The Lessons of Gainsharing Assisting Hospitals Achieve Greater

























- Slides: 25

The Lessons of Gainsharing Assisting Hospitals Achieve Greater Efficiency and Improved Quality Through Gainsharing Seton Hall Law School October 28, 2011 © Applied Medical Software, Inc, 2011. The AMS Performance Based Incentive System ® (AMS PBIS ®) are registered trademarks of Applied Medical Software, Inc. and may not be used without the prior written consent of Applied Medical Software, Inc. The AMS PBIS® is patent protected (US Patents: 7, 546, 245; 7, 640, 173; 7, 640, 174, and 7, 716, 067). . applied medical software 595 Haddon Avenue Collingswood, NJ 08108 856. 858. 3822

Fundamental Distinction § ACO: – Top down approach – New structure created – Empowered to carry out a broad array of regulatory objectives § Gainsharing – Bottom up approach – A program is implemented to respond directly to specific regulatory objectives 2 applied medical software

AMS: Applied Medical Software § Principals were the architects of the first system of payment by the case (DRG). § The original New Jersey Experiment served as the prototype for the Medicare PPS. § AMS is involved in national gainsharing initiatives. § AMS provides the gainsharing component in all but one of the current Medicare Demonstrations. § The AMS Performance Based Incentive System® for Physicians (AMS PBIS®) has received 4 patents. 3 applied medical software

Why Implement Gainsharing? § Many efforts aimed at efficiency/quality improvements underway at hospitals - BUT • Are you getting the attention and involvement needed from all physicians? • Do physicians understand how they are performing against the goals and specifically where/how they need to change in order to achieve the goals? • Is the hospital delivering the right kind of data, on a regular basis, that provides direction on where to change behavior? • Is the hospital providing any incentive to physicians to make the effort to get involved and change? 4 applied medical software

Quick, Simple Method to Align and Achieve Physician and Hospital Goals § Not complicated – achieve the goal, get rewarded § Quick start-up, payments to doctors within the year, collaboration/ improvements begin immediately § Data is readily available & accepted as valid § Flexible - adaptable to special needs of each hospital § Perfect tool in CMS/CMMI Bundled Payment Initiatives (Model 1, or as part of Models 2 -4), ACO strategy or alternative to ACO. 5 applied medical software

AMS Gainsharing Projects § NJ Physician Hospital Collaboration Medicare Demonstration § Beth Israel Medical Center Medicare Gainsharing Demonstration § Continuum Health Partners Commercial Gainsharing Program § Horizon Blue Cross/Blue Shield § Greater NY Hospital Association Commercial Gainsharing Program 6 applied medical software

CMS/CMMI Bundled Payments for Care Improvement Initiative § Announced August 23, 2011 § Four distinct models; 3 focus on acute hospital care, one on long term care. § Model 1 is most like New Jersey and New York Medicare Demonstrations – Letters of Intent (Non Binding) to develop a program due October 6 – Applications due November 18 7 applied medical software

AMS PBIS® The Methodology 8 applied medical software

AMS PBIS®: Design Principles Purpose: Recognize the important role of physicians in contributing to efficient hospital operational performance • • • Rewards achieved levels of performance. Incents improved performance. Compensates loss of income for medical admissions. Protects and maintains quality of care. Provides framework for care redesign and quality improvement. Measurement: Performance is rewarded based on regionally developed Best Practice Norms • • 25 th percentile of patient costs (patients with lowest cost) in region or system Excludes psych, normal newborns and deliveries Severity adjusted DRGs used for costing Responsible Physician/ Physician of Record is eligible • Medical cases = discharging (attending) physician • Surgical cases = surgeon of record 9 applied medical software

Major Design Decisions Minimize Operational Issues • All necessary information extracted from routinely collected data (UB 04) • Start with inpatient stay • RCC cost-finding-industry standard • Select Responsible Physician (trade offs) • No change in the current process or form of payment • Contains key quality safeguards • Uniform, auditable, replicable and easily implemented 10 applied medical software

Major Design Decisions (Cont’d) Patient Protection / Methodological • Adjustment for Severity of Illness insures correct amount of resources (eliminates incentives for “cherry picking”, “quickersicker, “stinting” and “steering”) • Best Practice Norms derived from practice in the community • Evaluation based on overall performance; no penalties related to individual case (i. e. outliers) • Incentive amounts are reasonable (consistent with Medicare PIP rules) • Limit on incentive payments to discourage new and untried practices • Physician incentives may be conditioned upon compliance with clinical quality measures specified by hospital steering committee 11 applied medical software

Securing Physician “Buy-In” The Program • Strictly voluntary • No change in form or process of payment • Provides detailed data on individual physician utilization and quality metrics, adjusted for severity of illness • Provides ongoing feedback to physicians on his/her individual performance • Encompasses non-clinical and clinical opportunities • Quality evaluation is based on overall performance, not individual cases • Incentive only/no risk or penalties, based on individual performance • Incentive awarded to responsible physician; no need to form artificial groups • Incentive can be continuous; not one time 12 applied medical software

