Thymic Neuroendocrine Tumors Demographics Treatment and Survival Charles
- Slides: 16
Thymic Neuroendocrine Tumors: Demographics, Treatment and Survival Charles T. Bakhos MD MS, Aitua Salami MD MPH, Larry Kaiser MD, Roman V. Petrov MD Ph. D, Abbas E. Abbas MD MS Temple University Hospital, Philadelphia, PA ISMICS Meeting Warsaw, Poland June 2020
Thymic Neuroendocrine Tumors: Demographics, Treatment and Survival No disclosures
Introduction • Thymic neuroendocrine tumors (TNET): • Non-thymomatous malignancy • ~ 1 / 5 000 US population 1 • 0. 4% of all carcinoid tumors • Recently distinguished form thymic carcinomas (WHO) • Lack of outcomes data for TNET 1. Chaer R et al. Primary neuroendocrine tumors of the thymus. Ann Thorac Surg 2002
Introduction Knowledge gap: • Survival outcomes of TNET have not been thoroughly compared Study aim: • To examine the demographic, clinical, treatment and survival characteristics of TNET.
Methods • Study design: • Retrospective cohort study using the NCDB (2004 – 2015) • Inclusion criteria: • Histologic diagnosis of TNET • WHO ICD-0 -3 • Exclusion criteria: • Age < 18 years • Incomplete staging data
Methods • Primary outcomes: • Overall survival • Secondary outcomes: • Demographic, clinical, treatment characteristics • Statistical analyses: • Survival analyses • Multivariable logistic and cox regression
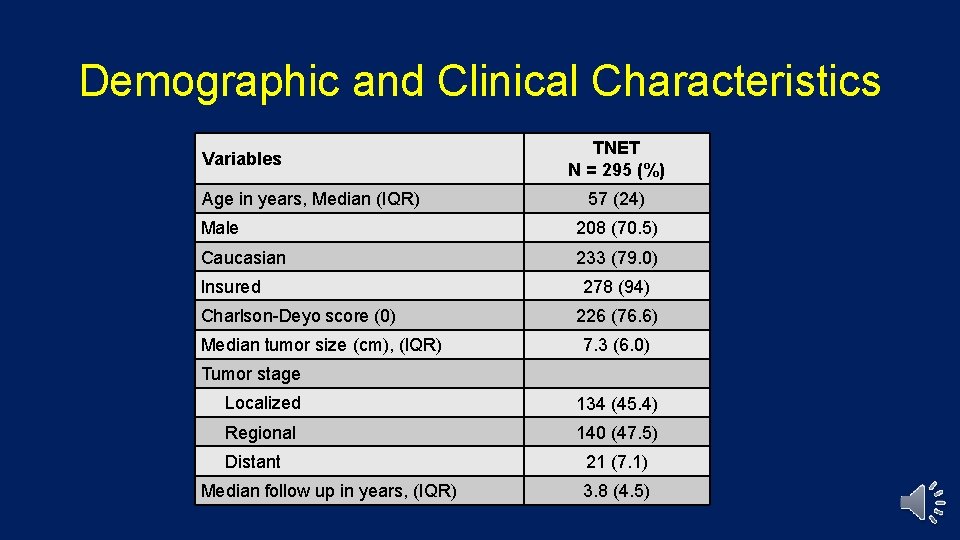
