Understanding the MACRA Quality Payment Program st o


- Slides: 14
Understanding the MACRA Quality Payment Program
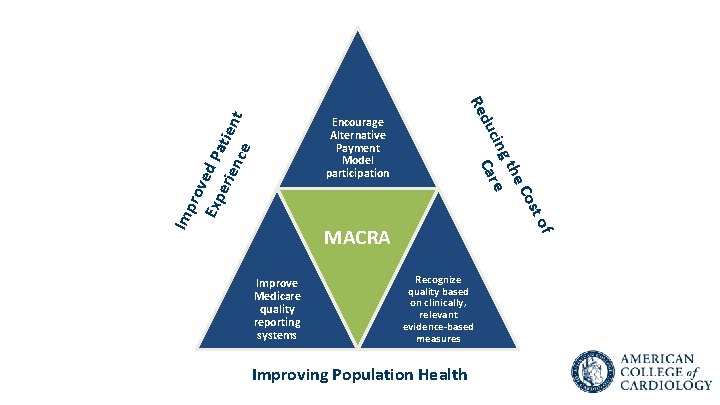
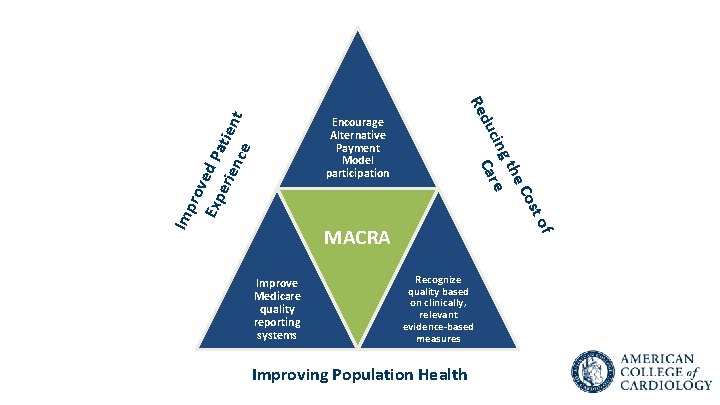
st o Imp rov Exp ed Pa eri enc tient e Co he gt cin Care du Re Encourage Alternative Payment Model participation Improve Medicare quality reporting systems f MACRA Recognize quality based on clinically, relevant evidence-based measures Improving Population Health

MACRA Impact on Health Care Delivery Will be Profound
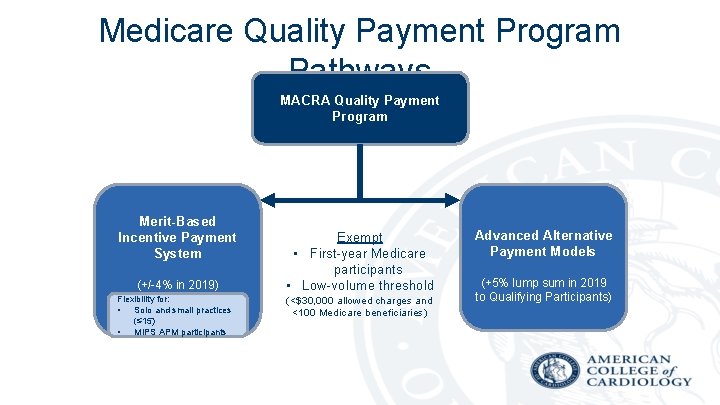
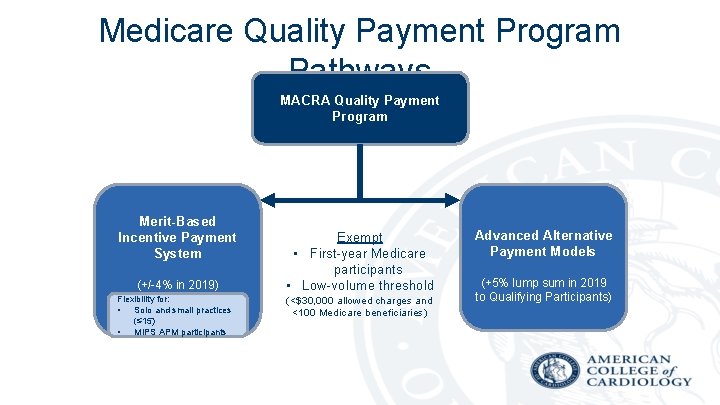
Medicare Quality Payment Program Pathways MACRA Quality Payment Program Merit-Based Incentive Payment System (+/-4% in 2019) Flexibility for: • Solo and small practices (≤ 15) • MIPS APM participants Exempt • First-year Medicare participants • Low-volume threshold (<$30, 000 allowed charges and <100 Medicare beneficiaries) Advanced Alternative Payment Models (+5% lump sum in 2019 to Qualifying Participants)
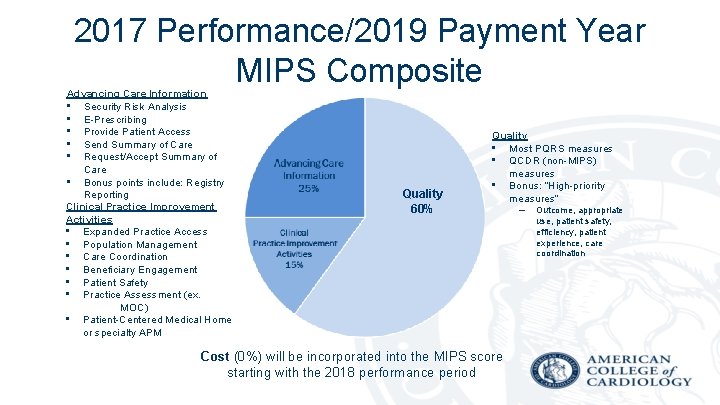
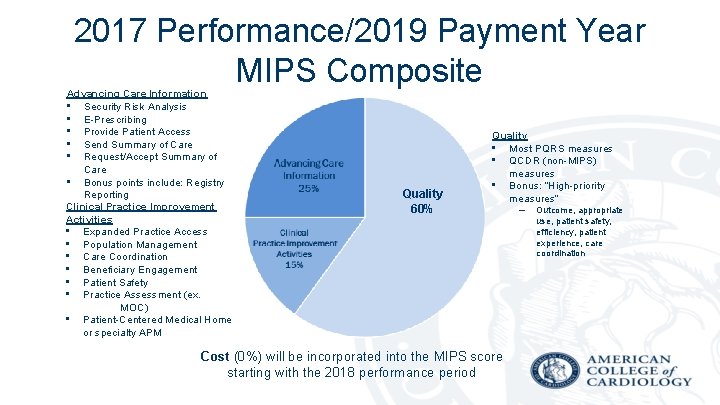