Economic Framework § Allows hospitals to incent physicians financially for improved quality of care and improved efficiency: up to 25% of physician fees (50% under CMS Bundled Payment Initiatives), in accordance with legal/regulatory restrictions § Creates a collaborative environment where both hospital and physician incentives are aligned. § Rewards achieved level of physician performance. § Provides incentives for improved performance. § Provides loss of income protection. 13 applied medical software

Methodological Steps § Determine cost per case (ratio of cost to charges). § Classify patients into All Patient Refined Diagnosis Related Groups (APR DRGs – DRGs adjusted for Severity of Illness). § Determine Best Practice Norms. § Group patients by physician. § Measure physician performance. § Compute performance incentive and loss of income payments. 14 applied medical software

Methodology for Best Practice Norms OBJECTIVE: Assure that standards are attainable • At least ten (10) patients per physician within a product line; • At least five (5) qualifying physicians within a product line; • At least three (3) patients within an APR DRG (to adjust for casemix and severity of illness); and • If the above criteria are met, the Best Practice Norm is set at 25 th percentile of patient cost (patients with the lowest cost). 15 applied medical software

Sample Practice Changes that Contributed to Improve Efficiency and Quality of Care § Increased detail/accuracy and timeliness of documentation § Earlier consultation with Discharge Planner § Round/writing discharge order prior to noon and increase discharges on weekends § Increase understanding/interest in implant costs and implementation of demand matching § Decrease time between request for consultation and occurrence of consultation § Earlier transition from ICU to standard acute floor 16 applied medical software

NJ Medicare Demo - 12 hospitals 3 Payment Period Results (18 months) 1, 300 physicians – 76, 226 Medicare admissions § $38, 590, 485 cumulative savings, $540 or 5. 6% per admission § “Leverage”: ratio of incentives paid to cumulative savings is approximately 1 to 4. 5 § Four hospitals achieved savings per admission in excess of 12% § Five hospitals were between 9. 8% and 7. 3% § Three hospitals were under 2%, but showing positive trends NOTE: The statements contained in this document are solely those of AMS and do not necessarily reflect the views or policies of CMS. 17 applied medical software

AMS PBIS® Sample Reports 18 applied medical software

Physician Incentives Improvement • An individual physician’s performance compared to his/her own performance over time – base year (e. g. 2009) to rate year. * Performance • An individual physician’s performance compared to his/her peers – Best Practice Norm. * *All computations are adjusted for case-mix, severity of illness and inflation. 19 applied medical software

20

21

Savings Opportunities by Physician 22 applied medical software

23

24

Contacts Michael Kalison, Esq. Chairman Applied Medical Software 908. 647. 4600 mkalison@kmjhlaw. com Jo Surpin President Applied Medical Software 856. 858. 3822 ext 205 jsurpin@appliedmedicalsoftware. com 25 applied medical software
 Gainsharing definition
Gainsharing definition Scanlon plan
Scanlon plan Chapter 41 assisting in geriatrics
Chapter 41 assisting in geriatrics Chapter 42 assisting in other medical specialties
Chapter 42 assisting in other medical specialties Chapter 5 assisting with the nursing process
Chapter 5 assisting with the nursing process The adaa was formed in 1924 by:
The adaa was formed in 1924 by: Chapter 38 assisting with a general physical examination
Chapter 38 assisting with a general physical examination Chapter 31 assisting in a medical emergency
Chapter 31 assisting in a medical emergency Rop santa cruz
Rop santa cruz Pearson's comprehensive medical assisting
Pearson's comprehensive medical assisting Chapter 6 general anatomy
Chapter 6 general anatomy Assisting in microbiology and immunology
Assisting in microbiology and immunology Welcoming and greeting the guest procedure
Welcoming and greeting the guest procedure Chapter 42 assisting in other medical specialties
Chapter 42 assisting in other medical specialties Chapter 41 assisting in geriatrics
Chapter 41 assisting in geriatrics Verb form of advertisement
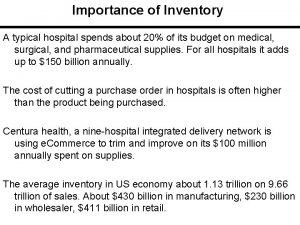
Verb form of advertisement Inventory cycle time
Inventory cycle time Arogyakiranam
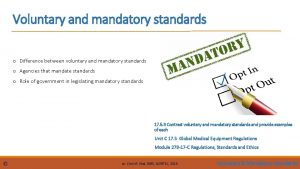
Arogyakiranam Dnv niaho standards
Dnv niaho standards Voluntary standards are known as
Voluntary standards are known as Portsmouth hospitals nhs trust jobs
Portsmouth hospitals nhs trust jobs Simon sheppard nhs birmingham
Simon sheppard nhs birmingham Graban lean hospitals download
Graban lean hospitals download Ipsg
Ipsg Process governance
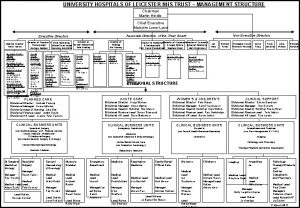
Process governance University hospitals
University hospitals