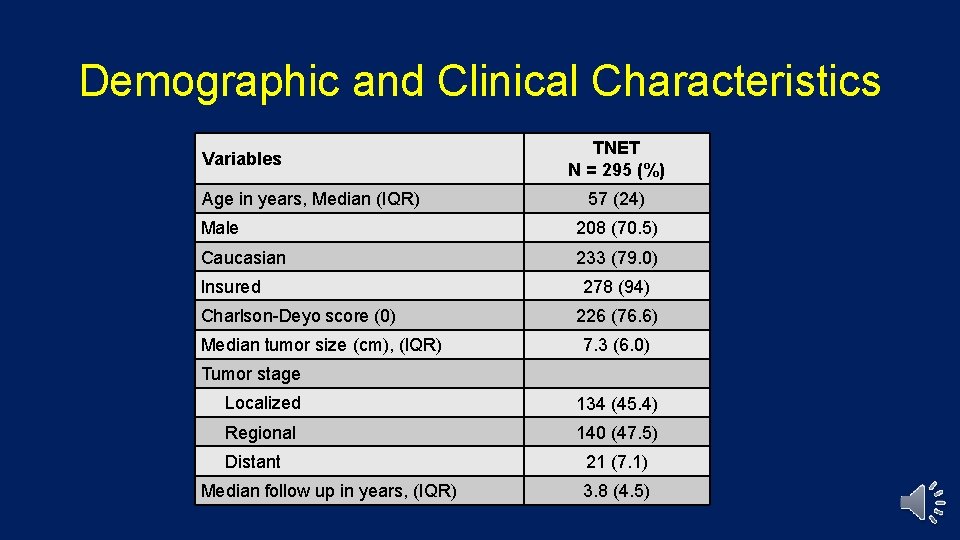
Demographic and Clinical Characteristics Variables Age in years, Median (IQR) TNET N = 295 (%) 57 (24) Male 208 (70. 5) Caucasian 233 (79. 0) Insured Charlson-Deyo score (0) Median tumor size (cm), (IQR) 278 (94) 226 (76. 6) 7. 3 (6. 0) Tumor stage Localized 134 (45. 4) Regional 140 (47. 5) Distant Median follow up in years, (IQR) 21 (7. 1) 3. 8 (4. 5)
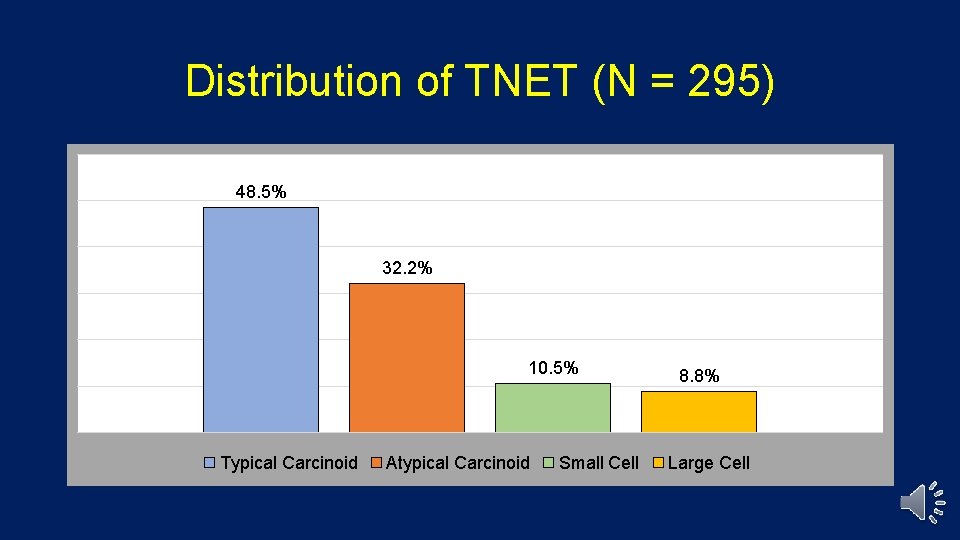
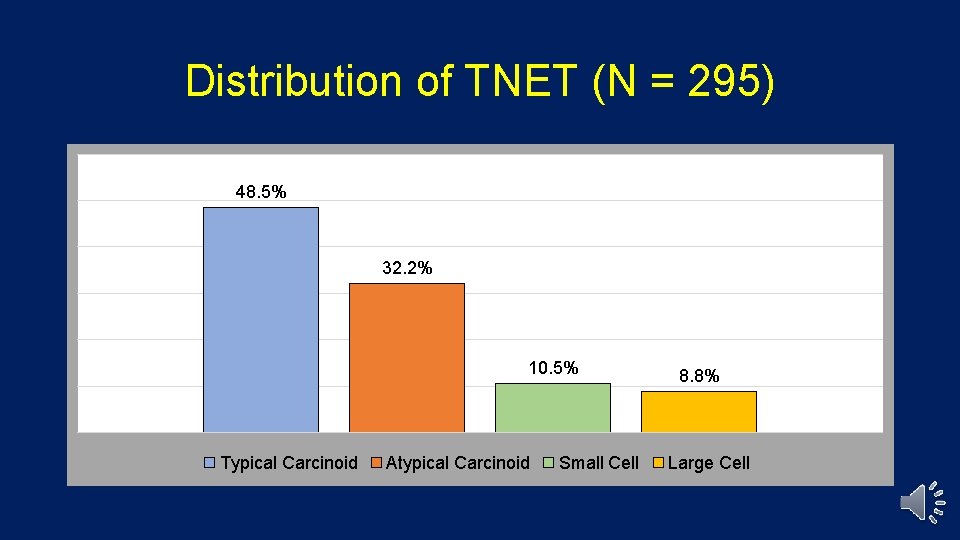
Distribution of TNET (N = 295) 48. 5% 32. 2% 10. 5% Typical Carcinoid Atypical Carcinoid Small Cell 8. 8% Large Cell
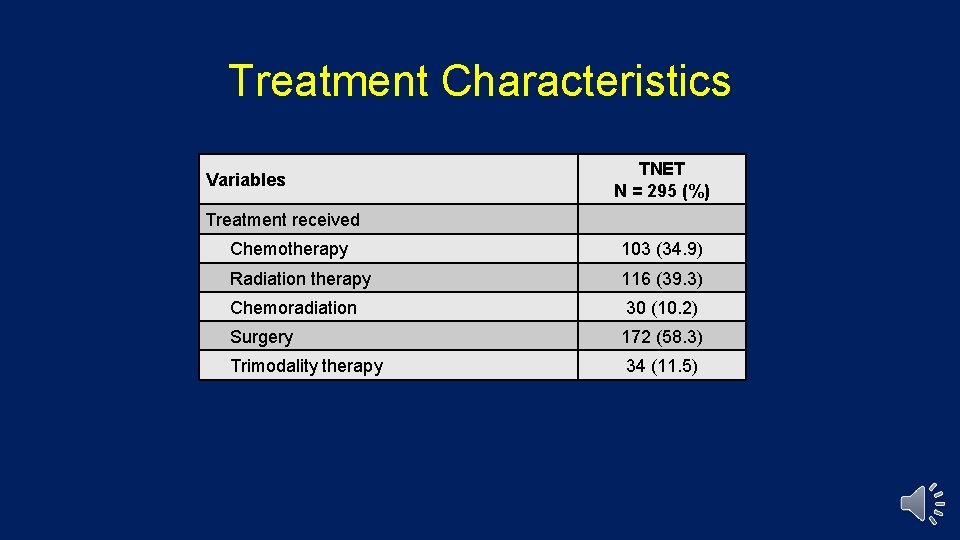
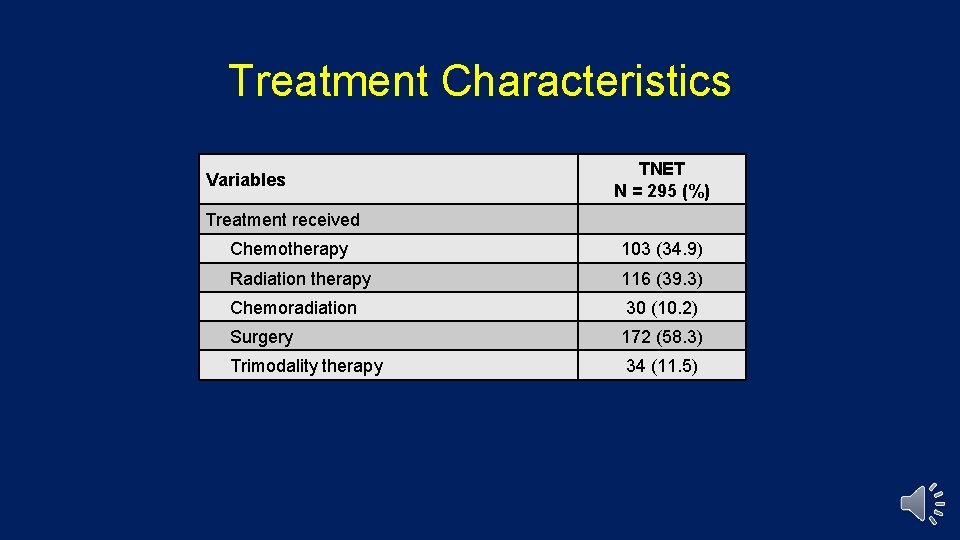
