Soft Markers Dr F Rahimi Tehran University of
















- Slides: 43

ﺳﻮﻧﻮگﺮﺍﻓی ﺳﻪ ﻣﺎﻫﻪ ﺩﻭﻡ ﻭ Soft Markers Dr. F Rahimi Tehran University of Medical Scienc Yas Hospital

ﺳﻮﻧﻮگﺮﺍﻓی ﺳﻪ ﻣﺎﻫﻪ ﺩﻭﻡ ﻭ Soft Markers As part of standard prenatal care recommends ultrasound examination for all pregnant patients on mid-trimester usually done at 16 to 22 weeks.
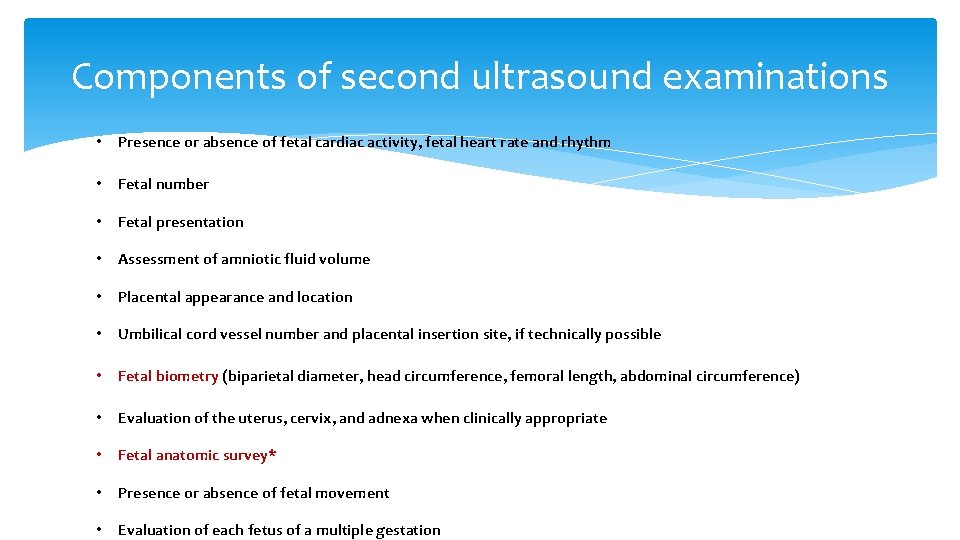
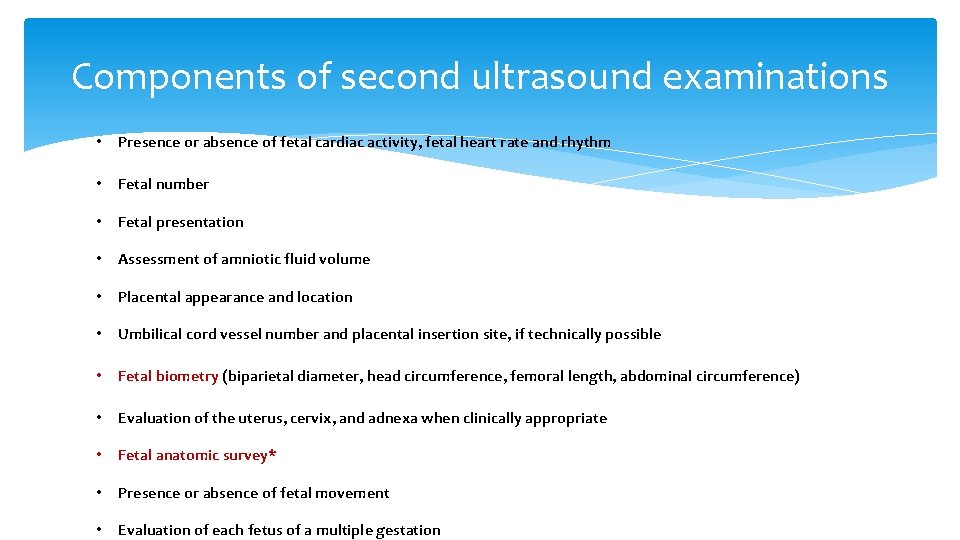
Components of second ultrasound examinations • Presence or absence of fetal cardiac activity, fetal heart rate and rhythm • Fetal number • Fetal presentation • Assessment of amniotic fluid volume • Placental appearance and location • Umbilical cord vessel number and placental insertion site, if technically possible • Fetal biometry (biparietal diameter, head circumference, femoral length, abdominal circumference) • Evaluation of the uterus, cervix, and adnexa when clinically appropriate • Fetal anatomic survey* • Presence or absence of fetal movement • Evaluation of each fetus of a multiple gestation

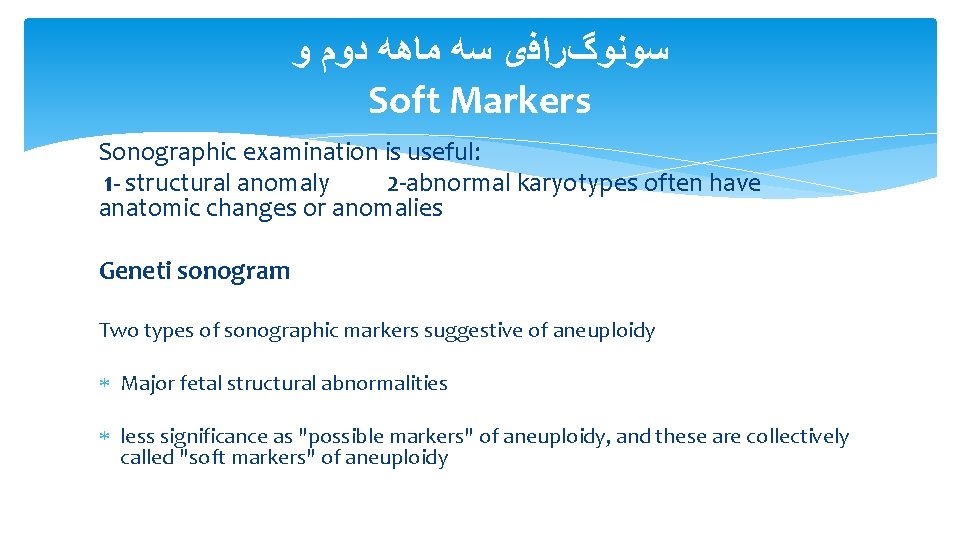
ﺳﻮﻧﻮگﺮﺍﻓی ﺳﻪ ﻣﺎﻫﻪ ﺩﻭﻡ ﻭ Soft Markers Sonographic examination is useful: 1 - structural anomaly 2 -abnormal karyotypes often have anatomic changes or anomalies Geneti sonogram Two types of sonographic markers suggestive of aneuploidy Major fetal structural abnormalities less significance as "possible markers" of aneuploidy, and these are collectively called "soft markers" of aneuploidy
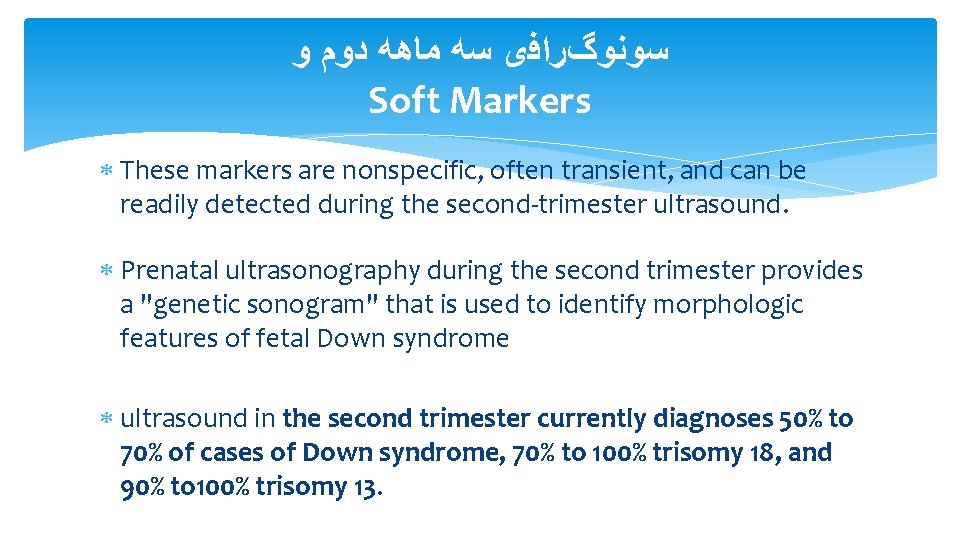
ﺳﻮﻧﻮگﺮﺍﻓی ﺳﻪ ﻣﺎﻫﻪ ﺩﻭﻡ ﻭ Soft Markers These markers are nonspecific, often transient, and can be readily detected during the second-trimester ultrasound. Prenatal ultrasonography during the second trimester provides a "genetic sonogram" that is used to identify morphologic features of fetal Down syndrome ultrasound in the second trimester currently diagnoses 50% to 70% of cases of Down syndrome, 70% to 100% trisomy 18, and 90% to 100% trisomy 13.
