Racial and ethnic disparities in childhood immunization coverage

- Slides: 21
Racial and ethnic disparities in childhood immunization coverage: United States, 1998 -2003 Lawrence Barker, Ph. D Philip Smith, Ph. D Kate M. Shaw, MS Susan Y. Chu, Ph. D, MSPH Qian Li, BA Jeanne M. Santoli, MD National Immunization Program Centers for Disease Control and Prevention
Acknowledgements • We thank the many people who contribute to the National Immunization Survey (NIS), the data source for these results.
Background • Institute of Medicine finding in Unequal Treatment: “Racial and ethnic disparities in healthcare exist and … are unacceptable. ” • Childhood immunization coverage levels are at all time high levels and racial/ethnic disparities narrowed through the 90’s. • Was this narrowing continuing?

Background and Preview of Results • Racial and ethnic disparities in immunization coverage among preschool children are much smaller than among adults. • We will show that: Disparities in coverage exist among preschool children. • Disparity between black and white children is growing. •
National Immunization Survey (NIS) • RDD telephone survey conducted annually in 50 states and 28 large urban areas • Households screened for children 19 -35 mos of age • Household provides demographic data, including race/ethnicity • Household asked for permission to contact providers • Only provider-validated immunizations are used
NIS, continued • Statistical adjustments for • Non-telephone households • Provider non-response • About 34, 000 interviews completed annually • About 22, 000 with provider validated doses
Coverage measure • 4: 3: 1: 3: 3 coverage • 4+ DTa. P, 3+ polio, 1+ MCV, 3+ Hib, and 3+ hep. B vaccine • Universally recommended vaccines for children by 18 months of age except for newer varicella vaccine and PCV 7
Method to measure disparity trends • Examined trends in the difference in coverage between white and black, white and Hispanic • Used robust regression, an extension of straight line regression
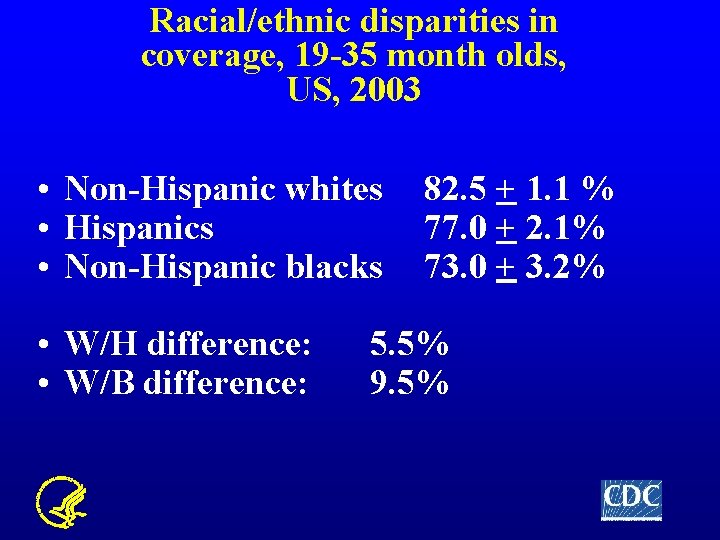
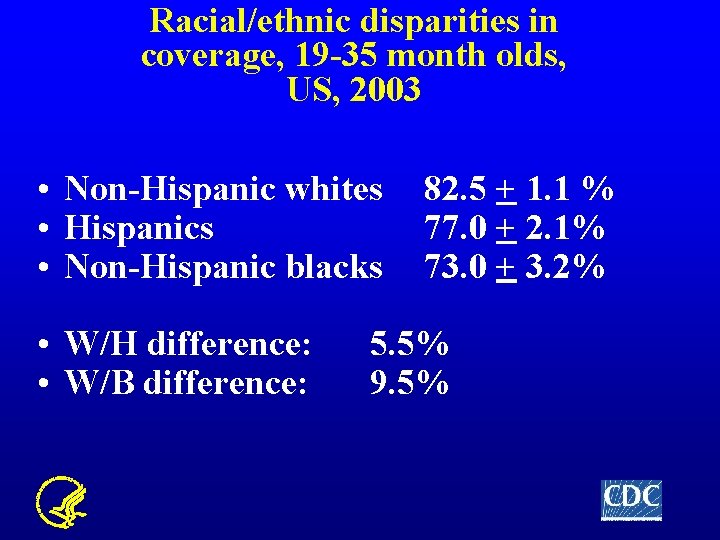
Racial/ethnic disparities in coverage, 19 -35 month olds, US, 2003 • Non-Hispanic whites • Hispanics • Non-Hispanic blacks • W/H difference: • W/B difference: 82. 5 + 1. 1 % 77. 0 + 2. 1% 73. 0 + 3. 2% 5. 5% 9. 5%
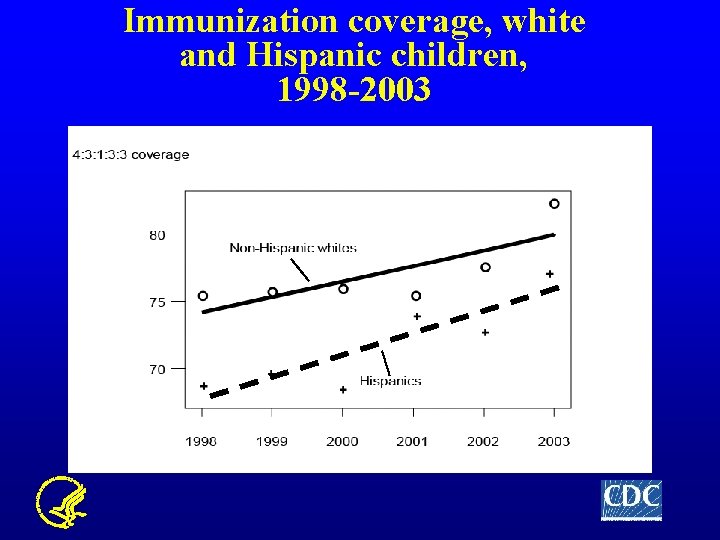
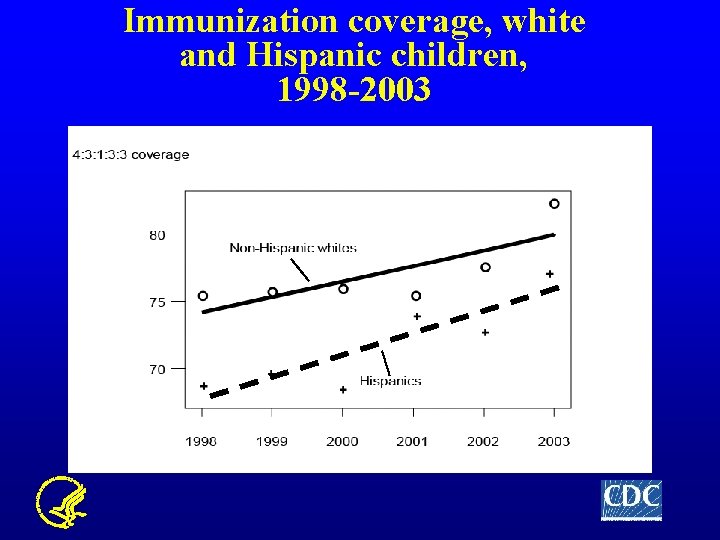
Immunization coverage, white and Hispanic children, 1998 -2003
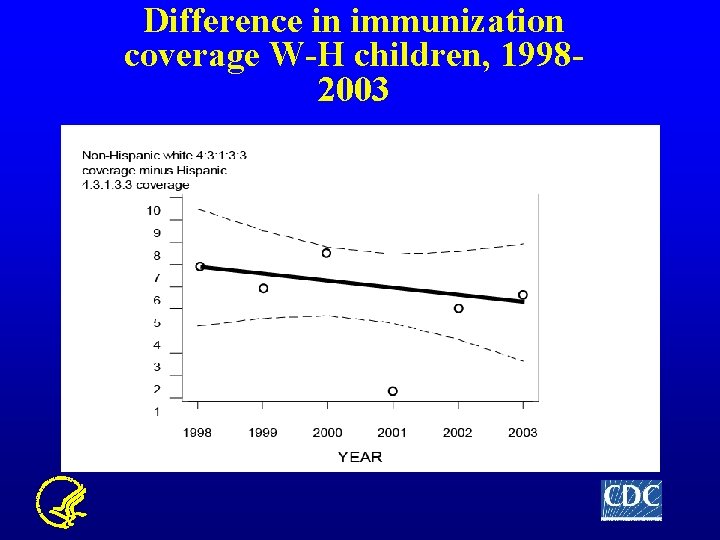
