Worried Teens Worried Parents Anxiety in Teens What








- Slides: 28
Worried Teens, Worried Parents Anxiety in Teens: What to look for & How to help Collingwood Collegiate Institute November 19, 2015 Gwen Jamieson, MSW RSW GBFHT Child and Youth Team

The Georgian Bay Family Health Team We are a collaborative team of interdisciplinary health care professionals delivering quality health care in a patient-centered environment. WHAT IS A FAMILY HEALTH TEAM? Family Health Teams are primary health care organizations that include a team of family physicians, nurse practitioners, registered nurses, social workers, dietitians, and other professionals who work together to provide primary health care for their community. They ensure that people receive the care they need in their communities, as each team is set-up based on local health and community needs. THE GBFHT IS MADE UP OF: Doctors: Nurse Practitioners; Wound Care Nurse; Hypertension Nurse; Smoking Cessation Nurse Ontario Telemedicine Coordinator; Diabetes Educators Registered Dietitian Occupational Therapists; Health Promoter & Mental Health Counsellors
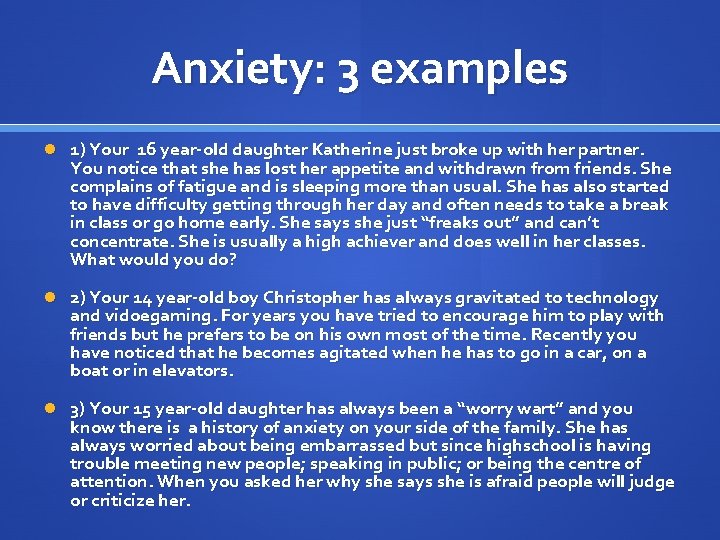
Anxiety: 3 examples 1) Your 16 year-old daughter Katherine just broke up with her partner. You notice that she has lost her appetite and withdrawn from friends. She complains of fatigue and is sleeping more than usual. She has also started to have difficulty getting through her day and often needs to take a break in class or go home early. She says she just “freaks out” and can’t concentrate. She is usually a high achiever and does well in her classes. What would you do? 2) Your 14 year-old boy Christopher has always gravitated to technology and vidoegaming. For years you have tried to encourage him to play with friends but he prefers to be on his own most of the time. Recently you have noticed that he becomes agitated when he has to go in a car, on a boat or in elevators. 