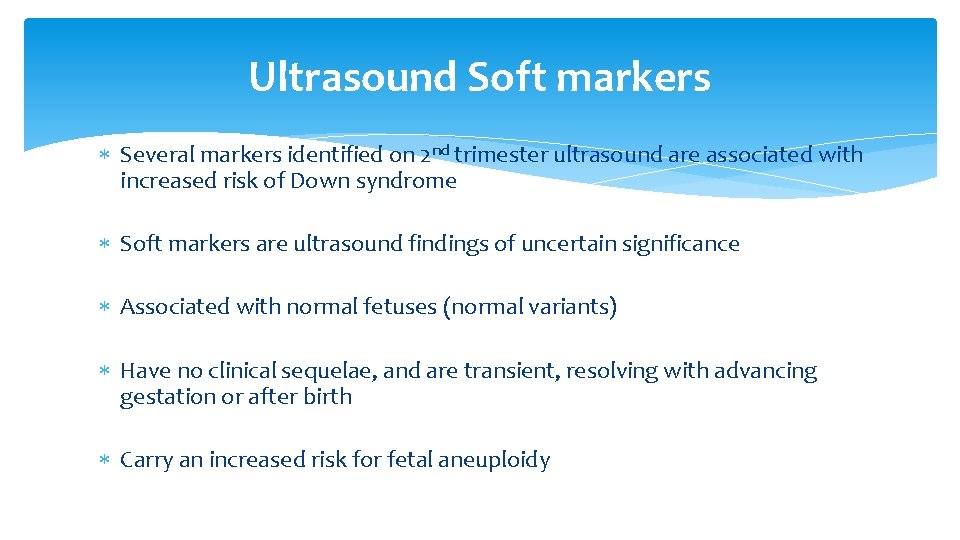
Ultrasound Soft markers Several markers identified on 2 nd trimester ultrasound are associated with increased risk of Down syndrome Soft markers are ultrasound findings of uncertain significance Associated with normal fetuses (normal variants) Have no clinical sequelae, and are transient, resolving with advancing gestation or after birth Carry an increased risk for fetal aneuploidy
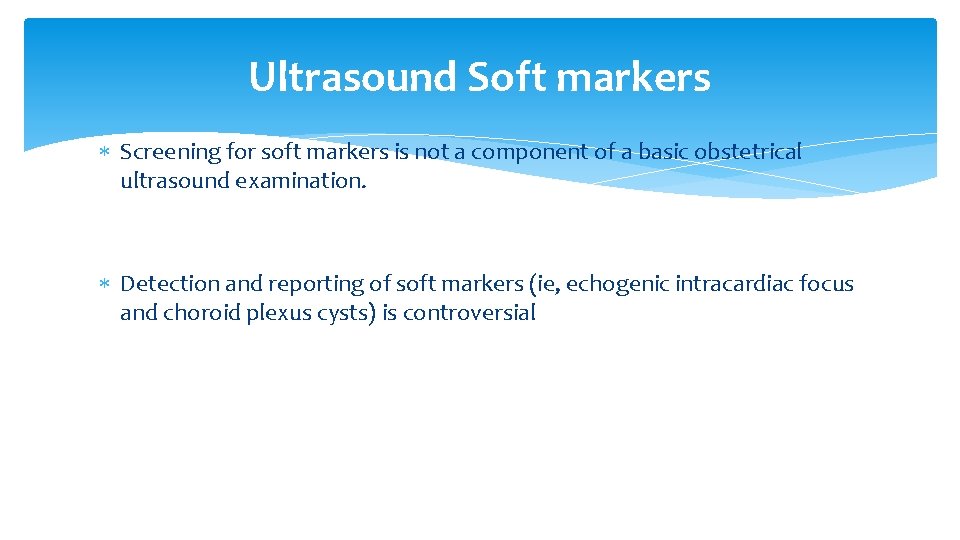
Ultrasound Soft markers Screening for soft markers is not a component of a basic obstetrical ultrasound examination. Detection and reporting of soft markers (ie, echogenic intracardiac focus and choroid plexus cysts) is controversial
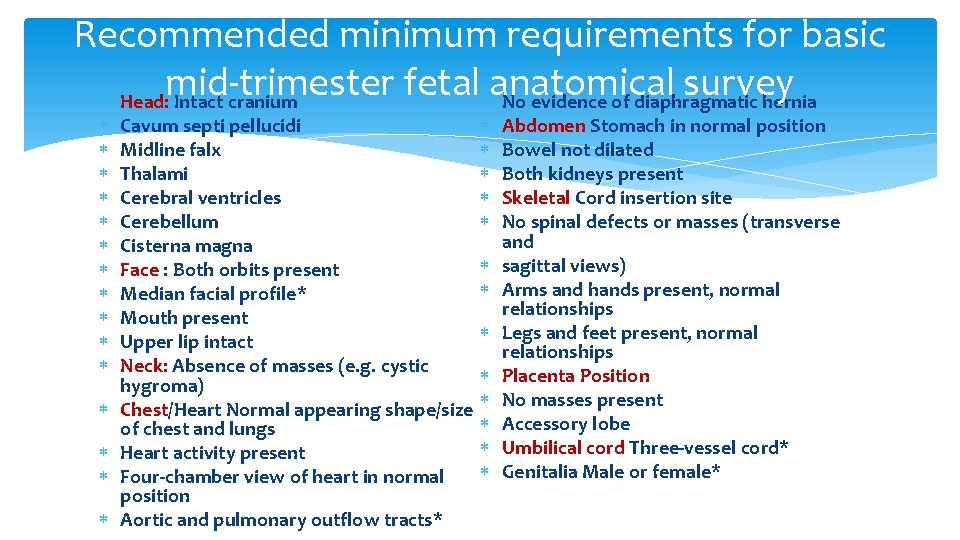
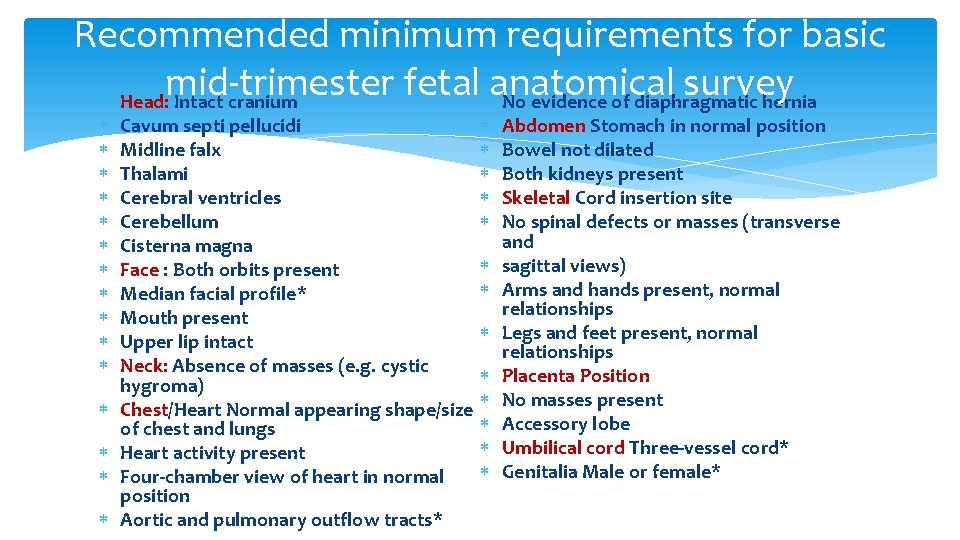
Recommended minimum requirements for basic mid-trimester fetal anatomical survey Head: Intact cranium No evidence of diaphragmatic hernia Cavum septi pellucidi Midline falx Thalami Cerebral ventricles Cerebellum Cisterna magna Face : Both orbits present