Treatment Characteristics Variables TNET N = 295 (%) Treatment received Chemotherapy 103 (34. 9) Radiation therapy 116 (39. 3) Chemoradiation 30 (10. 2) Surgery 172 (58. 3) Trimodality therapy 34 (11. 5)
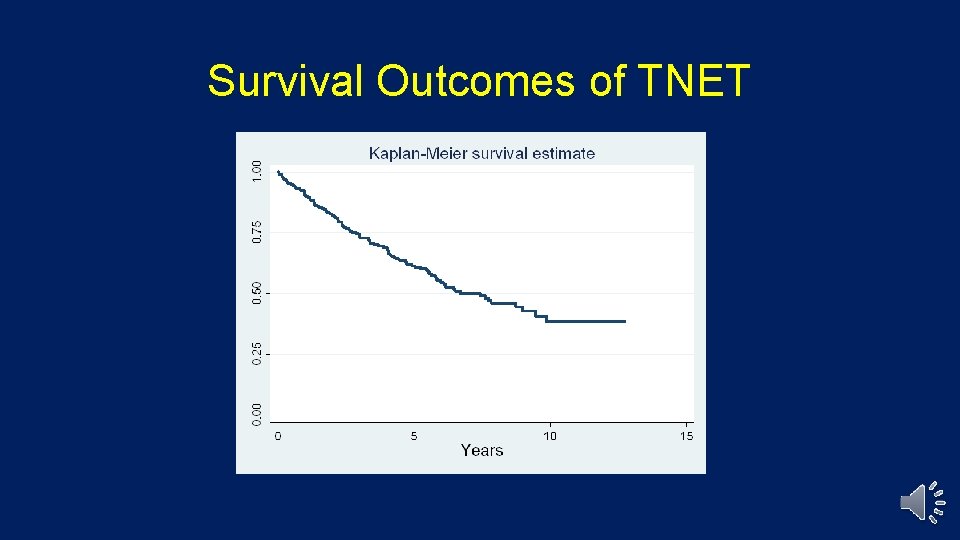
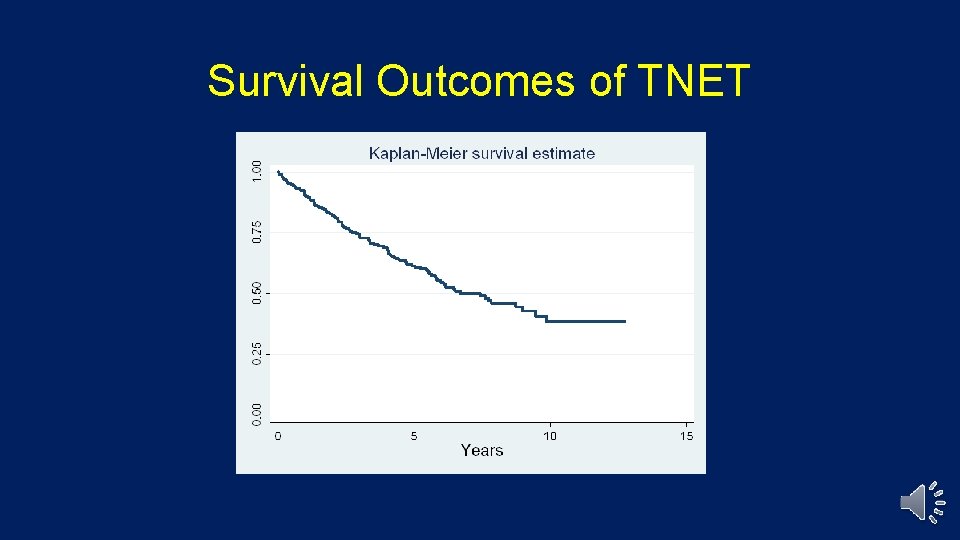
Survival Outcomes of TNET
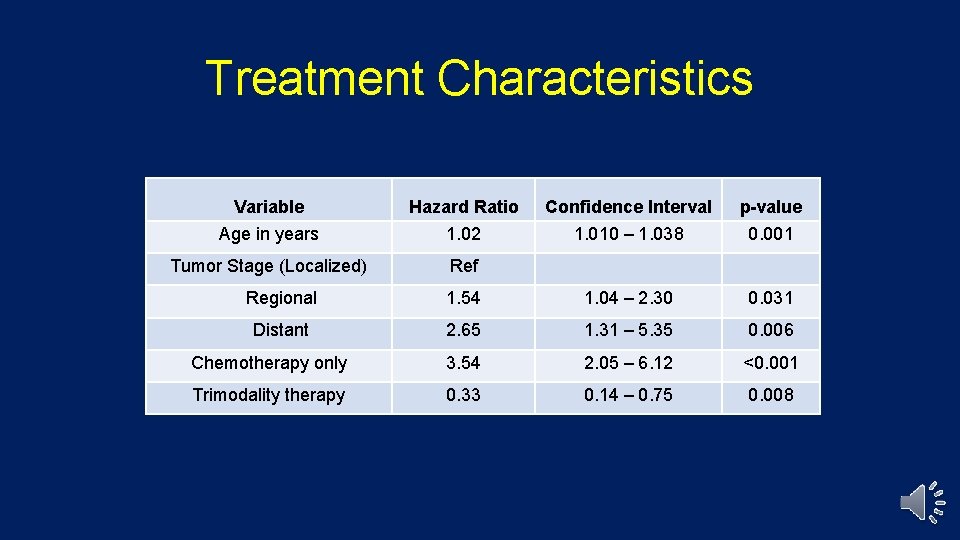
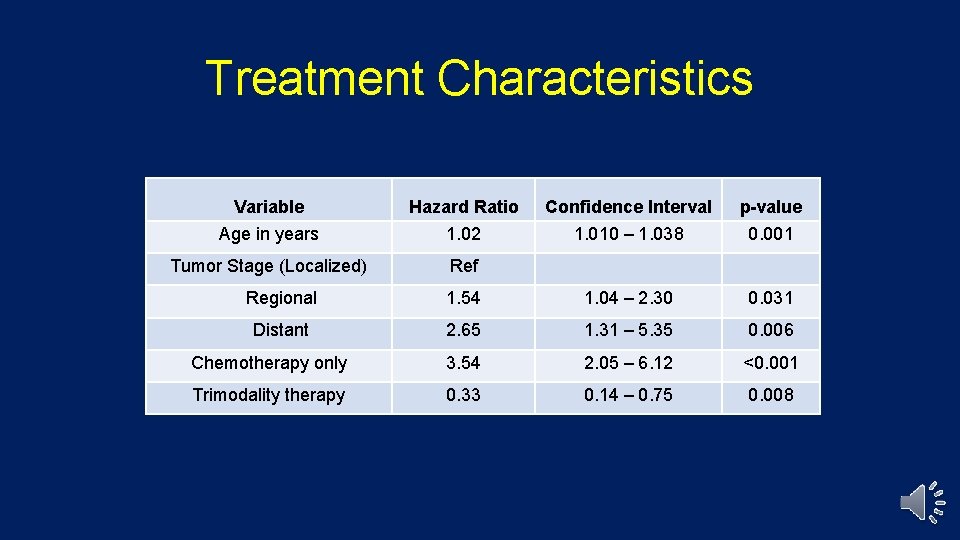
Treatment Characteristics Variable Age Variable in years Hazard Ratio 1. 02 Hazard Ratio Age in(Localized) years Tumor Stage 1. 02 Ref Tumor Stage (Localized) Regional Ref 1. 54 Confidence Interval Confidence 1. 010 Interval – 1. 038 p-value 1. 010 – 1. 038 0. 001 1. 04 – 2. 30 1. 54 1. 