Chapter 2 Ethical and Legal Issues Roosevelt Health






- Slides: 39
Chapter 2: Ethical and Legal Issues Roosevelt Health Science Clinical Rotations Successful Nursing Assistant Care, 2 nd Ed. (Ch. 2) Simmers DHO Health Science, 8 th ED. (Ch. 5) Medical Assisting: Administrative & Clinical Competencies, 7 th ED (Unit 4, 5)
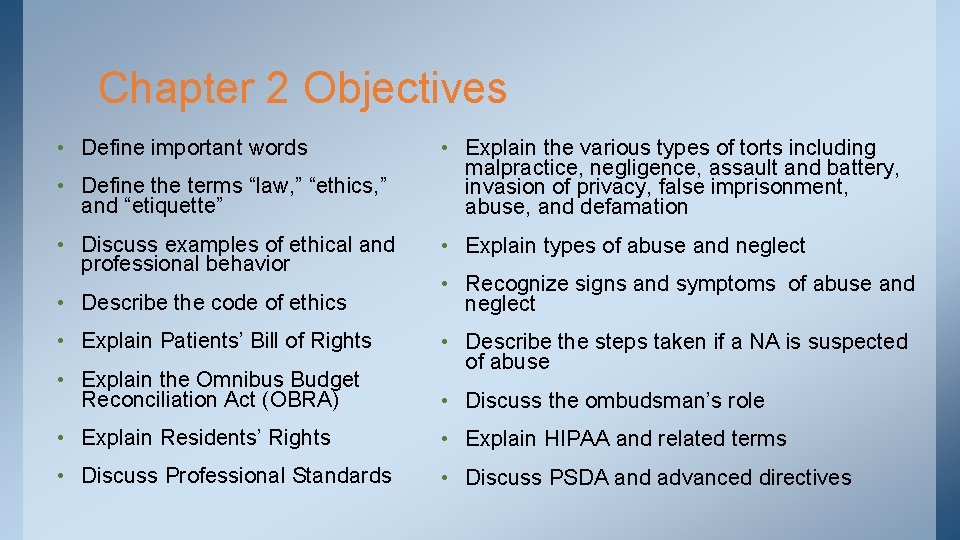
Chapter 2 Objectives • Define important words • Define the terms “law, ” “ethics, ” and “etiquette” • Discuss examples of ethical and professional behavior • Explain the various types of torts including malpractice, negligence, assault and battery, invasion of privacy, false imprisonment, abuse, and defamation • Explain types of abuse and neglect • Describe the code of ethics • Recognize signs and symptoms of abuse and neglect • Explain Patients’ Bill of Rights • Describe the steps taken if a NA is suspected of abuse • Explain the Omnibus Budget Reconciliation Act (OBRA) • Discuss the ombudsman’s role • Explain Residents’ Rights • Explain HIPAA and related terms • Discuss Professional Standards • Discuss PSDA and advanced directives
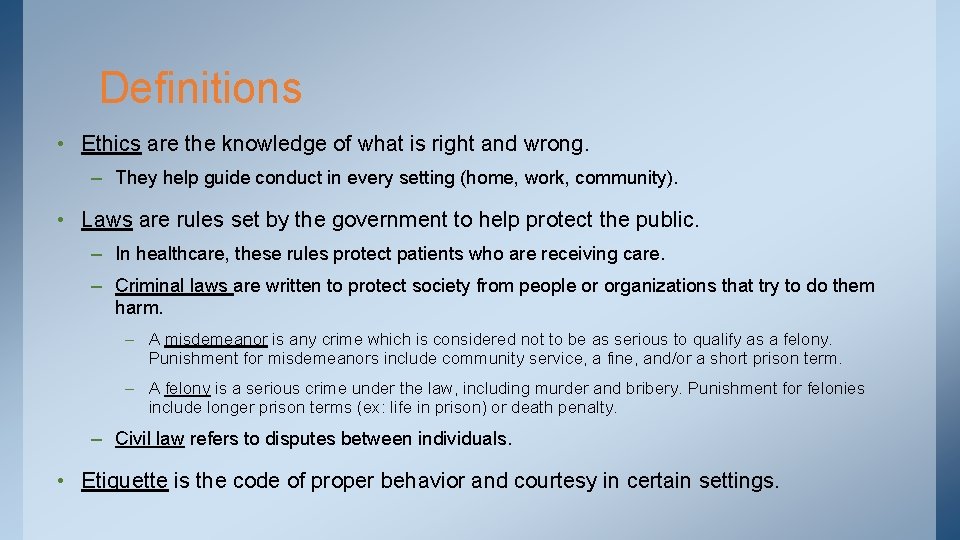
Definitions • Ethics are the knowledge of what is right and wrong. – They help guide conduct in every setting (home, work, community). • Laws are rules set by the government to help protect the public. – In healthcare, these rules protect patients who are receiving care. – Criminal laws are written to protect society from people or organizations that try to do them harm. – A