SERVICE USERLED EDUCATION PROGRAMME TO COUNTER HEALTHCARE PROVIDER


- Slides: 13
SERVICE USER-LED EDUCATION PROGRAMME TO COUNTER HEALTHCARE PROVIDER STEREOTYPES, PREJUDICE AND DISCRIMINATION ASSOCIATED WITH MENTAL DISTRESS End discrimination. Promote recovery, inclusion and respect for human rights.
ABOUT US Dr Sarah Gordon Project Lead / Senior Research Fellow Rachel Tester Project Manager / Research Fellow Dasha Fedchuk Assistant Project Manager / Assistant Research Fellow Jeremy Tumoana Service User Lead Responsiveness to, and inclusiveness of, indigenous Māori peoples Tracey Gardiner Research Assistant Numerous Service User Educators and Two Programme Partners Leadership team comprised of the personnel above, the Convenors of each of the programmes 2
WHY TARGET MEDICAL SCHOOLS? Henderson, C. , Noblett, J. , Parke, H. , Clement, S. , Caffrey, A. , Gale-Grant, O. , . . . & Thornicroft, G. (2014). Mental health-related stigma in health care and mental health-care settings. The Lancet Psychiatry, 1(6), 467 -482. Thornicroft, G. (2011). Physical health disparities and mental illness: the scandal of premature mortality. The British Journal of Psychiatry, 199(6), 441 -442. 3
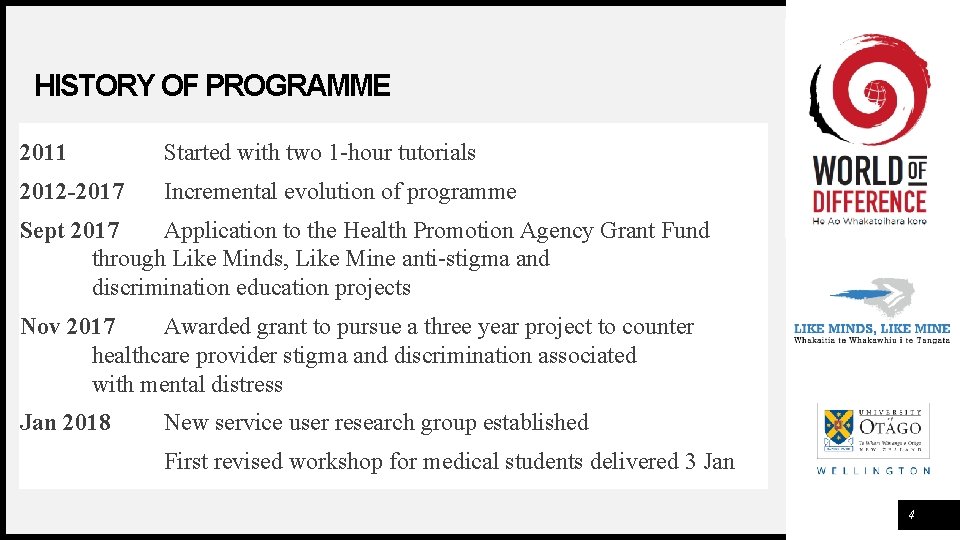
HISTORY OF PROGRAMME 2011 Started with two 1 -hour tutorials 2012 -2017 Incremental evolution of programme Sept 2017 Application to the Health Promotion Agency Grant Fund through Like Minds, Like Mine anti-stigma and discrimination education projects