Special Needs Plan Model of Care Training The

- Slides: 23

Special Needs Plan Model of Care Training The Way to Age Well in New York | 866 -586 -8044 | agewellnewyork. com
Overview • • • • Purpose and Use of a Model of Care (MOC) Key Components of the MOC Goals of the MOC Age. Well New York member populations Interdisciplinary Care Team (IDT) Health Risk Assessments (HRAs) and Risk Stratification Individualized Care Plan (ICP) Care Transition protocols Measurable Goals Provider Roles and Responsibilities Communication Network Performance and Health Outcomes Measurement Patient Experience 2
Purpose and Use of a Model of Care (MOC) • The Age. Well New York Model of Care is the framework for a comprehensive and collaborative care management delivery system to promote, improve and sustain member health outcomes across the care continuum in accordance with the requirements of the Medicaid and Medicare programs. • The MOC represents a comprehensive program for person centered care planning and coordination that addresses the entire array of acute care, primary care, behavioral health, specialist services, and long term care services and supports that enrollees need. • For enrollees, the MOC is used to improve: access to needed services, affordable and cost effective care, transitions across health care settings and providers, access to preventive health services, and health outcomes. 3
Key Components of the Model of Care • • • Understanding of the target population Measurable goals Staff structure and care management roles Interdisciplinary care team (IDT) Provider network having specialized expertise and using clinical guidelines MOC training for staff and provider network Health risk assessments (HRA) Communication network Care management for the most vulnerable subpopulations Performance and health outcomes measurement Use of self directed services 4
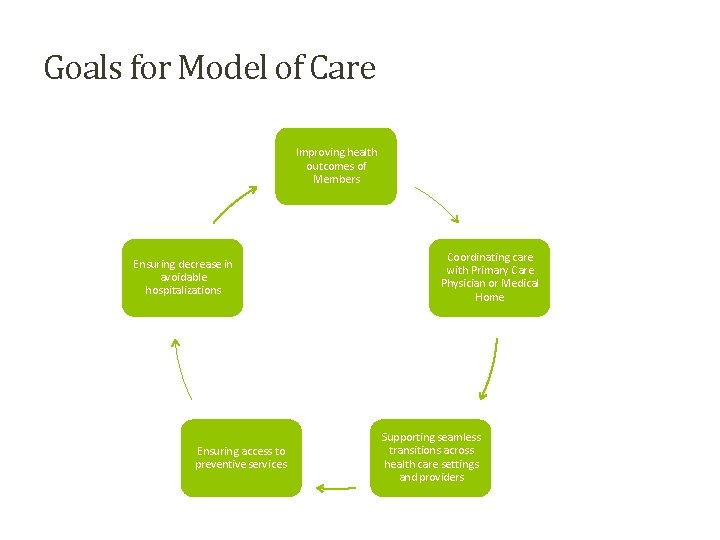
Model of Care Goals • Improve access to essential services such as medical, mental health and social services • Improve access to affordable care • Improve coordination of care through an identified point of contact • Improve seamless transitions of care across healthcare settings, providers and health services • Decrease avoidable hospital admissions and readmissions • Improve access to preventive health services • Assure appropriate utilization of services • Promote completion of advance directives • Improve beneficiary health 5
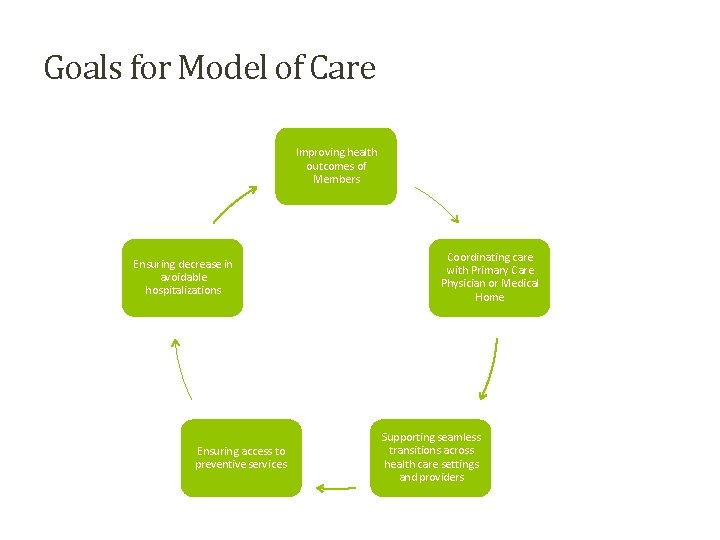
Goals for Model of Care Improving health outcomes of Members Ensuring decrease in avoidable hospitalizations Ensuring access to preventive services Coordinating care with Primary Care Physician or Medical Home Supporting seamless transitions across health care settings and providers 6
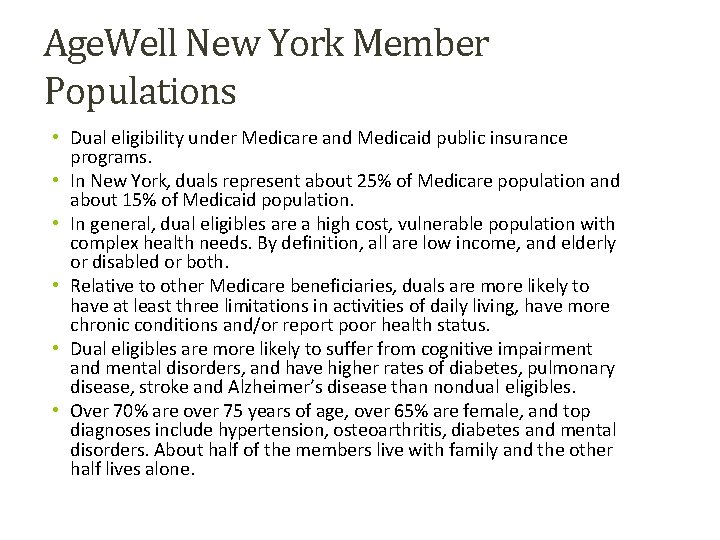
Age. Well New York Member Populations • Dual eligibility under Medicare and Medicaid public insurance programs. • In New York, duals represent about 25% of Medicare population and about 15% of Medicaid population. • In general, dual eligibles are a high cost, vulnerable population with complex health needs. By definition, all are low income, and elderly or disabled or both. • Relative to other Medicare beneficiaries, duals are more likely to have at least three limitations in activities of daily living, have more chronic conditions and/or report poor health status. • Dual eligibles are more likely to suffer from cognitive impairment and mental disorders, and have higher rates of diabetes, pulmonary disease, stroke and Alzheimer’s disease than nondual eligibles. • Over 70% are over 75 years of age, over 65% are female, and top diagnoses include hypertension, osteoarthritis, diabetes and mental disorders. About half of the members live with family and the other half lives alone. 7