misdemeanor is any crime which is considered not to be as serious to qualify as a felony. Punishment for misdemeanors include community service, a fine, and/or a short prison term. – A felony is a serious crime under the law, including murder and bribery. Punishment for felonies include longer prison terms (ex: life in prison) or death penalty. – Civil law refers to disputes between individuals. • Etiquette is the code of proper behavior and courtesy in certain settings.
How can you show ethical behavior as a healthcare provider?
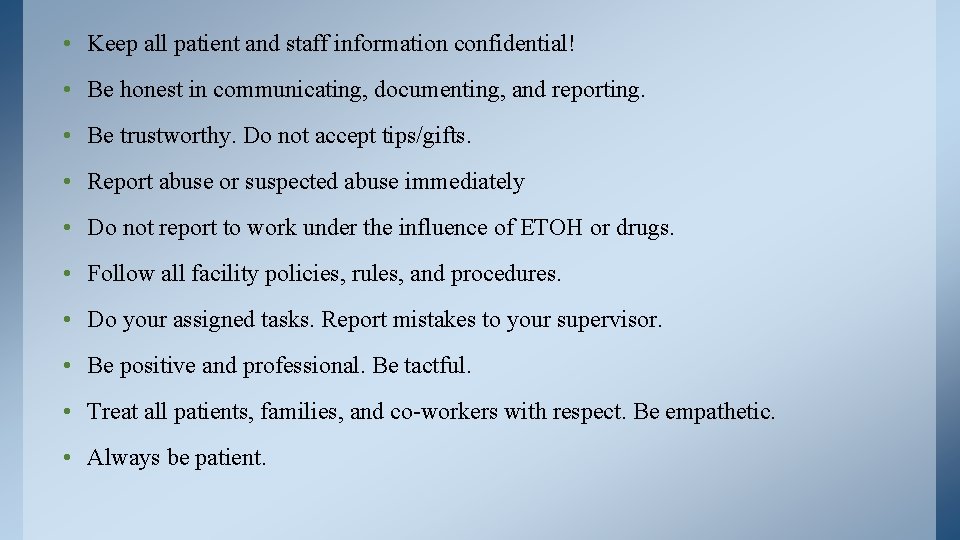
• Keep all patient and staff information confidential! • Be honest in communicating, documenting, and reporting. • Be trustworthy. Do not accept tips/gifts. • Report abuse or suspected abuse immediately • Do not report to work under the influence of ETOH or drugs. • Follow all facility policies, rules, and procedures. • Do your assigned tasks. Report mistakes to your supervisor. • Be positive and professional. Be tactful. • Treat all patients, families, and co-workers with respect. Be empathetic. • Always be patient.
Ethics • Legal responsibilities are determined by law. Ethics are a set of principles relating to what is morally right or wrong. • Ethics provide a standard of conduct or code of behavior, so that a healthcare provider can analyze information and make decisions based on what people believe is right and good conduct. • All medical professions have a Code of Ethics, a set of guidelines adopted by a profession to regulate that profession.
