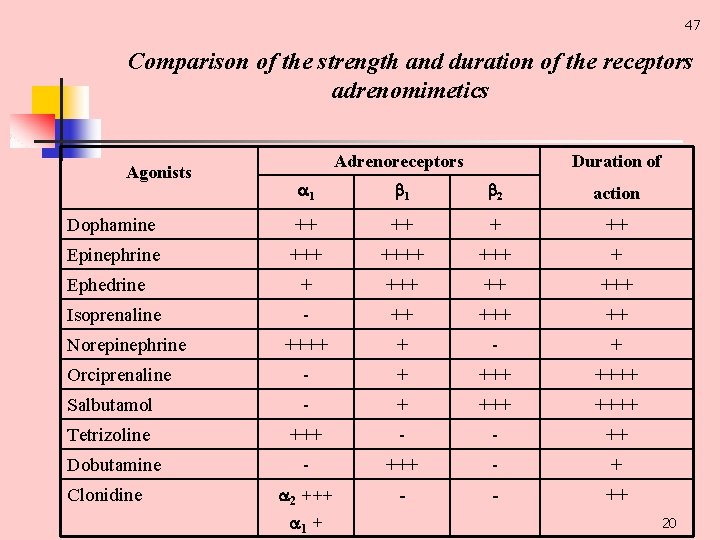
47 Comparison of the strength and duration of the receptors adrenomimetics Agonists Adrenoreceptors Duration of 1 1 2 action Dophamine ++ ++ Epinephrine ++++ +++ + Ephedrine + ++ +++ Isoprenaline ++ ++++ + + Orciprenaline + ++++ Salbutamol + ++++ Tetrizoline +++ ++ Dobutamine +++ + 2 +++ ++ Norepinephrine Clonidine 1 + 20
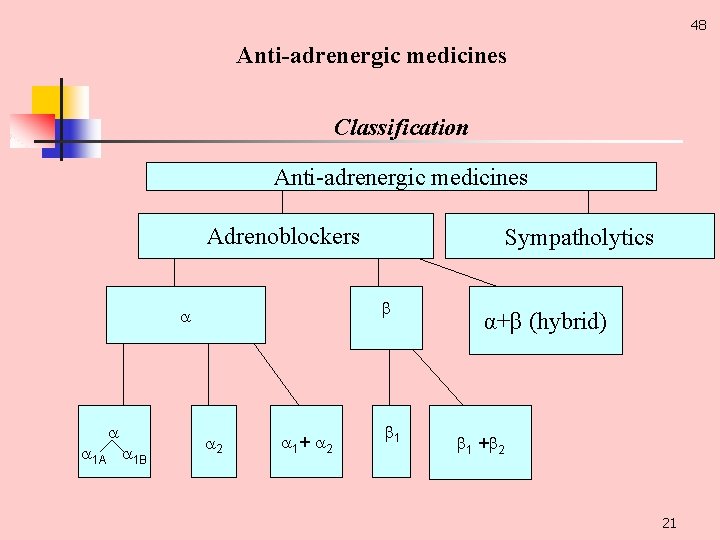
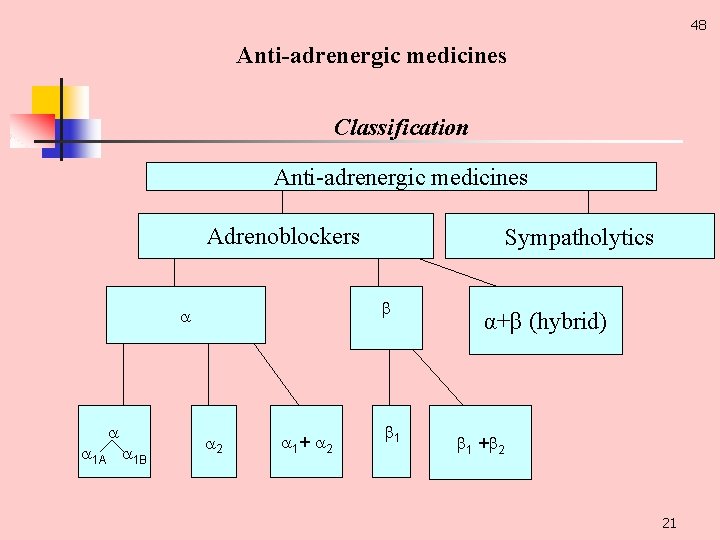
48 Anti-adrenergic medicines Classification Anti adrenergic medicines Adrenoblockers 1 А 1 В Sympatholytics 2 1+ 2 1 α+β (hybrid) 1 + 2 21
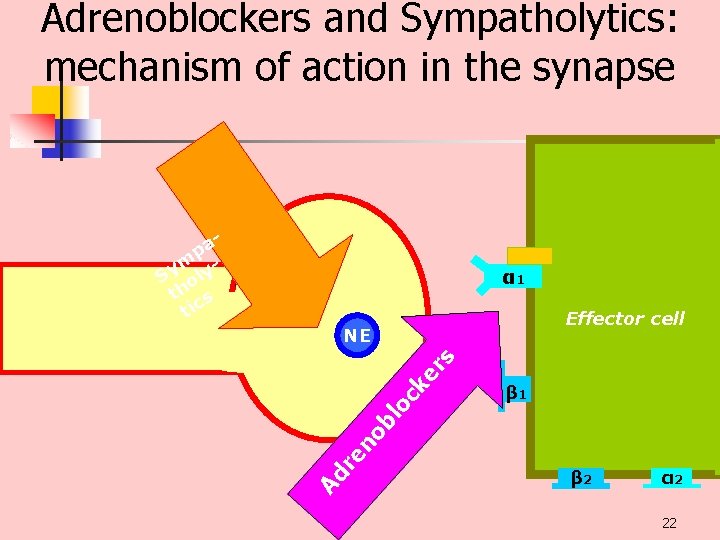
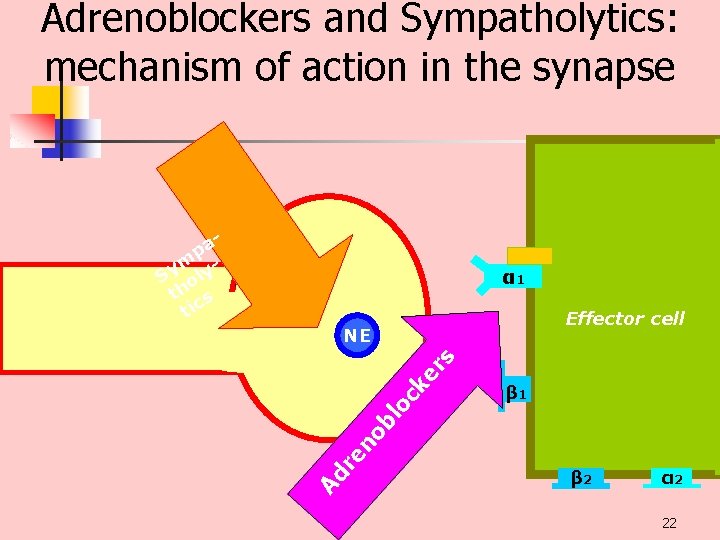
Adrenoblockers and Sympatholytics: mechanism of action in the synapse pa m Sy oly th s tic α 1 Effector cell β 1 Ad re no bl oc ke rs NE β 2 α 2 22
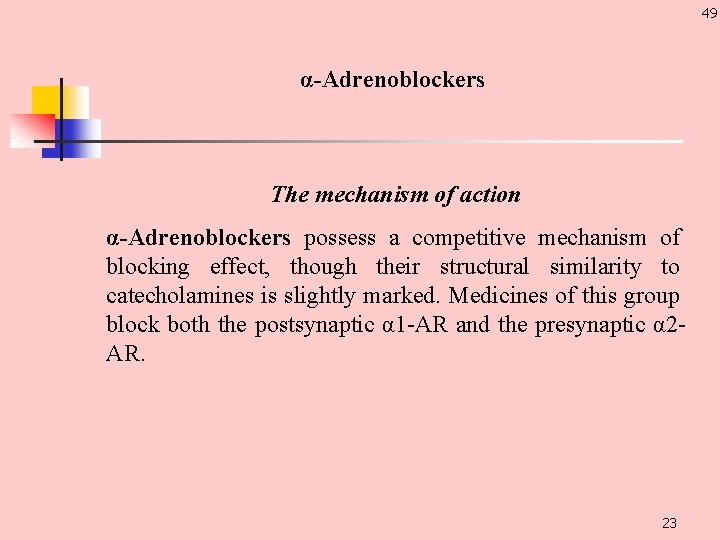
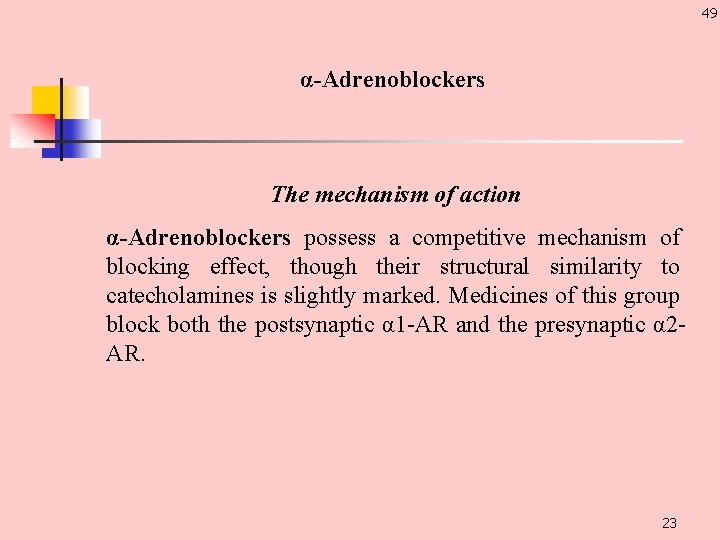
49 α-Adrenoblockers The mechanism of action α-Adrenoblockers possess a competitive mechanism of blocking effect, though their structural similarity to catecholamines is slightly marked. Medicines of this group block both the postsynaptic α 1 AR and the presynaptic α 2 AR. 23
