The legal and ethical aspects of working with






- Slides: 39
The legal and ethical aspects of working with information about medicines Angela Emerson Wessex Regional Drug and Medicines Information Centre
Aim n To be able to make decisions taking into account legal and ethical considerations when working with information about medicines.
Objectives n By the end of this session you will be able to: – Handle ethical dilemmas in MI – Describe key legislation that impacts upon MI practice
Decision-making process n Ethical n Legal n Professional n Organisational
Ethical constraints n What are ethics…. . – A code of behaviour considered correct, especially of a profession or individual. – They are moral principles or values held by an individual or group.
Ethical theories n Consequence-based approach – The consequences of what we do matter…but matter to whom? – Lying is wrong because of the negative consequences it may cause but in certain circumstances it may be okay n Rule-based approach (aka deontology) – The rules matter – Lying is always wrong, regardless of any potential good
Ethical decision-making n Recognises problem needs to be solved or difficult choice made n Identifies the possible courses of action n Chooses and takes one course of action n Accepts responsibility for the action taken and the outcomes which are a result of the choices made
Ethical decision-making in MI n How long does it take for cannabis to leave the body? n Enquirer going for a job interview tomorrow.
Ethical decision-making in MI n Many situations faced are unambiguous – the decision will be obvious n Often a conflict between your job (providing information) and duty to another person n Different MIPs may reach different decisions in same circumstances
Ethical decision-making in MI n In practice most arise from members of the public n May also arise from police, media, legal representatives n Often not perceived as an ethical dilemma from the enquirer’s perspective
General principles n You do not have to answer every question that you are asked – how to say ‘no’ n Always give yourself appropriate thinking time n Consult with an appropriate colleague and/or manager before answering
General principles n There is no one “right” answer to most dilemmas but you should be able to justify what you do n Do not answer queries that are beyond you sphere of expertise or resources n Research you answers thoroughly and document everything you do
Guidance n General – Medicines, Ethics & Practice Guide: A guide for pharmacists • Act in the interest of patients and other members of the public • Ensure knowledge, skills and practice are up to date • Demonstrate integrity and probity, adhere to accepted standards of conduct and do not bring the profession into disrepute n Specific – UKMI Guidance • Police, media, third party, legal proceedings etc.




Constraints n Ethical n Legal n Professional n Organisational

Legal considerations Data Protection Act (DPA) 1998 n Common Law of Confidentiality n Human Rights Act 1998 n n Medicines Act 1968 and off/unlicensed medicines n Malpractice Law
Working with information n Justification for observing confidence n The obligation of confidence – Negligence and professional misconduct – Exceptions (patient consent, need to know [vs. curiosity], threat to others, public debate and press freedom [health professionals with HIV]) DPA 1998 n Common Law of Confidentiality n Human Rights Act 1998 n n Caldicott Guardians
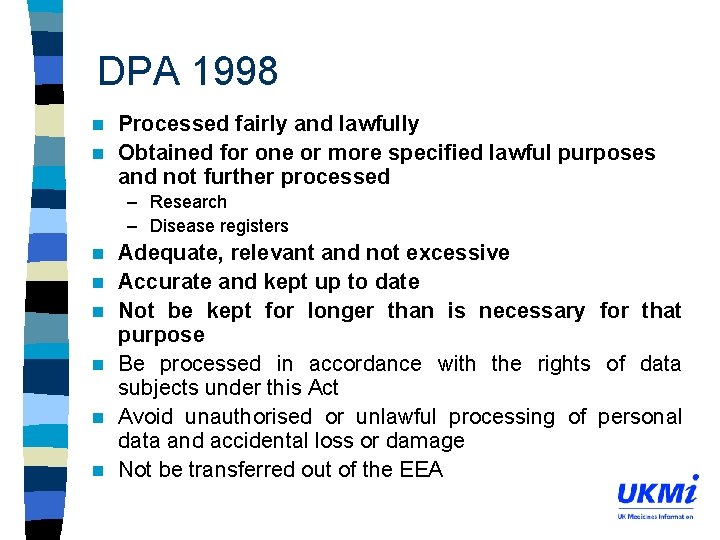
DPA 1998 n DPA 1998 effective from March 2000. n Provides a framework that governs the processing of personal data of the living. n Seeks to strengthen the individual’s right to privacy in terms of data processing by applying 8 principles.