3) Your 15 year-old daughter has always been a “worry wart” and you know there is a history of anxiety on your side of the family. She has always worried about being embarrassed but since highschool is having trouble meeting new people; speaking in public; or being the centre of attention. When you asked her why she says she is afraid people will judge or criticize her.
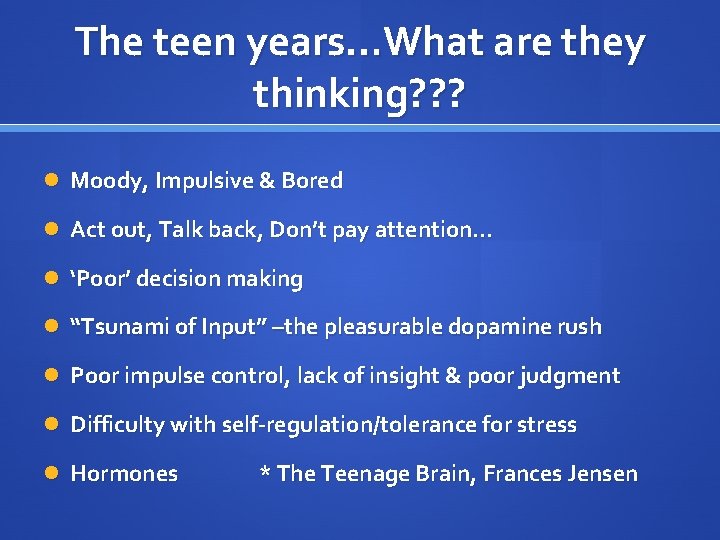
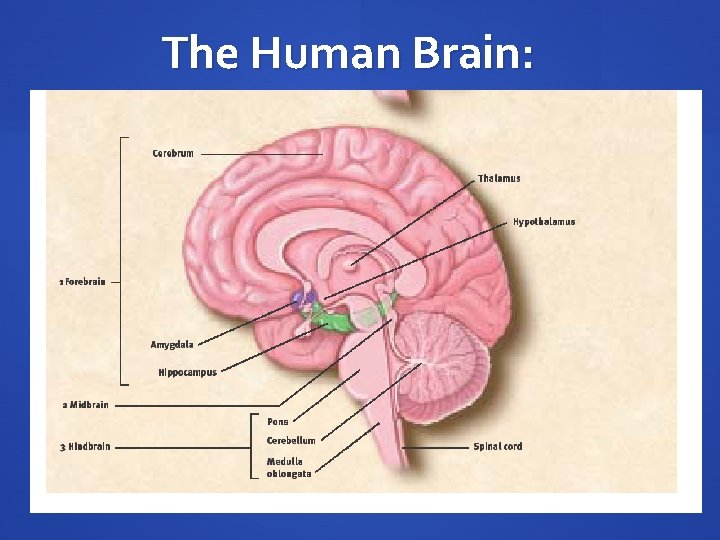
The teen years…What are they thinking? ? ? Moody, Impulsive & Bored Act out, Talk back, Don’t pay attention… ‘Poor’ decision making “Tsunami of Input” –the pleasurable dopamine rush Poor impulse control, lack of insight & poor judgment Difficulty with self-regulation/tolerance for stress Hormones * The Teenage Brain, Frances Jensen
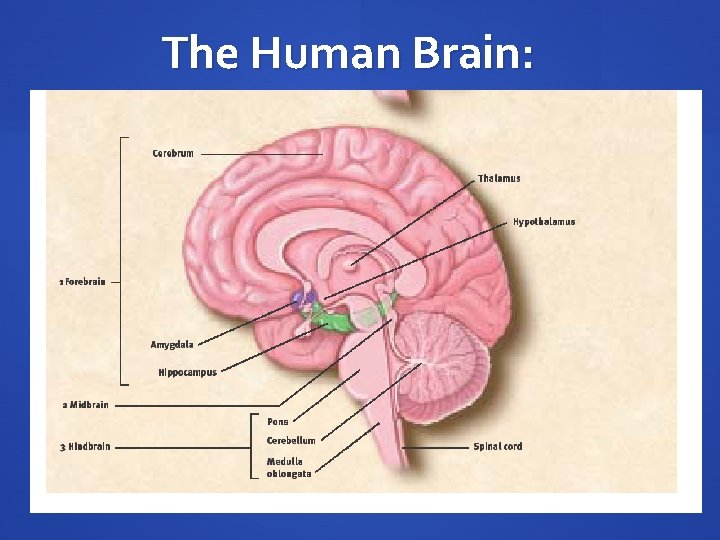
The Human Brain:
What is Anxiety? When is it normal? The Security System is responsible for our body’s anxiety symptoms and for relaxation. Our ‘alarm’ overactivates the bodily functions we need for fight-flight-freeze responses. Our heart rate goes up and our muscles tense. Anxiety is a NORMAL part of life for everyone, especially children. We need it to help us discern whether a situation is safe Common normal anxiety responses in children and teens include: Separation from parents in early childhood Taking an exam in school Giving a presentation in front of a class Interviewing for college Difficulty with night time and/or sleep
Temperament Children and Teens who have “cautious” or “sensitive” temperaments or dispositions can also be at higher risk of developing anxiety around: A strong sense of responsibility Perfectionism High standards of achievement and/or unrealistic expectations Difficulty relaxing Tendency to please others Difficulty with assertiveness Oversensitivity to criticism or rejection Tendency to worry