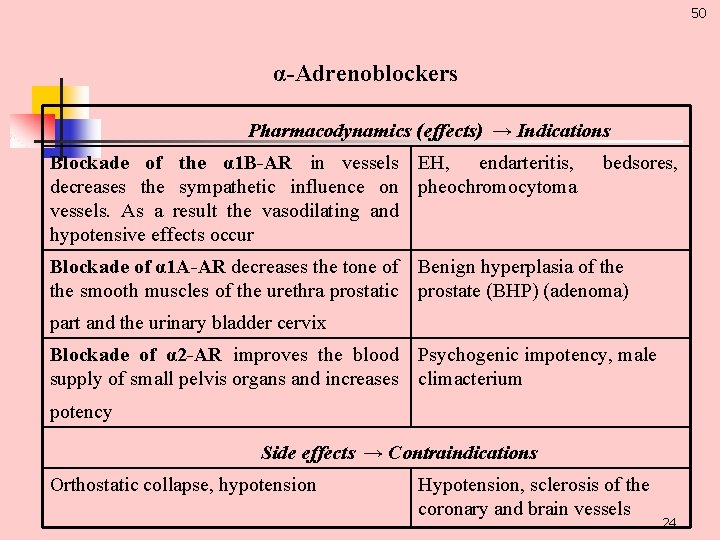
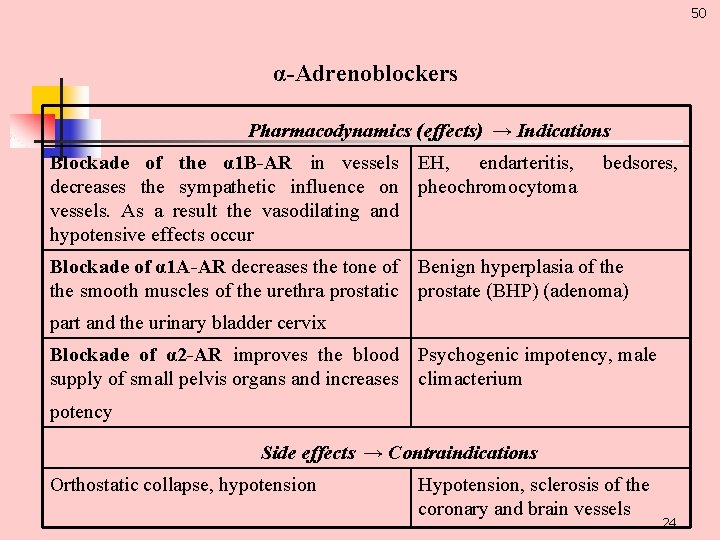
50 α-Adrenoblockers Pharmacodynamics (effects) → Indications Blockade of the α 1 B-AR in vessels EH, endarteritis, decreases the sympathetic influence on pheochromocytoma vessels. As a result the vasodilating and hypotensive effects occur bedsores, Blockade of α 1 A-AR decreases the tone of Benign hyperplasia of the smooth muscles of the urethra prostatic prostate (BHP) (adenoma) part and the urinary bladder cervix Blockade of α 2 -AR improves the blood Psychogenic impotency, male supply of small pelvis organs and increases climacterium potency Side effects → Contraindications Orthostatic collapse, hypotension Hypotension, sclerosis of the coronary and brain vessels 24
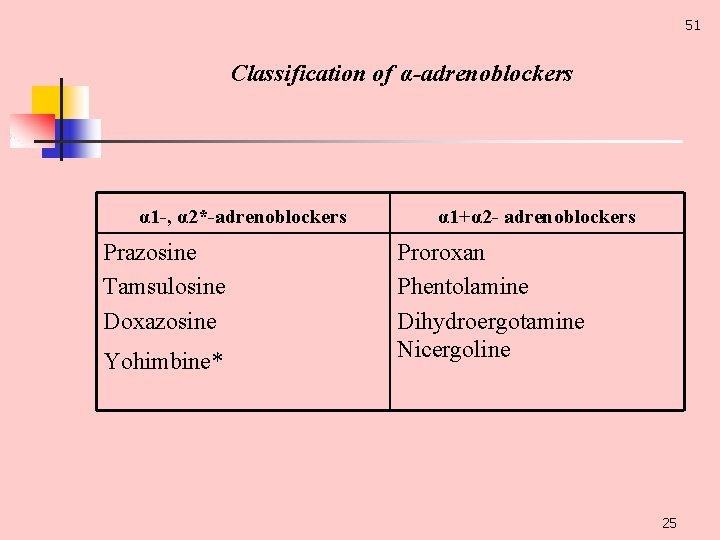
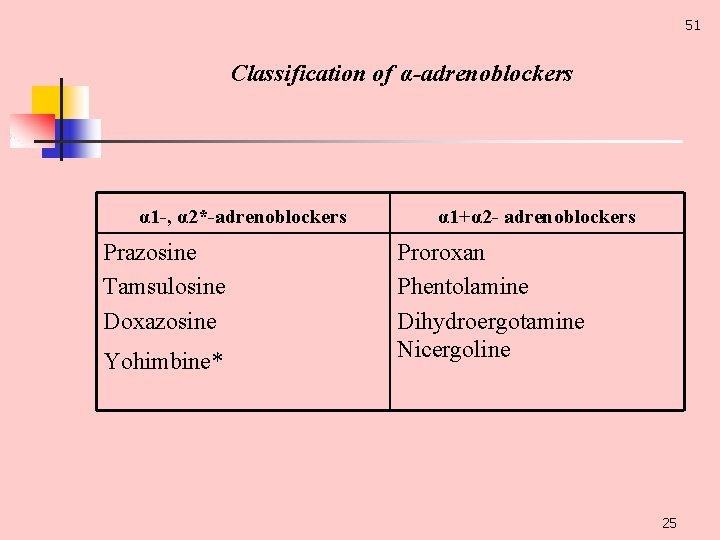