Median facial profile* Mouth present Upper lip intact Neck: Absence of masses (e. g. cystic hygroma) Chest/Heart Normal appearing shape/size of chest and lungs Heart activity present Four-chamber view of heart in normal position Aortic and pulmonary outflow tracts* Abdomen Stomach in normal position Bowel not dilated Both kidneys present Skeletal Cord insertion site No spinal defects or masses (transverse and sagittal views) Arms and hands present, normal relationships Legs and feet present, normal relationships Placenta Position No masses present Accessory lobe Umbilical cord Three-vessel cord* Genitalia Male or female*
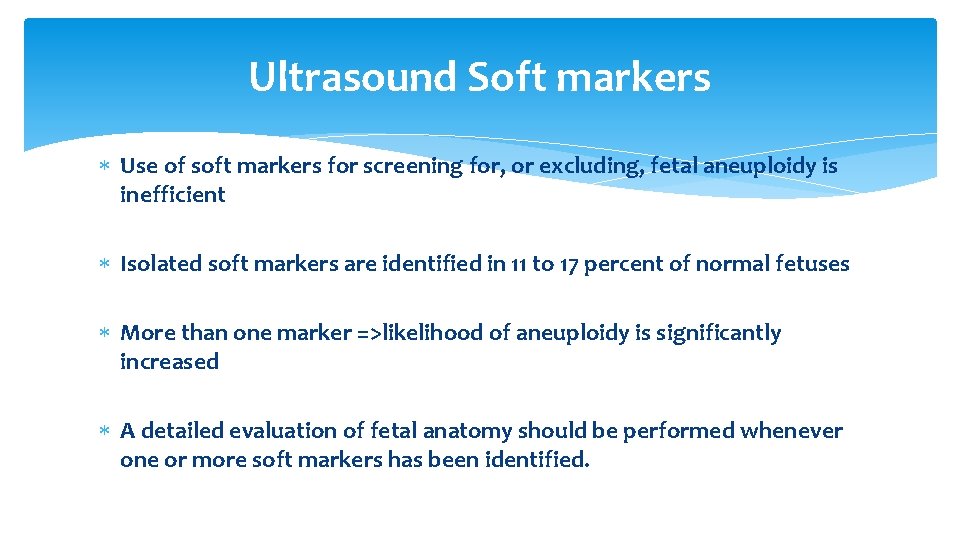
Ultrasound Soft markers Use of soft markers for screening for, or excluding, fetal aneuploidy is inefficient Isolated soft markers are identified in 11 to 17 percent of normal fetuses More than one marker =>likelihood of aneuploidy is significantly increased A detailed evaluation of fetal anatomy should be performed whenever one or more soft markers has been identified.