As modern healthcare advances, many ethical dilemmas for healthcare providers… Is euthanasia (assisted suicide) justified in certain patients? Should a patient be told that a healthcare provider has HIV/AIDS?

Should aborted fetuses be used for research? Do parents have a religious right to refuse a life-saving blood transfusion for their child? Can a healthcare facility refuse to provide expensive treatment such a bone marrow transplant if a patient cannot pay for the treatment? Should people be allowed to sell organs for use in transplants?

If a person can benefit from marijuana, should a physician be allowed to prescribe it as a treatment? Should animals be used in medical research even if it results in the death of the animal? Should aborted embryos be Should human beings used to obtain stem cells be cloned? for research, especially since scientists may be able Should genetic researchers to use stem cells to cure be allowed to transplant diseases such as diabetes, specific genes to create the osteoporosis, and “perfect” human being? Parkinson’s?
Patients’ Rights • Federal and state legislation requires healthcare agencies to have written policies regarding patients’ rights, or the factors of care that patients can expect to receive. – Agencies expect all personnel to respect and honor these rights. • The American Hospital Association has affirmed a Patients’ Bill of Rights that is recognized and honored by many healthcare facilities. • This bill of rights states, in part, that a patient has the right to: – Considerate and respectful care – Obtain complete, current information concerning diagnosis, treatment, and prognosis, – Receive information necessary to give informed consent prior to the start of any procedure or treatment.

Patients’ Rights • Patients’ Bill of Rights continued – Have advanced directives for health care and/or refuse treatment to the extent permitted under law – Privacy concerning a medical care program – Confidential treatment of all communications and records – A reasonable response to a request for services – Obtain information regarding any relationship of the hospital to other healthcare and educational institutions – Be advised of and have the right to refuse to participate in any research project – Expect reasonable continuity of care – Review medical records and examine bills and receive an explanation of all care and charges – Be informed of any hospital rules, regulations, and/or policies and the resources available to resolve disputes or grievances.
Omnibus Budget Reconciliation Act (OBRA) • Passed in 1987 in order to set minimum standards of care, including standardizing training of CNAs. – Created in response to poor care, bad conditions, and abuse in nursing homes. • As of 2013 in Texas, CNAs must complete 100 hours to sit for skill and written certification exams. 60 hours of classroom material, 40 hours of clinical training. – Basic requirements from OBRA include 75 hours total for training. • OBRA requires that – CNAs attend regular in-service education – CNAs to be registered with the state. – Nursing home meet designated minimum staff requirements – Complete assessments on every resident (MDS) – Nursing homes allow for Residents’ Rights

Residents’ Rights • Residents’ Rights specify how residents must be treated while living in a facility. • Every long-term care facility must inform residents or their guardians of these rights and a copy must be posted in each facility. • They include: – Free choice regarding physician, treatment, care, and participation in research – Freedom from abuse and chemical or physical restraints – Privacy and confidentiality of personal and clinical records – Accommodation of needs and choice regarding activities, schedules, and health care – Voice grievances without fear of retaliation or discrimination – Organize and participate in family/resident groups and in social, religious, and community activities
Residents’ Rights • Residents’ Rights continued: – Information on medical benefits, medical records, survey results, deficiencies of the facility, and advocacy groups including the ombudsman program – Manage personal funds and use personal possessions – Unlimited access to immediate family or relatives and to share a bedroom with his or her spouse, if both are residents – Remain in the facility and not be transferred or discharged except for medical reasons, the welfare of the resident or others, failure to pay, or if the facility either cannot meet the resident’s needs or cease to operate • All states have adopted these rights, and some have added additional rights. • Health care workers can face job loss, fines, and even imprisonment if they do not follow and grant established patients’ or residents’ rights.