When is it a disorder? Disorders are commonly measured by the degree to which anxiety interferes with learning, social development, persistence of anxiety symptoms and amount of emotional distress by the child. The following areas are where these typically impact their functioning on a day-to day basis: School attendance Academic motivation Learning ability Memory Social life Concentration Attention Sleep & Appetite
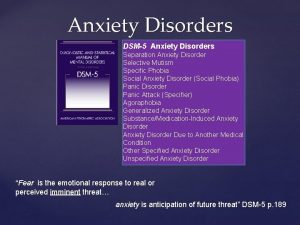
Anxiety Disorders Common anxiety diagnoses in children include: Generalized anxiety disorder Panic Disorder Separation anxiety disorder Social Anxiety Disorder Specific phobias Obsessive Compulsive Disorder, Post-Traumatic Stress Disorder, Developmental Trauma Disorder are less common than the above but still under the umbrella of anxiety disorders.
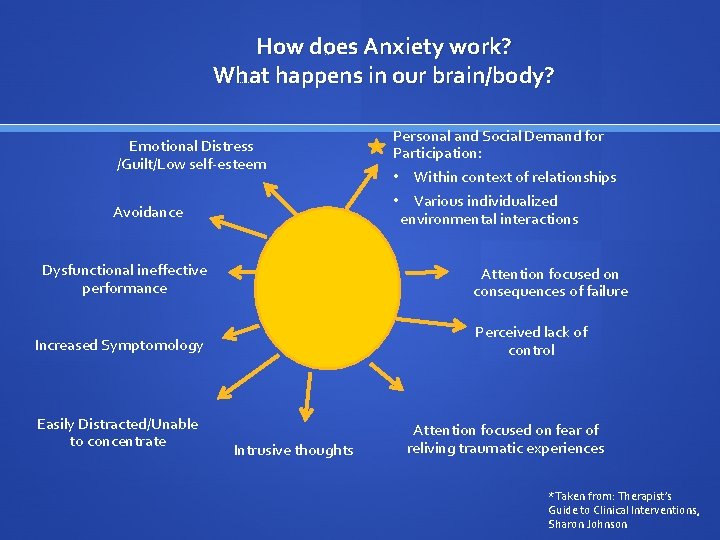
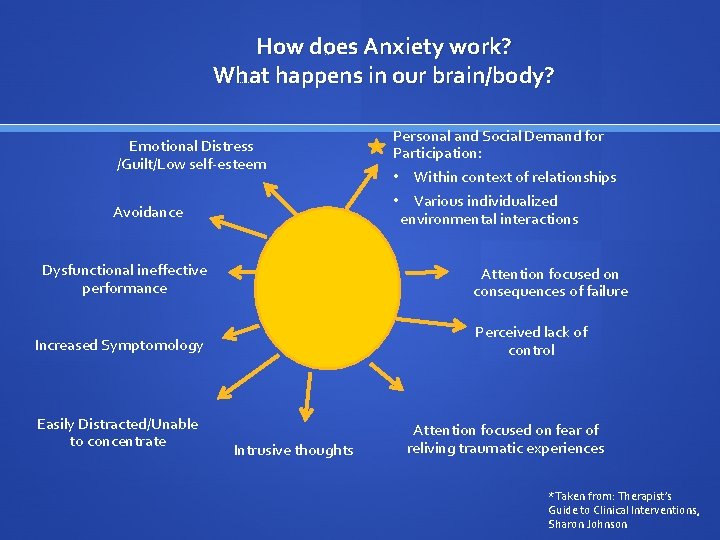
How does Anxiety work? What happens in our brain/body? Relative comfort Distances self, tries not to think about self-imposed limitation Emotional Distress /Guilt/Low self-esteem Avoidance Dysfunctional ineffective performance • Within context of relationships • Various individualized environmental interactions Attention focused on consequences of failure Perceived lack of control Increased Symptomology Easily Distracted/Unable to concentrate Personal and Social Demand for Participation: Intrusive thoughts Attention focused on fear of reliving traumatic experiences *Taken from: Therapist’s Guide to Clinical Interventions, Sharon Johnson
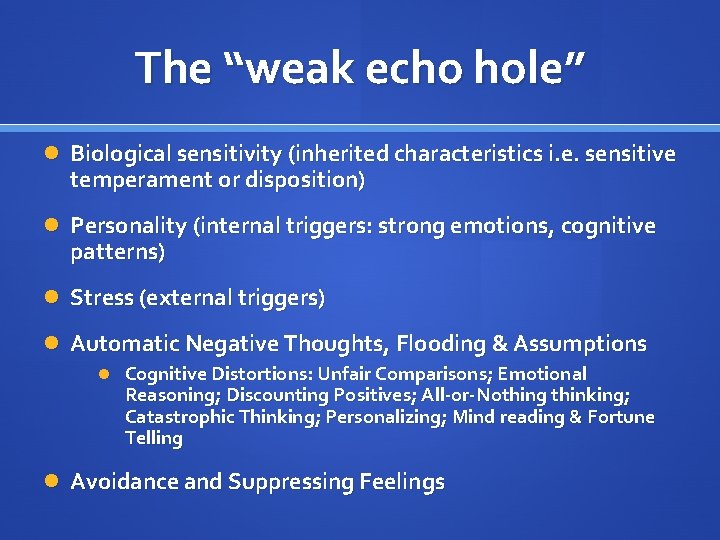
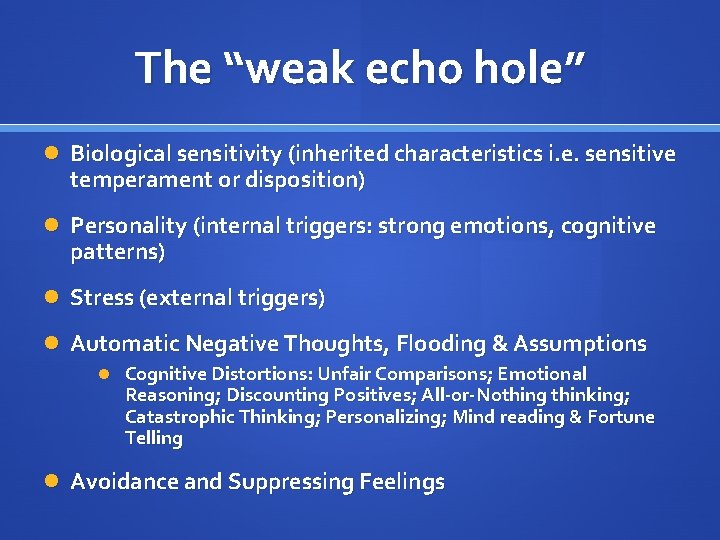
The “weak echo hole” Biological sensitivity (inherited characteristics i. e. sensitive temperament or disposition) Personality (internal triggers: strong emotions, cognitive patterns) Stress (external triggers) Automatic Negative Thoughts, Flooding & Assumptions Cognitive Distortions: Unfair Comparisons; Emotional Reasoning; Discounting Positives; All-or-Nothing thinking; Catastrophic Thinking; Personalizing; Mind reading & Fortune Telling Avoidance and Suppressing Feelings