51 Classification of α-adrenoblockers α 1 -, α 2*-adrenoblockers Prazosine Tamsulosine Doxazosine Yohimbine* α 1+α 2 - adrenoblockers Proroxan Phentolamine Dihydroergotamine Nicergoline 25
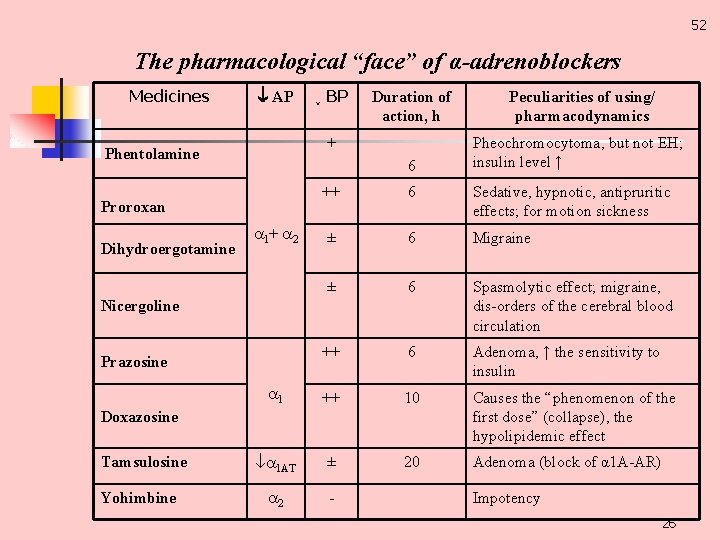
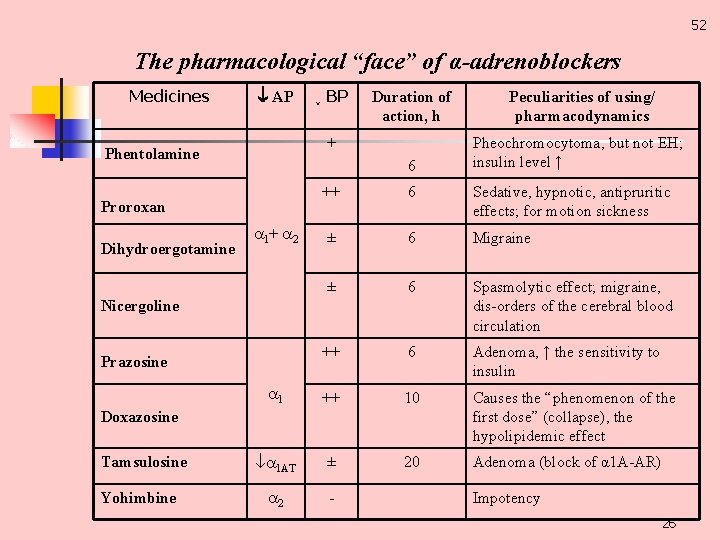
52 The pharmacological “face” of α-adrenoblockers Medicines АР Duration of action, h Peculiarities of using/ pharmacodynamics 6 Pheochromocytoma, but not EH; insulin level ↑ + Phentolamine ++ 6 Sedative, hypnotic, antipruritic effects; for motion sickness ± 6 Migraine ± 6 Spasmolytic effect; migraine, dis orders of the cerebral blood circulation ++ 6 Adenoma, ↑ the sensitivity to insulin 1 ++ 10 Causes the “phenomenon of the first dose” (collapse), the hypolipidemic effect 1 АТ ± 20 Adenoma (block of α 1 A AR) 2 Proroxan Dihydroergotamine ↓ BP 1+ 2 Nicergoline Prazosine Doxazosine Tamsulosine Yohimbine Impotency 26
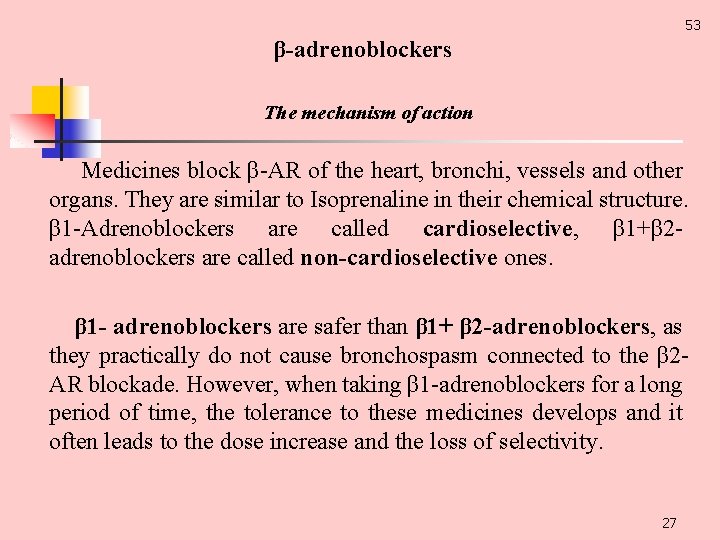
53 β-adrenoblockers The mechanism of action Medicines block β AR of the heart, bronchi, vessels and other organs. They are similar to Isoprenaline in their chemical structure. β 1 Adrenoblockers are called