Sexually Transmitted Diseases STDs STDs syndromes Initiallyonly five


- Slides: 21
Sexually Transmitted Diseases (STDs)
�STDs - syndromes. �Initially-only five classical venereal diseases; syphilis, gonorrhoea, chancroid, lymphogranuloma venereum (LGV) and donovanosis. � “Second generation” STDs- Hepatitis B, HIV, Herpes etc. 2
Problem Statement World �World Health Organization - Sexually Transmitted Infections (STIs) and their complications - top five diseases categories for which adults in developing countries seek health care. � About one million new infections - every day. �If HIV, human papilloma virus (HPV) and human simplex virus (HSV) infections - included, the number of new cases - three times higher. 3
India � 40 million cases - every year. �Result of STD/RTI community based survey - 6% of the adult population or 30 million - infected with RTIs. �The 2005 ICMR multicentre rapid assessment survey (RAS) indicates that 12% �of female clients and 6% of male clients attending the out-patient departments for complaints �related to STI/RTI. • 40% of women suffer from STI/RTIs at any given point of time but only 1% of both partners take the treatment. • Southern states-LGV, GI, HIV etc. • Social stigma -concealment of facts - exact prevalence in the community not known - always under reporting. 4 Source: NACO
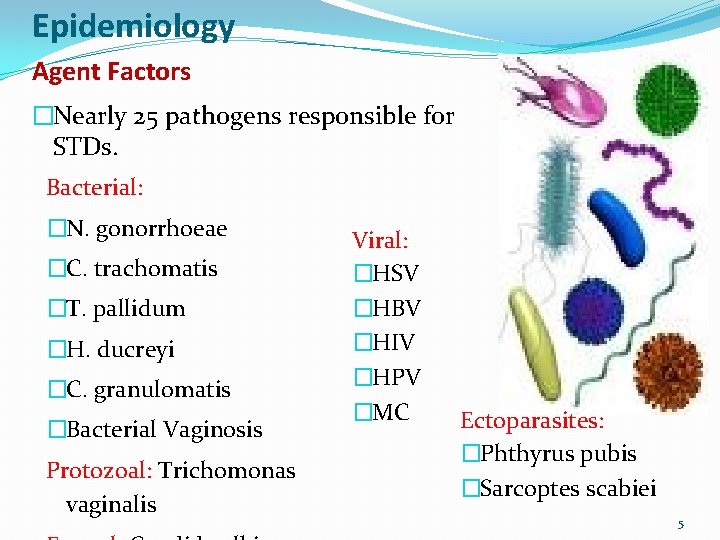
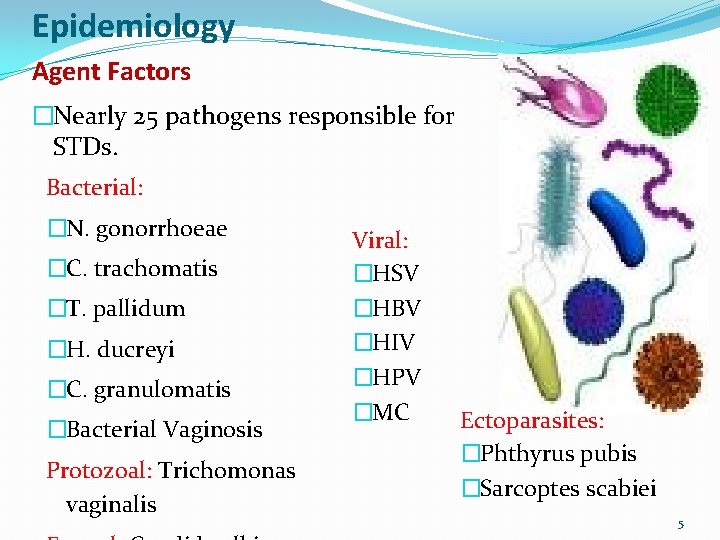
Epidemiology Agent Factors �Nearly 25 pathogens responsible for STDs. Bacterial: �N. gonorrhoeae �C. trachomatis �T. pallidum �H. ducreyi �C. granulomatis �Bacterial Vaginosis Protozoal: Trichomonas vaginalis Viral: �HSV �HBV �HIV �HPV �MC Ectoparasites: �Phthyrus pubis �Sarcoptes scabiei 5
Host Factors �Age group - 20 -30 years. �Incidence more in males but severity is highest in females. �More in single, divorced/ separated. �In lower SE group. �Foetus and neonate badly affected. �Circumcision- Protected 6
Demographic Factors �Migration, increase in age of marriage, population explosion – increase in No. of youngs. �Disaster - social disruption and migration of affected population to the safer areas of camps – �Overcrowding and extra marital relations. �Sexual exploitation of vulnerable groups especially children. 7