Nov 2017 Awarded grant to pursue a three year project to counter healthcare provider stigma and discrimination associated with mental distress Jan 2018 New service user research group established First revised workshop for medical students delivered 3 Jan 4
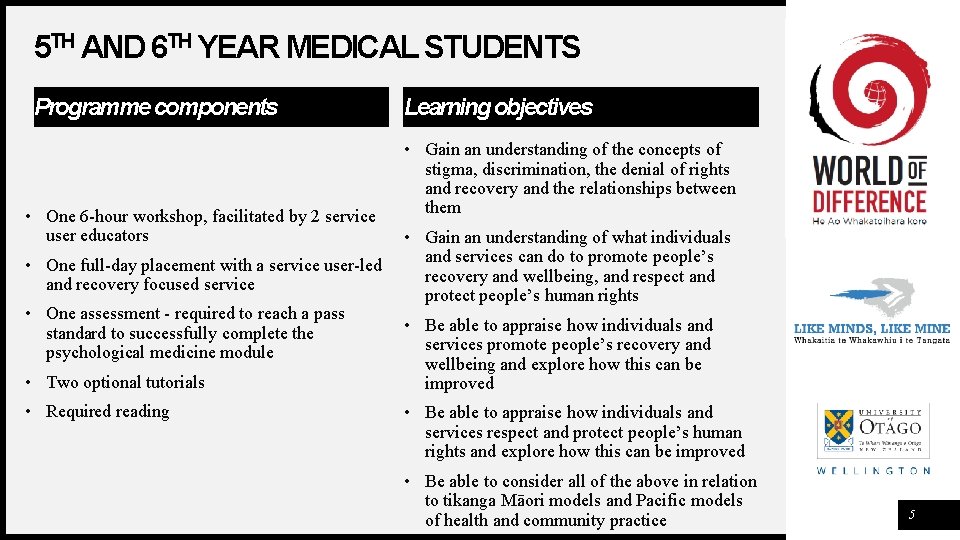
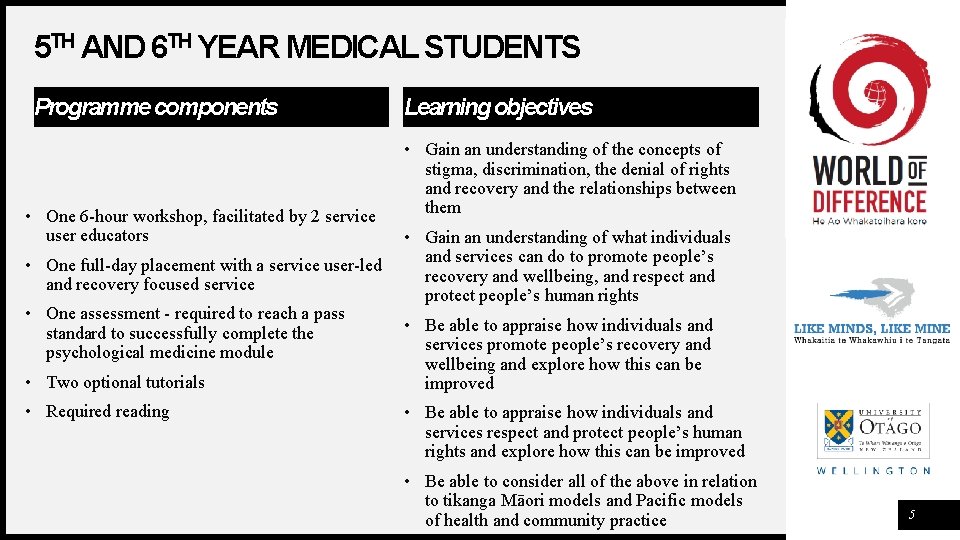
5 TH AND 6 TH YEAR MEDICAL STUDENTS Programme components • One 6 -hour workshop, facilitated by 2 service user educators Learning objectives • Gain an understanding of the concepts of stigma, discrimination, the denial of rights and recovery and the relationships between them • Gain an understanding of what individuals and services can do to promote people’s • One full-day placement with a service user-led recovery and wellbeing, and respect and recovery focused service protect people’s human rights • One assessment - required to reach a pass • Be able to appraise how individuals and standard to successfully complete the services promote people’s recovery and psychological medicine module wellbeing and explore how this can be • Two optional tutorials improved • Required reading • Be able to appraise how individuals and services respect and protect people’s human rights and explore how this can be improved • Be able to consider all of the above in relation to tikanga Māori models and Pacific models of health and community practice 5
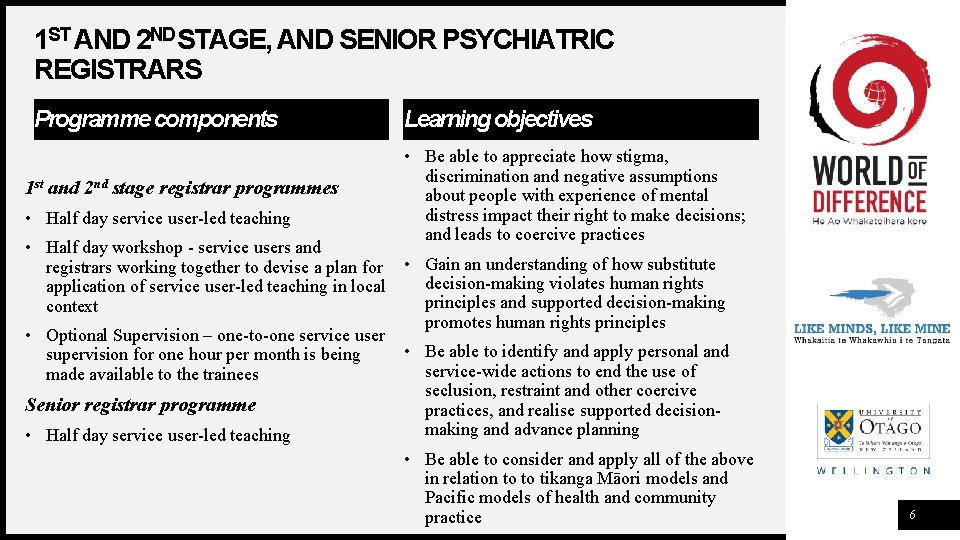
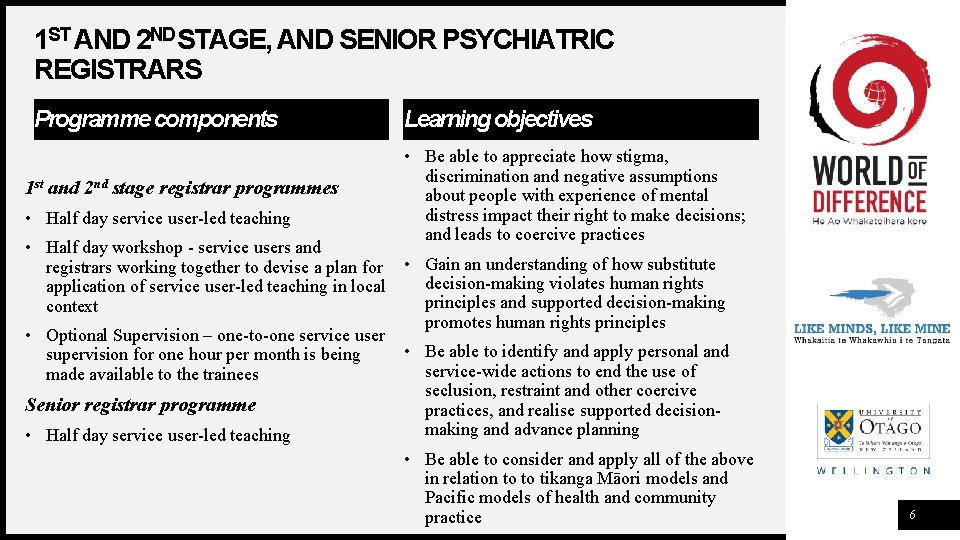