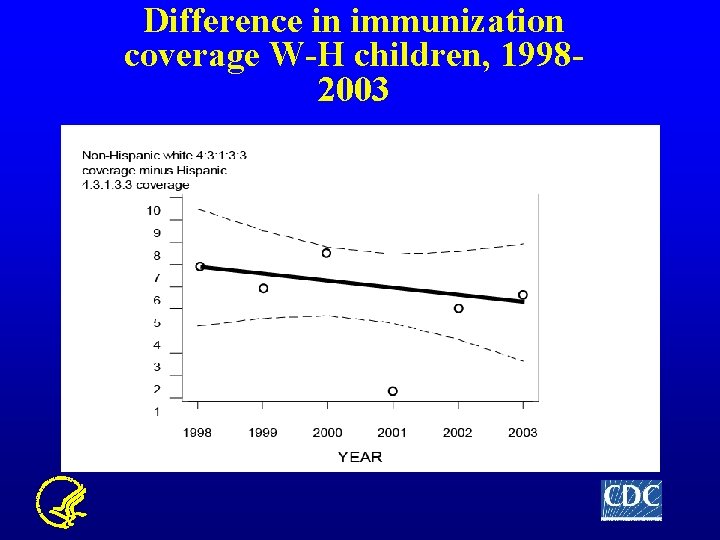
Difference in immunization coverage W-H children, 19982003
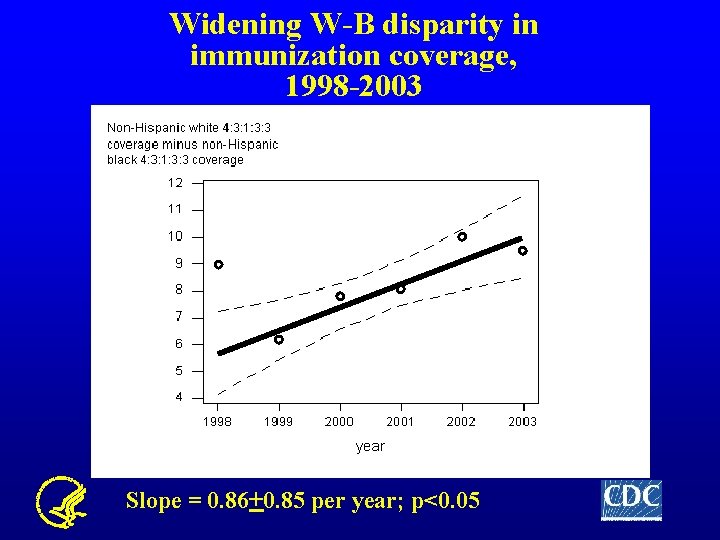
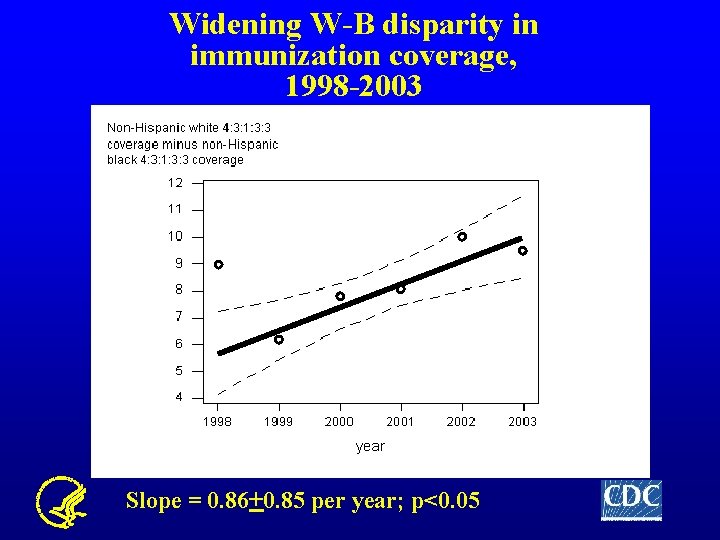
Widening W-B disparity in immunization coverage, 1998 -2003 Slope = 0. 86+0. 85 per year; p<0. 05
Reasons for the widening W-B disparity in coverage? • Preceding results are national level and do not consider differences in SES, etc. • So we explored further by stratifying our results by income; maternal education; marital status; number of providers; type of provider; geographic region • Only difference was that widening was occurring primarily in the NE
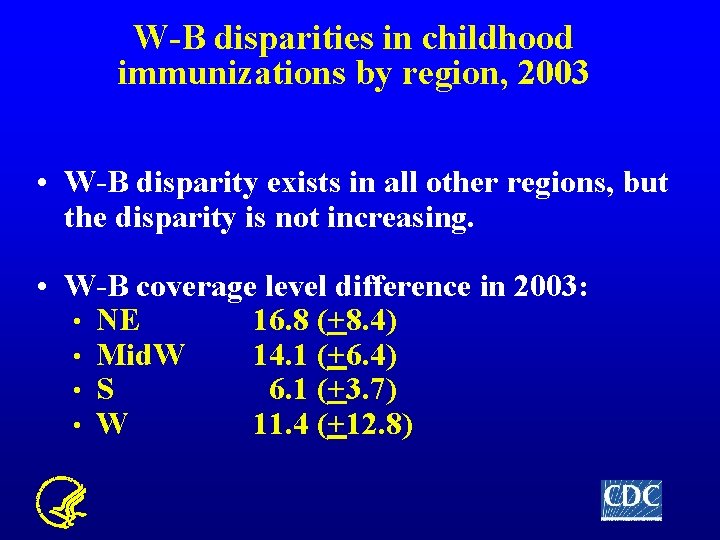
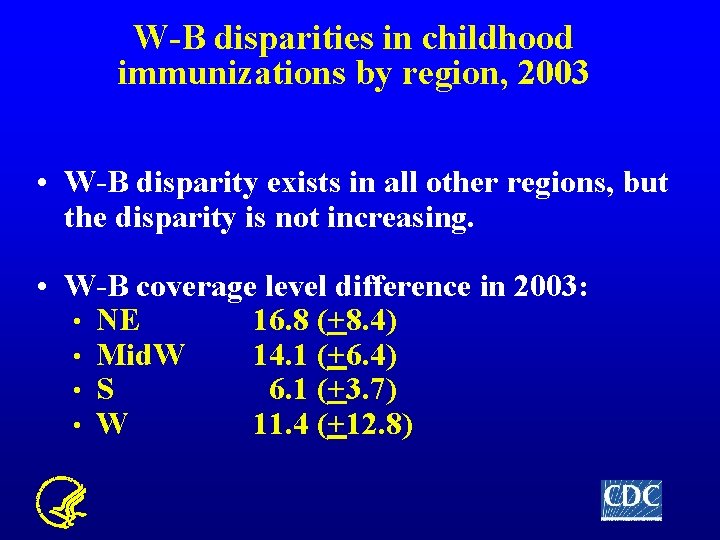
W-B disparities in childhood immunizations by region, 2003 • W-B disparity exists in all other regions, but the disparity is not increasing. • W-B coverage level difference in 2003: • NE 16. 8 (+8. 4) • Mid. W 14. 1 (+6. 4) • S 6. 1 (+3. 7) • W 11. 4 (+12. 8)
W-B disparity increase in the NE • Was the increasing W-B disparity related to increasing poverty? • No. • The percentage of black children living in poverty in the NE did not increase between 1998 -2003
