SEPSIS 3 James S Kennedy MD CCS CDIP
- Slides: 13
SEPSIS - 3 James S. Kennedy, MD, CCS, CDIP President and Chief Medical Officer CDIMD – Physician Champions Smyrna, Tennessee jkennedy@cdimd. com – (615) 479 -7021 1
Sepsis Redefinition (Sepsis-3) February 23, 2016 • Announced at the SCCM meeting in Orlando on February 22, 2016 • Published in JAMA on February 23, 2016 http: //www. tinyurl. com/2016 sepsis 2
Sepsis Redefinition February 23, 2016 • Sepsis is now defined as a ‘life-threatening organ dysfunction due to a dysregulated host response to infection’ – In this new definition the concept of the nonhomeostatic host response to infection is strongly stressed while the SIRS criteria have been removed – The inflammatory response accompanying infection (pyrexia, neutrophilia, etc) often represent an appropriate host response to any infection, and this may not necessarily be life-threatening. 3
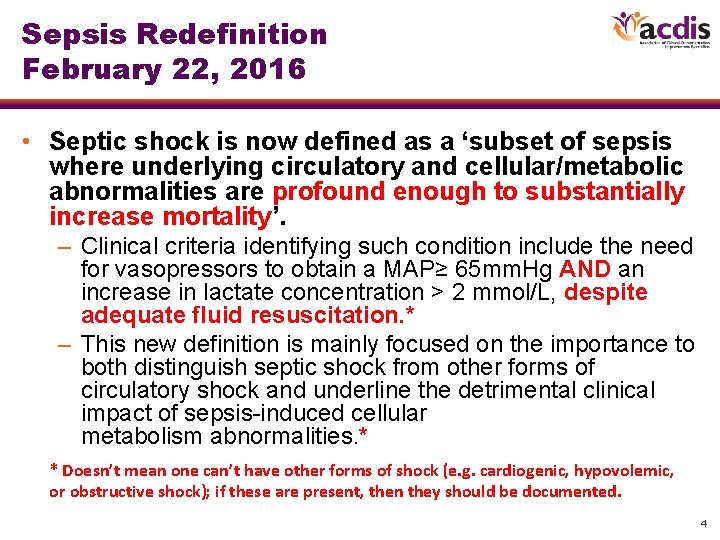
Sepsis Redefinition February 22, 2016 • Septic shock is now defined as a ‘subset of sepsis where underlying circulatory and cellular/metabolic abnormalities are profound enough to substantially increase mortality’. – Clinical criteria identifying such condition include the need for vasopressors to obtain a MAP≥ 65 mm. Hg AND an increase in lactate concentration > 2 mmol/L, despite adequate fluid resuscitation. * – This new definition is mainly focused on the importance to both distinguish septic shock from other forms of circulatory shock and underline the detrimental clinical impact of sepsis-induced cellular metabolism abnormalities. * * Doesn’t mean one can’t have other forms of shock (e. g. cardiogenic, hypovolemic, or obstructive shock); if these are present, then they should be documented. 4
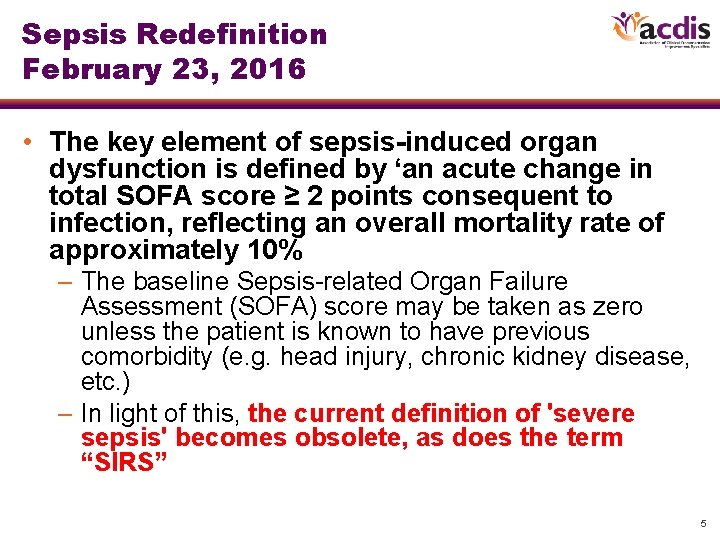