cardioselective, β 1+β 2 adrenoblockers are called non-cardioselective ones. β 1 - adrenoblockers are safer than β 1+ β 2 -adrenoblockers, as they practically do not cause bronchospasm connected to the β 2 AR blockade. However, when taking β 1 adrenoblockers for a long period of time, the tolerance to these medicines develops and it often leads to the dose increase and the loss of selectivity. 27
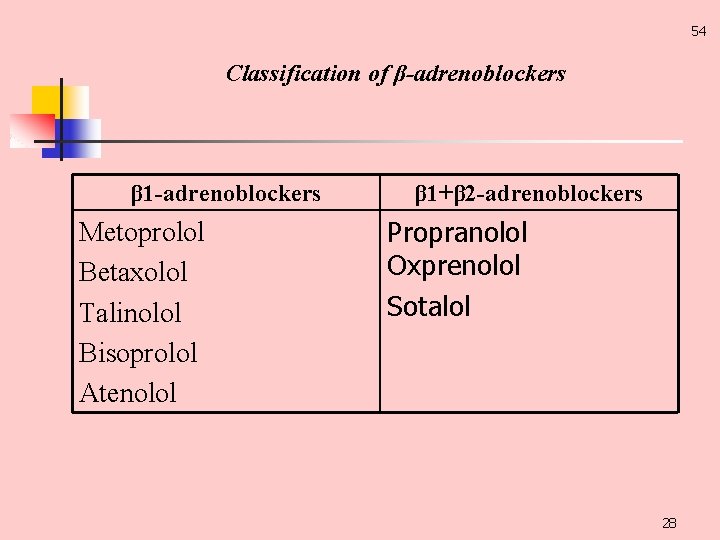
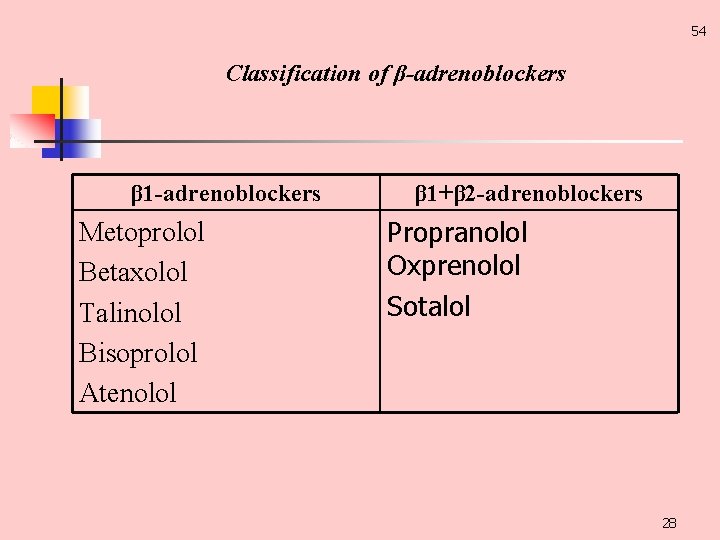
54 Classification of β-adrenoblockers β 1 -adrenoblockers Metoprolol Betaxolol Talinolol Bisoprolol Atenolol β 1+β 2 -adrenoblockers Propranolol Oxprenolol Sotalol 28
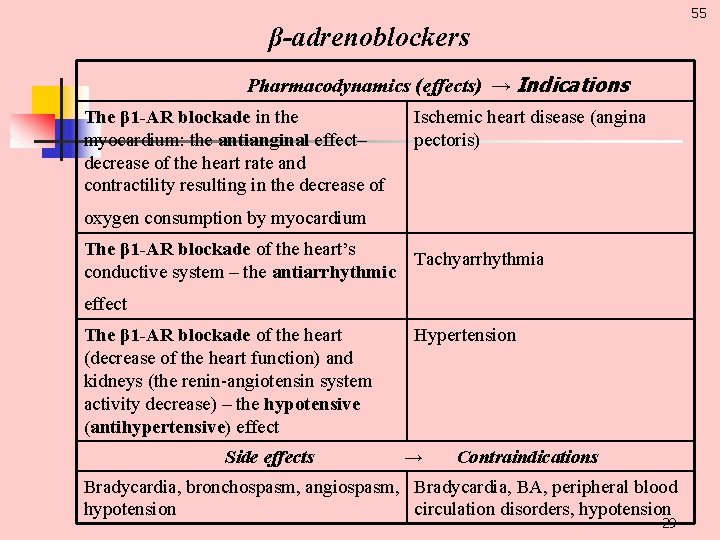
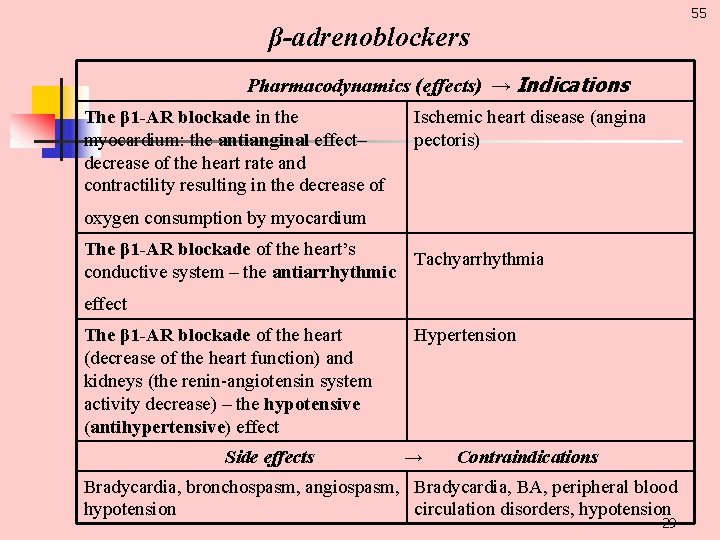
55 β-adrenoblockers Pharmacodynamics (effects) → Indications The β 1 -AR blockade in the myocardium: the antianginal effect– decrease of the heart rate and contractility resulting in the decrease of Ischemic heart disease (angina pectoris) oxygen consumption by myocardium The β 1 -AR blockade of the heart’s Tachyarrhythmia