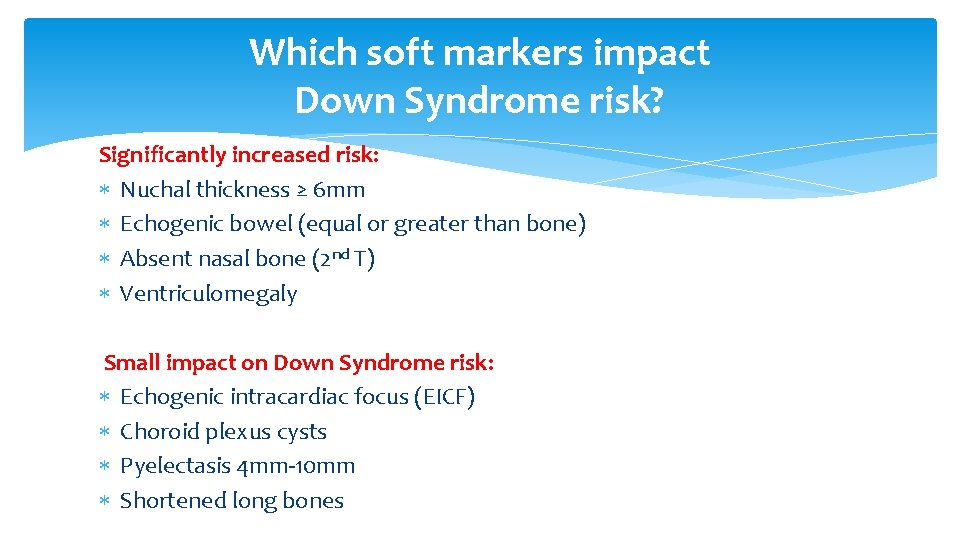
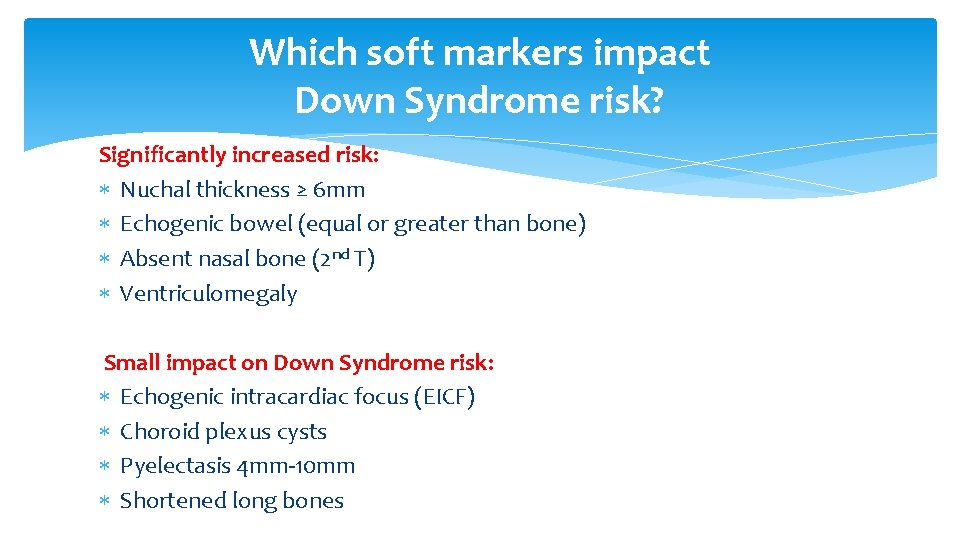
Which soft markers impact Down Syndrome risk? Significantly increased risk: Nuchal thickness ≥ 6 mm Echogenic bowel (equal or greater than bone) Absent nasal bone (2 nd T) Ventriculomegaly Small impact on Down Syndrome risk: Echogenic intracardiac focus (EICF) Choroid plexus cysts Pyelectasis 4 mm-10 mm Shortened long bones
Increased Nuchal fold The most sensitive (40 to 50 percent) and specific (99 percent) single ultrasound marker for Down syndrome in the second trimester (15 to 20 weeks but not later) An increased nuchal fold is detected in 20 to 33 percent of fetuses with Down syndrome and 0. 5 to 2 percent of euploid fetuses Measurement between the outer edge of the occipital bone to the outer margin of the skin and is taken in the axial plane

Echogenic bowel The bowel is considered to be echogenic when it is bright compared to the adjacent bone. A echogenic bowel is reported to be present in 0. 2– 1. 4% of 2 nd trimester USs and be diffuse or focal. When present it can be associated with aneuploidy (trisomy 21), congenital infection (CMV, toxoplasmosis, parvovirus), cystic fibrosis, intra amniotic bleeding, IUGR



Absent or Hypoplastic Nasal Bone Fetal profile is viewed in the midsagittal plane, the nasal bone synostosis appears as a thin echogenic line within the bridge of the nose Is absent in about 30 to 40 percent of Down syndrome fetuses and 0. 3 to 0. 7 percent of euploid fetuses Is hypoplastic in about 50 to 60 percent of Down syndrome fetuses and 6 to 7 percent of euploid fetuses A single pre-defined threshold for abnormal nasal bone length (≤ 2. 5 mm) a gestational age-based threshold (<2. 5 th or 5 th centile) based on the di stribution of nasal bone length in normal fetuses
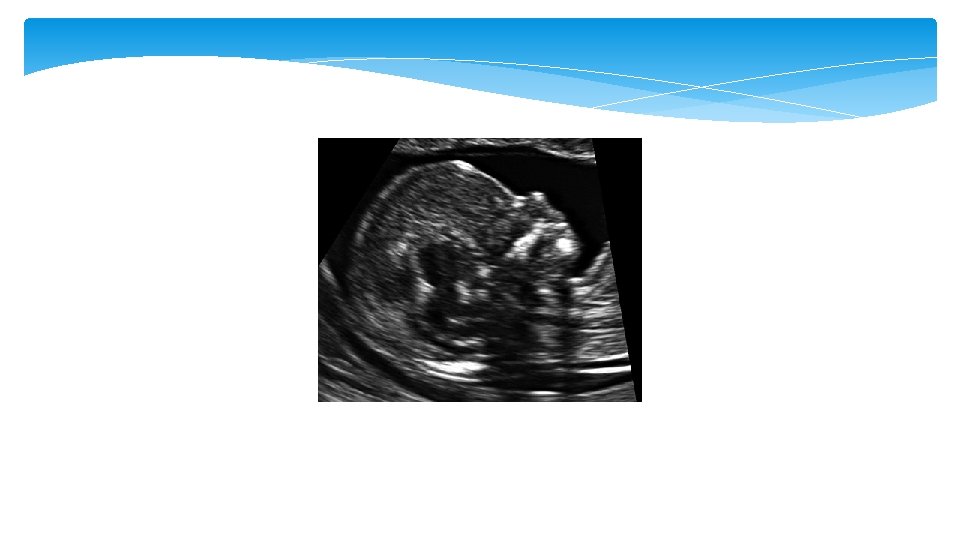

Mild ventriculomegaly Ventriculomegaly is a condition caused when there is dilated atrium beyond 10 mm. The mild ventriculomegaly (MVM), or what is called borderline ventriculomegaly, range between 10 – 12 mm and 10– 15 mm. It can be an isolated finding or be associated with an underlying cranial defect or anomaly such as agenesis of the corpus callosum

Ventriculomegaly Isolated ventriculomegaly is a risk factor for Down syndrome Mild ventriculomegaly is detected in 4 to 13 percent of fetuses with Down syndrome and 0. 1 to 0. 4 percent of euploid fetuses The risk of abnormal outcome, such as Down syndrome, increases with the degree of ventriculomegaly, progression of ventriculomegaly, and presence of other anomalies.