Staff Structure & Care Management Roles • The structure of the Model of Care is comprised of employed and contracted staff the perform administrative, clinical and oversight functions. • Examples of Administrative functions: • Enrollment processing, eligibility verification, reporting and member reconciliation • Adjudication of claims, third party recovery, authorization administration, data collection and analytics • Member and provider customer service • Management of contract & product support, regulatory compliance, internal business area support 8
Staff Structure & Care Management Roles • Examples of Clinical Functions: • Care Management, developing care plan in conjunction with member and Interdisciplinary Care Team • Member Education • Analysis and evaluation of program goals • Examples of Administrative & Clinical Oversight • Professional staff credentialing • Utilization management including prior authorization & notification • Develop evidence based criteria by reviewing available evidence, current standards of practice & existing coverage positions as defined by laws, rules and regulations. • Investigate and conduct reviews to confirm corporate compliance program 9
Interdisciplinary Care Team (ICT) • Each member is assigned to an ICT, which has the primary purpose of coordinating the delivery of services and benefits to address member specific needs • Members of the ICT are determined by analysis of the members initial health risk assessment and subsequent assessments. • Typically, ICT composition includes the assigned Care Manager, Primary Care Physician, specialists involved in the care of the members, home and community based providers, the member and caregivers/family. 10
Interdisciplinary Team (ICT) • Additional ICT members may include nurse practitioner, pharmacist, restorative therapists, nutritionist, health educator, other disease management specialists. • Care Management team assumes critical role in coordinating and communicating with the ICT and the member. 11
Health Risk Assessments (HRAs) • Use of standardized, comprehensive approach to collecting, analyzing and communicating health risk assessment information. Identify current and future health risks. • It also serves to identify and survey elderly and frail members at risk for increased emergency department visits, hospitalization and skilled nursing facility admission. • Age. Well New York may use a modified version of the CDC’s Health Risk Assessment tool along with other customized assessments such as: Falls Risk Assessment Diabetic Knowledge Assessment Braden Scale Assessment Home Environment Assessment Respiratory/Cardiac Assessment Emergency Assessments Transportation Assessment 12
Health Risk Assessments (HRAs) • HRAs performed on initial assessment and reassessments may, when necessary, include full medication review. Results discussed with member’s Primary Care Physician to avoid poly-pharmacy, drug-to-drug interactions, decreased potentiated side effects, sub-therapeutic dosages, and actual or perceived allergies or side effects. • HRA reviews allow for prioritization of problems and interventions within the plan of care and identification of gaps in continuity of care guided in evidence-based practices. 13