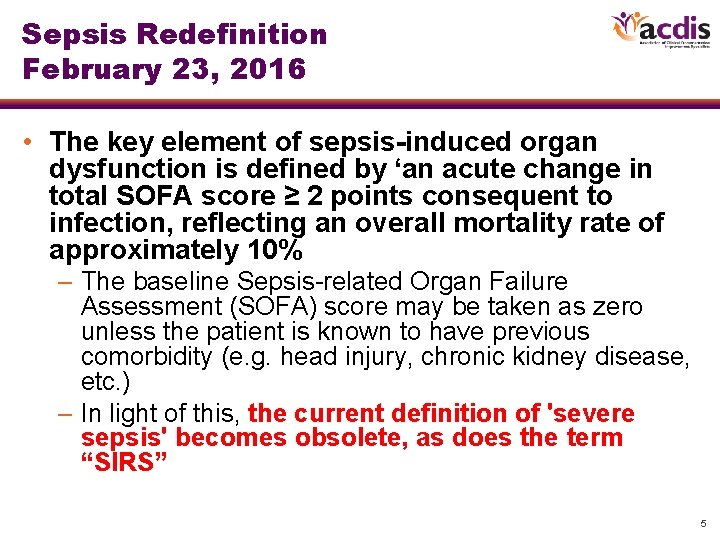
Sepsis Redefinition February 23, 2016 • The key element of sepsis-induced organ dysfunction is defined by ‘an acute change in total SOFA score ≥ 2 points consequent to infection, reflecting an overall mortality rate of approximately 10% – The baseline Sepsis-related Organ Failure Assessment (SOFA) score may be taken as zero unless the patient is known to have previous comorbidity (e. g. head injury, chronic kidney disease, etc. ) – In light of this, the current definition of 'severe sepsis' becomes obsolete, as does the term “SIRS” 5
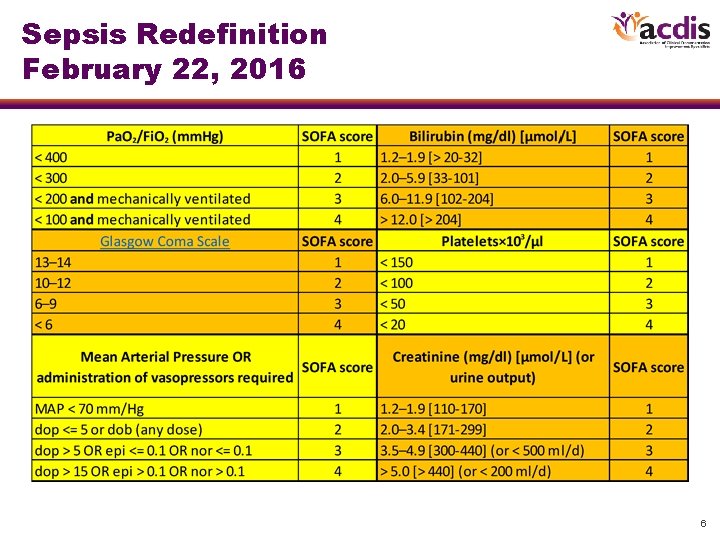
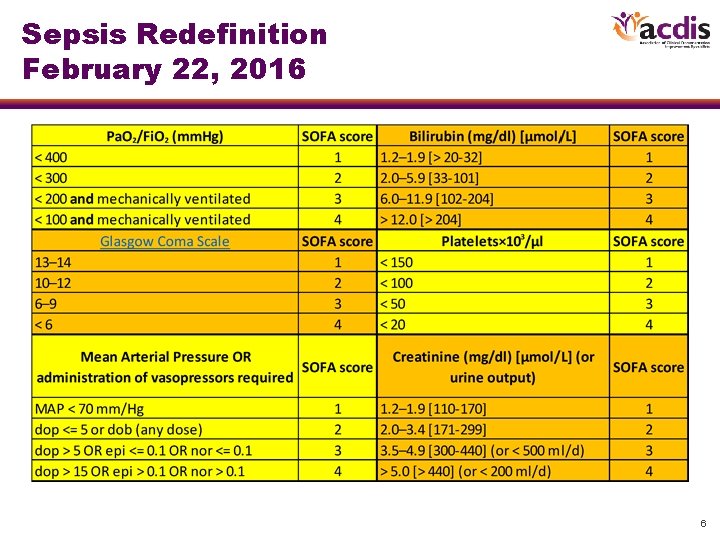
Sepsis Redefinition February 22, 2016 6
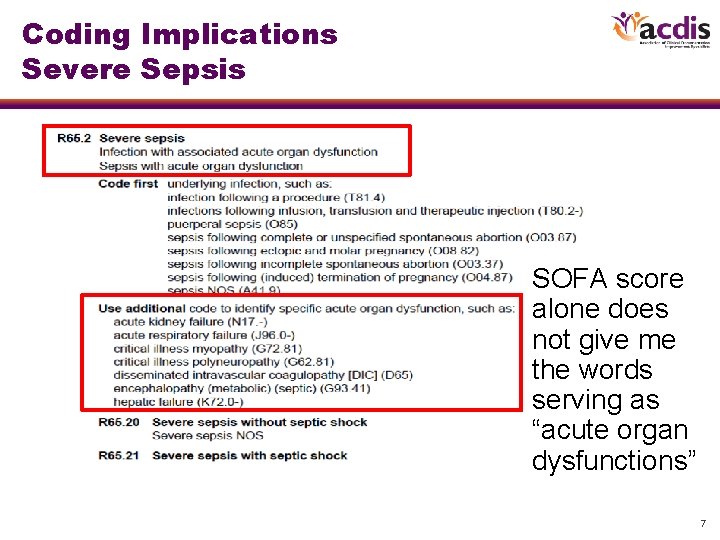
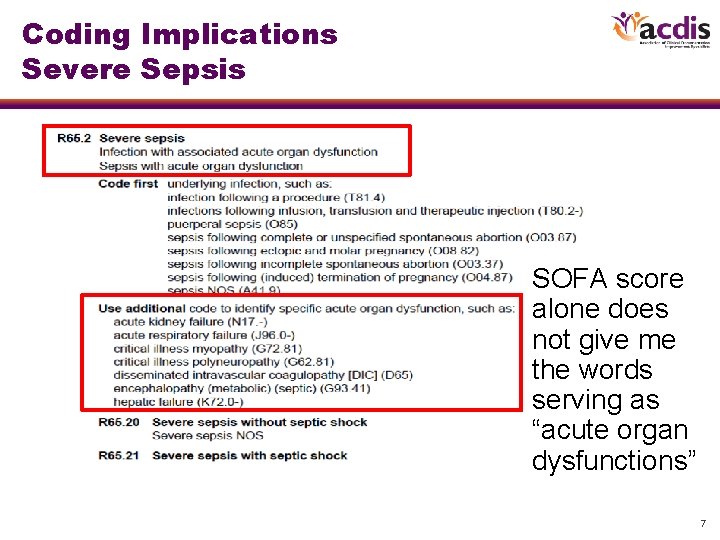
Coding Implications Severe Sepsis SOFA score alone does not give me the words serving as “acute organ dysfunctions” 7
