Pyelonephritis Key Points Pyelonephritis is an infection and





- Slides: 20

Pyelonephritis

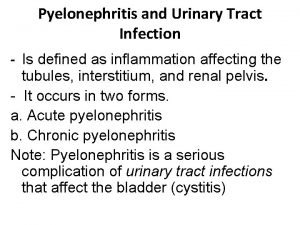
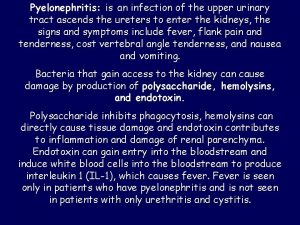
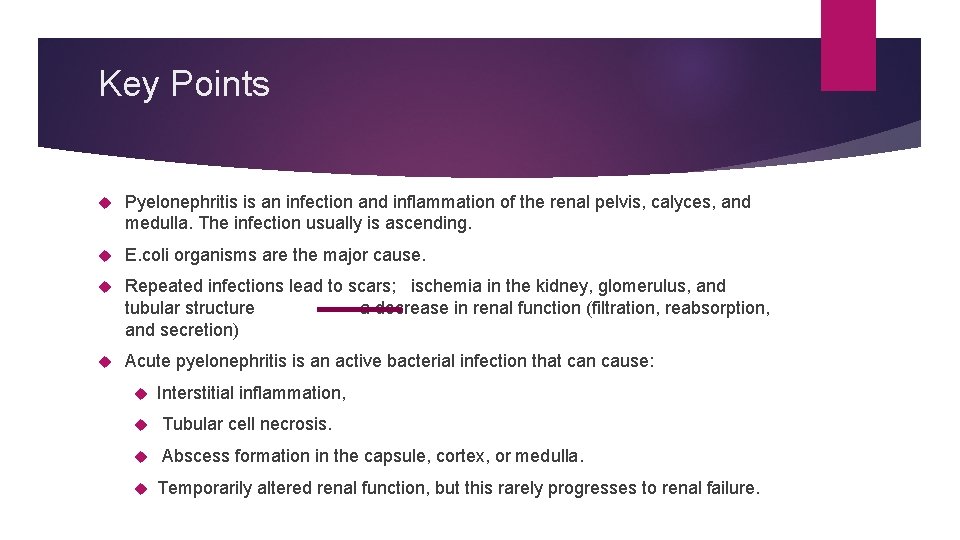
Key Points Pyelonephritis is an infection and inflammation of the renal pelvis, calyces, and medulla. The infection usually is ascending. E. coli organisms are the major cause. Repeated infections lead to scars; ischemia in the kidney, glomerulus, and tubular structure a decrease in renal function (filtration, reabsorption, and secretion) Acute pyelonephritis is an active bacterial infection that can cause: Interstitial inflammation, Tubular cell necrosis. Abscess formation in the capsule, cortex, or medulla. Temporarily altered renal function, but this rarely progresses to renal failure.
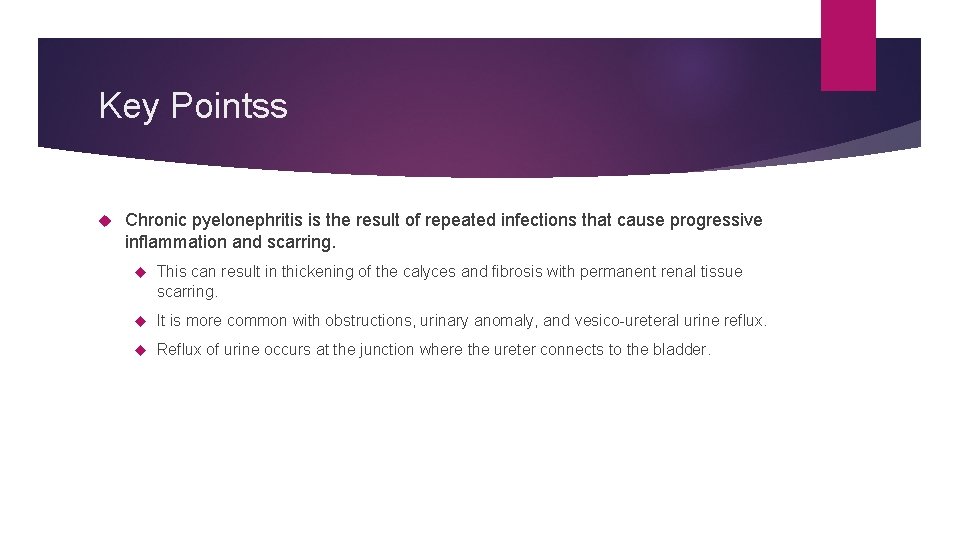
Key Pointss Chronic pyelonephritis is the result of repeated infections that cause progressive inflammation and scarring. This can result in thickening of the calyces and fibrosis with permanent renal tissue scarring. It is more common with obstructions, urinary anomaly, and vesico-ureteral urine reflux. Reflux of urine occurs at the junction where the ureter connects to the bladder.
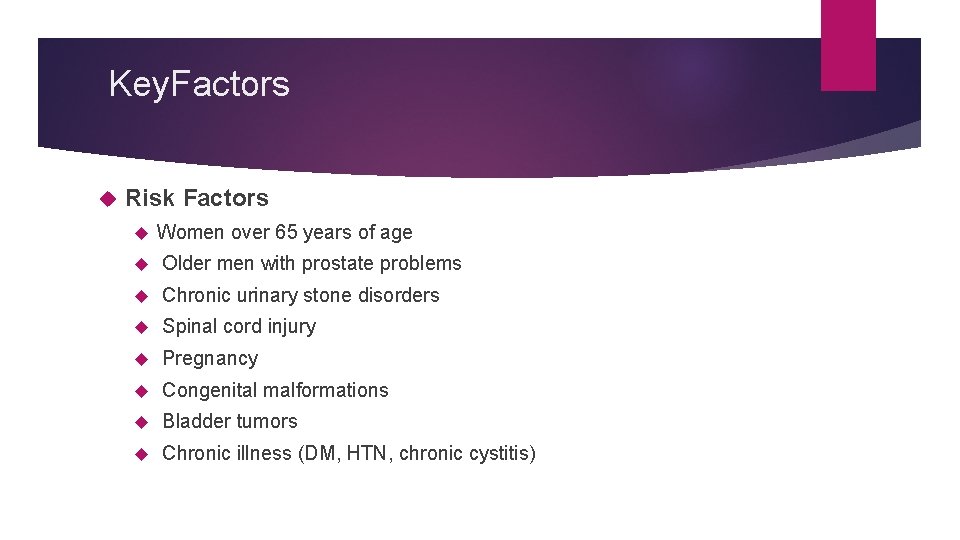
Key. Factors Risk Factors Women over 65 years of age Older men with prostate problems Chronic urinary stone disorders Spinal cord injury Pregnancy Congenital malformations Bladder tumors Chronic illness (DM, HTN, chronic cystitis)