How does anxiety present in Teens? Children and Teens often present and experience different mood changes than adults. Several large studies show teens specifically worry about family/home issues; political concerns; preparation for the future; personal appearance; social relations and school * *The Worried Child, Paul Foxman
Signs and Symptoms of an anxious teen Look for the following signs and symptoms: Children with immature cognitive linguistic development may have difficulty communicating or describing mood. They may describe physical complaints or unexplained aches and pains Sad facial expressions or poor eye contact May appear as “acting out” Reckless behaviour, hostile angry interactions or violence Loss of interest or withdrawal from peers or school activities School refusal, frequent absences or problems at school Self-depreciation and extreme sensitivity to criticism Problems with attention and concentration Boredom with peers, families or activities that were otherwise engaging
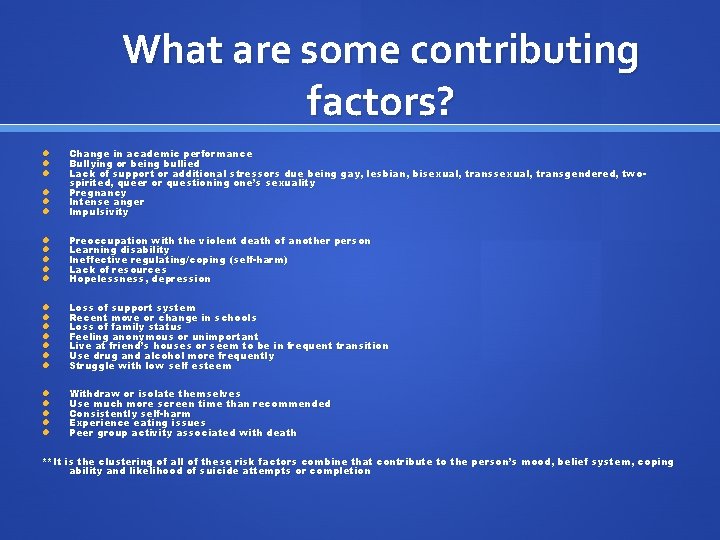
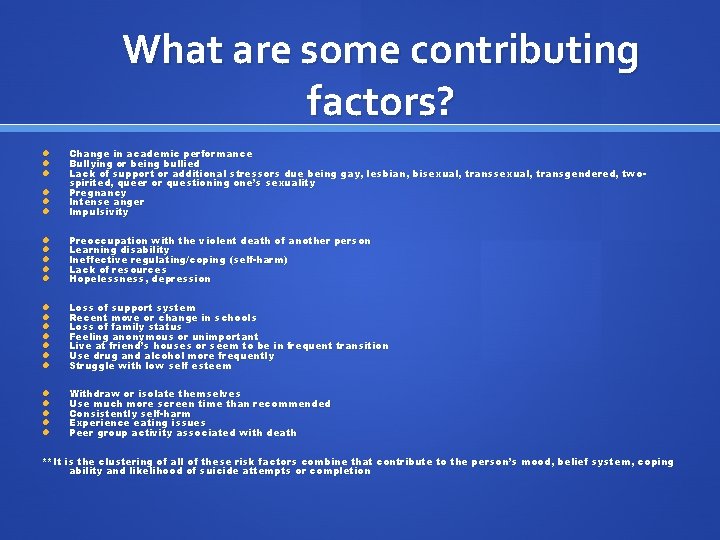
What are some contributing factors? Change in academic performance Bullying or being bullied Lack of support or additional stressors due being gay, lesbian, bisexual, transgendered, twospirited, queer or questioning one’s sexuality Pregnancy Intense anger Impulsivity Preoccupation with the violent death of another person Learning disability Ineffective regulating/coping (self-harm) Lack of resources Hopelessness, depression Loss of support system Recent move or change in schools Loss of family status Feeling anonymous or unimportant Live at friend’s houses or seem to be in frequent transition Use drug and alcohol more frequently Struggle with low self esteem Withdraw or isolate themselves Use much more screen time than recommended Consistently self-harm Experience eating issues Peer group activity associated with death **It is the clustering of all of these risk factors combine that contribute to the person’s mood, belief system, coping ability and likelihood of suicide attempts or completion