Professional Standards • All professions have professional standards that are set to protect yourself, your employer, and the patient • Basic standards include: – Perform only those procedures for which you have been trained and are legally permitted to do. – Use approved, correct methods while performing any procedure – Obtain proper authorization before performing any procedure – Identify the patient – Obtain the patient’s consent before performing any procedure – Observe all safety precautions – Think before you speak and carefully consider everything you say – If any error occurs or you make a mistake, report it immediately to your supervisor – Behave professionally in dress, language, manners, and actions
Scope of Practice • The scope of practice describes the procedures, actions, and processes that a healthcare practitioner is permitted to undertake in keeping with the terms of their professional license. – RNs can perform medical assessments, obtain specimen for testing, implement treatments but cannot diagnose patients or prescribe medications – ATs can perform medical assessments, design rehabilitation for injuries, perform manipulations and joint mobilizations but cannot relocate a dislocated shoulder or perform surgery – In some states a paramedic is allows to perform a percutaneous cricothyrotomy if all other airway management fails. • Know your scope of practice, and do not perform anything beyond your level of training according to the law!
Torts • A tort is a wrongful act that does not involve a contract, sometime called a civil wrong instead of a crime. • A tort occurs when a person is harmed or injured because a health care provider does not meet the established or expected standards of care. • Common torts include: – Malpractice: the failure of a professional to use the degree of skill and learning commonly expected in that individual’s profession, resulting in injury, loss, or damage to the person receiving care. – Negligence: failure to give care that is normally expect of a person in a particular position, resulting in injury to another person. – Active neglect: purposely harming a person physically, mentally, or emotionally by failing to provide needed care. – Passive neglect: unintentional harming a person physically, mentally, or emotionally by failing to provide needed care.
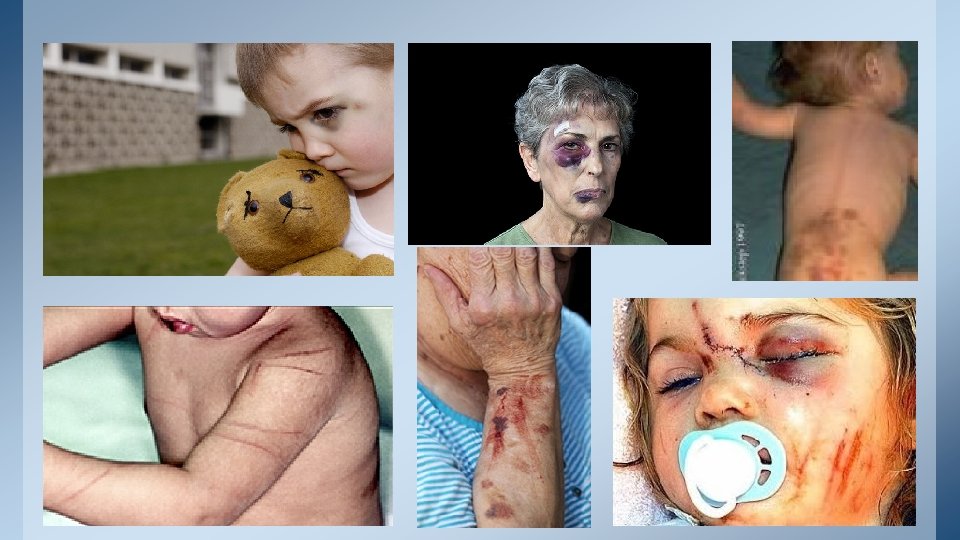
Torts • More common torts include: – Assault and battery: assault includes a threat or attempt to injure, and battery includes the unlawful touching of another person without consent. – Invasion of privacy: includes physical and informational. Physical invasion of privacy includes unnecessarily exposing an individual, while informational refers to revealing personal information about the individual without that person’s consent. – False imprisonment: refers to restraining or restricting an individual’s freedom without authorization. Ex: keeping patient against their will or applying physical restraints without proper authorization or with no justification. – Abuse: includes any care that results in physical harm, pain, or mental anguish. Examples of types of abuse include: – Physical abuse: hitting, forcing people against their will, restraining movement, depriving people of food or water, and/or not providing physical care.