conductive system – the antiarrhythmic effect The β 1 -AR blockade of the heart (decrease of the heart function) and kidneys (the renin angiotensin system activity decrease) – the hypotensive (antihypertensive) effect Side effects Hypertension → Contraindications Bradycardia, bronchospasm, angiospasm, Bradycardia, BA, peripheral blood hypotension circulation disorders, hypotension 29
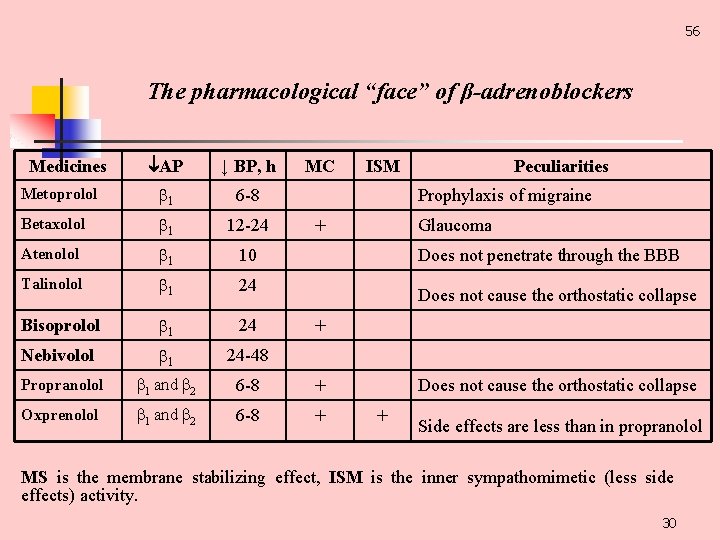
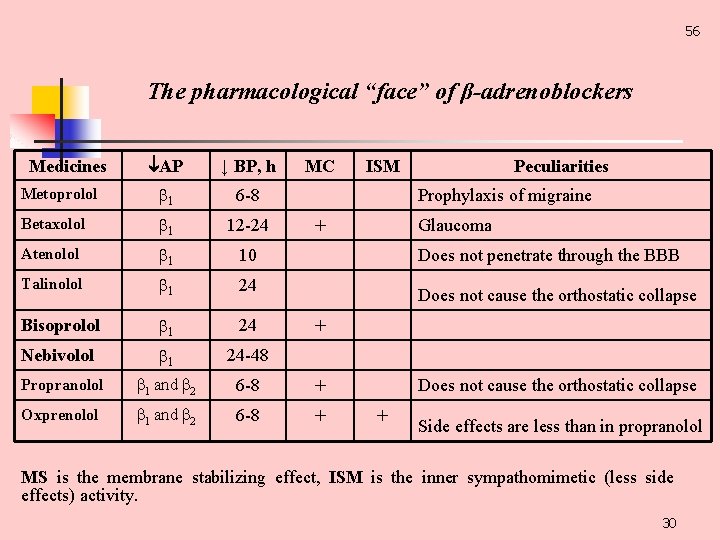
56 The pharmacological “face” of β-adrenoblockers АР ↓ BP, h Metoprolol 1 6 8 Betaxolol 1 12 24 Atenolol 1 10 Talinolol 1 24 Bisoprolol 1 24 Nebivolol 1 24 48 Propranolol 1 and 2 6 8 + Oxprenolol 1 and 2 6 8 + Medicines МС ISM Peculiarities Prophylaxis of migraine Glaucoma + Does not penetrate through the BBB Does not cause the orthostatic collapse + Side effects are less than in propranolol MS is the membrane stabilizing effect, ISM is the inner sympathomimetic (less side effects) activity. 30
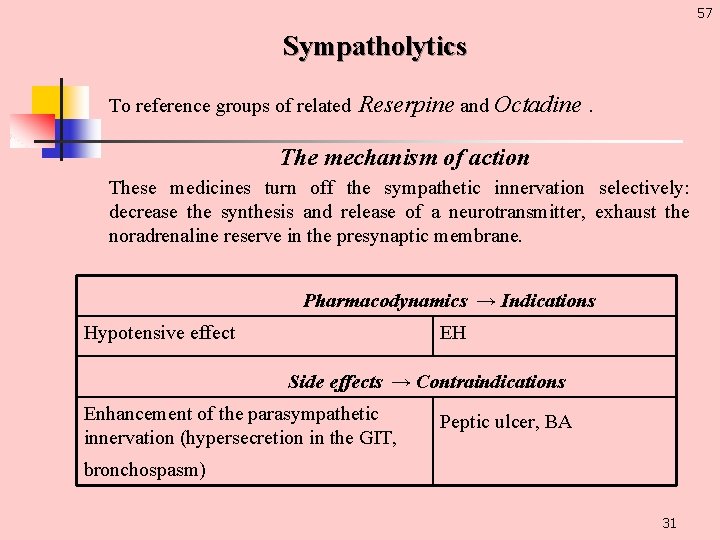
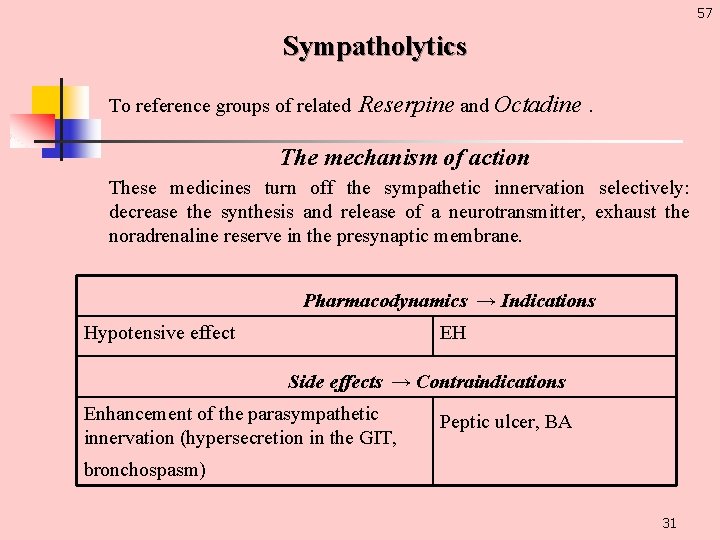
