SECONDARY ADRENAL INSUFFICIENCY CAUSING VISUAL HALLUCINATIONS MON 453



![References [1] Arlt W, Allolio B. Adrenal Insufficiency. Lancet. 2003; 361: 1881 -1893 [2] References [1] Arlt W, Allolio B. Adrenal Insufficiency. Lancet. 2003; 361: 1881 -1893 [2]](https://slidetodoc.com/presentation_image/11bd22e02c5741d9e785d3523842f617/image-14.jpg)
- Slides: 15
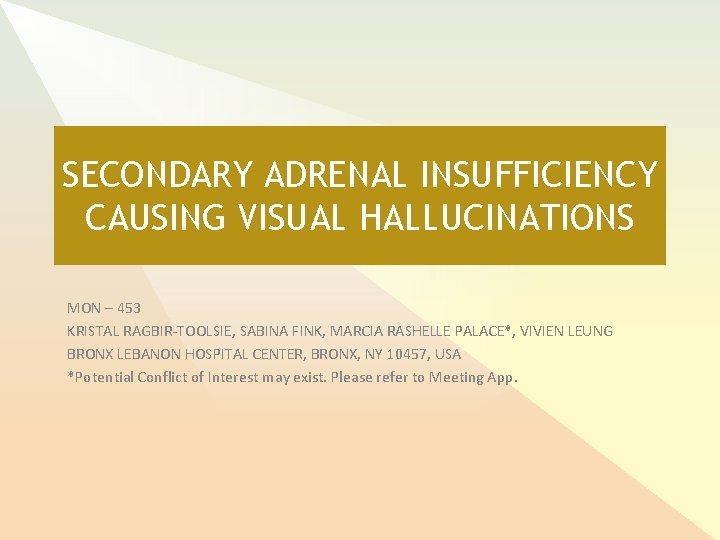
SECONDARY ADRENAL INSUFFICIENCY CAUSING VISUAL HALLUCINATIONS MON – 453 KRISTAL RAGBIR-TOOLSIE, SABINA FINK, MARCIA RASHELLE PALACE*, VIVIEN LEUNG BRONX LEBANON HOSPITAL CENTER, BRONX, NY 10457, USA *Potential Conflict of Interest may exist. Please refer to Meeting App.

Introduction § Secondary Adrenal Insufficiency due to hypothalamic-pituitary failure § Prevalence of 150 -280 per million [1] § Presents with vague symptoms that make the diagnosis challenging. § The psychiatric manifestations of the condition are often overlooked in the clinical setting, though well described in the literature [2 -6].