Social Factors � Prostitution � Broken Homes � Sexual Disharmony � Easy Money � Urbanization and Industrialization � Social Disruption � International Travel � Changing Behaviour � Social Stigma � Alcoholism � Other Addiction 8
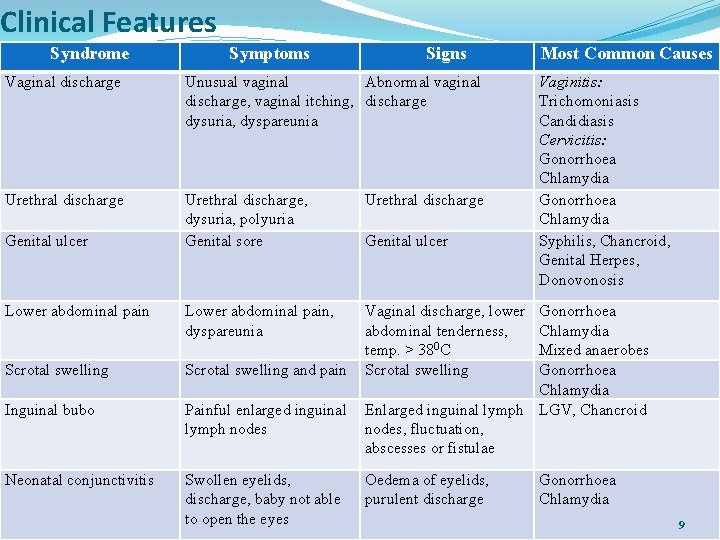
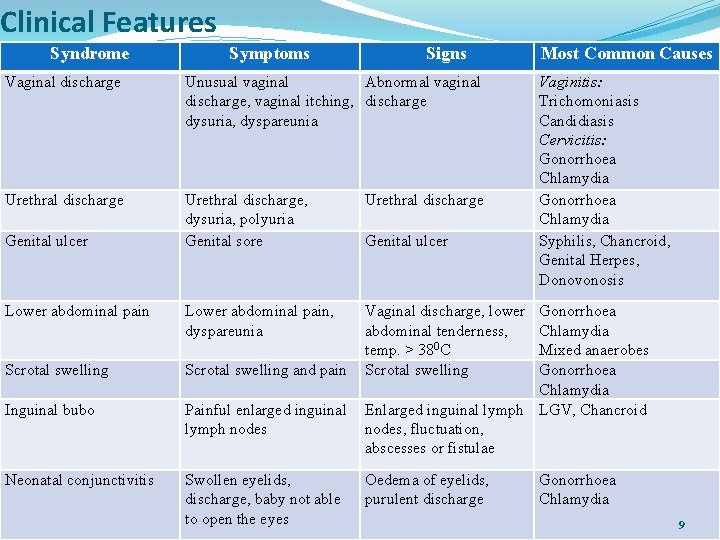
Clinical Features Syndrome Symptoms Signs Vaginal discharge Unusual vaginal Abnormal vaginal discharge, vaginal itching, discharge dysuria, dyspareunia Urethral discharge, dysuria, polyuria Genital sore Urethral discharge Lower abdominal pain, dyspareunia Scrotal swelling and pain Vaginal discharge, lower abdominal tenderness, temp. > 380 C Scrotal swelling Inguinal bubo Painful enlarged inguinal lymph nodes Neonatal conjunctivitis Swollen eyelids, discharge, baby not able to open the eyes Genital ulcer Most Common Causes Vaginitis: Trichomoniasis Candidiasis Cervicitis: Gonorrhoea Chlamydia Syphilis, Chancroid, Genital Herpes, Donovonosis Gonorrhoea Chlamydia Mixed anaerobes Gonorrhoea Chlamydia Enlarged inguinal lymph LGV, Chancroid nodes, fluctuation, abscesses or fistulae Oedema of eyelids, purulent discharge Gonorrhoea Chlamydia 9
�Syndromic Case Management �Simple, comprehensive, scientific method for treatment of STIs �endorsed by WHO for resource limiting settings especially in rural areas. �Syndromes - easily diagnosed and treatment is given at the first line health facility. �Effective against mixed infection and provides opportunities for preventive strategies and promotion of condoms. �In emergency situations - scarcity of resources and laboratories for the diagnosis of the cases - this approach is cost effective. 10
�Genital ulcers - common features in cases of syphilis, chancroid and granuloma inguinale. �In camps and shelters, if one case of genital ulcer - same etiological agent is implicated in other cases of genital ulcers. �Person with genital ulcer - more vulnerable to get HIV infection. �In the current scenario of HIV/AIDS pandemic, these patients should be given due attention. �History taking �Behavioural risk assessment- appropriate education & councelling preceded 11