1 ST AND 2 ND STAGE, AND SENIOR PSYCHIATRIC REGISTRARS Programme components 1 st and 2 nd stage registrar programmes • Half day service user-led teaching Learning objectives • Be able to appreciate how stigma, discrimination and negative assumptions about people with experience of mental distress impact their right to make decisions; and leads to coercive practices • Half day workshop - service users and registrars working together to devise a plan for • Gain an understanding of how substitute decision-making violates human rights application of service user-led teaching in local principles and supported decision-making context promotes human rights principles • Optional Supervision – one-to-one service user • Be able to identify and apply personal and supervision for one hour per month is being service-wide actions to end the use of made available to the trainees seclusion, restraint and other coercive Senior registrar programme practices, and realise supported decisionmaking and advance planning • Half day service user-led teaching • Be able to consider and apply all of the above in relation to to tikanga Māori models and Pacific models of health and community practice 6
EVALUATION: QUANTITATIVE 1. Pre/post attitude change evaluation – all programmes • Recovery Attitudes Questionnaire-16 • Opening Minds Stigma Scale for Health Care Providers 7
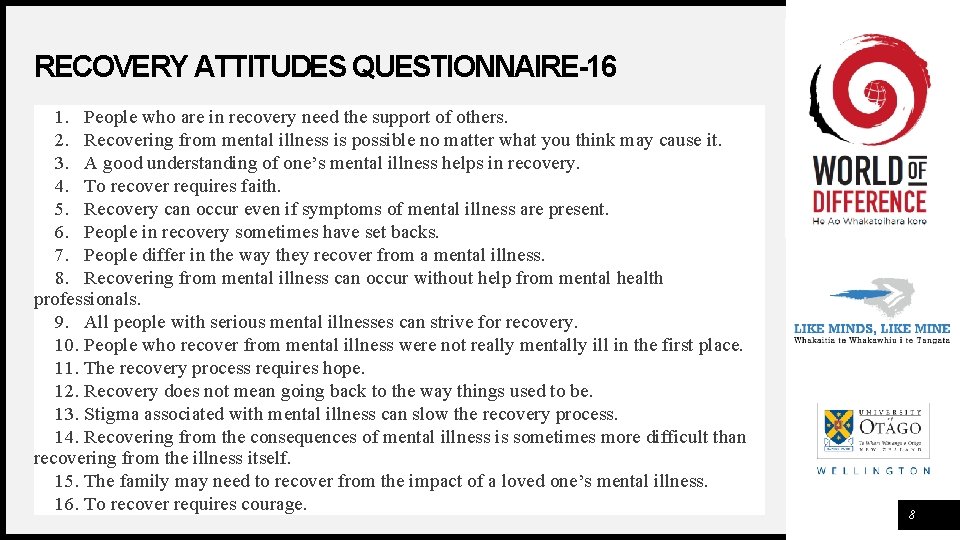
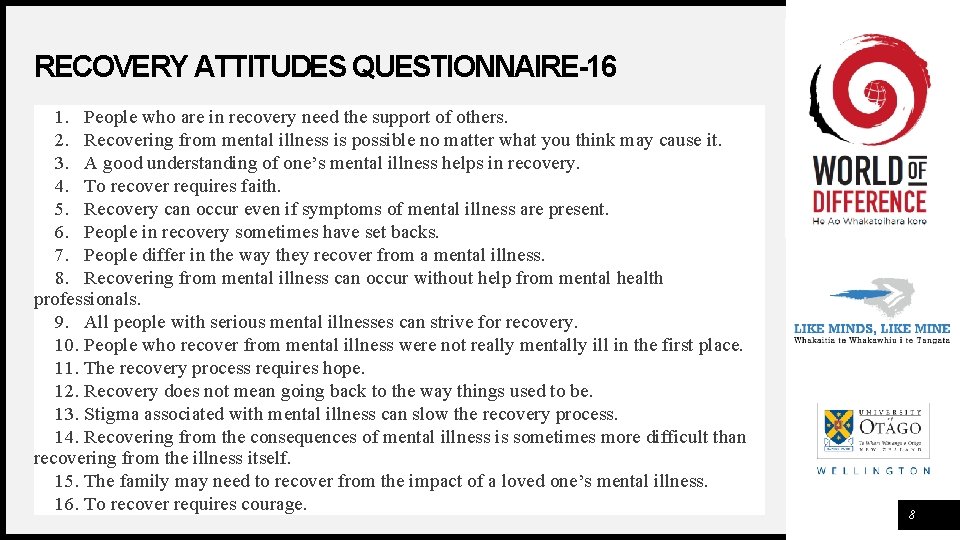