57 Sympatholytics To reference groups of related Reserpine and Octadine. The mechanism of action These medicines turn off the sympathetic innervation selectively: decrease the synthesis and release of a neurotransmitter, exhaust the noradrenaline reserve in the presynaptic membrane. Pharmacodynamics → Indications Hypotensive effect EH Side effects → Contraindications Enhancement of the parasympathetic innervation (hypersecretion in the GIT, Peptic ulcer, BA bronchospasm) 31
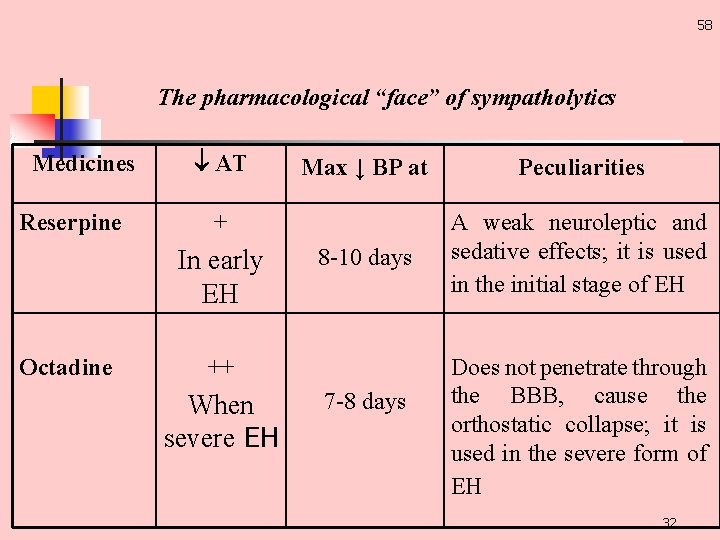
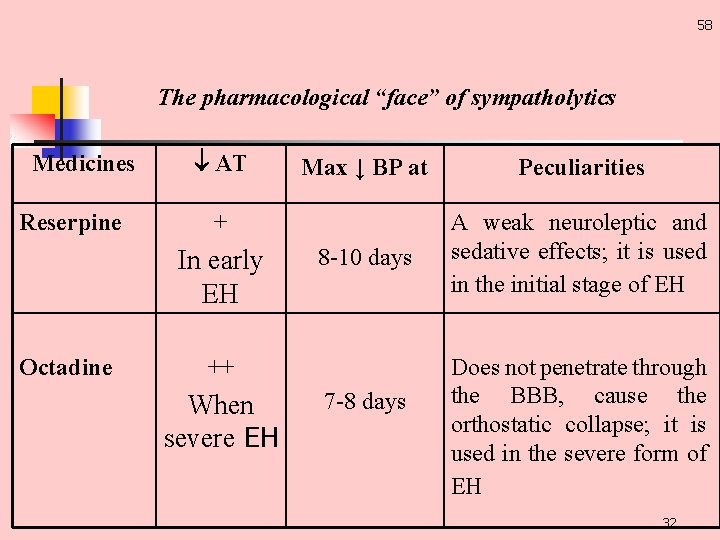
58 The pharmacological “face” of sympatholytics Medicines Reserpine АТ Peculiarities 8 10 days A weak neuroleptic and sedative effects; it is used in the initial stage of EH + In early EH Octadine Max ↓ BP at ++ When severe EH 7 8 days Does not penetrate through the BBB, cause the orthostatic collapse; it is used in the severe form of EH 32

59 Thank you! 33
 National medicines policy
National medicines policy Ibn sina university of medical and pharmaceutical sciences