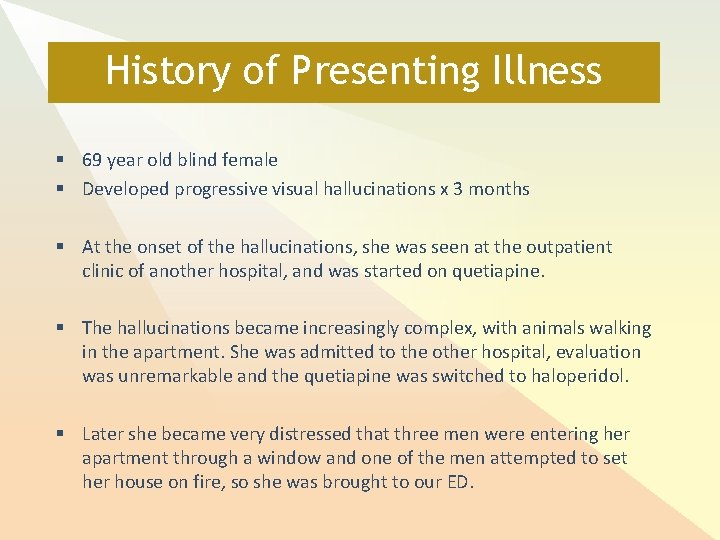
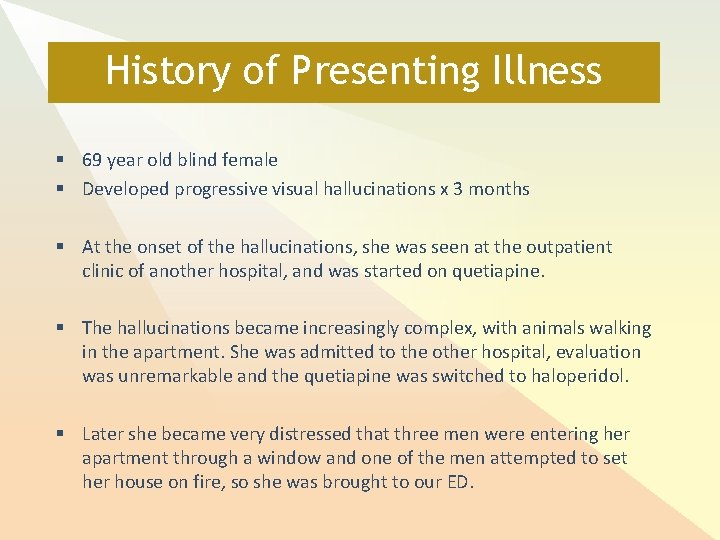
History of Presenting Illness § 69 year old blind female § Developed progressive visual hallucinations x 3 months § At the onset of the hallucinations, she was seen at the outpatient clinic of another hospital, and was started on quetiapine. § The hallucinations became increasingly complex, with animals walking in the apartment. She was admitted to the other hospital, evaluation was unremarkable and the quetiapine was switched to haloperidol. § Later she became very distressed that three men were entering her apartment through a window and one of the men attempted to set her house on fire, so she was brought to our ED.
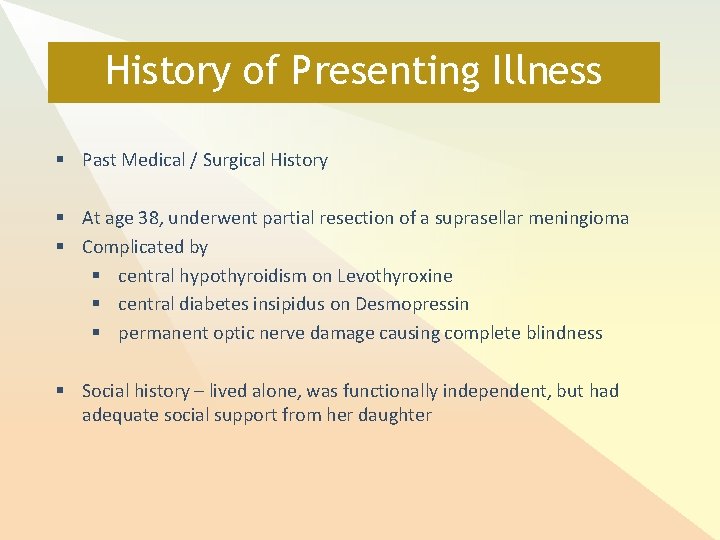
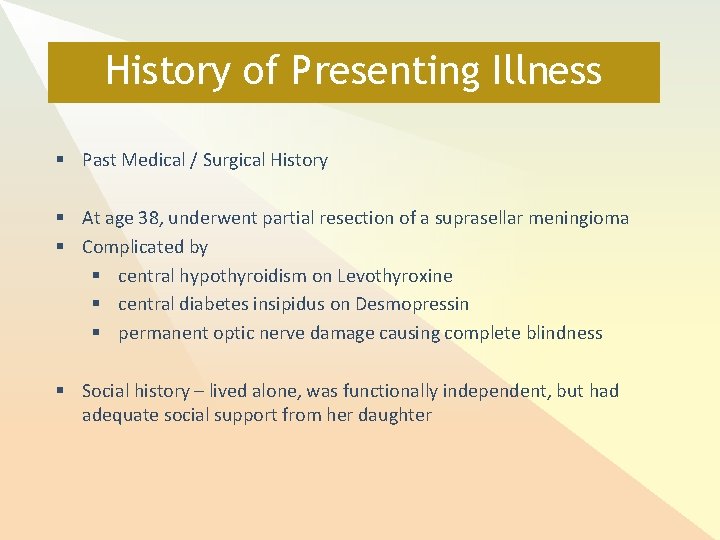
History of Presenting Illness § Past Medical / Surgical History § At age 38, underwent partial resection of a suprasellar meningioma § Complicated by § central hypothyroidism