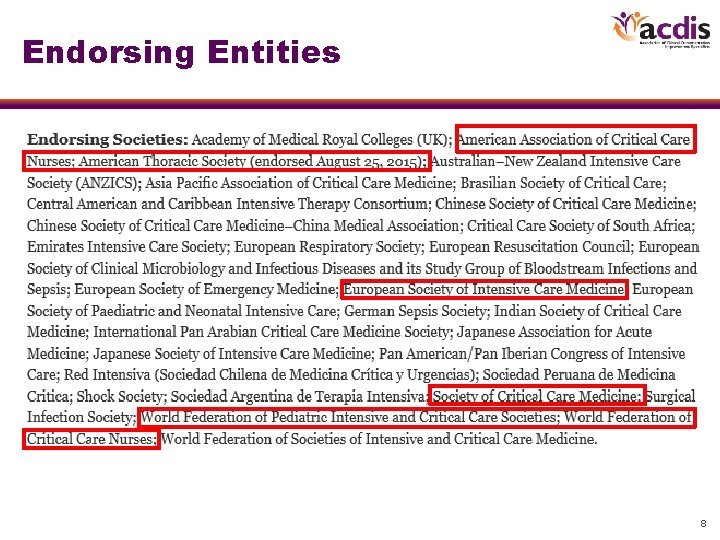
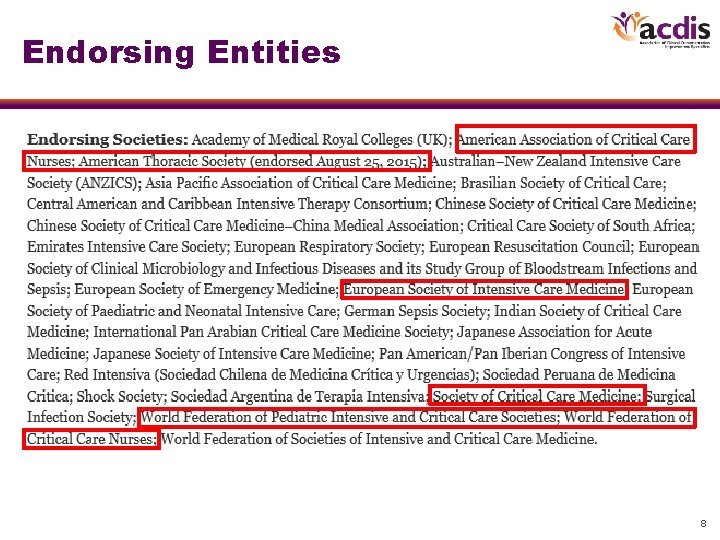
Endorsing Entities. . . 8
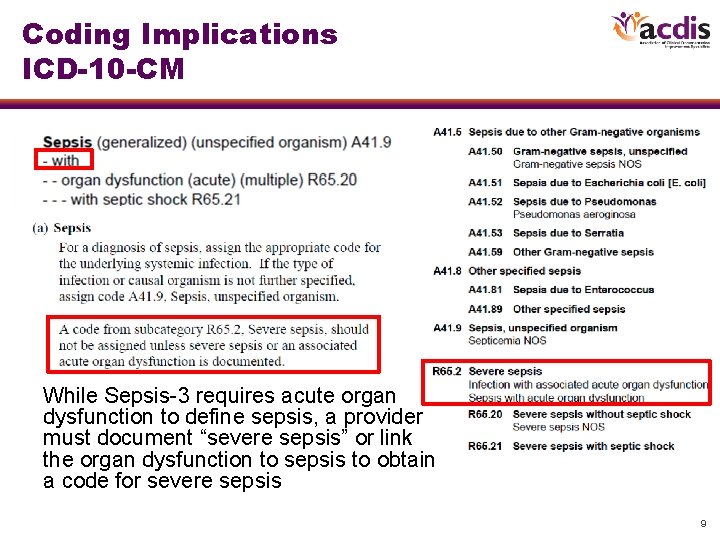
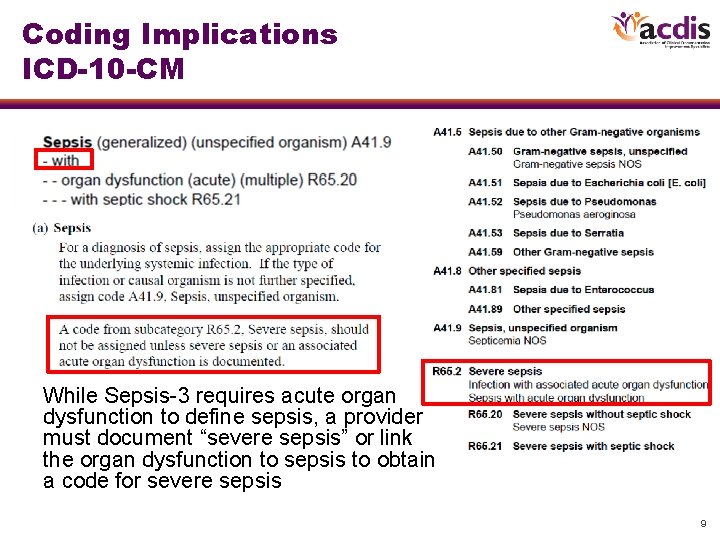
Coding Implications ICD-10 -CM While Sepsis-3 requires acute organ dysfunction to define sepsis, a provider must document “severe sepsis” or link the organ dysfunction to sepsis to obtain a code for severe sepsis 9
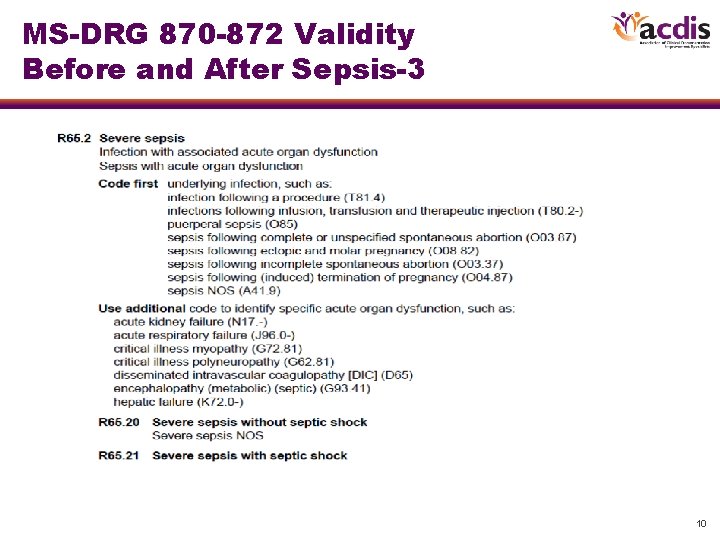
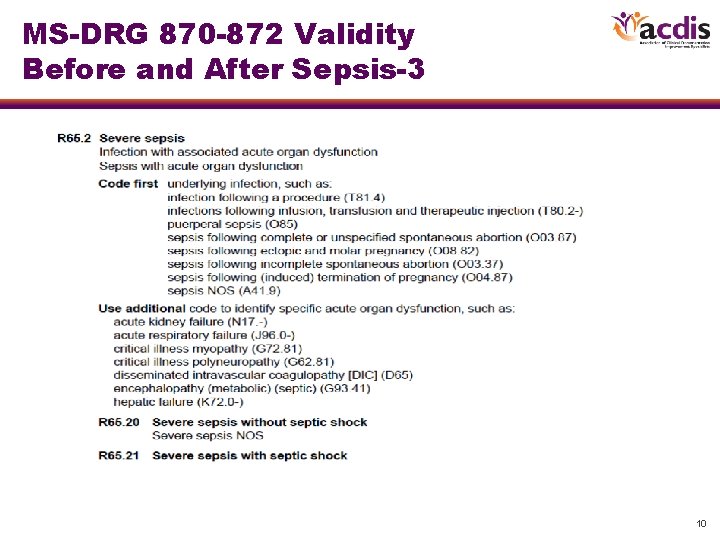
MS-DRG 870 -872 Validity Before and After Sepsis-3 10
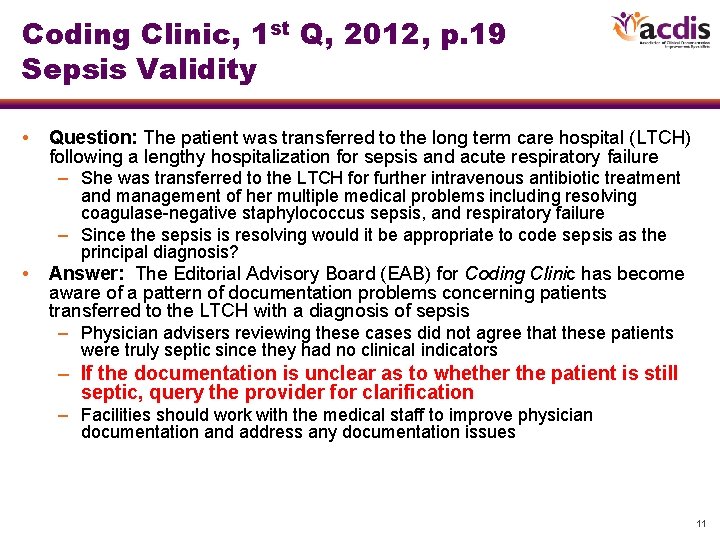
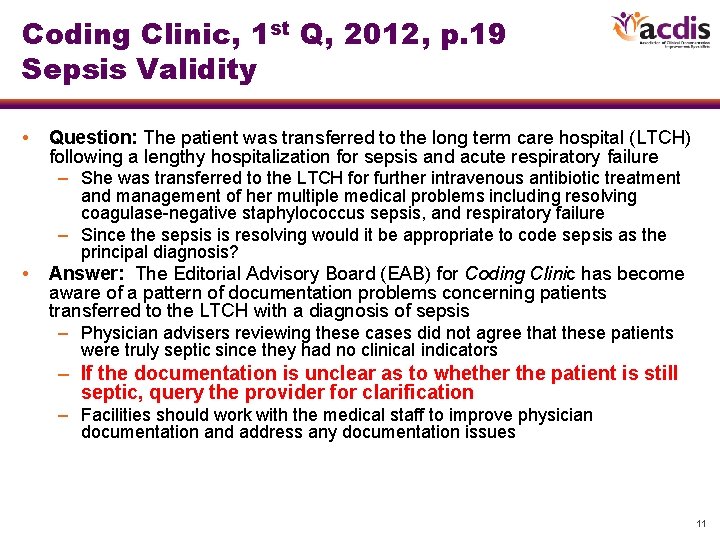
Coding Clinic, 1 st Q, 2012, p. 19 Sepsis Validity • Question: The patient was transferred to the long term care hospital (LTCH) following a lengthy hospitalization for sepsis and acute respiratory failure – She was transferred to the LTCH for further