Ibn sina university of medical and pharmaceutical sciences Brno veterinary
Brno veterinary Veterinary and pharmaceutical university brno
Veterinary and pharmaceutical university brno Veterinary medicines directorate
Veterinary medicines directorate Chapter 19 lesson 1 the role of medicines
Chapter 19 lesson 1 the role of medicines Staff of marvelous medicines
Staff of marvelous medicines Refrigerant management program
Refrigerant management program The drug basket method is used to dispense medication
The drug basket method is used to dispense medication Niyog-niyogan benefits
Niyog-niyogan benefits European directorate for the quality of medicines
European directorate for the quality of medicines What steps did roosevelt take to solve each problem?
What steps did roosevelt take to solve each problem? Nhs dictionary of medicines and devices
Nhs dictionary of medicines and devices Stockley’s drug interaction
Stockley’s drug interaction Ectoparasiticides veterinary medicines
Ectoparasiticides veterinary medicines Ratiograstin
Ratiograstin Medicines complete
Medicines complete Cqc medicines management
Cqc medicines management Medicines information centre
Medicines information centre Medicinescomplete martindale
Medicinescomplete martindale Pharmac special foods
Pharmac special foods Ggc medicines
Ggc medicines Federal agency for medicines and health products
Federal agency for medicines and health products Pharmacology and venipuncture in radiology pdf
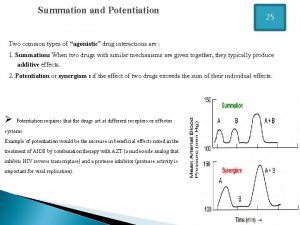
Pharmacology and venipuncture in radiology pdf Drug summation examples
Drug summation examples Zero order kinetics
Zero order kinetics What is ion trapping in pharmacology
What is ion trapping in pharmacology Drug metabolism definition
Drug metabolism definition Chapter 30 principles of pharmacology
Chapter 30 principles of pharmacology What is ion trapping in pharmacology
What is ion trapping in pharmacology Alia drug testing
Alia drug testing First pass effect
First pass effect First pass effect in pharmacology
First pass effect in pharmacology Mechanism of drug action
Mechanism of drug action