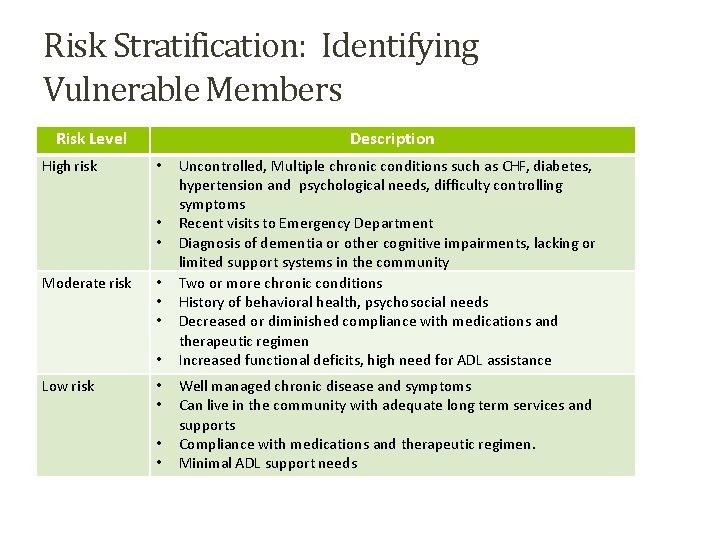
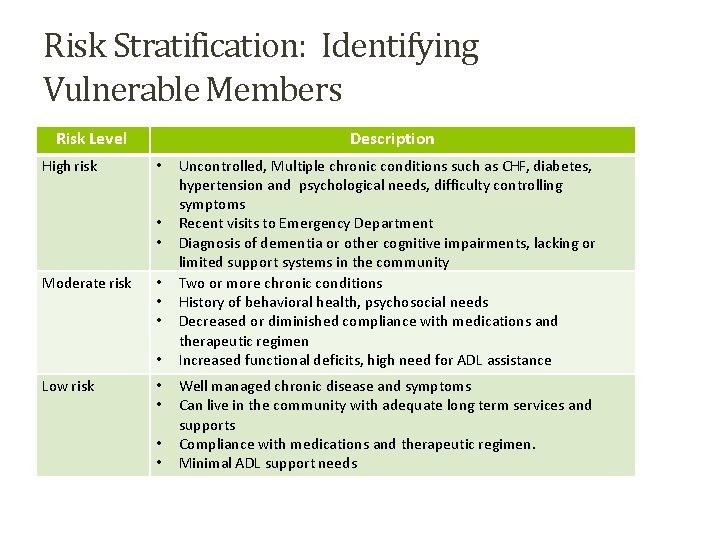
Risk Stratification: Identifying Vulnerable Members Risk Level High risk Description • • • Moderate risk • • Low risk • • Uncontrolled, Multiple chronic conditions such as CHF, diabetes, hypertension and psychological needs, difficulty controlling symptoms Recent visits to Emergency Department Diagnosis of dementia or other cognitive impairments, lacking or limited support systems in the community Two or more chronic conditions History of behavioral health, psychosocial needs Decreased or diminished compliance with medications and therapeutic regimen Increased functional deficits, high need for ADL assistance Well managed chronic disease and symptoms Can live in the community with adequate long term services and supports Compliance with medications and therapeutic regimen. Minimal ADL support needs 14
Individualized Care Plan (ICP) • The ICP is a comprehensive, person centered plan of care describing in detail the member’s health and medical needs, personal goals, and care management and coordination of services across the continuum of care. • The Interdisciplinary Care Team (ICT), led by the Care Manager, develops the ICP with the involvement of the member and/or family/caregivers. • The Care Manager maintains monthly communication with the members to address any issues or questions about the ICP and/or services and benefits. • The ICP identifies and reflects the member’s unique needs and the services and care needed to meet those needs. Special services and benefits are included in the ICP according to the needs identified through the Health Risk Assessments (HRAs) 15
Individualized Care Plan (ICP) • The outcomes of the are measured and documented in the care plan. Member preferences for care documented in the ICP. • The ICP also addresses add-on benefits and services for vulnerable beneficiaries such as those with dementia, IV drug abusers, those with frequent falls, member utilizing 9 or more medications, unmanaged chronic disease, end-of life matters or no relationship with a PCP. Add- on benefits would include meal programs, wellness programs, smoking cessation programs, and specialized medication management. • ICPs are reviewed and revised by the member assigned Care Manager, in coordination with the member’s PCP, every six months or more frequently as called for when there has been a change in a member’s condition or other triggering events. 16
Care Transition Protocols When members are transitioning from one healthcare setting to another, Age. Well New York will ensure that Care Management, the ICT and involved providers follow safe and effective protocols to facilitate a smooth transition from one setting to another. Age. Well New York accomplishes this through timely and early identification of the member’s need for such care setting transition, a standardized and well documented process for communication among settings and related Care Management/ICT determinations and actions. Care transitions are coordinated by the Intensive Care Manager of the Transitions of Care team. The Care Manager is an RN and is assisted by a service coordinator. A social worker is available, as needed. As a functional unit, the Transitions of Care Team follows the protocols identified below, and documents such in the members care management record.