04 – 2. 30 0. 031 2. 65 1. 31 – 5. 35 0. 006 Chemotherapy only 3. 54 2. 05 – 6. 12 Trimodality therapy 0. 33 0. 14 – 0. 75 Distant 2. 65 p-value 0. 001 0. 031 1. 31 – 5. 35 0. 006 2. 05 – 6. 12 <0. 001 0. 14 – 0. 75 0. 008
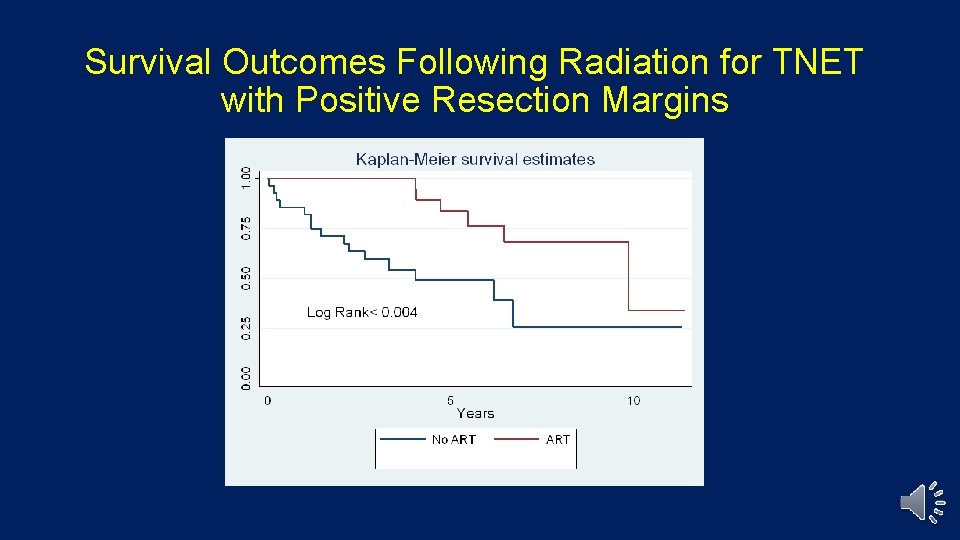
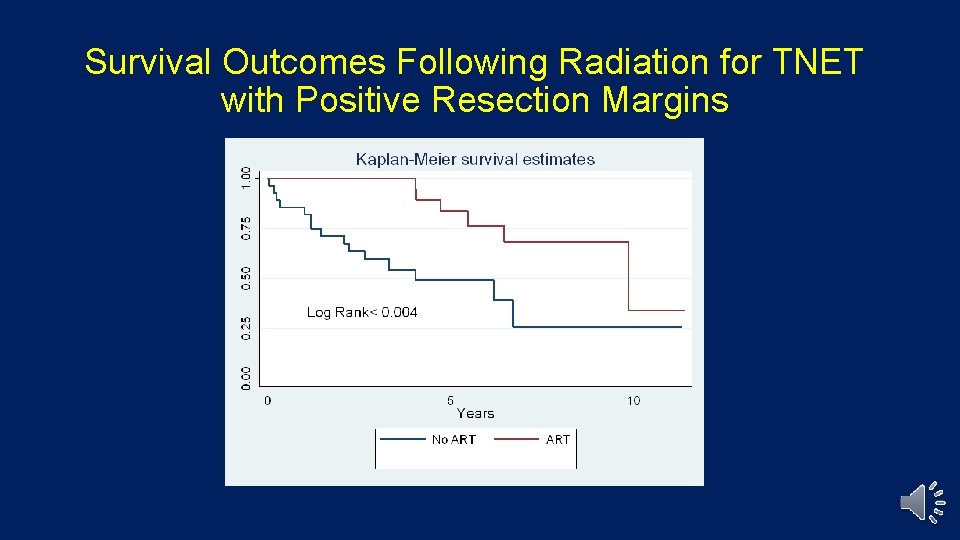
Survival Outcomes Following Radiation for TNET with Positive Resection Margins
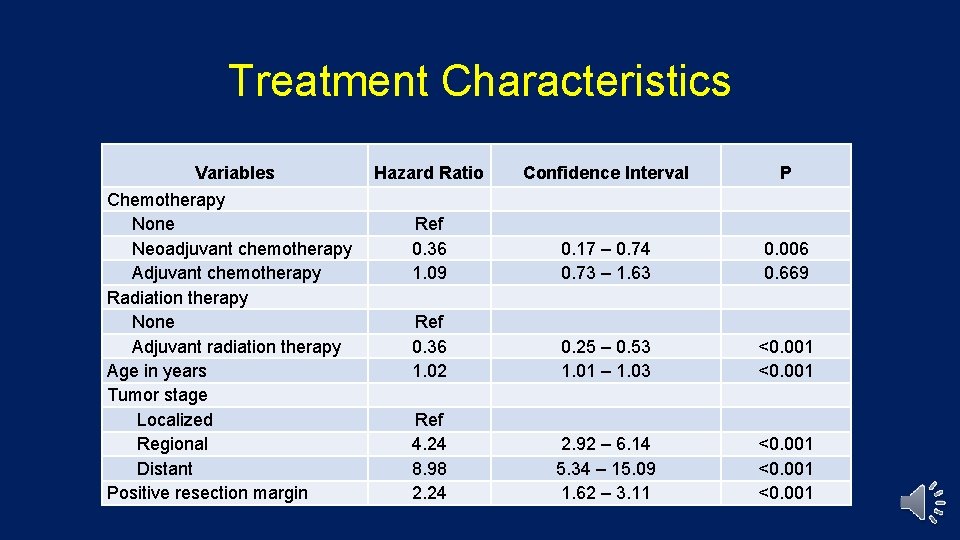
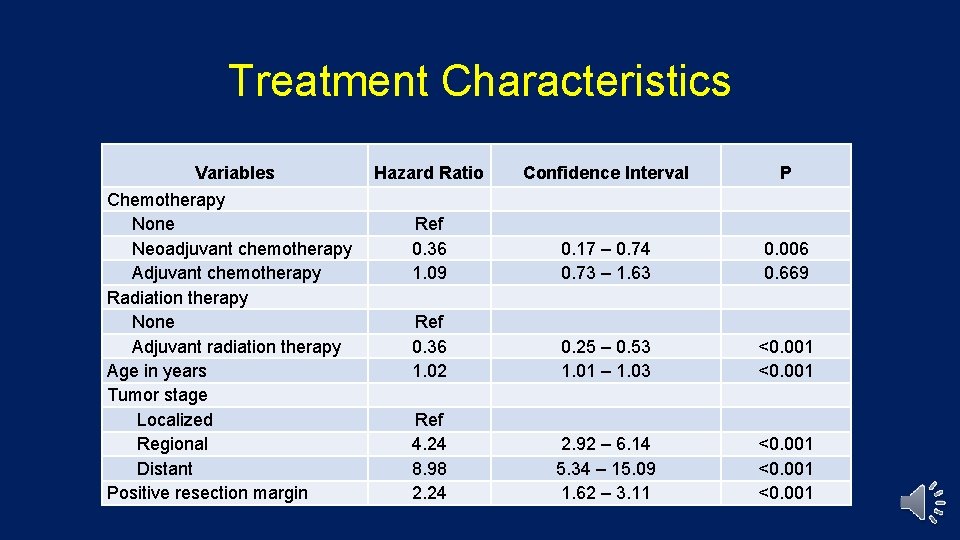
Treatment Characteristics Variables Chemotherapy None Neoadjuvant chemotherapy Adjuvant chemotherapy Radiation therapy None Adjuvant radiation therapy Age in years Tumor stage Localized Regional Distant Positive resection margin Hazard Ratio Confidence Interval P Ref 0. 