intravenous antibiotic treatment and management of her multiple medical problems including resolving coagulase-negative staphylococcus sepsis, and respiratory failure – Since the sepsis is resolving would it be appropriate to code sepsis as the principal diagnosis? • Answer: The Editorial Advisory Board (EAB) for Coding Clinic has become aware of a pattern of documentation problems concerning patients transferred to the LTCH with a diagnosis of sepsis – Physician advisers reviewing these cases did not agree that these patients were truly septic since they had no clinical indicators – If the documentation is unclear as to whether the patient is still septic, query the provider for clarification – Facilities should work with the medical staff to improve physician documentation and address any documentation issues 11
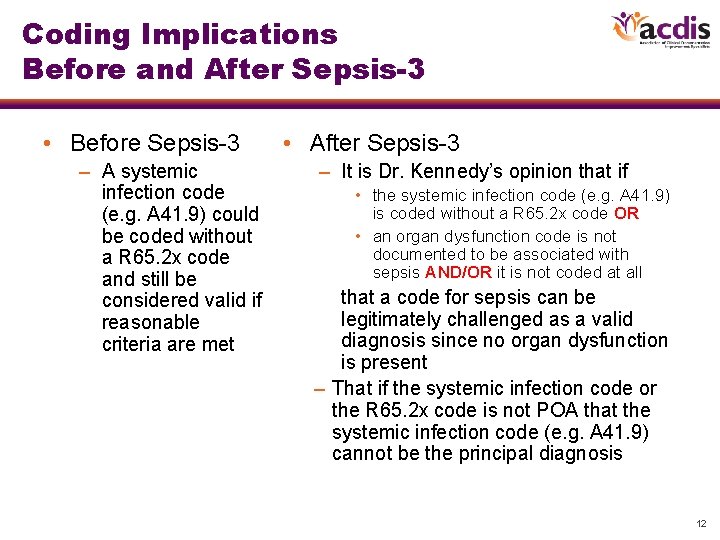
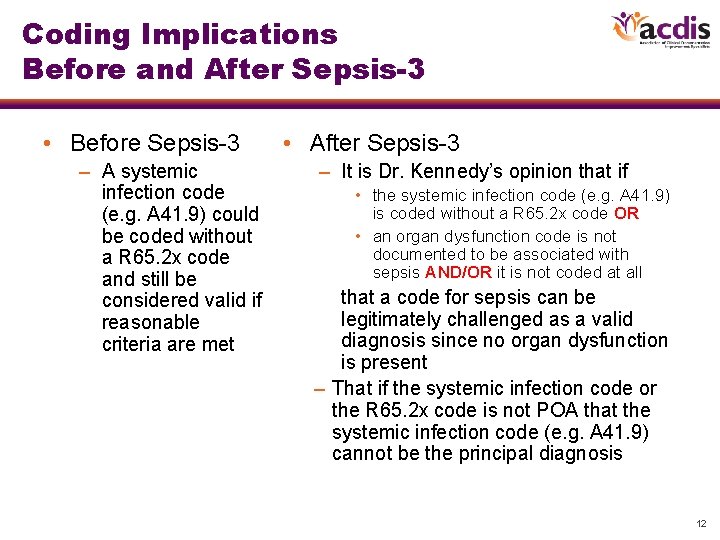