Echogenic focus (EF) of the heart An is definced as an echogenic area located in the region of the papillary muscles but not attached to the ventricular walls. They move with the atrioventricular valve and can occur in either cardiac ventricle, but are mainly seen in the left ventricle EF are seen in approximately 4% of obstetric sonograms with the lowest prevalence in Black populations and highest rates seen in Asian women


Choriod plexus (CP) cysta Cysts that are seen within the substance of the choroid plexus. They can be single or multiple, unilateral or bilateral, and occur with an incidence of approximately 1%. They may result from entrapement of cerebral spinal fluid with tangled villi. As the stroma of decreases with increasing gestational age this fluid is relased and the cyst resolves. For this reason more than 95% of these cysts resolve by the end of the second trimester

Renal Pyelectasis Mild pyelectasis refers to dilatation of the renal pelvis >4– 5 mm and <10 mm in the antero-posterior diameter measured in transverse section of the fetal abdomen. The cut-off value which is most frequently used in this dimesion is >4 mm in the 2 nd trimester and >7 mm thereafter
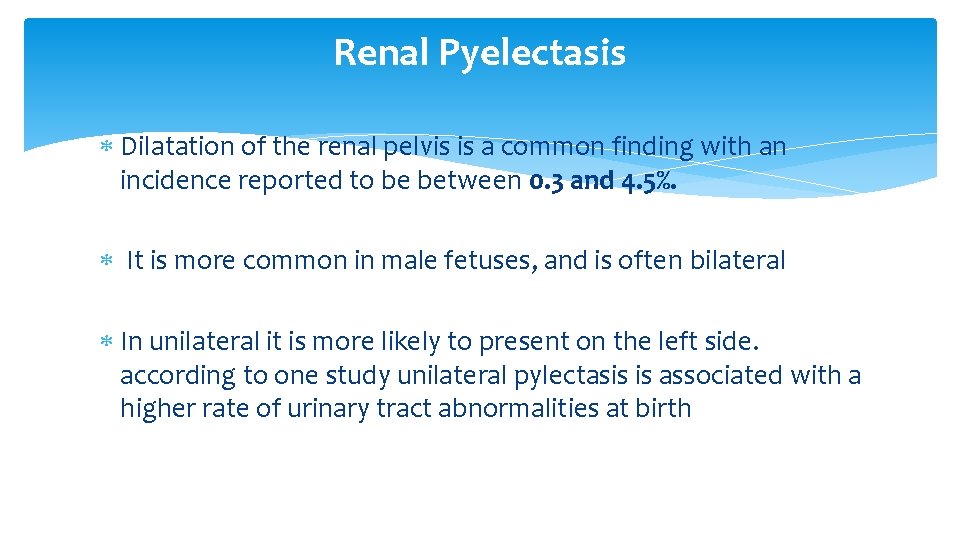
Renal Pyelectasis Dilatation of the renal pelvis is a common finding with an incidence reported to be between 0. 3 and 4. 5%. It is more common in male fetuses, and is often bilateral In unilateral it is more likely to present on the left side. according to one study unilateral pylectasis is associated with a higher rate of urinary tract abnormalities at birth

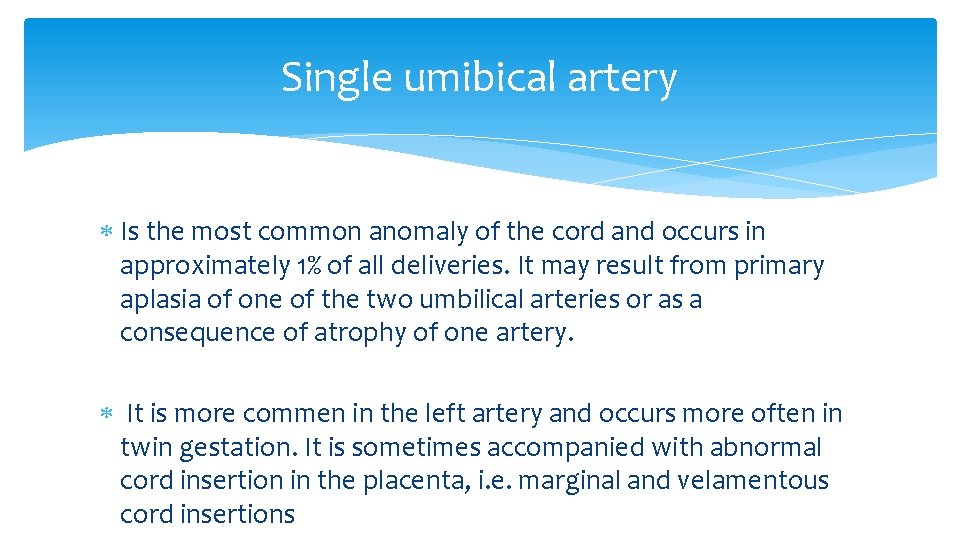
Single umibical artery Is the most common anomaly of the cord and occurs in approximately 1% of all deliveries. It may result from primary aplasia of one of the two umbilical arteries or as a consequence of atrophy of one artery. It is more commen in the left artery and occurs more often in twin gestation. It is sometimes accompanied with abnormal cord insertion in the placenta, i. e. marginal and velamentous cord insertions
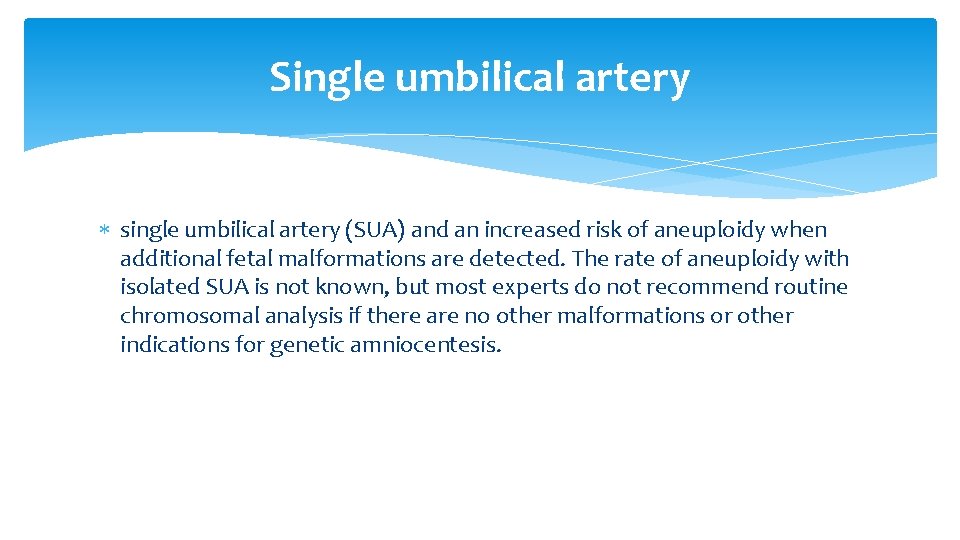
Single umbilical artery single umbilical artery (SUA) and an increased risk of aneuploidy when additional fetal malformations are detected. The rate of aneuploidy with isolated SUA is not known, but most experts do not recommend routine chromosomal analysis if there are no other malformations or other indications for genetic amniocentesis.