Torts • More common torts include: – Verbal abuse: speaking harshly, swearing or shouting, using inappropriate words to describe a person’s race or nationality, and/or writing threats or abusive statements. – Psychological abuse: threatening harm; denying rights; belittling, intimidating, or ridiculing the person; and/or threatening to reveal information about the person. – Sexual abuse: any sexual touching or act, using sexual gestures, and/or suggesting sexual behavior, even if the patient is willing or tries to initiate it. ***Patients may experience abuse before entering a healthcare facility, such as domestic abuse, child abuse, or elder abuse. – Defamation: occurs when false statements either cause a person to be ridiculed or damage the person’s reputation. Incorrect information given out in error can result in defamation. – If the information is spoken, it is called slander. – If the information is written, it is known as libel.
Torts- Keys to Remember • Patients must give consent for any care, and they have the right to refuse care. – Some procedures or practices require written consent from the patient, such as surgery or experimental procedures. Verbal consent is permitted in other cases, but the law states that this must be “informed consent. ” – Informed consent is permission granted voluntarily by a person who is of sound mind after the procedure and all risks involved have been explained in terms the person can understand. • Patients have the right to leave a hospital or health care facility without a physician’s permission. If this happens, the patient is usually asked to sign an AMA form. • Physical restraints should be used only to protect patients from harming themselves or others and when all other measures to control the situation have failed. – A physician’s order must be obtained before they are used, and strict guidelines must be observed while they are in use. • Healthcare workers are required by law to immediately report any signs and symptoms of abuse to their immediate supervisor.
S/SX of Abuse (physical) • Unexplained broken bones • Unexplained bruising • Unexplained weight loss, extremely dry and cracked skin, or signs of dehydration • Similar injuries that occur over and over, such as an injury shaped like a belt buckle • Missing hair • Burns shaped in certain ways, like a cigarette burn or a burn caused by an iron • Blood in underwear • Bite marks or scratches • Broken or missing teeth • Bruising in the genital area
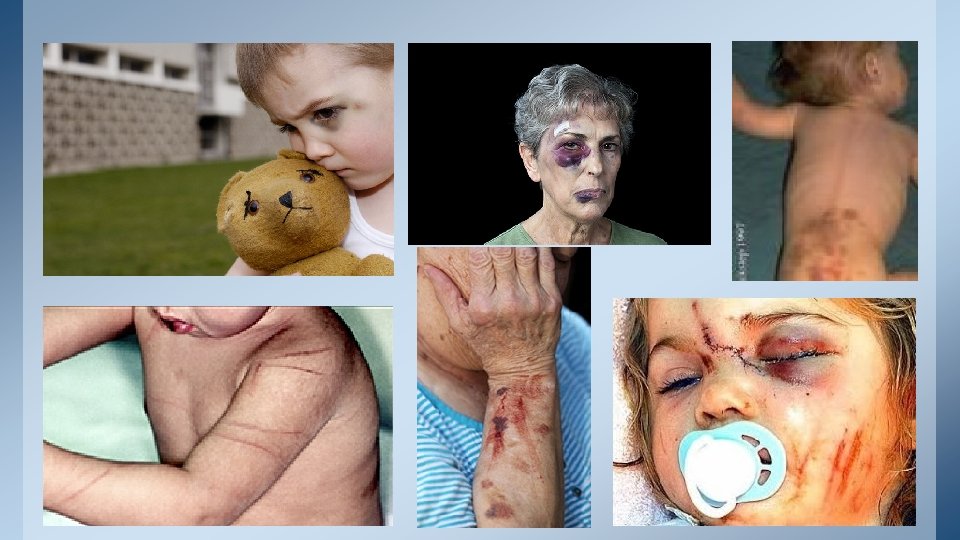
S/SX of Abuse (psychological) • Depression or withdrawal • Mood swings • Aggressive behavior • Fear and anxiety, especially when a certain caregiver is present • Lack of appetite • Fear of being left alone • Irrational fears or a change in personality

S/SX of Neglect • Sores on the body • Ragged or dirty fingernails • Weight loss or signs of dehydration • Soiled clothes or bed linens • Frequent complaints of hunger or thirst • Ripped or torn clothing • Strong smell of urine • Damaged or poorly-fitting hearing aids, glasses, or dentures • Unclean body • Unanswered call lights • Dirty, matted, or unstyled hair
Other S/SX of Abuse • Missed doctor’s appointments • Changing doctors frequently • Wearing makeup or sunglasses to hide injuries • Family concern that abuse is occurring • Person does not seem to be taking his medication • Caregiver does not allow anyone to be alone with the patient.