Diagnostic procedures and Nursing Interventions Urinalysis and urine culture and sensitivity (clean catch, urethral cath, suprapubic needle aspiration) Dark color, cloudy appearance, foul odor. Bacturia, sediment, WBCs, & RBCs. Positive leukocyte esterase (85 to 90% specific). Positive nitrate (95% specific). protineuria WBC count and differential: White blood cell count at or above 10, 000/mm 3 with shift to the left indicates increased number of immature cells in response to infection. Blood cultures will be positive for the presence of bacteria if a systemic infection is present.
Diagnostic procedures and Nursing Interventions KFT: creatinine & BUN are elevated during acute episodes and consistently elevated with chronic infection. C-reactive protein is elevated during exacerbating inflammatory processes. ESR is elevated during acute or chronic inflammation.
Diagnostic procedures and Nursing Interventions CT scanning - To identify alterations in renal parenchymal perfusion; alterations in contrast excretion, perinephric fluid, and nonrenal disease; gas-forming infections; hemorrhage; inflammatory masses; and obstruction MRI – To detect renal infection or masses and urinary obstruction, as well as to evaluate renal vasculature Ultrasonography - To screen for urinary obstruction in children admitted for febrile illnesses and to examine patients for renal abscesses, acute focal bacterial nephritis, and stones X-ray of kidneys, ureters, and bladder (KUB) may demonstrate calculi or structural abnormalities. Intravenous pyelogram (IVP) may demonstrate calculi, structural, or vascular abnormalities. Assess renal function and allergy to contrast dye prior to the procedure. Bowel preparation may be prescribed prior to the procedure for image clarity. Hydration prior to the procedure and diuretic administration following the procedure may be prescribed to reduce the risk of nephrotoxicity. Gallium scan may indicate active pyelonephritis or abscesses.