2017 Performance/2019 Payment Year MIPS Composite Advancing Care Information • Security Risk Analysis • E-Prescribing • Provide Patient Access • Send Summary of Care • Request/Accept Summary of Care • Bonus points include: Registry Reporting Clinical Practice Improvement Activities • Expanded Practice Access • Population Management • Care Coordination • Beneficiary Engagement • Patient Safety • Practice Assessment (ex. MOC) • Patient-Centered Medical Home or specialty APM Quality 60% Quality • Most PQRS measures • QCDR (non-MIPS) measures • Bonus: “High-priority measures” Cost (0%) will be incorporated into the MIPS score starting with the 2018 performance period – Outcome, appropriate use, patient safety, efficiency, patient experience, care coordination
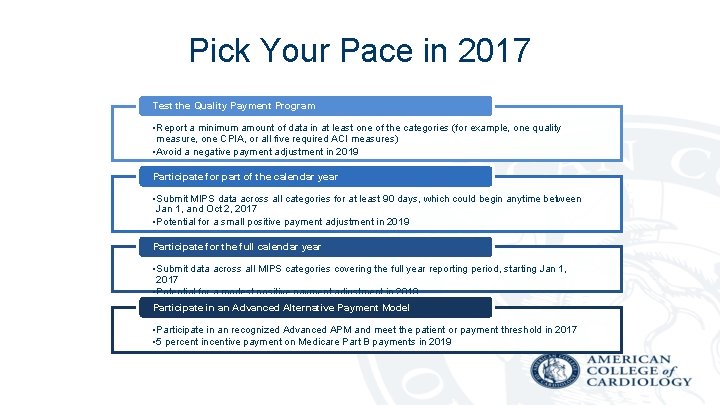
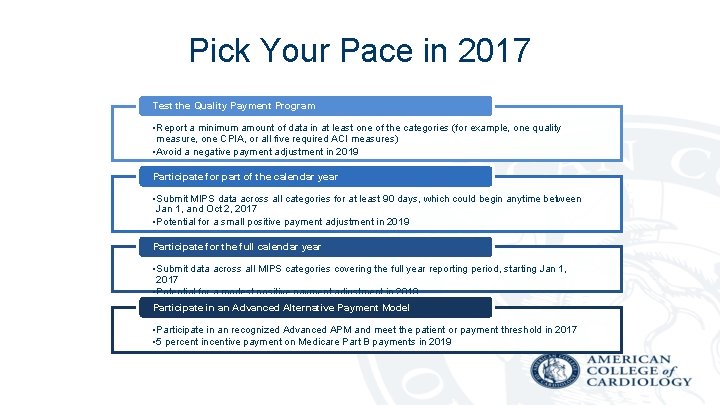
Pick Your Pace in 2017 Test the Quality Payment Program • Report a minimum amount of data in at least one of the categories (for example, one quality measure, one CPIA, or all five required ACI measures) • Avoid a negative payment adjustment in 2019 Participate for part of the calendar year • Submit MIPS data across all categories for at least 90 days, which could begin anytime between Jan 1, and Oct 2, 2017 • Potential for a small positive payment adjustment in 2019 Participate for the full calendar year • Submit data across all MIPS categories covering the full year reporting period, starting Jan 1, 2017 • Potential for a modest positive payment adjustment in 2019 Participate in an Advanced Alternative Payment Model • Participate in an recognized Advanced APM and meet the patient or payment threshold in 2017 • 5 percent incentive payment on Medicare Part B payments in 2019
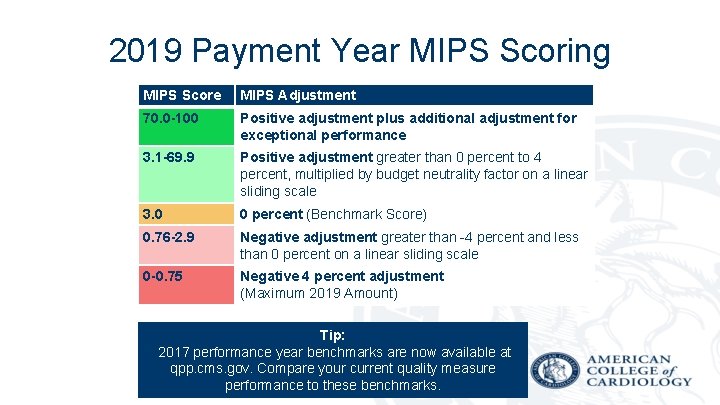
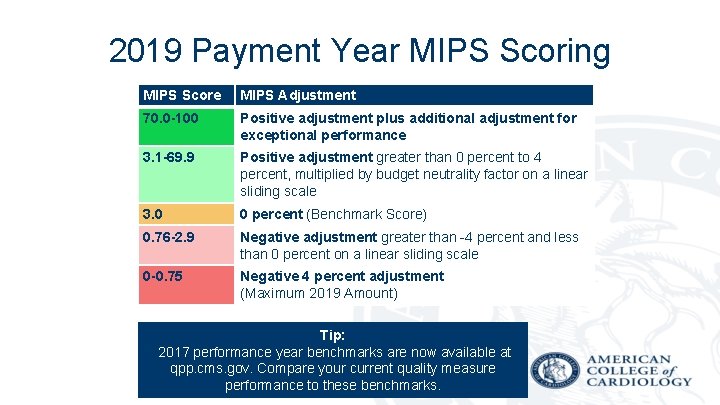
2019 Payment Year MIPS Scoring MIPS Score MIPS Adjustment 70. 0 -100 Positive adjustment plus additional adjustment for exceptional performance 3. 1 -69. 9 Positive adjustment greater than 0 percent to 4 percent, multiplied by budget neutrality factor on a linear sliding scale 3. 0 0 percent (Benchmark Score) 0. 76 -2. 9 Negative adjustment greater than -4 percent and less than 0 percent on a linear sliding scale 0 -0. 75 Negative 4 percent adjustment (Maximum 2019 Amount) Tip: 2017 performance year benchmarks are now available at qpp. cms. gov. Compare your current quality measure performance to these benchmarks.