What happens if a healthcare worker is suspected of abuse?
Handling Suspected Abuse • Immediate suspension • Notification of certifying or licensing body, as well as facility administrator. • A full, confidential investigation is done. • There may be a hearing, decision of the hearing and an appeal process if the investigation find merit in the accusations. • Nursing and nursing assistants have an abuse registry, shared among states. Employers check this registry before hiring.
Ombudsman’s Role • In nursing homes in the United States, an ombudsman is the legal advocate for residents. • The ombudsman visits the facility and listens to residents. – He/she will decide what course of action to take if there is a problem, help settle disputes and resolve conflict. • The is an ongoing presence in nursing homes to monitor care and conditions by the ombudsman.
Ombudsman’s Role • Typical duties performed by an ombudsman: – Advocates for Residents’ Rights and quality care – Educates consumers and care providers – Investigates and resolves complaints; works with investigators from the police, adult protective services, and health departments – Appears in court and/or in legal hearings – Give information to the public • There also state agencies that can assist people with concerns about a facility. – State Department of Health and the State Department of Health and Human Services
Health Insurance Portability and Accountability Act (HIPAA) • HIPAA was passed in 1996, as law written to protect the privacy of health information. • It identifies Protected Health Information that must remain confidential. – PHI is information that can be used to identify a person and relates to the patient’s past, present, or future physical or mental condition; any health care that patient has had; or payment for that health care. – PHI includes the patient’s name, address, telephone number, medical record, social security number, e-mail address, and other information. – MUST REMAIN SECURE AT ALL TIMES • HIPAA applies to all healthcare providers, including MD/DO, RN/BSN, LVN/LPN, PT, OT, AT, CNA, EMT, etc.
Health Insurance Portability and Accountability Act (HIPAA) • HIPAA regulations in the Privacy Rule require every healthcare provider to inform patients about how their health information is used. • Patients must sign a consent form ascertaining that they have received information before any healthcare provider can use health information for diagnosis, treatment, billing, insurance claims, or quality of care assessments. • Before a health care provider can release information to anyone else, such as another healthcare provider, attorney, insurance company, federal or state agency, or even other members of the patient’s family, a patient must sign an authorization form for the release of this information. – This authorization form must identify the purpose or need for the information, the extent of the information that may be released, any limits on the release of information, date of authorization, and signature of a person authorized to give consent.
Health Insurance Portability and Accountability Act (HIPAA) • Never share any protected information with anyone who is not directly involved in the patient’s care. • If a friend asks you about a patient’s condition, the correct response is “I cannot share that information. It is confidential. ” • Some ways to keep information confidential are: – Do not give out health information on the phone unless you know you are speaking with an approved staff member. – Do not give any personal information to any visitors, no matter who they are. – Never share a medical record with anyone other than staff members directly involved in the resident’s care. – Double check fax numbers before faxing information. Use a cover sheet. – Return charts to their proper place after use.
Exceptions to HIPAA • The only exceptions to these regulations is for the release of information on diseases or injuries that must be reported by law to protect the safety and welfare of the public. • Exceptions include births, deaths, injuries caused by violence that require police involvement, communicable disease, and sexually transmitted diseases. – Communicable diseases can be spread. – Infectious diseases designated as notifiable include, but are not limited to: – Anthrax, West Nile virus, Cholera, Dengue fever, Diphtheria, Gonorrhea, Hepatitis A, B, C, HIV, Listeriosis, Lyme disease, Malaria, Measles, Mumps, Whooping cough, Plague, Polio, Rubella, Smallpox, Syphilis, Tetanus, TB, Typhoid fever, VRSA, MRSA, Varicella, Ebola, etc.