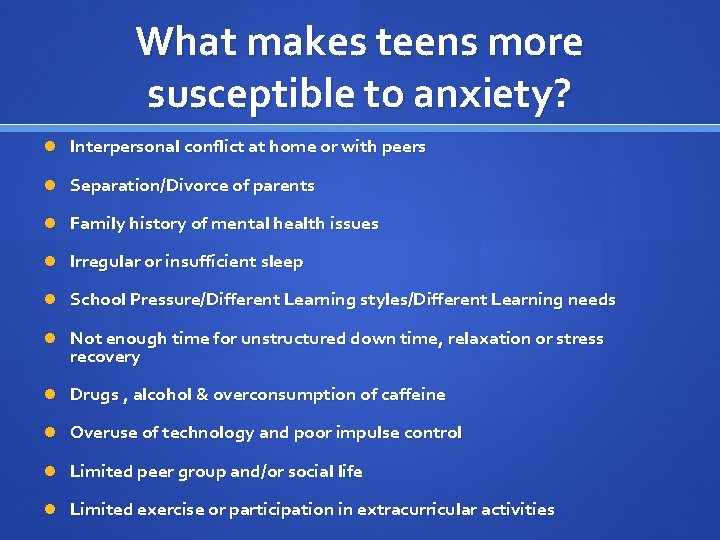
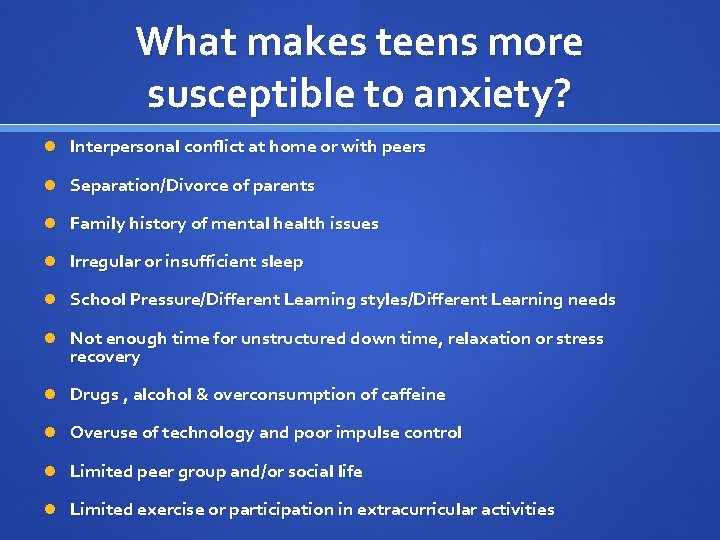
What makes teens more susceptible to anxiety? Interpersonal conflict at home or with peers Separation/Divorce of parents Family history of mental health issues Irregular or insufficient sleep School Pressure/Different Learning styles/Different Learning needs Not enough time for unstructured down time, relaxation or stress recovery Drugs , alcohol & overconsumption of caffeine Overuse of technology and poor impulse control Limited peer group and/or social life Limited exercise or participation in extracurricular activities

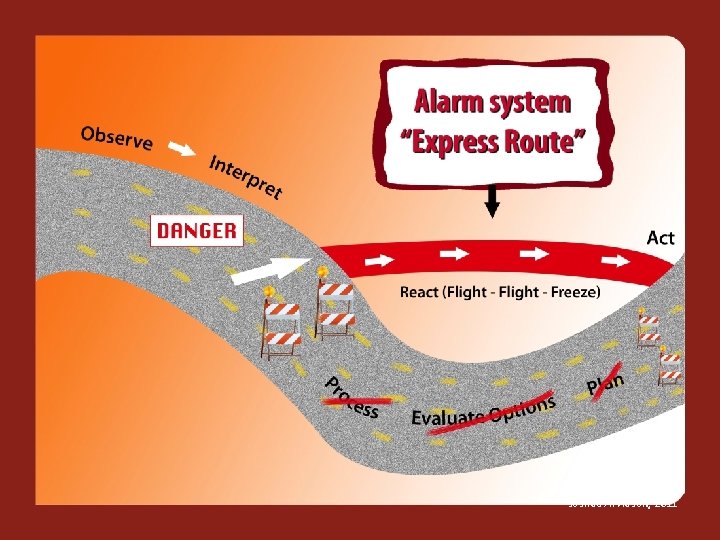
Joshua Arvidson, 2011 16
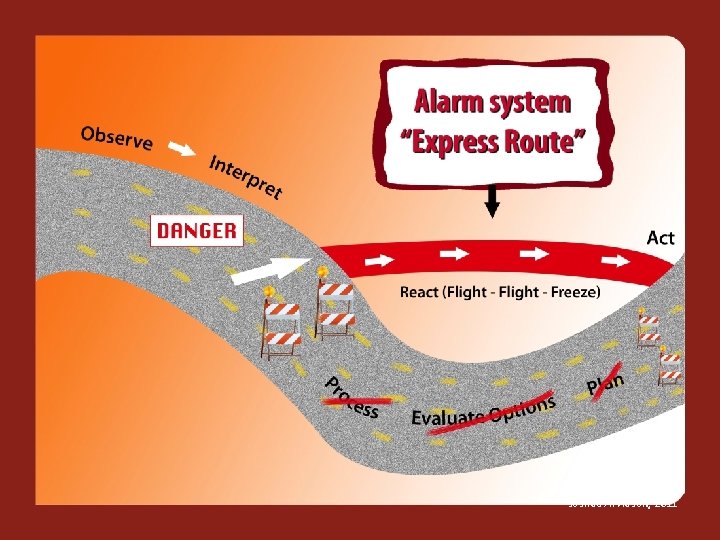
Joshua Arvidson, 2011 17

Joshua Arvidson, 2011 18
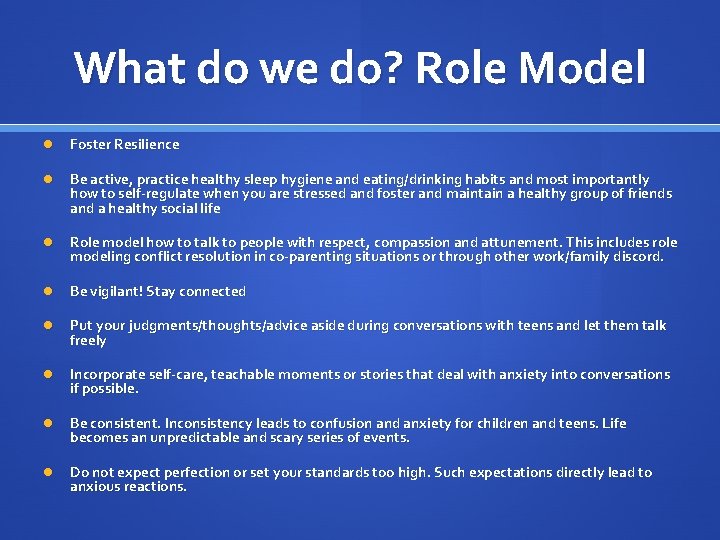
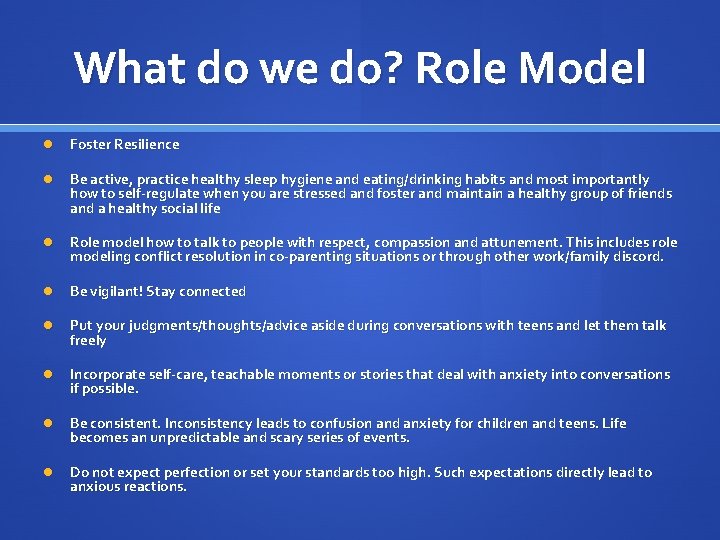
What do we do? Role Model Foster Resilience Be active, practice healthy sleep hygiene and eating/drinking habits and most importantly how to self-regulate when you are stressed and foster and maintain a healthy group of friends and a healthy social life Role model how to talk to people with respect, compassion and attunement. This includes role modeling conflict resolution in co-parenting situations or through other work/family discord. Be vigilant! Stay connected Put your judgments/thoughts/advice aside during conversations with teens and let them talk freely Incorporate self-care, teachable moments or stories that deal with anxiety into conversations if possible. Be consistent. Inconsistency leads to confusion and anxiety for children and teens. Life becomes an unpredictable and scary series of events. Do not expect perfection or set your standards too high. Such expectations directly lead to anxious reactions.