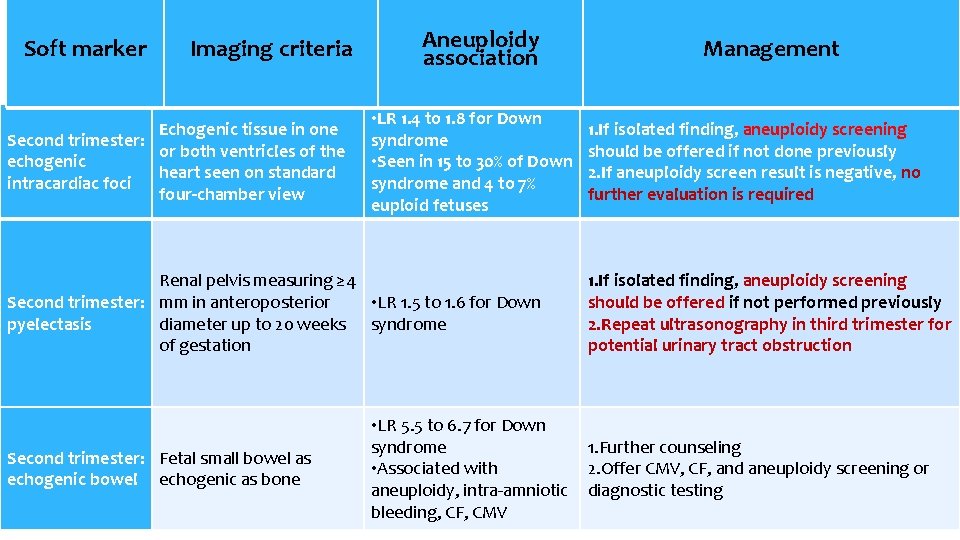
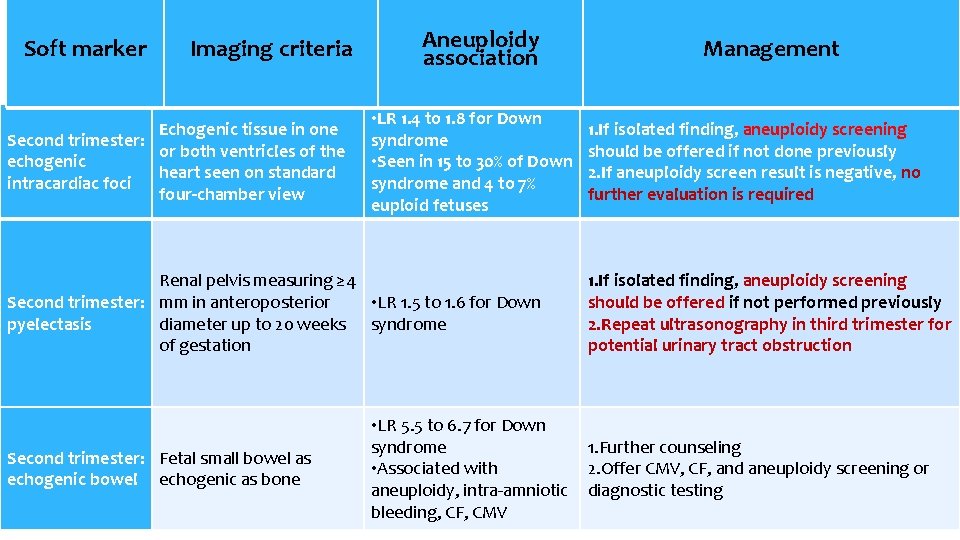
Soft marker Imaging criteria Echogenic tissue in one Second trimester: or both ventricles of the echogenic heart seen on standard intracardiac foci four-chamber view Aneuploidy association • LR 1. 4 to 1. 8 for Down syndrome • Seen in 15 to 30% of Down syndrome and 4 to 7% euploid fetuses Renal pelvis measuring ≥ 4 Second trimester: mm in anteroposterior • LR 1. 5 to 1. 6 for Down pyelectasis diameter up to 20 weeks syndrome of gestation Second trimester: Fetal small bowel as echogenic bowel echogenic as bone • LR 5. 5 to 6. 7 for Down syndrome • Associated with aneuploidy, intra-amniotic bleeding, CF, CMV Management 1. If isolated finding, aneuploidy screening should be offered if not done previously 2. If aneuploidy screen result is negative, no further evaluation is required 1. If isolated finding, aneuploidy screening should be offered if not performed previously 2. Repeat ultrasonography in third trimester for potential urinary tract obstruction 1. Further counseling 2. Offer CMV, CF, and aneuploidy screening or diagnostic testing
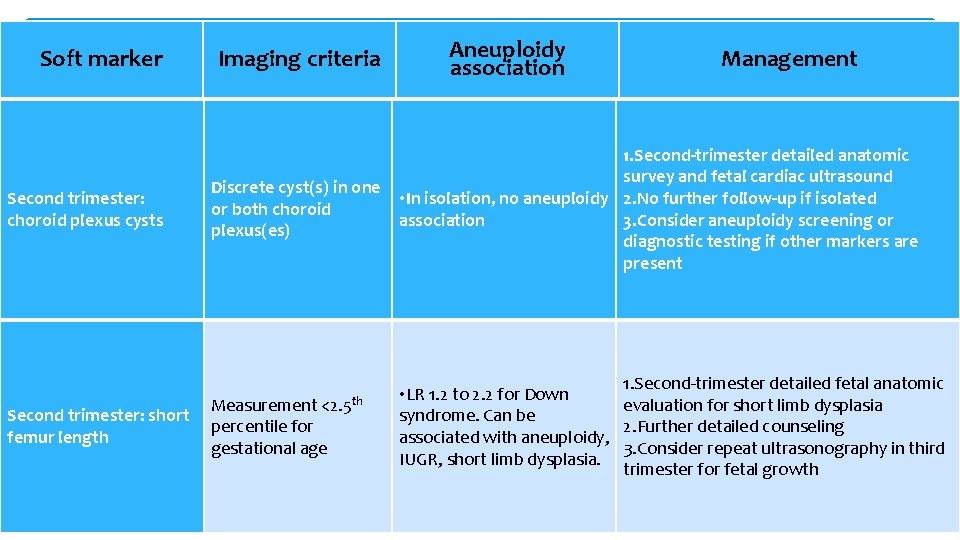
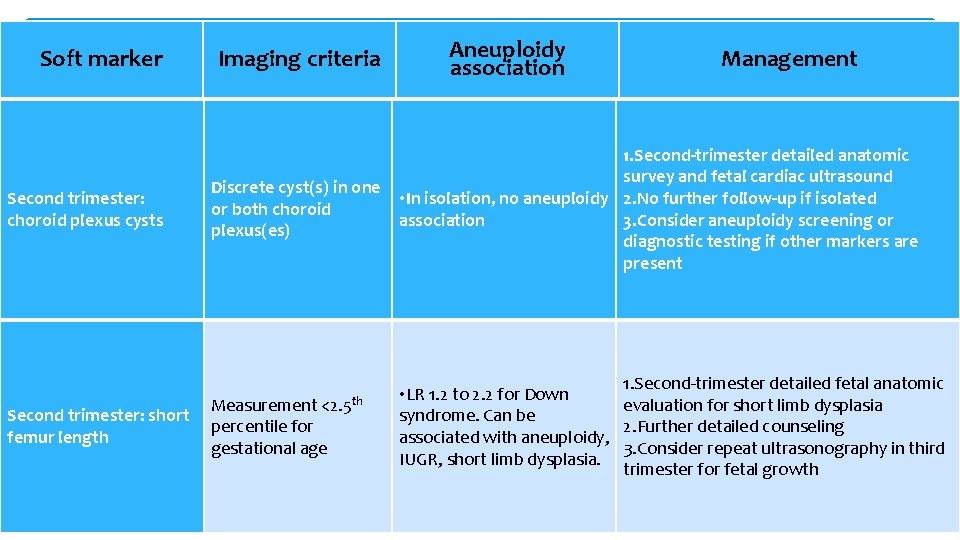
Soft marker Second trimester: choroid plexus cysts Second trimester: short femur length Imaging criteria Aneuploidy association Management 1. Second-trimester detailed anatomic survey and fetal cardiac ultrasound Discrete cyst(s) in one • In isolation, no aneuploidy 2. No further follow-up if isolated or both choroid association 3. Consider aneuploidy screening or plexus(es) diagnostic testing if other markers are present Measurement <2. 5 th percentile for gestational age 1. Second-trimester detailed fetal anatomic • LR 1. 2 to 2. 2 for Down evaluation for short limb dysplasia syndrome. Can be 2. Further detailed counseling associated with aneuploidy, 3. Consider repeat ultrasonography in third IUGR, short limb dysplasia. trimester for fetal growth
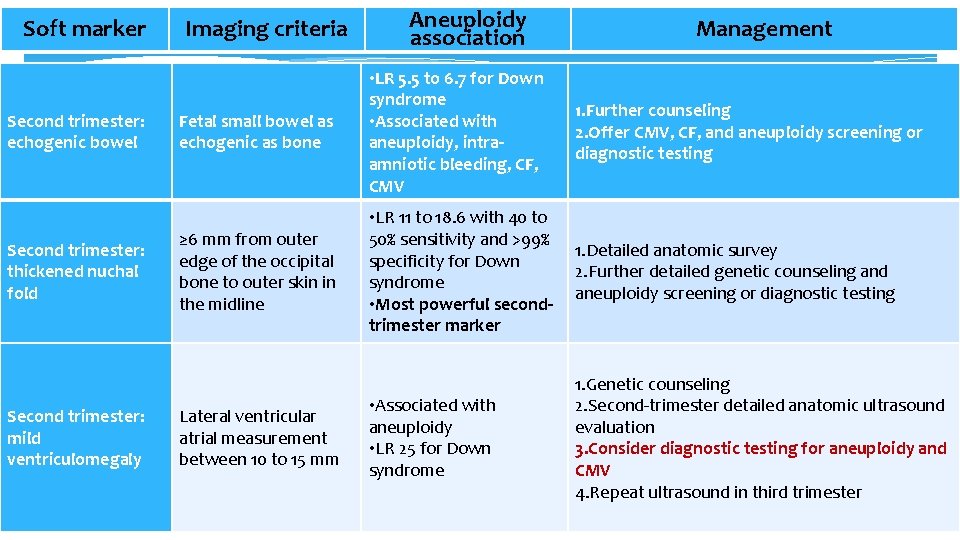
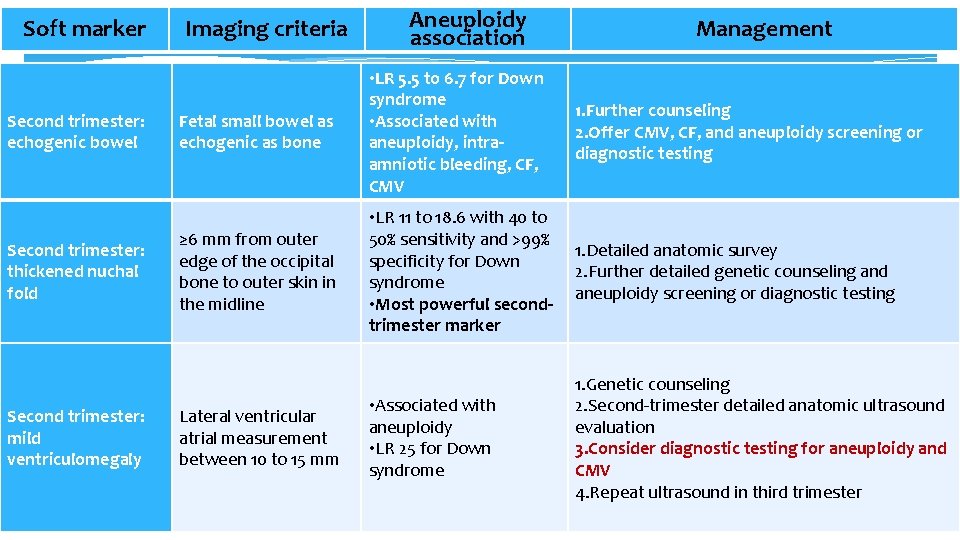