Patient Self-Determination Act (PSDA) • Federal law passed in 1990, encourages people to make decisions about advance directives. – Advanced Directives are written documents or oral statements that allow people to decide what kind of medical care they wish to have if they are unable to make those decisions themselves. – It can also designate someone else to make medical decisions for a person if that person is disabled. • Living Wills and Durable Power of Attorney for Health Care examples. – Ex: a person may specify that certain measures are to be taken or withheld if he/she is in a coma.
Patient Self-Determination Act (PSDA) • A Durable Power of Attorney (POA)for Health Care is a signed, dated, and witnessed paper that appoints someone to make the medical decisions for a person in the event he/she becomes unable to do so. • A do-not-resuscitate (DNR) order tells medical professionals not to perform CPR, medical procedures used to restart a person’s heart and breathing. – Generally these orders are used by people who are in the final stages of a terminal illness or who have a very serious condition. • Having an advance directive is not legally required. However, it is a good way to make sure a person’s wishes regarding medical care and honored. – It can be changed or canceled at any time, either in writing or verbally, or both.
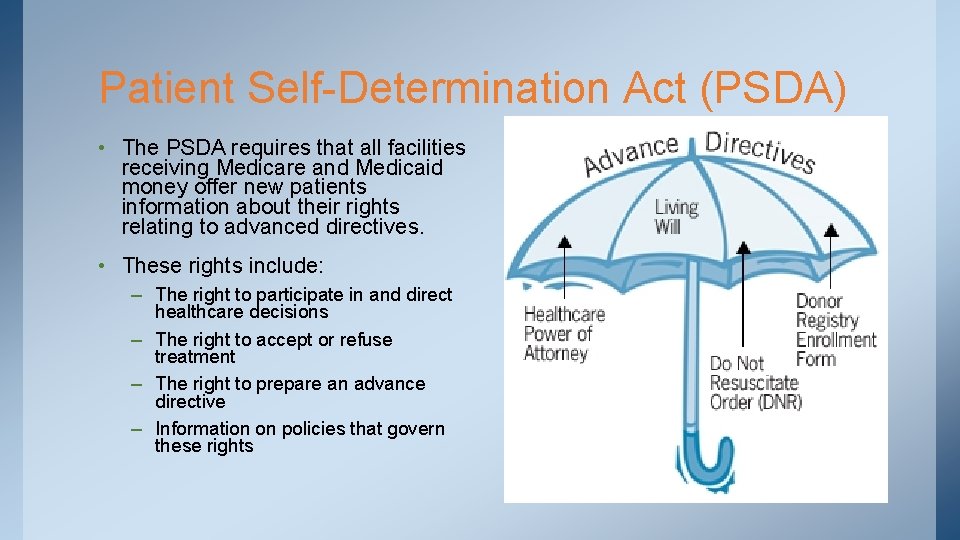
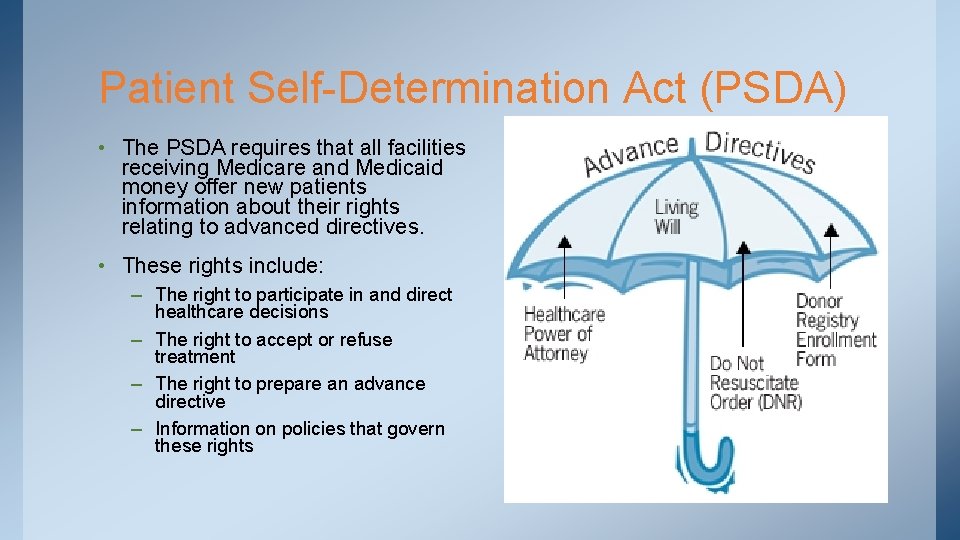
Patient Self-Determination Act (PSDA) • The PSDA requires that all facilities receiving Medicare and Medicaid money offer new patients information about their rights relating to advanced directives. • These rights include: – The right to participate in and direct healthcare decisions – The right to accept or refuse treatment – The right to prepare an advance directive – Information on policies that govern these rights
 Legal aspects of community health
Legal aspects of community health Chapter 2 ethical and legal issues
Chapter 2 ethical and legal issues Chapter 3 medical legal and ethical issues
Chapter 3 medical legal and ethical issues Legal and ethical issues chapter 3
Legal and ethical issues chapter 3 Legal and ethical issues chapter 5
Legal and ethical issues chapter 5 Emt chapter 3 medical legal and ethical issues
Emt chapter 3 medical legal and ethical issues Chapter 6 legal and ethical issues
Chapter 6 legal and ethical issues Legal and ethical issues chapter 5
Legal and ethical issues chapter 5 Chapter 3 legal and ethical aspects of nursing
Chapter 3 legal and ethical aspects of nursing Ethical and legal issues chapter 2