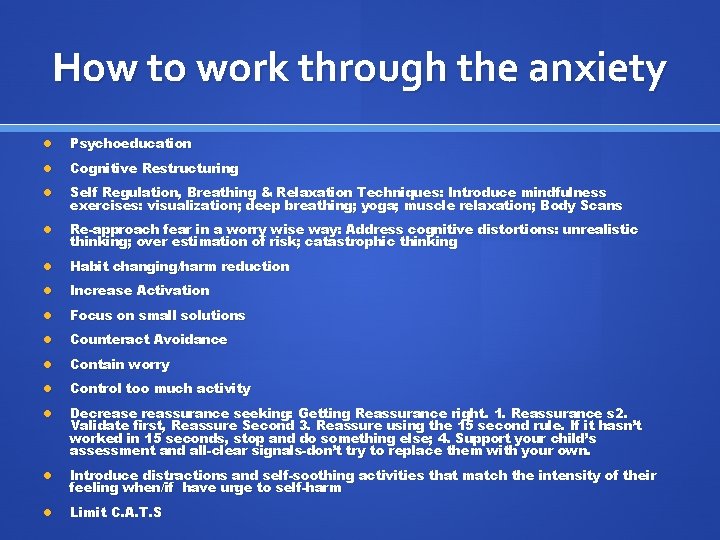
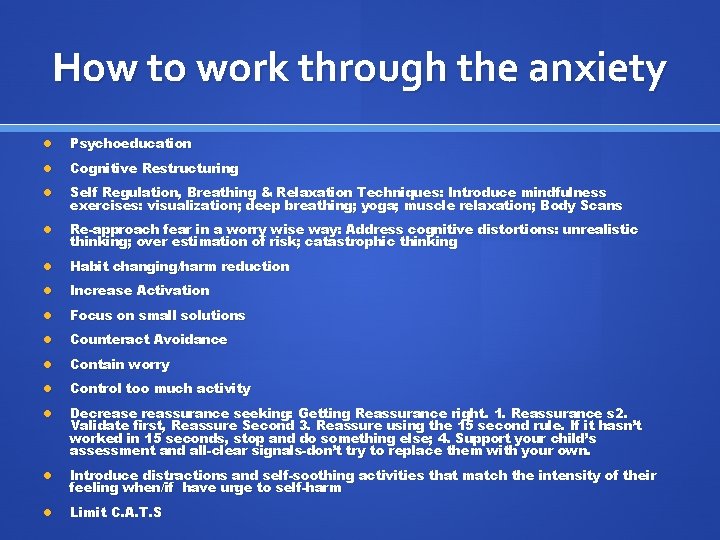
How to work through the anxiety Psychoeducation Cognitive Restructuring Self Regulation, Breathing & Relaxation Techniques: Introduce mindfulness exercises: visualization; deep breathing; yoga; muscle relaxation; Body Scans Re-approach fear in a worry wise way: Address cognitive distortions: unrealistic thinking; over estimation of risk; catastrophic thinking Habit changing/harm reduction Increase Activation Focus on small solutions Counteract Avoidance Contain worry Control too much activity Decrease reassurance seeking: Getting Reassurance right. 1. Reassurance s 2. Validate first, Reassure Second 3. Reassure using the 15 second rule. If it hasn’t worked in 15 seconds, stop and do something else; 4. Support your child’s assessment and all-clear signals-don’t try to replace them with your own. Introduce distractions and self-soothing activities that match the intensity of their feeling when/if have urge to self-harm Limit C. A. T. S
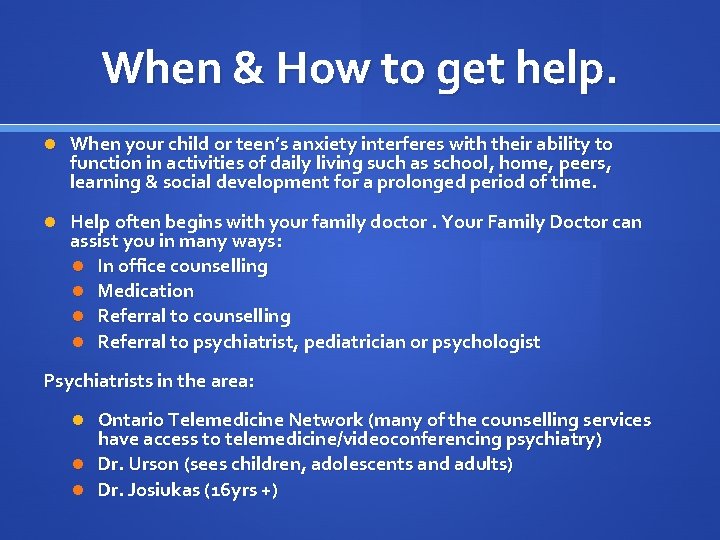
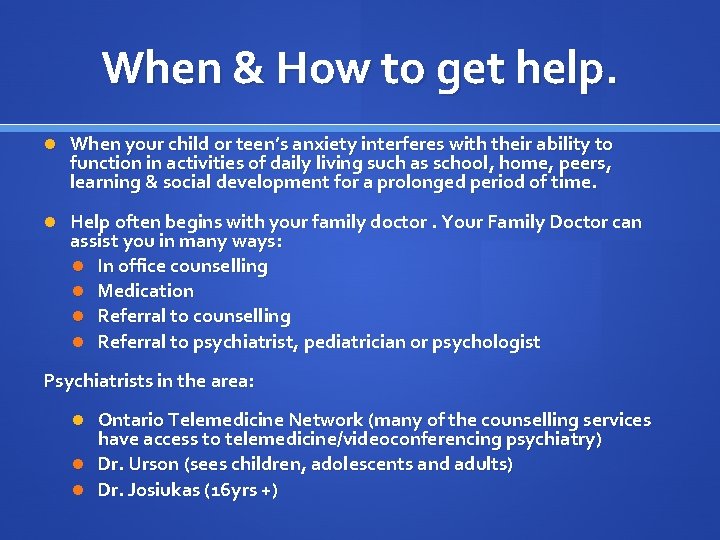
When & How to get help. When your child or teen’s anxiety interferes with their ability to function in activities of daily living such as school, home, peers, learning & social development for a prolonged period of time. Help often begins with your family doctor. Your Family Doctor can assist you in many ways: In office counselling Medication Referral to counselling Referral to psychiatrist, pediatrician or psychologist Psychiatrists in the area: Ontario Telemedicine Network (many of the counselling services have access to telemedicine/videoconferencing psychiatry) Dr. Urson (sees children, adolescents and adults) Dr. Josiukas (16 yrs +)