on Levothyroxine § central diabetes insipidus on Desmopressin § permanent optic nerve damage causing complete blindness § Social history – lived alone, was functionally independent, but had adequate social support from her daughter
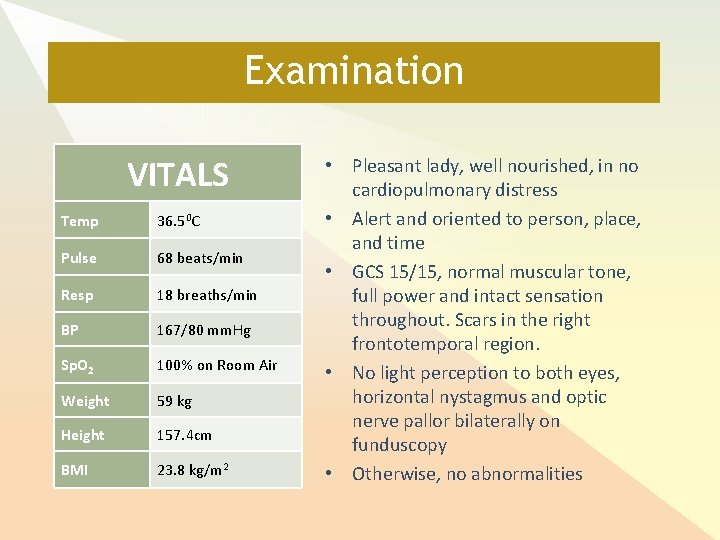
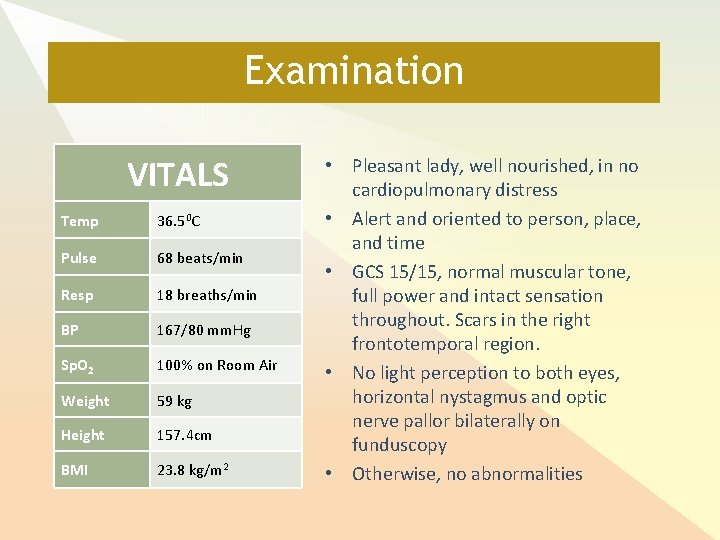
Examination VITALS Temp 36. 50 C Pulse 68 beats/min Resp 18 breaths/min BP 167/80 mm. Hg Sp. O 2 100% on Room Air Weight 59 kg Height 157. 4 cm BMI 23. 8 kg/m 2 • Pleasant lady, well nourished, in no cardiopulmonary distress • Alert and oriented to person, place, and time • GCS 15/15, normal muscular tone, full power and intact sensation throughout. Scars in the right frontotemporal region. • No light perception to both eyes, horizontal nystagmus and optic nerve pallor bilaterally on funduscopy • Otherwise, no abnormalities
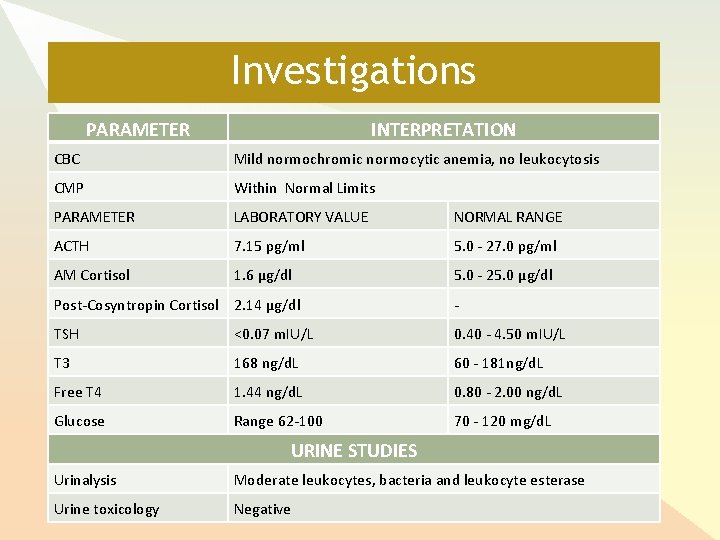
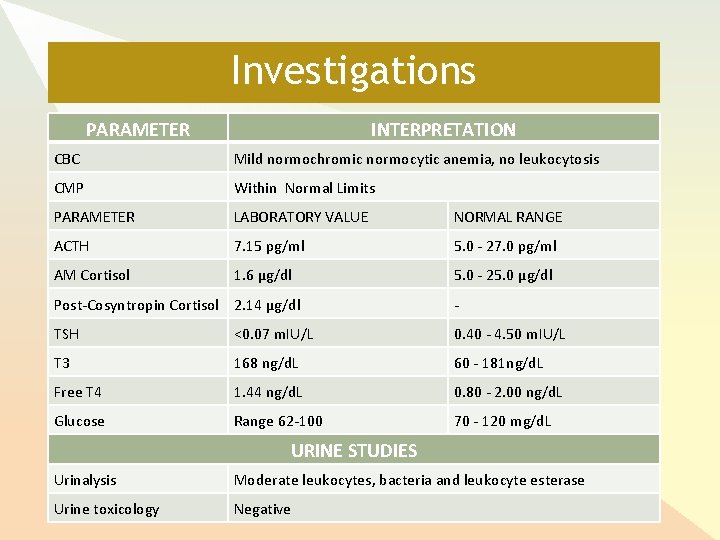