Coding Implications Before and After Sepsis-3 • Before Sepsis-3 – A systemic infection code (e. g. A 41. 9) could be coded without a R 65. 2 x code and still be considered valid if reasonable criteria are met • After Sepsis-3 – It is Dr. Kennedy’s opinion that if • the systemic infection code (e. g. A 41. 9) is coded without a R 65. 2 x code OR • an organ dysfunction code is not documented to be associated with sepsis AND/OR it is not coded at all that a code for sepsis can be legitimately challenged as a valid diagnosis since no organ dysfunction is present – That if the systemic infection code or the R 65. 2 x code is not POA that the systemic infection code (e. g. A 41. 9) cannot be the principal diagnosis 12
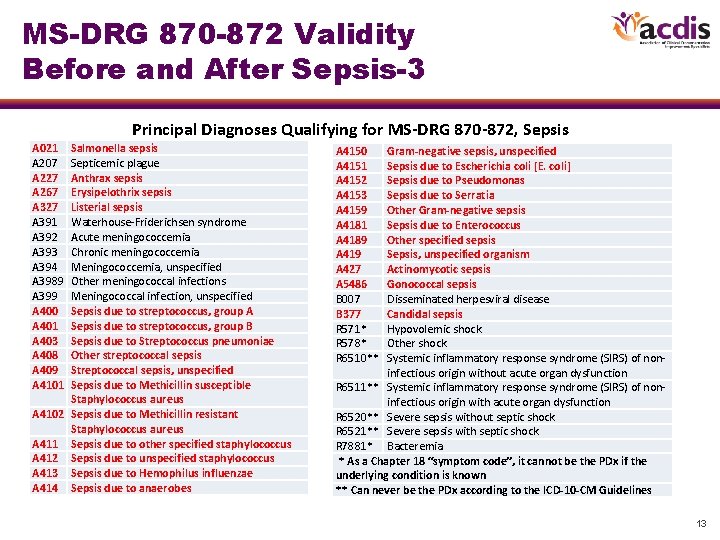
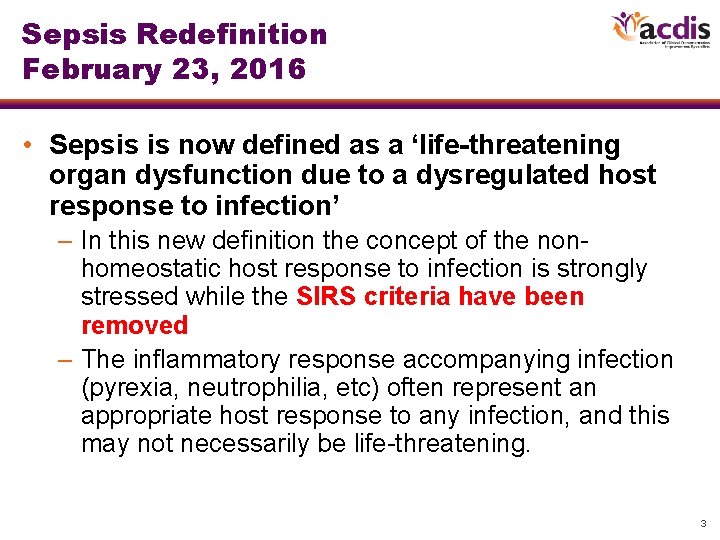