�Confidentiality �Physical Examination �Lab. Tests - Syndromic approach - Failure of treatment �Syndromic Diagnosis �Syndromic Treatment �Counselling �Condom Provision �Reporting �Partner Notification - Partner Treatment and Counselling � Clinical Follow up 12
�Uretheral Discharge - Gonococcal and chlamydial infections �Genital Ulcer – Syphilis, chancroid, genital herpes - wash with soap & water – if vesicles are seen or history of recurrence – Acyclovir - if no vesicle / history- Syphilis, chancroid �Vaginal Discharge – Vaginitis and cervicitis (Gonococcal and chlamydial infections) �Scrotal Swelling – Epididymo-orchitis (Gonococcal and chlamydial infections) �LAP – PID (Gonococcal and chlamydial infections & anerobic bacteria) �Inguinal Bubos – Chancroid or LGV �Ophth. Neon. - Gonococcal and chlamydial infections 13
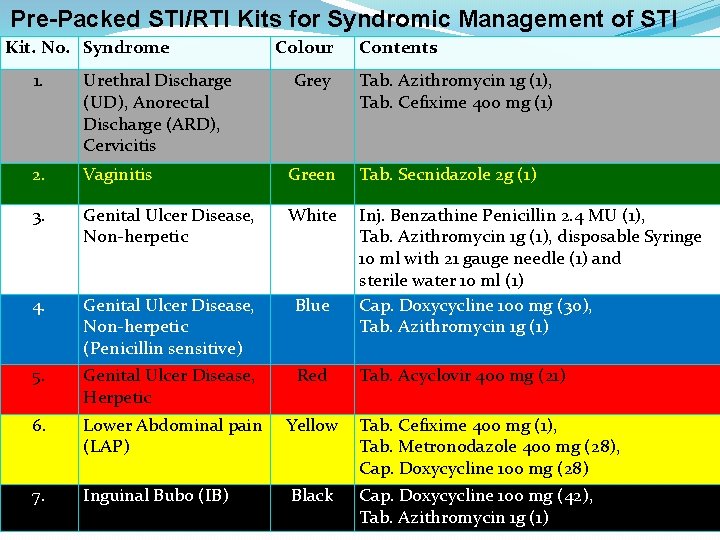
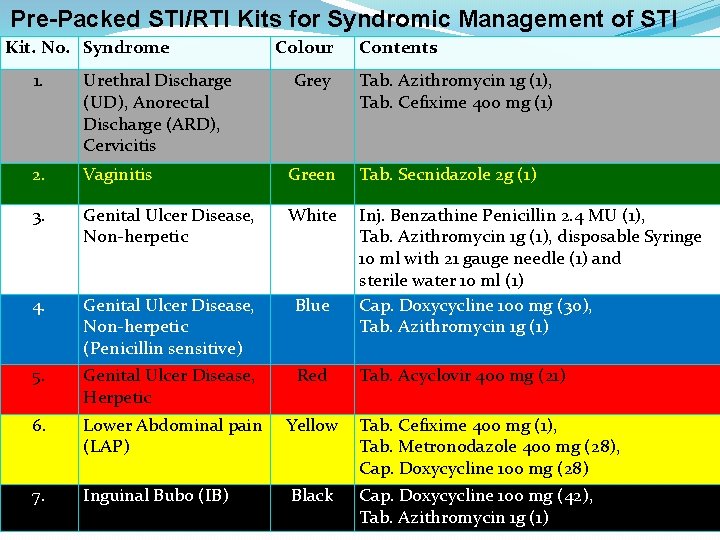
Pre-Packed STI/RTI Kits for Syndromic Management of STI Kit. No. Syndrome Colour Contents 1. Urethral Discharge (UD), Anorectal Discharge (ARD), Cervicitis Grey Tab. Azithromycin 1 g (1), Tab. Cefixime 400 mg (1) 2. Vaginitis Green Tab. Secnidazole 2 g (1) 3. Genital Ulcer Disease, Non-herpetic White 4. Genital Ulcer Disease, Non-herpetic (Penicillin sensitive) Blue Inj. Benzathine Penicillin 2. 4 MU (1), Tab. Azithromycin 1 g (1), disposable Syringe 10 ml with 21 gauge needle (1) and sterile water 10 ml (1) Cap. Doxycycline 100 mg (30), Tab. Azithromycin 1 g (1) 5. Genital Ulcer Disease, Herpetic Red 6. Lower Abdominal pain (LAP) Yellow Tab. Cefixime 400 mg (1), Tab. Metronodazole 400 mg (28), Cap. Doxycycline 100 mg (28) 7. Inguinal Bubo (IB) Black Cap. Doxycycline 100 mg (42), Tab. Azithromycin 1 g (1) Tab. Acyclovir 400 mg (21) 14

15
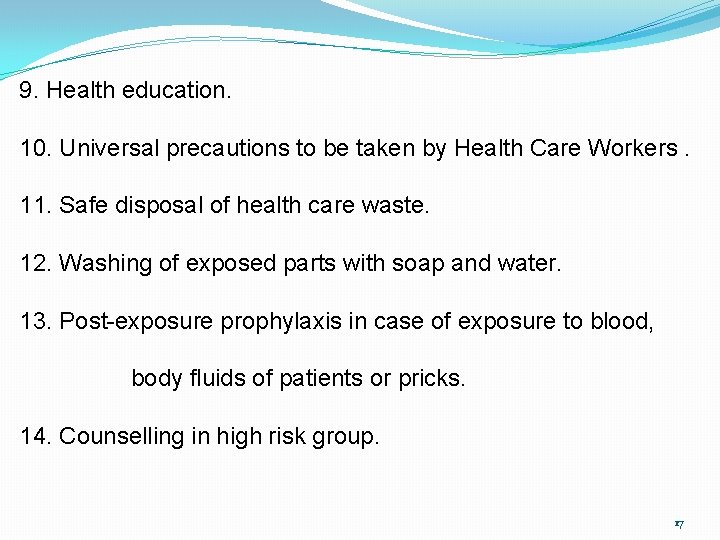
Prevention and Control (General) 1. Complete and adequate treatment to prevent resistance 2. Contact tracing and cluster testing for hidden cases. 3. Management of sexual partners with appropriate antibiotics. 4. Vaccination against hepatitis B. 5. Safe and voluntary blood donation and transfusion. 6. Use of barrier contraceptives. 7. Condom promotion campaign. 8. Safe sexual practices (Condom promotion). 16