Investigations PARAMETER INTERPRETATION CBC Mild normochromic normocytic anemia, no leukocytosis CMP Within Normal Limits PARAMETER LABORATORY VALUE NORMAL RANGE ACTH 7. 15 pg/ml 5. 0 - 27. 0 pg/ml AM Cortisol 1. 6 μg/dl 5. 0 - 25. 0 μg/dl Post-Cosyntropin Cortisol 2. 14 μg/dl - TSH <0. 07 m. IU/L 0. 40 - 4. 50 m. IU/L T 3 168 ng/d. L 60 - 181 ng/d. L Free T 4 1. 44 ng/d. L 0. 80 - 2. 00 ng/d. L Glucose Range 62 -100 70 - 120 mg/d. L URINE STUDIES Urinalysis Moderate leukocytes, bacteria and leukocyte esterase Urine toxicology Negative

Investigations: CT Head - - - Remote right frontal craniotomy and right frontotemporal craniectomy Post-aneurysmal clipping (two clips were seen in the suprasellar cistern); Partially calcified multilobulated mass in the suprasellar cistern, measuring 3. 1 x 1. 7 x 3. 5 cm. Ex-vacuo dilatation of the right frontal horn, associated with encephalomalacia of the inferior right frontal lobe No acute hemorrhage or infarct. MRI for further evaluation was deferred due to the presence of aneurysm clips.