Soft marker Second trimester: echogenic bowel Second trimester: thickened nuchal fold Second trimester: mild ventriculomegaly Imaging criteria Aneuploidy association Management Fetal small bowel as echogenic as bone • LR 5. 5 to 6. 7 for Down syndrome • Associated with aneuploidy, intraamniotic bleeding, CF, CMV 1. Further counseling 2. Offer CMV, CF, and aneuploidy screening or diagnostic testing ≥ 6 mm from outer edge of the occipital bone to outer skin in the midline • LR 11 to 18. 6 with 40 to 50% sensitivity and >99% specificity for Down syndrome • Most powerful secondtrimester marker 1. Detailed anatomic survey 2. Further detailed genetic counseling and aneuploidy screening or diagnostic testing • Associated with aneuploidy • LR 25 for Down syndrome 1. Genetic counseling 2. Second-trimester detailed anatomic ultrasound evaluation 3. Consider diagnostic testing for aneuploidy and CMV 4. Repeat ultrasound in third trimester Lateral ventricular atrial measurement between 10 to 15 mm
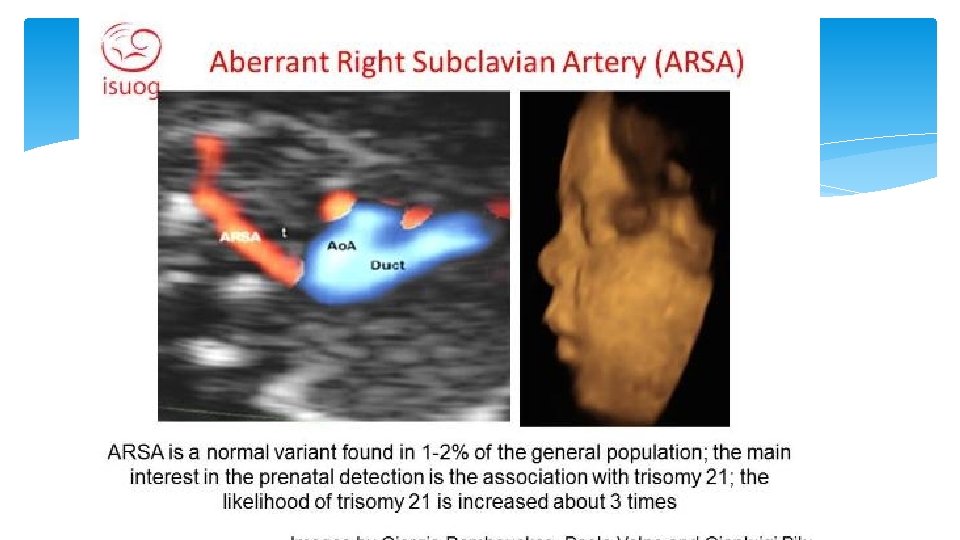
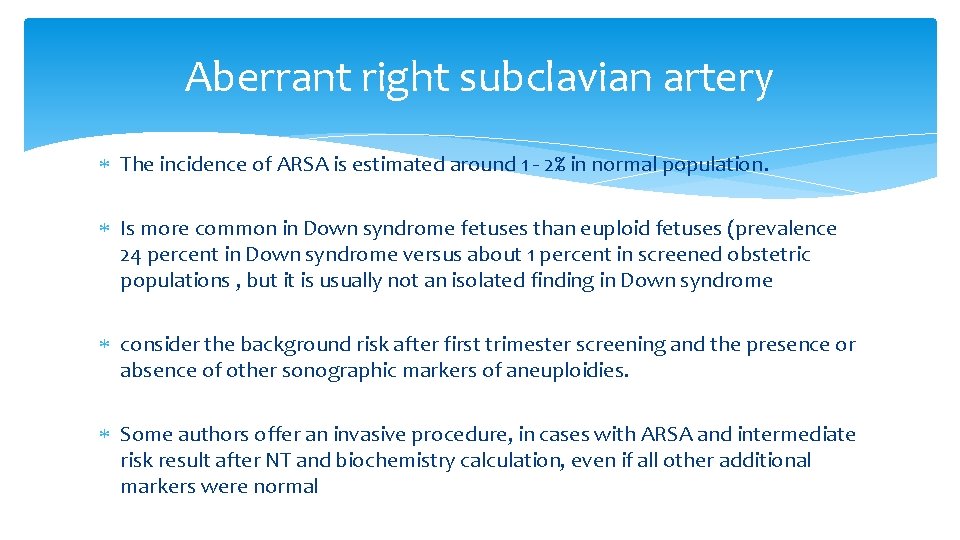
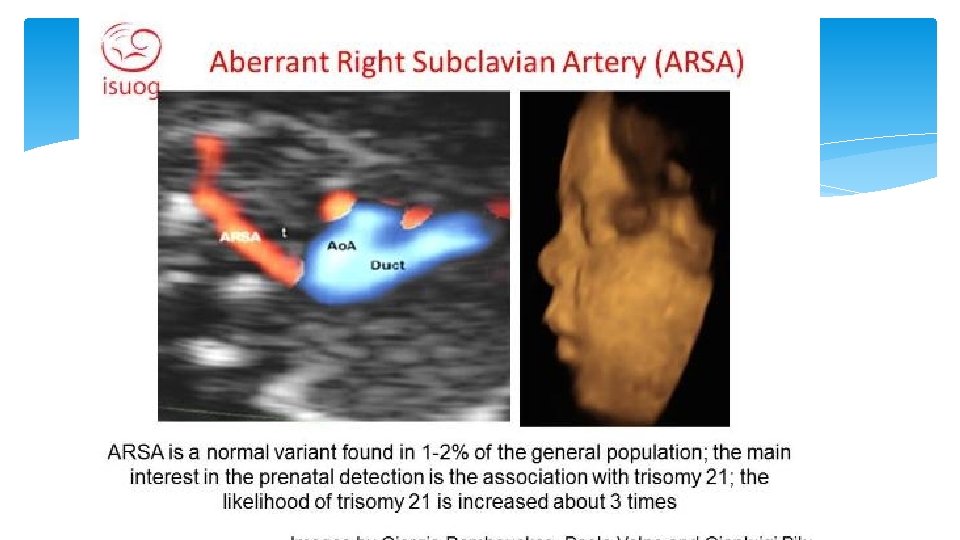
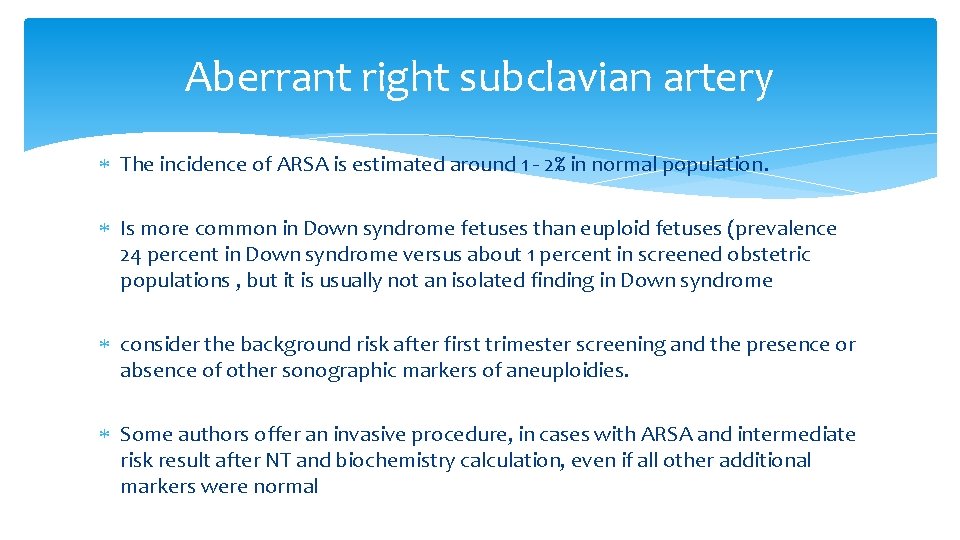
Aberrant right subclavian artery The incidence of ARSA is estimated around 1 - 2% in normal population. Is more common in Down syndrome fetuses than euploid fetuses (prevalence 24 percent in Down syndrome versus about 1 percent in screened obstetric populations , but it is usually not an isolated finding in Down syndrome consider the background risk after first trimester screening and the presence or absence of other sonographic markers of aneuploidies. Some authors offer an invasive procedure, in cases with ARSA and intermediate risk result after NT and biochemistry calculation, even if all other additional markers were normal


Thank you for attention
 Conus arteriosus
Conus arteriosus Ang namumuno sa bansang iran upang makamit ang kalayaan
Ang namumuno sa bansang iran upang makamit ang kalayaan Amin hossein rahimi
Amin hossein rahimi Sonia rahimi
Sonia rahimi Kid science hall tehran
Kid science hall tehran Tehran conference apush
Tehran conference apush Tehran hash download