36 1. 09 0. 17 – 0. 74 0. 73 – 1. 63 0. 006 0. 669 Ref 0. 36 1. 02 0. 25 – 0. 53 1. 01 – 1. 03 <0. 001 Ref 4. 24 8. 98 2. 24 2. 92 – 6. 14 5. 34 – 15. 09 1. 62 – 3. 11 <0. 001
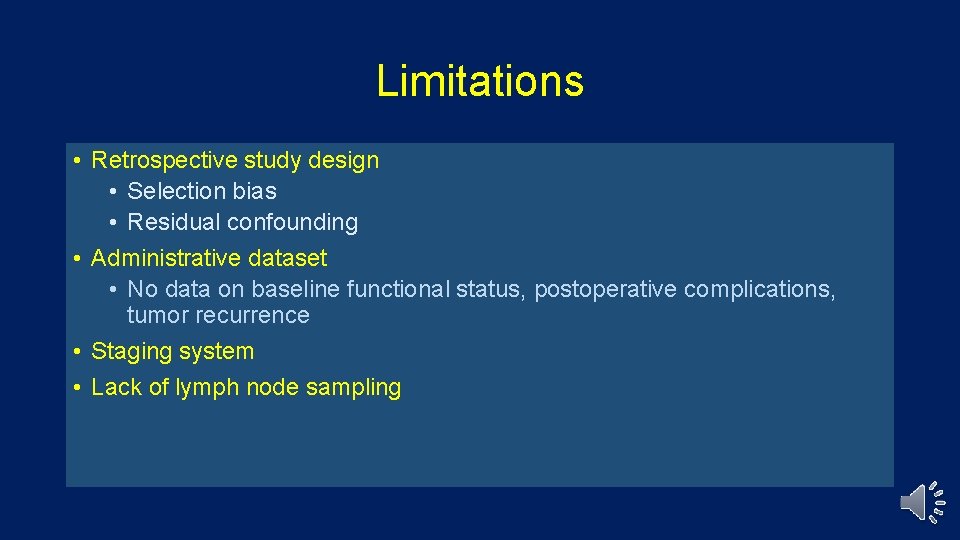
Limitations • Retrospective study design • Selection bias • Residual confounding • Administrative dataset • No data on baseline functional status, postoperative complications, tumor recurrence • Staging system • Lack of lymph node sampling
Conclusions • TNET are rare and aggressive mediastinal tumors of the thymus • Trimodality therapy is associated with improved survival • Lymph node dissection seems to be underutilized in