Investigations • At another institution prior to this admission: • EEG showed cerebral dysfunction • Video EEG reported as normal
Treatment After confirmation of secondary adrenal insufficiency - started oral hydrocortisone 10 mg in AM and 5 mg in PM UTI was treated - Ceftriaxone 1 g IV daily for 5 days. Low normal glucose levels were seen - levels below 70 mg/d. L were corrected with oral glucose and intravenous dextrose administration.
Follow Up At clinic follow up visits: - Reported improvement of hallucinations Far less intrusive tone Marked improvement in appetite Gained weight since discharge

Diagnostic Considerations for Visual Hallucinations Organic causes – Delirium unlikely due to the absence of metabolic derangements and the treatment of presumed urinary tract infection without improvement. Other organic causes such as migraines, seizures, CVA and temporal masses were ruled out. Charles Bonnet Syndrome [7] Seen in blind patients with insight into their blindness. Unlikely, given the duration of her blindness and the acuity of her symptoms. Primary psychiatric diagnosis Unlikely given the lack of psychiatric or substance use history, late onset of psychosis, and acute onset of visual hallucinations. Tried on several different anti-psychotics with no relief in symptomatology
Diagnostic Considerations for Visual Hallucinations Chronic secondary adrenal insufficiency - Normal HPA function post op without overt AI x 3 decades post op - Re-exploration of HPA axis integrity warranted given acute psycosis Labs showed - low baseline cortisol level - insufficient stimulation after corticotrophin injection - Inappropriately low-normal ACTH value Treatment - Glucocorticoid replacement therapy resulted in improvement of symptoms: visual hallucinations, appetite and weight
Conclusions As the presenting symptoms of chronic adrenal insufficiency are often nonspecific, a high index of suspicion for this condition is paramount, especially in patients with prior pituitary surgery. In this patient, visual hallucinations were the only symptom of secondary adrenal insufficiency. Failure to recognize this condition led to mismanagement with ineffective anti-psychotic regimens before the correct diagnosis was made. This case highlights the importance of periodically re-testing HPA axis function in patients with prior pituitary surgery, and re-examining organic causes of hallucinations when multiple anti-psychotic regimens fail.
![References 1 Arlt W Allolio B Adrenal Insufficiency Lancet 2003 361 1881 1893 2 References [1] Arlt W, Allolio B. Adrenal Insufficiency. Lancet. 2003; 361: 1881 -1893 [2]](https://slidetodoc.com/presentation_image/11bd22e02c5741d9e785d3523842f617/image-14.jpg)
References [1] Arlt W, Allolio B. Adrenal Insufficiency. Lancet. 2003; 361: 1881 -1893 [2] Anglin RE, Rosebush PI, Maxurek MF. The Neuropsychiatric Profile of Addison's Disease: Revisiting a Forgotten Phenomenon. J Neuropsychiatry Clin Neurosci. 2006; 18(4): 450 -459 [3] Nwokolo M, Fletcher J. Rare Case of hypopituitarism with psychosis. Endocrinology, Diabetes & Metabolism Case Reports. Published Online: 2013; doi: 10. 1530/EDM-13 -0007 [4] Kate S, Dhanwal DK, Kumar S, et al. Acute psychosis as a presentation of hypopituitarism. BMJ Case Rep. Published Online: 2013; doi: 10. 1136/bcr-2012008516 [5] Abdel-Motleb M. The Neuropsychiatric Aspect of Addison's Disease: A Case Report. Innov Clin Neurosci. 2012; 9(10): 34 -35 [6] Pavlovic A, Sivakumar V. Hypoadrenalism presenting as a range of mental disorders. BMJ Case Reports. Published Online: 2011; doi 10. 1136/bcr. 09. 2010. 3305 [7] Teeple RC, B. S. , Caplan, JP, et al. Visual Hallucinations: Differential Diagnosis and Treatment. Prim Care Companion J Clin Psychiatry. 2009; 11(1): 26 -32
Thank You