Diagnostic procedures and Nursing Interventions Surgical procedures may be needed to terminate the infectious process. Pyelolithotomy Nephrectomy – removal of a stone from the kidney – removal of the kidney Ureteral diversion or re-implantation of the ureter to restore bladder drainage Ureteroplasty – repair or revision of the ureter

Assessment The classic presentation in patients with acute pyelonephritis is as follows: Fever - This is not always present, but when it is, it is not unusual for the temperature to exceed 39. 4°C Tachycardia, tachypnea, hypertension, Chills Costovertebral angle pain - Pain may be mild, moderate, or severe; flank or costovertebral angle tenderness is most commonly unilateral over the involved kidney, although bilateral discomfort may be present Nausea and/or vomiting - These vary in frequency and intensity, from absent to severe; anorexia is common in patients with acute pyelonephritis Gross hematuria (hemorrhagic cystitis), unusual in males with pyelonephritis, occurs in 30 -40% of females, most often young women. Burning, urgency, and frequency with urination Nocturia
Assessment Inability to concentrate urine or conserve sodium (chronic pyelonephritis) The classic manifestations of acute pyelonephritis observed in adults are often absent in children, particularly neonates and infants. In children aged 2 years or younger, the most common signs and symptoms of urinary tract infection (UTI) are as follows: Failure to thrive Feeding difficulty Fever Vomiting
Assess/Monitor Nutritional status Intake and output Fluid and electrolyte balance Pain status
NANDANursing. Diagnoses Acute pain Deficient knowledge Activity intolerance Anxiety Impaired urinary elimination
Nursing. Interventions Manage pain. Narcotic analgesics Non-steroidal anti-inflammatory agents (NSAIDs)
Nursing. Interventions Antibiotic therapy (IV) according to C&S is essential in the treatment of acute pyelonephritis and prevents progression of the infection Patients presenting with complicated pyelonephritis should be managed as inpatients and treated empirically with broad-spectrum parenteral antibiotics Maintain antibiotic schedules to maximize medication effectiveness. Teach self-administration of prescribed medications. Increase fluid intake to 2 to 3 L/day unless contraindicated. Monitor temperature and administer antipyretic as needed. Provide emotional support. Assist with personal hygiene.
Nursing. Interventions In addition to antibiotics, surgery may be necessary to treat the following manifestations of acute pyelonephritis: Renal cortical abscess (renal carbuncle): Surgical drainage (if patients do not respond to antibiotic therapy); other surgical options are enucleation of the carbuncle and nephrectomy Renal corticomedullary abscess: Incision and drainage, nephrectomy Perinephric abscess: Drainage, nephrectomy Calculi-related urinary tract infection (UTI): Extracorporeal shockwave lithotripsy (ESWL) or endoscopic, percutaneous, or open surgery Renal papillary necrosis: CT scan guided drainage or surgical drainage with debridement Xanthogranulomatous pyelonephritis: Nephrectomy
Complicationsand. Nursing. Implications Septic Shock Initiate life-support interventions as needed. Renal Failure Monitor intake and output. Monitor renal function studies for elevations in BUN and creatinine. Identify signs, such as hypotension, tachycardia, and fever. Encourage increased fluid intake. Hypertension Monitor blood pressure for trends. Report changes from baseline.

 Chapter 10 crafting the brand positioning
Chapter 10 crafting the brand positioning Point of difference and point of parity
Point of difference and point of parity Nitrofurantonin
Nitrofurantonin Pyelonephritis
Pyelonephritis Post streptococcal glomerulonephritis
Post streptococcal glomerulonephritis Necrosis
Necrosis Pyelonephritis causes
Pyelonephritis causes Tabaxin
Tabaxin Benign nephrosclerosis pathology outlines
Benign nephrosclerosis pathology outlines Pyelonephritis
Pyelonephritis Pyelonep
Pyelonep Py/o medical term
Py/o medical term Peylonephritis
Peylonephritis Cysto pyelonephritis
Cysto pyelonephritis Nursing management of pyelonephritis
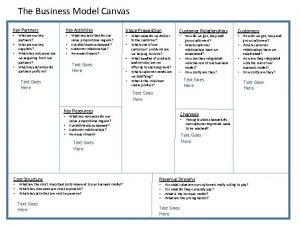
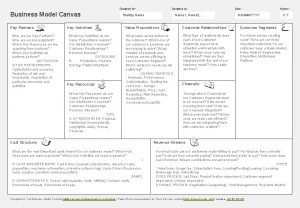
Nursing management of pyelonephritis Example of business model
Example of business model Key partners
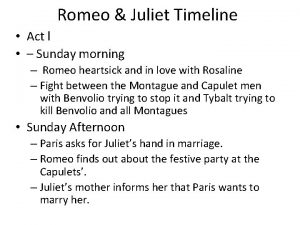
Key partners Timeline for romeo and juliet
Timeline for romeo and juliet Key points of romeo and juliet
Key points of romeo and juliet Main themes of romeo and juliet
Main themes of romeo and juliet Understanding points lines and planes answer key
Understanding points lines and planes answer key