Increasing W-B Disparity in the NE Region, 1998 -2003 • In fact, the W-B disparity was not increasing among children living below poverty • Could reflect impact of entitlement programs such as VFC • But the W-B disparity was increasing among children living at or above poverty
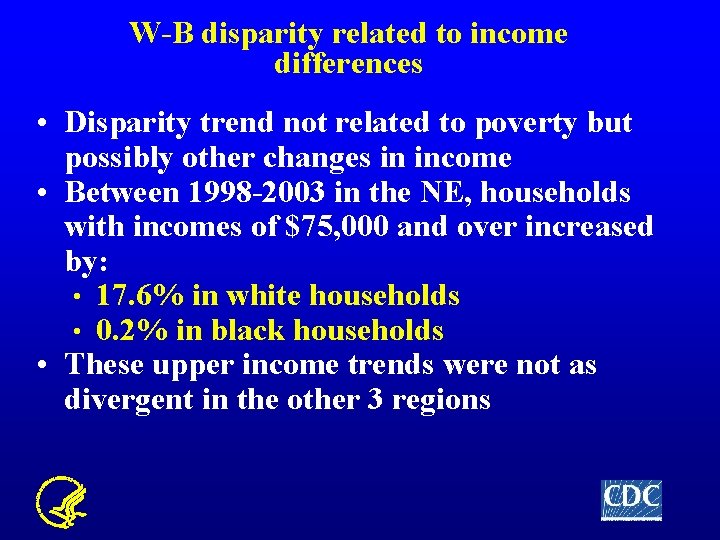
W-B disparity related to income differences • Disparity trend not related to poverty but possibly other changes in income • Between 1998 -2003 in the NE, households with incomes of $75, 000 and over increased by: • 17. 6% in white households • 0. 2% in black households • These upper income trends were not as divergent in the other 3 regions
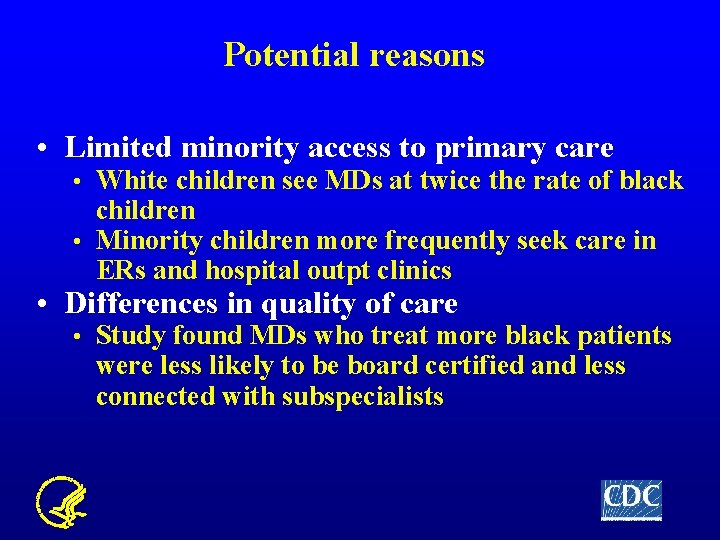
Potential reasons • Limited minority access to primary care White children see MDs at twice the rate of black children • Minority children more frequently seek care in ERs and hospital outpt clinics • • Differences in quality of care • Study found MDs who treat more black patients were less likely to be board certified and less connected with subspecialists
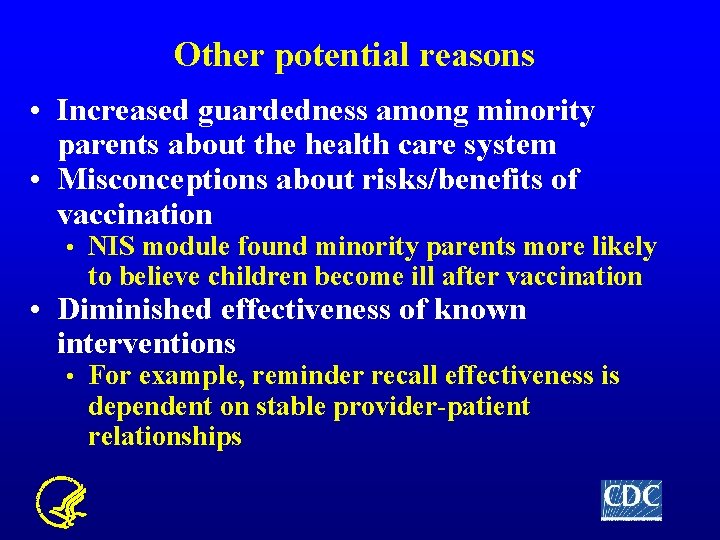
Other potential reasons • Increased guardedness among minority parents about the health care system • Misconceptions about risks/benefits of vaccination • NIS module found minority parents