RECOVERY ATTITUDES QUESTIONNAIRE-16 1. People who are in recovery need the support of others. 2. Recovering from mental illness is possible no matter what you think may cause it. 3. A good understanding of one’s mental illness helps in recovery. 4. To recover requires faith. 5. Recovery can occur even if symptoms of mental illness are present. 6. People in recovery sometimes have set backs. 7. People differ in the way they recover from a mental illness. 8. Recovering from mental illness can occur without help from mental health professionals. 9. All people with serious mental illnesses can strive for recovery. 10. People who recover from mental illness were not really mentally ill in the first place. 11. The recovery process requires hope. 12. Recovery does not mean going back to the way things used to be. 13. Stigma associated with mental illness can slow the recovery process. 14. Recovering from the consequences of mental illness is sometimes more difficult than recovering from the illness itself. 15. The family may need to recover from the impact of a loved one’s mental illness. 16. To recover requires courage. 8
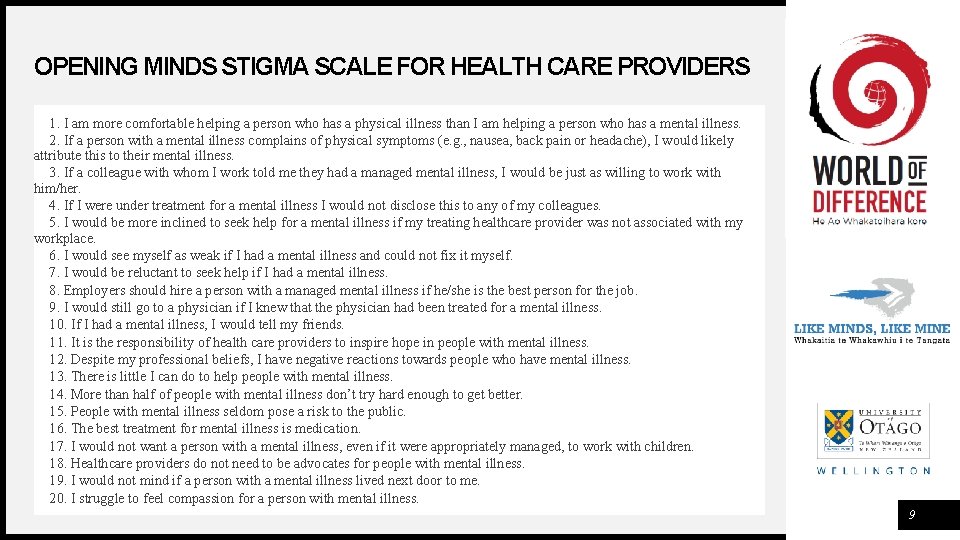
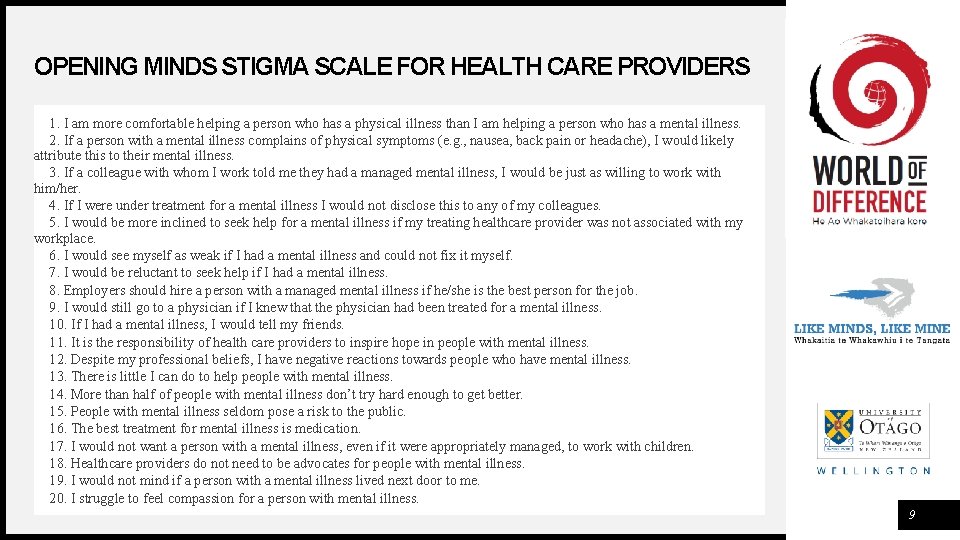
OPENING MINDS STIGMA SCALE FOR HEALTH CARE PROVIDERS 1. I am more comfortable helping a person who has a physical illness than I am helping a person who has a mental illness. 2. If a person with a mental illness complains of physical symptoms (e. g. , nausea, back pain or headache), I would likely attribute this to their mental illness. 