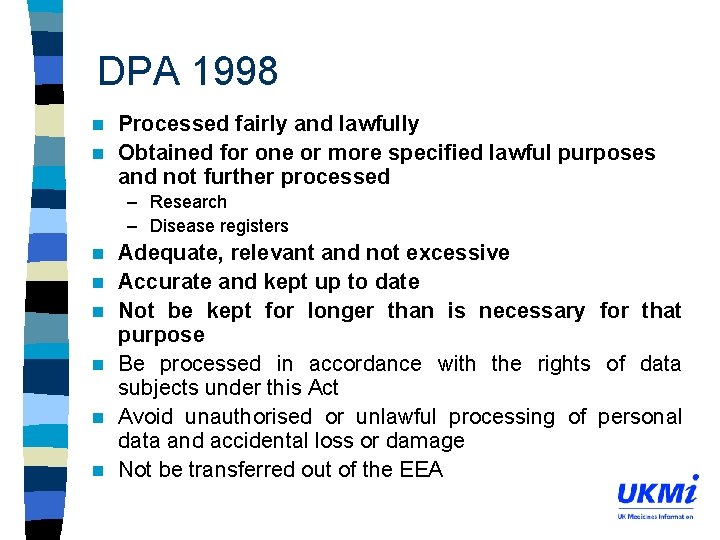
DPA 1998 Processed fairly and lawfully n Obtained for one or more specified lawful purposes and not further processed n – Research – Disease registers n n n Adequate, relevant and not excessive Accurate and kept up to date Not be kept for longer than is necessary for that purpose Be processed in accordance with the rights of data subjects under this Act Avoid unauthorised or unlawful processing of personal data and accidental loss or damage Not be transferred out of the EEA
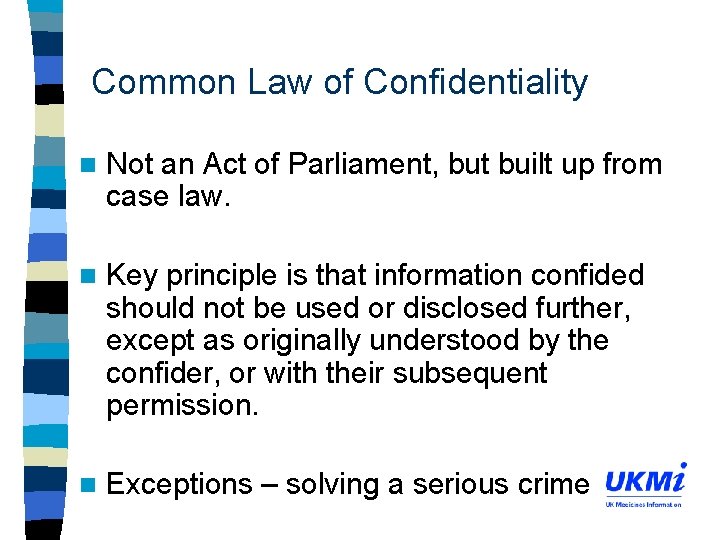
Common Law of Confidentiality n Not an Act of Parliament, but built up from case law. n Key principle is that information confided should not be used or disclosed further, except as originally understood by the confider, or with their subsequent permission. n Exceptions – solving a serious crime
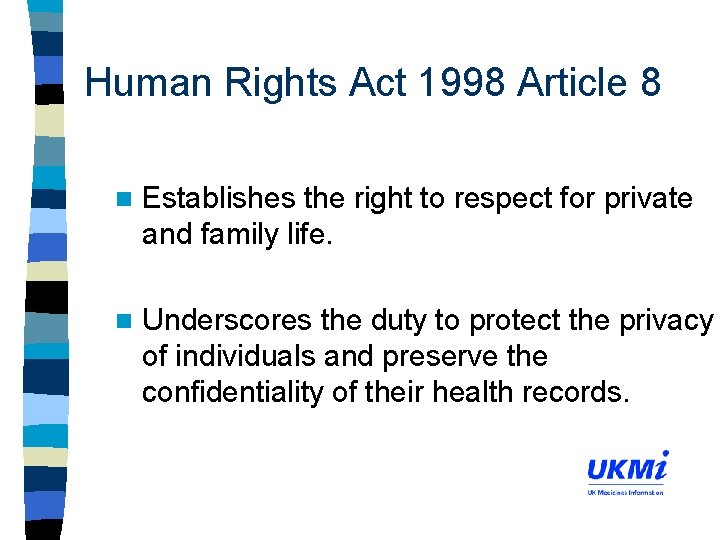
Human Rights Act 1998 Article 8 n Establishes the right to respect for private and family life. n Underscores the duty to protect the privacy of individuals and preserve the confidentiality of their health records.