Tehran hash download Periprostetic
Periprostetic Hepatitis comparison
Hepatitis comparison The map below shows the location of chicxulub crater
The map below shows the location of chicxulub crater Covert prestige definition
Covert prestige definition Floating red markers nuns shape
Floating red markers nuns shape Stansw meet the markers
Stansw meet the markers Discourse markers examples
Discourse markers examples A short section of corrugated roadway
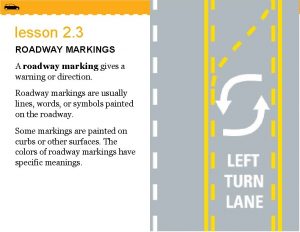
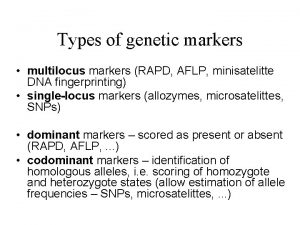
A short section of corrugated roadway Rflp vs rapd
Rflp vs rapd Discourse marker
Discourse marker Discourse markers examples
Discourse markers examples Discourse markers
Discourse markers St andrews eap conference
St andrews eap conference Volcanic ash
Volcanic ash 1000 foot markers runway
1000 foot markers runway Types of discourse
Types of discourse Relative clause examples with answers
Relative clause examples with answers Stance markers
Stance markers Discourse markers and linkers
Discourse markers and linkers Present perfect tense markers
Present perfect tense markers Penina wants to insert markers
Penina wants to insert markers Voice markers they say i say
Voice markers they say i say Past perfect қазақша
Past perfect қазақша What does the yield sign mean drivers ed
What does the yield sign mean drivers ed Semantic markers examples
Semantic markers examples Nais salary data
Nais salary data What is social variation
What is social variation Definition of independent clause
Definition of independent clause Markers of hbv infection
Markers of hbv infection The old man next to me on the pier was muttering to himself
The old man next to me on the pier was muttering to himself Neurocutaneous markers
Neurocutaneous markers Difference between selectable and screenable markers
Difference between selectable and screenable markers Marker beacon
Marker beacon Metacognitive markers examples
Metacognitive markers examples Cuando usamos el past continuous
Cuando usamos el past continuous Discource markers
Discource markers Sistema complemento funções
Sistema complemento funções