more likely to believe children become ill after vaccination • Diminished effectiveness of known interventions • For example, reminder recall effectiveness is dependent on stable provider-patient relationships
Childhood Immunization Disparities Workgroup • Formed by NIP in August 2004; Lead by Maureen Kolasa • Objective: to address racial and ethnic disparities in immunization coverage among US preschool children • Compiling existing information • Identifying data gaps • Planning future analyses, new collaborations and research projects
Conclusion The childhood immunization program is one of the great public health successes. Coverage is at all time highs, and disparities had been narrowing. This is a call to action – persistent and, in some places, growing disparities need to be addressed. If childhood immunizations are showing these trends, likely other health programs are at risk of reversing previous closing gaps.
 Chapter 10 racial and ethnic relations review worksheet
Chapter 10 racial and ethnic relations review worksheet Chapter 10 racial and ethnic relations
Chapter 10 racial and ethnic relations Chapter 10 racial and ethnic relations review worksheet
Chapter 10 racial and ethnic relations review worksheet Early childhood and middle childhood
Early childhood and middle childhood Chapter 3 health wellness and health disparities
Chapter 3 health wellness and health disparities Maternal and infant health disparities
Maternal and infant health disparities 30-30-30 model of health disparities
30-30-30 model of health disparities Health disparities meaning
Health disparities meaning Health disparities meaning
Health disparities meaning Non malficence
Non malficence Black studies and the racial mountain
Black studies and the racial mountain Jim crow laws in what region or regions did it exist
Jim crow laws in what region or regions did it exist Racial wealth gap simulation
Racial wealth gap simulation Promoting racial literacy in schools
Promoting racial literacy in schools Anti imperialist league apush
Anti imperialist league apush Racial prejudice
Racial prejudice Don tiburcio de espadaña symbolism
Don tiburcio de espadaña symbolism Racial insults
Racial insults Chapter 16 section 3 segregation and discrimination
Chapter 16 section 3 segregation and discrimination Cartel ley organica contra la discriminacion racial
Cartel ley organica contra la discriminacion racial Democracia racial
Democracia racial Lesson 2 discrimination
Lesson 2 discrimination