Measurable Goals • Improving access to essential services by meeting or exceeding standards for access to routine care, non-urgent sick care, wellness care, mental health services and emergency follow-up services, as examples. • Improving access to affordable care by encouraging use of network providers, and addressing issues arising out of grievances and action appeals. • Improving coordination of care by an identified point of contact, i. e. , Care Manager, assisting the member in navigation of health system and communicating routinely with the ICT. • Improving seamless transitions of care by recognizing complex health needs, and transmitting health information on a timey basis for a smooth transition across settings, providers and post-discharge from an inpatient or residential facility. • Improving access to preventive health services by promoting and educating members about value of preventive and wellness services. • Assuring appropriate utilization of services by avoiding over use and under use of services through clinical coverage decisions based on available evidence-based guidelines. • Improving members health outcomes by a formal process to monitor and evaluate the necessity, appropriateness, efficiency, effectiveness, and safety of health and medical services ordered for and provided to members. 17
Provider Roles and Responsibilities Age. Well New York recognizes the primary care physician (PCP) as the ICT member who determines ultimately which services the member will receive. The PCP works collaboratively with the Care Manger and the ICT to make a determination based on the comprehensive health risk assessment (HRA), psychosocial and changing clinical needs of the member. The Age. Well New York Provider Manual is issued to each provider and outlines the roles and responsibilities of all providers including PCPs. It also outlines expectations, including but not limited to, timeliness of scheduling services, prevention of duplicative services, improved access to care across the continuum, services requiring prior authorization and expectations regarding cultural competence. The Care Manager and PCP coordinate to ensure that services requiring prior authorization and/or transition from one level of care to another are appropriately documented in the care management record.
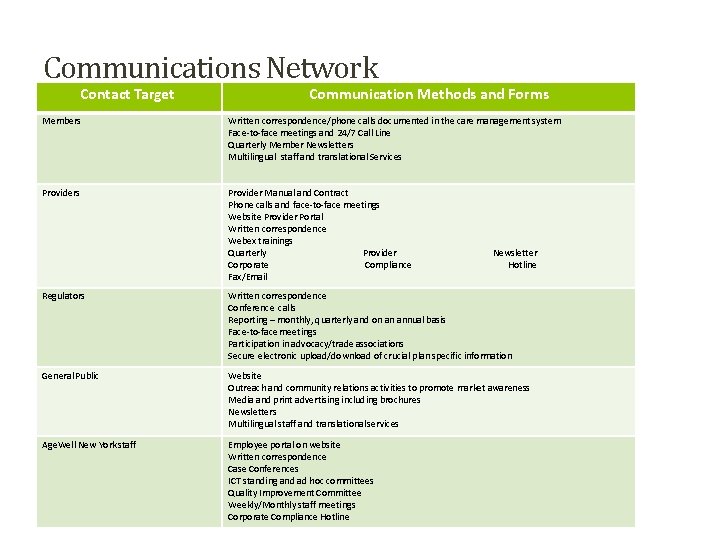
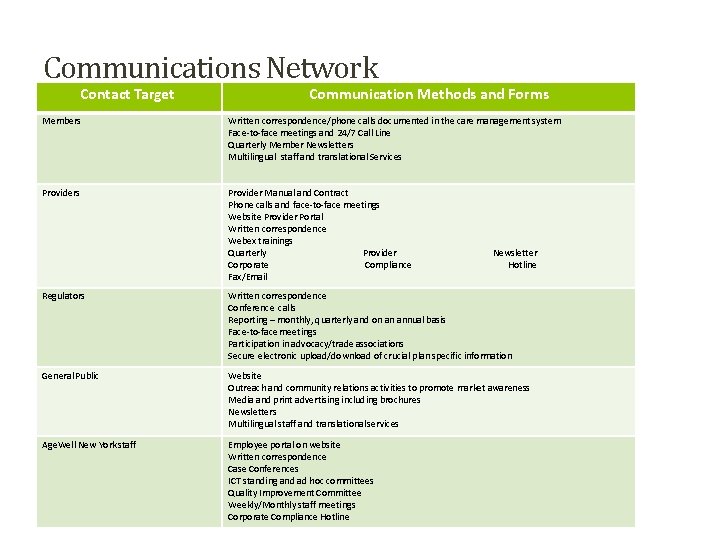