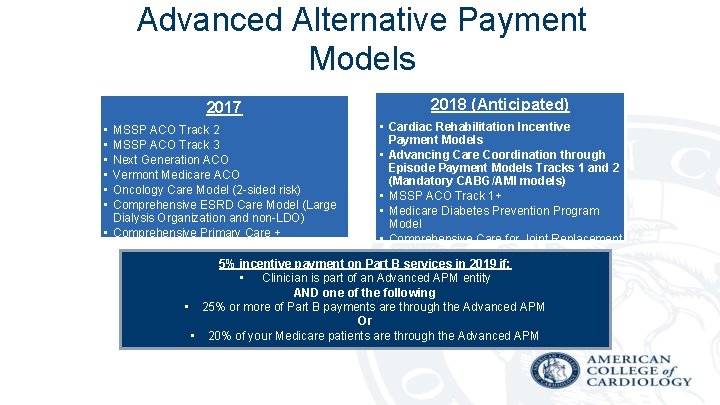
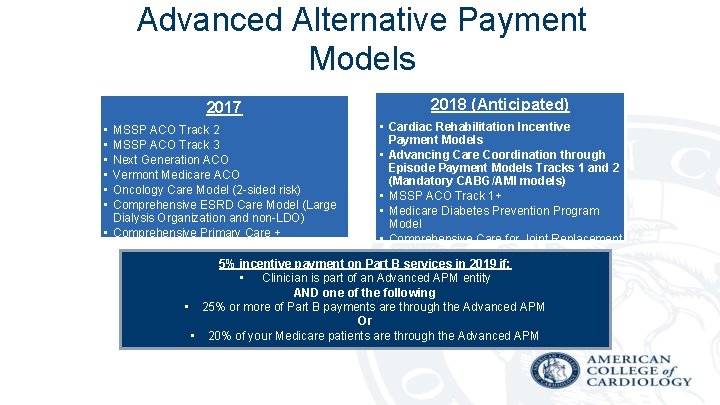
Advanced Alternative Payment Models 2017 • • • 2018 (Anticipated) • Cardiac Rehabilitation Incentive Payment Models • Advancing Care Coordination through Episode Payment Models Tracks 1 and 2 (Mandatory CABG/AMI models) • MSSP ACO Track 1+ • Medicare Diabetes Prevention Program Model • Comprehensive Care for Joint Replacement Model (CEHRT track) 5% incentive payment on Part B services in 2019 if: • Clinician is part of an Advanced APM entity AND one of the following • 25% or more of Part B payments are through the Advanced APM Or • 20% of your Medicare patients are through the Advanced APM MSSP ACO Track 2 MSSP ACO Track 3 Next Generation ACO Vermont Medicare ACO Oncology Care Model (2 -sided risk) Comprehensive ESRD Care Model (Large Dialysis Organization and non-LDO) • Comprehensive Primary Care +
Advocacy Efforts will Continue • 2017 and 2018 will likely be transition years with ongoing refinements to the QPP – Those already familiar with the current Medicare programs (PQRS, EHR Incentive, Value Modifier) will be best prepared • ACC working with Congress, HHS and CMS to ensure that the QPP supports evidence-based, cost-effective, high quality care
Recognizing NCDR Participation • NCDR registries as a way to • ACC staff is working towards creating specific NCDR meet reporting requirements Registry-based solutions to under three MIPS the Clinical Practice components: Improvement Activities – Quality participation requirement. – Advancing care information – Clinical Practice Improvement Activities
The Quality Payment Program Began Jan 1, 2017 ü Ensure that you have been successful in the existing programs – PQRS, Meaningful Use, Value Modifier ü Find out if you are participating in an alternative payment model ü Work with your administrator to find and understand your cost and quality data ü Make care coordination an organizational priority ü Focus on proper documentation ü Watch qpp. cms. gov and acc. org/macra for updates and tips ü E-mail macra@acc. org with questions

There Will Be Additional Opportunities for ACC to Provide Input Into How the MACRA Quality Payment Program Will Function MACRA t a e b ill w e W ! e l b a the t
More information is available on the ACC’s online MACRA hub at www. ACC. org/MACRA Updates are provided via the hub and through the ACC’s Advocate newsletter.