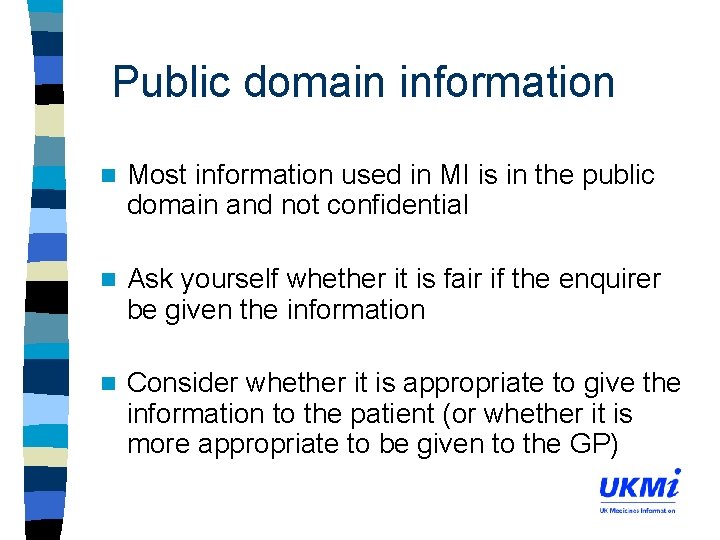
Public domain information n Most information used in MI is in the public domain and not confidential n Ask yourself whether it is fair if the enquirer be given the information n Consider whether it is appropriate to give the information to the patient (or whether it is more appropriate to be given to the GP)
Freedom of Information Act 2000 n The Act gives right to access information held by public bodies including the NHS n If patients wish to obtain information about themselves then the DPA 1998 applies. n If the information is not about them but about a public authority then the FOI applies.
Working with off/unlicensed medicines n Off-licence n Medicines vs unlicensed Act 1968 and off/unlicensed drug use n Liability and unlicensed drugs – Strict liability or fault (negligent) liability
Working with off/unlicensed medicines – Tell the patient about known ADRs and that there may be other unknown ADRs – Tell the patient about that the drug/dose/indication is not licensed by the authorities – Reassure yourself that the body of opinion supports the use of the drug in these circumstances – Keep detailed records (eg in notes) surrounding decision to use – Review the patient regularly to assess benefit and ADRs

Working with copyright n Centrally negotiated NHS copyright agreement with CLA (www. cla. co. uk) n All NHS personnel n Breaching copyright is a legal offence and it is your responsibility to keep within the law.
When things go wrong – Malpractice Law n Malpractice litigation serves several functions – Seeking apologies and being held accountable – Incentive to HCPs to maintain a high standard of care – Retribution against HCPs (civil vs criminal) – Compensation
When things go wrong – Malpractice Law n Majority of malpractice cases brought under the law of negligence n 3 key factors must be proved – Duty of care – Failed to reach the standard required by the law, that is a standard acceptable to their peers – Injuries were due to the failure to practice properly and not another unrelated accident – the ‘but for’ test
When things go wrong – Malpractice Law Bolam v Friern Hospital Committee 1957 A person is not negligent if they acted in accordance with accepted practice at the time as decided by a responsible body of competent professional opinion.