Communications Network Contact Target Communication Methods and Forms Members Written correspondence/phone calls documented in the care management system Face-to-face meetings and 24/7 Call Line Quarterly Member Newsletters Multilingual staff and translational Services Provider Manual and Contract Phone calls and face-to-face meetings Website Provider Portal Written correspondence Webex trainings Quarterly Provider Corporate Compliance Fax/Email Newsletter Hotline Regulators Written correspondence Conference calls Reporting – monthly, quarterly and on an annual basis Face-to-face meetings Participation in advocacy/trade associations Secure electronic upload/download of crucial plan specific information General Public Website Outreach and community relations activities to promote market awareness Media and print advertising including brochures Newsletters Multilingual staff and translational services Age. Well New York staff Employee portal on website Written correspondence Case Conferences ICT standing and ad hoc committees Quality Improvement Committee Weekly/Monthly staff meetings Corporate Compliance Hotline 18
Performance and Health Outcomes Measurement • Age. Well’s Model of Care (MOC) uses evidence-based practices and applies continuous performance oversight to identify opportunities for improvement. • Evidence-based practices and various industry standards are applied to monitor and measure performance and health outcomes including: HEDIS, utilization management standards, member satisfaction studies, provider surveys, analyses of grievances and appeals, claims data, high cost and utilization outlier analyses, poly-pharmacy, and diseasespecific standards and practices, as examples. • Performance and Health Outcomes measurement is applied for the improvement of the MOC, and changes are communicated to members, network providers, IDTs, community partners and internal staff. 19
MEASURING PATIENT EXPERIENCE OF CARE Age. Well measures member satisfaction across all entire operations. All grievances and appeals are reviewed and classified for further analysis, identification of improvement opportunities, and then addressing any reason for dissatisfaction. Age. Well compiles member complaints and appeals by reason, practitioner and areas of care involved. Grievances and Appeals are categorized by: • • Quality of Care Access Service and Performance Financial
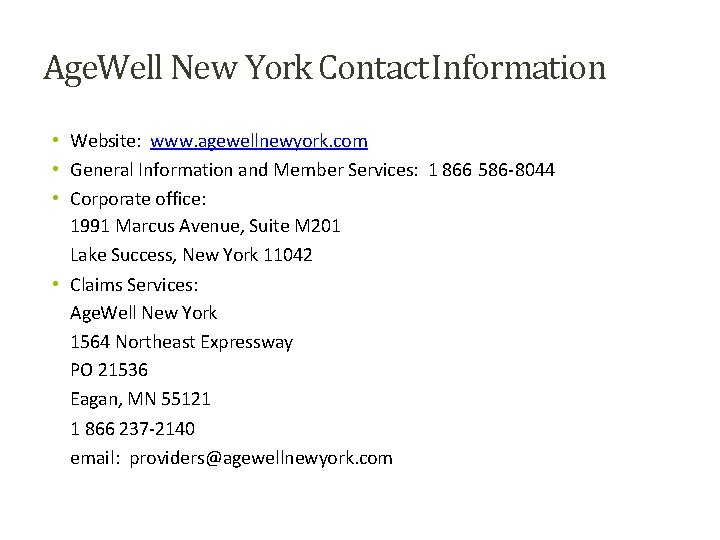
Age. Well New York Contact Information • Website: www. agewellnewyork. com • General Information and Member Services: 1 866 586 -8044 • Corporate office: 1991 Marcus Avenue, Suite M 201 Lake Success, New York 11042 • Claims Services: Age. Well New York 1564 Northeast Expressway PO 21536 Eagan, MN 55121 1 866 237 -2140 email: providers@agewellnewyork. com 20