MS-DRG 870 -872 Validity Before and After Sepsis-3 Principal Diagnoses Qualifying for MS-DRG 870 -872, Sepsis A 021 A 207 A 227 A 267 A 327 A 391 A 392 A 393 A 394 A 3989 A 399 A 400 A 401 A 403 A 408 A 409 A 4101 Salmonella sepsis Septicemic plague Anthrax sepsis Erysipelothrix sepsis Listerial sepsis Waterhouse-Friderichsen syndrome Acute meningococcemia Chronic meningococcemia Meningococcemia, unspecified Other meningococcal infections Meningococcal infection, unspecified Sepsis due to streptococcus, group A Sepsis due to streptococcus, group B Sepsis due to Streptococcus pneumoniae Other streptococcal sepsis Streptococcal sepsis, unspecified Sepsis due to Methicillin susceptible Staphylococcus aureus A 4102 Sepsis due to Methicillin resistant Staphylococcus aureus A 411 Sepsis due to other specified staphylococcus A 412 Sepsis due to unspecified staphylococcus A 413 Sepsis due to Hemophilus influenzae A 414 Sepsis due to anaerobes A 4150 A 4151 A 4152 A 4153 A 4159 A 4181 A 4189 A 419 A 427 A 5486 B 007 B 377 R 571* R 578* R 6510** Gram-negative sepsis, unspecified Sepsis due to Escherichia coli [E. coli] Sepsis due to Pseudomonas Sepsis due to Serratia Other Gram-negative sepsis Sepsis due to Enterococcus Other specified sepsis Sepsis, unspecified organism Actinomycotic sepsis Gonococcal sepsis Disseminated herpesviral disease Candidal sepsis Hypovolemic shock Other shock Systemic inflammatory response syndrome (SIRS) of noninfectious origin without acute organ dysfunction R 6511** Systemic inflammatory response syndrome (SIRS) of noninfectious origin with acute organ dysfunction R 6520** Severe sepsis without septic shock R 6521** Severe sepsis with septic shock R 7881* Bacteremia * As a Chapter 18 “symptom code”, it cannot be the PDx if the underlying condition is known ** Can never be the PDx according to the ICD-10 -CM Guidelines 13