Ethical and legal issues chapter 2 Chapter 2 ethical and legal issues
Chapter 2 ethical and legal issues Chapter 5 legal and ethical responsibilities
Chapter 5 legal and ethical responsibilities Legal and ethical issues chapter 5
Legal and ethical issues chapter 5 Chapter 2 ethical and legal issues
Chapter 2 ethical and legal issues Chapter 6 legal and ethical issues
Chapter 6 legal and ethical issues Chapter 6 legal and ethical issues
Chapter 6 legal and ethical issues Medical legal and ethical issues chapter 3
Medical legal and ethical issues chapter 3 Legal and ethical issues in media
Legal and ethical issues in media Legal, social, ethical and professional issues in computing
Legal, social, ethical and professional issues in computing Legal issues of ict in education
Legal issues of ict in education Ethical issues of e commerce
Ethical issues of e commerce Legal and ethical issues in computer security
Legal and ethical issues in computer security Professional and ethical issues during internship
Professional and ethical issues during internship Attack sophistication vs intruder technical knowledge
Attack sophistication vs intruder technical knowledge Ethical and legal issues affecting the nursing assistant
Ethical and legal issues affecting the nursing assistant What is the difference between ethical and legal issues
What is the difference between ethical and legal issues Legal and ethical issues in information security
Legal and ethical issues in information security Legal issues in psychiatric nursing
Legal issues in psychiatric nursing Chapter 5 legal and ethical responsibilities key terms
Chapter 5 legal and ethical responsibilities key terms Ethical issues in health promotion
Ethical issues in health promotion Dho chapter 5 legal and ethical responsibilities
Dho chapter 5 legal and ethical responsibilities Chapter 4 legal and ethical responsibilities
Chapter 4 legal and ethical responsibilities Nonmaleficence
Nonmaleficence Chapter 4 ethical issues
Chapter 4 ethical issues Chapter 4 ethical and social issues in information systems
Chapter 4 ethical and social issues in information systems Ethical issues in qualitative research chapter 4
Ethical issues in qualitative research chapter 4 Chapter 4 ethical issues
Chapter 4 ethical issues Chapter 4 ethical issues
Chapter 4 ethical issues The perceived relevance or importance of an ethical issue
The perceived relevance or importance of an ethical issue Legal and ethical responsibilities of a coach
Legal and ethical responsibilities of a coach