Rolling out of SHA 2011 and related Issues
- Slides: 13
Rolling out of SHA 2011 and related Issues A proposed approach Chandika Indikadahena Department of Health governance & financing, WHO, Geneva indikadahenac@who. int 1| OECD (Korea), APNHAN September 2 -3, 2015 – Seoul, Korea
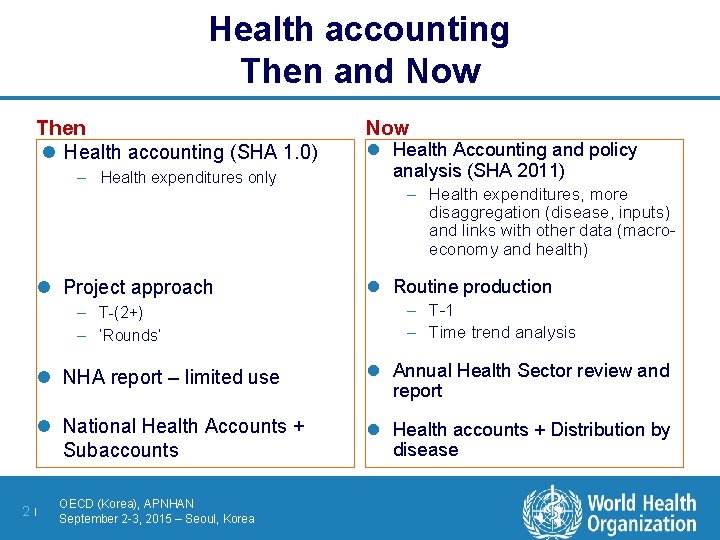
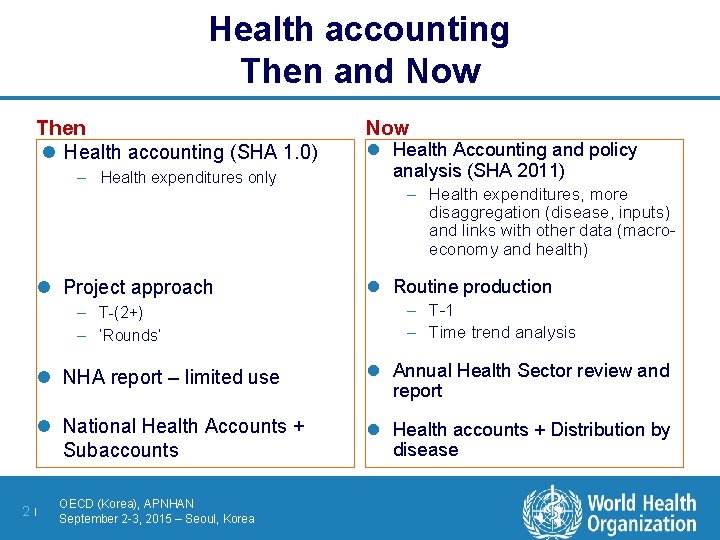
Health accounting Then and Now Then l Health accounting (SHA 1. 0) – Health expenditures only l Project approach – T-(2+) – ‘Rounds’ Now l Health Accounting and policy analysis (SHA 2011) – Health expenditures, more disaggregation (disease, inputs) and links with other data (macroeconomy and health) l Routine production – T-1 – Time trend analysis l NHA report – limited use l Annual Health Sector review and report l National Health Accounts + Subaccounts l Health accounts + Distribution by disease 2| OECD (Korea), APNHAN September 2 -3, 2015 – Seoul, Korea
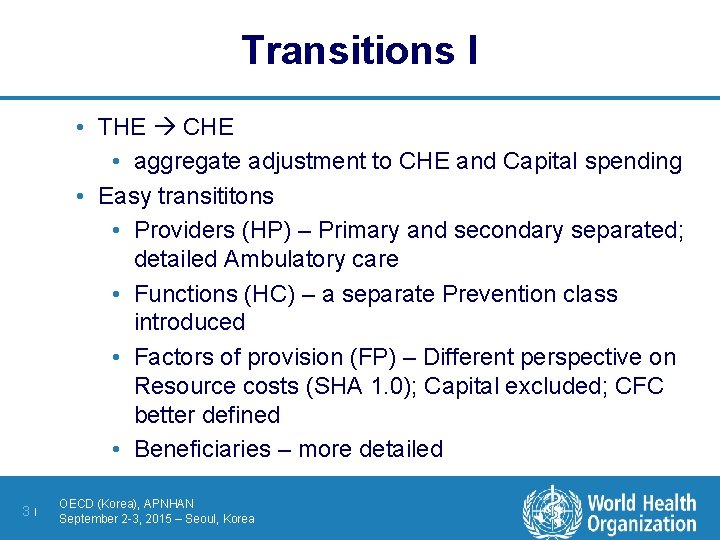
Transitions I • THE CHE • aggregate adjustment to CHE and Capital spending • Easy transititons • Providers (HP) – Primary and secondary separated; detailed Ambulatory care • Functions (HC) – a separate Prevention class introduced • Factors of provision (FP) – Different perspective on Resource costs (SHA 1. 0); Capital excluded; CFC better defined • Beneficiaries – more detailed 3| OECD (Korea), APNHAN September 2 -3, 2015 – Seoul, Korea
Transitions II 4| New concepts / classifiactions • Financing schemes HF • ‘Public – Private’ replaced by ‘compulsary & voluntary’ • Revenues of Schemes (source Revenue of receiver); • More attention paid for external resources (Direct & Indirect) • Capital goods HK • Extended concept of HC. R. 1 (SHA 1. 0) • Closer to SNA concepts • E&T, R&D as Memorandom items OECD (Korea), APNHAN September 2 -3, 2015 – Seoul, Korea
Consequences for data collection l Some classes change their contents – HF, FS, HC. 6 l Some classes change their position – HP. 4 and higher, some FP classes l New variables introduced (HK details) 5| OECD (Korea), APNHAN September 2 -3, 2015 – Seoul, Korea
Target l Shifting to SHA 2011 should not mean losing SHA 1. 0 information available – SHA 1. 0 data can/should be converted to SHA 2011 data l Objective is to produce at least 15 year time series (2000 -2014) of key health financing information (FS, FS. RI, FA, HF) • WHY? to inform policy makers • • 6| sustainability and predictability of funding; government commitment; efforts towards pooling-mechanisms HOW? • by collecting data from the largest two financing actors (Mo. H and households) OECD (Korea), APNHAN September 2 -3, 2015 – Seoul, Korea
Challenges : Backcasting l Easy for existing classifications – Eg. recoding classes l Could be difficult: – For other classifications (or parts) • In case some small items are to be deleted; the data might be difficult to track for earlier years – For new classifications? • Lack of data (new variables were not collected in the past) • Time constraints (digging out data for the past is time consuming) 7| OECD (Korea), APNHAN September 2 -3, 2015 – Seoul, Korea
WHO recommendations l Use SHA 2011 – standard methodology (SHA 2011) – Preferably using HA tools (supports full disease distribution) l yearly health accounts production – data used for annual reviews and budget planning processes – Tools help producing reports l advantages – better data quality (limited human manipulation) – transparency – consistent & harmonized data: across time & countries; by disease l Migration of earlier years to SHA 2011 l 8| To have a 15 year time series OECD (Korea), APNHAN September 2 -3, 2015 – Seoul, Korea