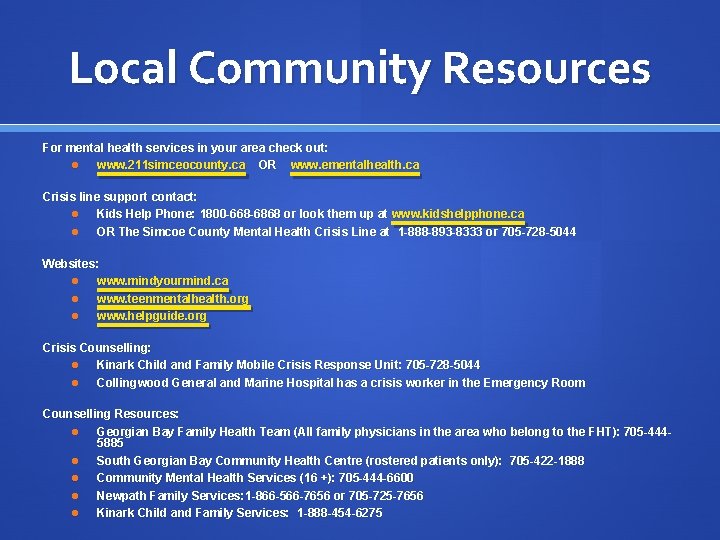
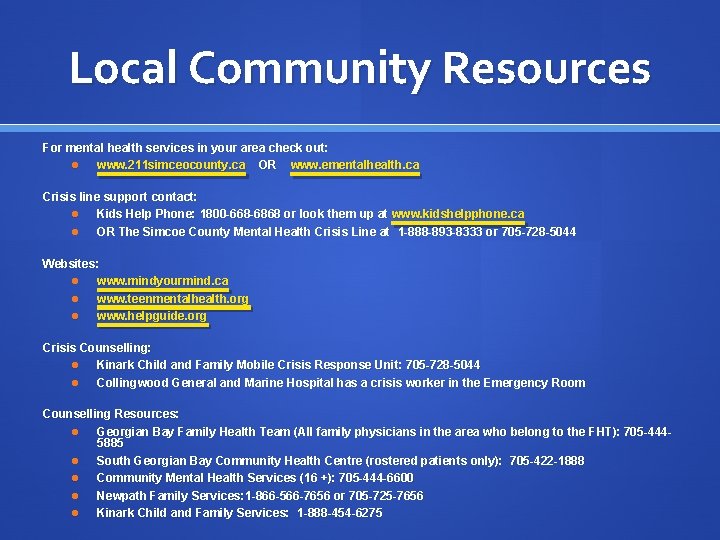
Local Community Resources For mental health services in your area check out: www. 211 simceocounty. ca OR www. ementalhealth. ca Crisis line support contact: Kids Help Phone: 1800 -668 -6868 or look them up at www. kidshelpphone. ca OR The Simcoe County Mental Health Crisis Line at 1 -888 -893 -8333 or 705 -728 -5044 Websites: www. mindyourmind. ca www. teenmentalhealth. org www. helpguide. org Crisis Counselling: Kinark Child and Family Mobile Crisis Response Unit: 705 -728 -5044 Collingwood General and Marine Hospital has a crisis worker in the Emergency Room Counselling Resources: Georgian Bay Family Health Team (All family physicians in the area who belong to the FHT): 705 -4445885 South Georgian Bay Community Health Centre (rostered patients only): 705 -422 -1888 Community Mental Health Services (16 +): 705 -444 -6600 Newpath Family Services: 1 -866 -566 -7656 or 705 -725 -7656 Kinark Child and Family Services: 1 -888 -454 -6275
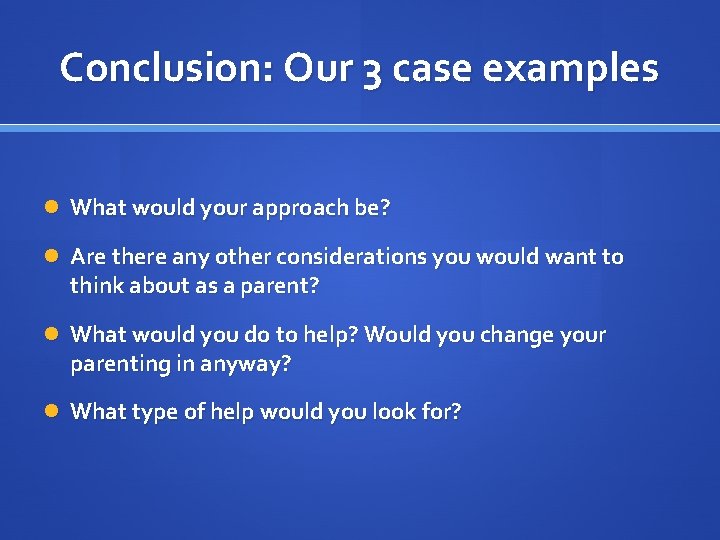
Conclusion: Our 3 case examples What would your approach be? Are there any other considerations you would want to think about as a parent? What would you do to help? Would you change your parenting in anyway? What type of help would you look for?