3. If a colleague with whom I work told me they had a managed mental illness, I would be just as willing to work with him/her. 4. If I were under treatment for a mental illness I would not disclose this to any of my colleagues. 5. I would be more inclined to seek help for a mental illness if my treating healthcare provider was not associated with my workplace. 6. I would see myself as weak if I had a mental illness and could not fix it myself. 7. I would be reluctant to seek help if I had a mental illness. 8. Employers should hire a person with a managed mental illness if he/she is the best person for the job. 9. I would still go to a physician if I knew that the physician had been treated for a mental illness. 10. If I had a mental illness, I would tell my friends. 11. It is the responsibility of health care providers to inspire hope in people with mental illness. 12. Despite my professional beliefs, I have negative reactions towards people who have mental illness. 13. There is little I can do to help people with mental illness. 14. More than half of people with mental illness don’t try hard enough to get better. 15. People with mental illness seldom pose a risk to the public. 16. The best treatment for mental illness is medication. 17. I would not want a person with a mental illness, even if it were appropriately managed, to work with children. 18. Healthcare providers do not need to be advocates for people with mental illness. 19. I would not mind if a person with a mental illness lived next door to me. 20. I struggle to feel compassion for a person with mental illness. 9
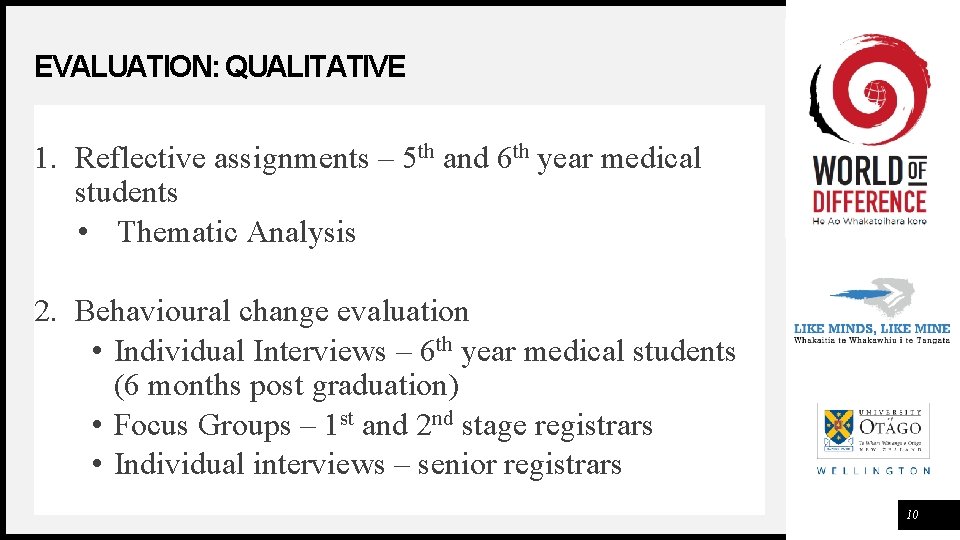
EVALUATION: QUALITATIVE 1. Reflective assignments – 5 th and 6 th year medical students • Thematic Analysis 2. Behavioural change evaluation • Individual Interviews – 6 th year medical students (6 months post graduation) • Focus Groups – 1 st and 2 nd stage registrars • Individual interviews – senior registrars 10

11

12
THANK YOU Dasha Fedchuk +64 04 918 - 5161 Dasha. Fedchuk@otago. ac. nz http: //otago. ac. nz/worldofdifference 13
 Evolution of soa
Evolution of soa Healthcare and the healthcare team chapter 2
Healthcare and the healthcare team chapter 2 Sports medicine definition
Sports medicine definition Vmware service provider program
Vmware service provider program National verifer
National verifer Hospitality service provider
Hospitality service provider Procurement service provider
Procurement service provider Full service provider
Full service provider Dsp service provider
Dsp service provider Primary service provider model
Primary service provider model Microsoft service provider license agreement
Microsoft service provider license agreement Internet telephony service provider
Internet telephony service provider Sales presentation for a managed service provider
Sales presentation for a managed service provider Hkdy service provider
Hkdy service provider