the surgical treatment of TNET. • Adjuvant radiation is associated with improved survival for margin positive TNET. • Prospective studies are warranted to better clarify the treatment algorithm for TNET.
Thymic Neuroendocrine Tumors: Demographics, Treatment and Survival Charles T. Bakhos MD MS, Aitua Salami MD, Larry Kaiser MD, Roman V. Petrov MD Ph. D, Abbas E. Abbas MD MS
 Thymic carcinoma symptoms
Thymic carcinoma symptoms State of survival survival of the fittest tweak
State of survival survival of the fittest tweak State of survival survival of the fittest stages
State of survival survival of the fittest stages Thymic tissue
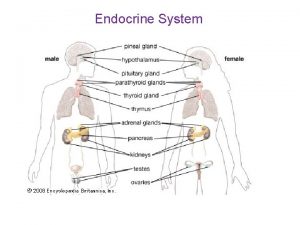
Thymic tissue Endocirne glands
Endocirne glands Malignant and benign tumors
Malignant and benign tumors Benign and malignant tumors
Benign and malignant tumors N
N Mechanisms of hypothalamic control over endocrine function
Mechanisms of hypothalamic control over endocrine function Neuroendocrine reflex
Neuroendocrine reflex Neuroendocrine syndromes in gynecology
Neuroendocrine syndromes in gynecology Strss
Strss Classification of testicular tumors robbins
Classification of testicular tumors robbins Cervical ectropion
Cervical ectropion Response evaluation criteria in solid tumors (recist)
Response evaluation criteria in solid tumors (recist) Codman üçgeni
Codman üçgeni Bone tumors
Bone tumors