When things go wrong – Malpractice Law n RPSGB Code of Ethics requires professional indemnity arrangements n NHS hospital pharmacists covered under the clinical negligence funding scheme for contracted duties. n Ensure job descriptions up-to-date
Constraints n Ethical n Legal n Professional n Organisational
Professional constraints Overlaps with legal and ethical constraints n Principal functions of professional bodies n – Maintain a register of qualified practitioners – Remove those unfit to practise due to ill health or misconduct – Oversee professional education – Give guidance on professional ethics n Self-regulation vs external accountability
Constraints n Ethical n Legal n Professional n Organisational
Organisational constraints n Overlaps n Check for with legal constraints if your Centre/Trust has a policy – Enquiries from the media – Enquiries involving legal proceedings (including those against your own Trust) – Enquiries from the police
Workshop n 5 groups of 5 -6 n 20 minutes n Feedback
Learning outcomes n By the end of this session you will be able to: – Handle ethical dilemmas in MI – Describe key legislation that impacts upon MI practice
 Chapter 3 legal and ethical issues
Chapter 3 legal and ethical issues Professional issues in cyber security
Professional issues in cyber security Ethical media issues
Ethical media issues Legal aspects of catering premises
Legal aspects of catering premises Mario full screen
Mario full screen Legal aspects of doing business in canada
Legal aspects of doing business in canada Irving isd v tatro
Irving isd v tatro Legal aspects of advertising
Legal aspects of advertising Legal aspects of project management
Legal aspects of project management Legal aspects of community health
Legal aspects of community health Legal aspects of nursing documentation
Legal aspects of nursing documentation Legal issues in nursing documentation
Legal issues in nursing documentation Legal aspects definition
Legal aspects definition The perceived relevance or importance of an ethical issue
The perceived relevance or importance of an ethical issue Legal and ethical issues in use of ict
Legal and ethical issues in use of ict Dho chapter 5 legal and ethical responsibilities
Dho chapter 5 legal and ethical responsibilities Legal and ethical issues in e commerce
Legal and ethical issues in e commerce Legal and ethical issues in computer security
Legal and ethical issues in computer security Ethical and legal issues involved in practicum
Ethical and legal issues involved in practicum Chapter 2 ethical and legal issues
Chapter 2 ethical and legal issues Chapter 3 medical legal and ethical issues
Chapter 3 medical legal and ethical issues Chapter 3 ethical and legal issues
Chapter 3 ethical and legal issues Legal and ethical responsibilities chapter 5
Legal and ethical responsibilities chapter 5 Chapter 5 legal and ethical responsibilities answer key
Chapter 5 legal and ethical responsibilities answer key Attack sophistication vs intruder technical knowledge
Attack sophistication vs intruder technical knowledge Legal and ethical issues chapter 5
Legal and ethical issues chapter 5 Legal and ethical issues chapter 3
Legal and ethical issues chapter 3 Chapter 4 legal and ethical responsibilities
Chapter 4 legal and ethical responsibilities Legal and ethical responsibilities of a coach
Legal and ethical responsibilities of a coach Chapter 6 legal and ethical issues
Chapter 6 legal and ethical issues Chapter 5 legal and ethical responsibilities
Chapter 5 legal and ethical responsibilities Ethical and legal issues chapter 2
Ethical and legal issues chapter 2 Ethical and legal issues chapter 2
Ethical and legal issues chapter 2 Chapter 5 legal and ethical responsibilities worksheet
Chapter 5 legal and ethical responsibilities worksheet Ethical and legal issues affecting the nursing assistant
Ethical and legal issues affecting the nursing assistant What is the difference between ethical and legal issues
What is the difference between ethical and legal issues What ishipaa
What ishipaa Legal and ethical issues chapter 5
Legal and ethical issues chapter 5 Chapter 2 ethical and legal issues
Chapter 2 ethical and legal issues Legal and ethical environment of business
Legal and ethical environment of business