9. Health education. 10. Universal precautions to be taken by Health Care Workers. 11. Safe disposal of health care waste. 12. Washing of exposed parts with soap and water. 13. Post-exposure prophylaxis in case of exposure to blood, body fluids of patients or pricks. 14. Counselling in high risk group. 17
Salient points to be remembered �Treat as per guidelines �Correct dose �Avoid sex during treatment �Help sexual partners to get treatment �Reduce risk of further acquiring infections (One Partner) �Protect against HIV/AIDS �Follow up �Education & counselling �Condom promotion �If wife pregnant - ANC clinic 18
Control of STDs � Initial Planning - Problem definition - Establishing priorities - Setting objectives - Considering strategies � Intervention strategies (a) Case detection (i) - Screening (ii) - Contact tracing (iii) - Cluster testing (b) Case Holding & Tt (c) Epidemiological treatment (d) Personal prophylaxis (e) H. E. 19
�Support Component - STD clinic - Lab. Services - Primary health care - MIS - Legislation (seek early Tt, name sexual partners, notification by G. P. ) Immoral trafficking (Prevention) Act, 1986 - Social welfare measures- Social therapy Rehabilitation of CSW, Ban on sale and access to pornographic material, healthy living conditions �Monitoring & evaluation 20
High-risk population groups: � STI/RTI services - provided through Targeted Interventions (TIs) to high-risk groups (HRGs). � Three recommended kinds of clinic settings: � TI-owned static clinics for locations with >1, 000 sex workers, , MSM, IDU � Fixed-day, fixed-time outreach clinics for locations with smaller number of sex workers � Referral linkage with government and private STI/RTI service providers in locations with <200 sex workers � TI owned STI/RTI clinics should have either on site laboratory facilities or link up with the nearest government laboratory performing syphilis screening. � ICTC � Referral to ART Centre 21