EXPENDITURE BY DISEASE l technically more rigorous than tracking expenditure on one disease only: – standard way to allocate shared expenditures such as health facility expenditures where interventions are being delivered l ensures consistency with TOTAL health expenditure l minimizes multiple parallel data collection initiatives (Saves time/resources) => More value for money (more technically rigorous estimates, at a lower cost) 9| OECD (Korea), APNHAN September 2 -3, 2015 – Seoul, Korea
Why Production Tool (HAPT)? l built in SHA 2011 classifications and beyond – – Flexibility within the framework Supports expenditure by disease (ICD – GBD) Built-in survey questionnaires Promotes Transparency l systematic / qualitative approach – – setting up the accounts data collection mapping them consistency across the years Built-in QC Reduces human errors l sustainable approach – replication of health accounts studies (stability over time) - faster – Institutional memory (addresses staff turnover) – Promotes institutionalization of HA production 10 | OECD (Korea), APNHAN September 2 -3, 2015 – Seoul, Korea
Reports Graphs & tables facilitate checking of results 1) Possibility to sketch expenditure flow by • • data source to send to the data providers; disease to send to the programs; type of provider to send to health care facilities; financier to send institutions (health insurance) or associations (NGOs) • Involves programs focal points; supports access to their expenditure data; helps validate the results 2) Possibility to produce tables per disease/type of provider/ funder/purchaser crossed with inputs or functions etc. • QCs check the coding against knowledge of the system 11 | OECD (Korea), APNHAN September 2 -3, 2015 – Seoul, Korea
ADDITIONAL VALIDATION l Validate against previous years – Conversion of old SHA 1. 0 studies l Compare with averages of regions / income level HEALTH ACCOUNTS REPORTS l Reports are supported with outputs of M 6 of HAPT: – flow of funds chart + standard tables + metadata + QCs l We propose to reduce textual contents in traditional reports ; which sometimes are not policy relevant 12 | OECD (Korea), APNHAN September 2 -3, 2015 – Seoul, Korea
Our Aims are … 1. Improved methodology : including expenditure by disease 2. Improved production process : yearly & timely data 3. Improved quality of data : more systematized process 4. Improved use of results : integrated in policy process 13 | OECD (Korea), APNHAN September 2 -3, 2015 – Seoul, Korea
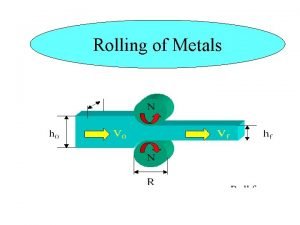
 Pack rolling
Pack rolling Rolling load equation
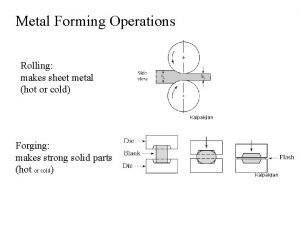
Rolling load equation Hot rolling and cold rolling
Hot rolling and cold rolling Hot rolling and cold rolling
Hot rolling and cold rolling Hot rolling vs cold rolling
Hot rolling vs cold rolling Get out get out get out of my head one direction
Get out get out get out of my head one direction Physical fitness is of two types related and related
Physical fitness is of two types related and related Skill and health related
Skill and health related Unbhr
Unbhr Issues or problems related to local governance/autonomy
Issues or problems related to local governance/autonomy Graphs of trig functions
Graphs of trig functions Csc graph
Csc graph Staying healthy assessment
Staying healthy assessment Sha questionnaire
Sha questionnaire