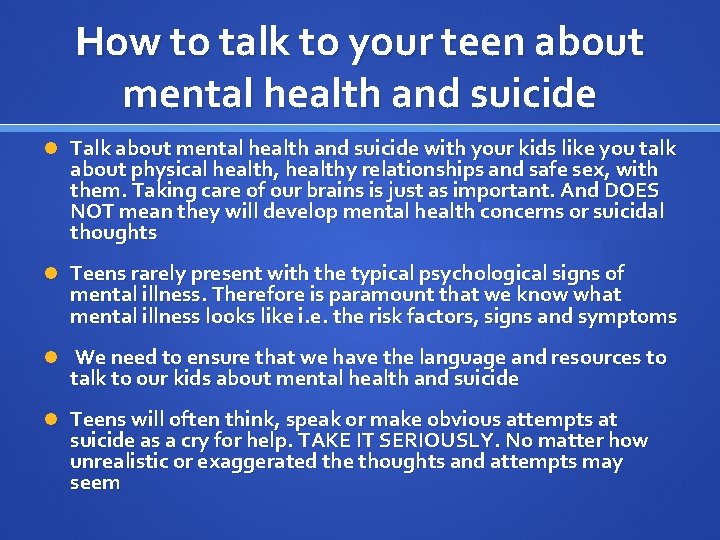
How to talk to your teen about mental health and suicide Talk about mental health and suicide with your kids like you talk about physical health, healthy relationships and safe sex, with them. Taking care of our brains is just as important. And DOES NOT mean they will develop mental health concerns or suicidal thoughts Teens rarely present with the typical psychological signs of mental illness. Therefore is paramount that we know what mental illness looks like i. e. the risk factors, signs and symptoms We need to ensure that we have the language and resources to talk to our kids about mental health and suicide Teens will often think, speak or make obvious attempts at suicide as a cry for help. TAKE IT SERIOUSLY. No matter how unrealistic or exaggerated the thoughts and attempts may seem

WHAT TO SAY: Responding to teens in trouble If your teen makes an “I wish I was dead” statement, do not dismiss it. Rather, use this as an opportunity to be curious about their thoughts “It sounds like you are having a really hard time right now. ” “I want to make sure you always have someone to talk to when you are feeling this way because we care about you and love you a lot Listen and attune yourself to them without imposing your thoughts, opinions or judgments If your teen talks about dying, make sure you ask them if they have a plan, time frame and means. It is important to remove any weapons, medication or other means of harming themselves – not because of trust, but because impulsivity can become a very dangerous symptom

What to Say: cont’d Kids need extra support and attention during these times. Work to avoid becoming detached from your teen when they are pulling away, even if it means a change in your approach Try to avoid continuous confrontation or power struggles with your teen as well as your co-parent about this issue Raise the issue and talk about mental health openly and without judgment so they know it is not something to be ashamed of and not a taboo subject If your child is cutting or acting out as a way of self-soothing, be gentle instead of angry. Try not to use shame-based discipline or further humiliate them. This will increase their feelings of worthlessness and selfhatred which may lead to more impulsive or dangerous cutting Even if this subject in relation to your child makes you feel extremely worried, remember to stay calm and raise the subject instead of avoiding it. Silence can be dangerous.

Developing a safety Plan with your teen Here is an example of a safety plan: When I am feeling overwhelmed and thinking about suicide, Ill take the following steps: 1. 2. 3. 4. 5. 6. 7. Take a deep breath and try to identify what’s troubling me right now Write down all of the feelings (sad, mad, lonely, helpless, scared etc. ) as a record for later Try to do things that help me feel better for at least 30 minutes (have a bath, talk to a friend, walk the dog, listen to upbeat music) Write down the individual negative thoughts and provide an alternative response that changes my perspective If suicidal thoughts continue, I will call my emergency person (name, phone number) If that person isn’t available, I will call the 24 hour crisis line (phone number) If I still feel suicidal and out-of-control, I will go to the nearest hospital emergency department Signature:

Crisis Support/Hospitalization If you are concerned about the immediate safety of your child or teen take them to your nearest emergency department at which time they will be assessed by an emergency physician and connected with the appropriate resources. If it is deemed that your child is at substantial risk of suicide and needs further hospitalization. the nearest pediatric inpatient psychiatry units are in Newmarket, Owensound or Orillia. This usually occurs when a child/teen is at high risk for suicide, lacks adequate supports, lacks adequate impulse control or is intoxicated or psychotic Other treatment facilities include but are not limited to: Youthdale Ontario Shores London Health Sciences Sick kids Mc. Master University Medical centre
 Parents parents
Parents parents Fiche histoire des arts frida kahlo
Fiche histoire des arts frida kahlo Parent frida kahlo
Parent frida kahlo Comparatives and superlatives slim
Comparatives and superlatives slim Why was von bulow worried about england france and russia
Why was von bulow worried about england france and russia When atticus speaks of defending tom robinson
When atticus speaks of defending tom robinson Red similes
Red similes Percy jackson and the lightning thief chapter 13
Percy jackson and the lightning thief chapter 13 Worried
Worried 7 habits of highly effective teens quotes
7 habits of highly effective teens quotes Png
Png 7 habits of highly effective teens habit 2
7 habits of highly effective teens habit 2 Love language test teenager
Love language test teenager Teens for unity
Teens for unity Proactive vs reactive 7 habits
Proactive vs reactive 7 habits 7 defective habits
7 defective habits Preteens nn
Preteens nn Project ideas for teens
Project ideas for teens Short term goals for teenager
Short term goals for teenager A-teens 사라 룸홀트
A-teens 사라 룸홀트 Qkeq-yvn8ew -site:youtube.com
Qkeq-yvn8ew -site:youtube.com Long term goals examples
Long term goals examples Tots tweens and teens
Tots tweens and teens Lifeseasons
Lifeseasons Janet belsky
Janet belsky One's accumulated knowledge would highlight intelligence
One's accumulated knowledge would highlight intelligence Nn teen porn
Nn teen porn Courage zone 7 habits
Courage zone 7 habits How does digital media try to hook you
How does digital media try to hook you