Providing respectful highquality care in Tshwane District Midwife
- Slides: 22
Providing respectful, high-quality care in Tshwane District Midwife Obstetric units: Implementation of a context-adaptable intervention package Sarie Oosthuizen 1, Anne-Marie Bergh 2, Robert Pattinson 2 1 Tshwane District Health Services and Department of Family Medicine, University of Pretoria 2 SAMRC Unit for Maternal and Infant Health Care Strategies, University of Pretoria 14 th Annual Conference, Society of Midwives of South Africa Klerksdorp, 22 -25 August 2017
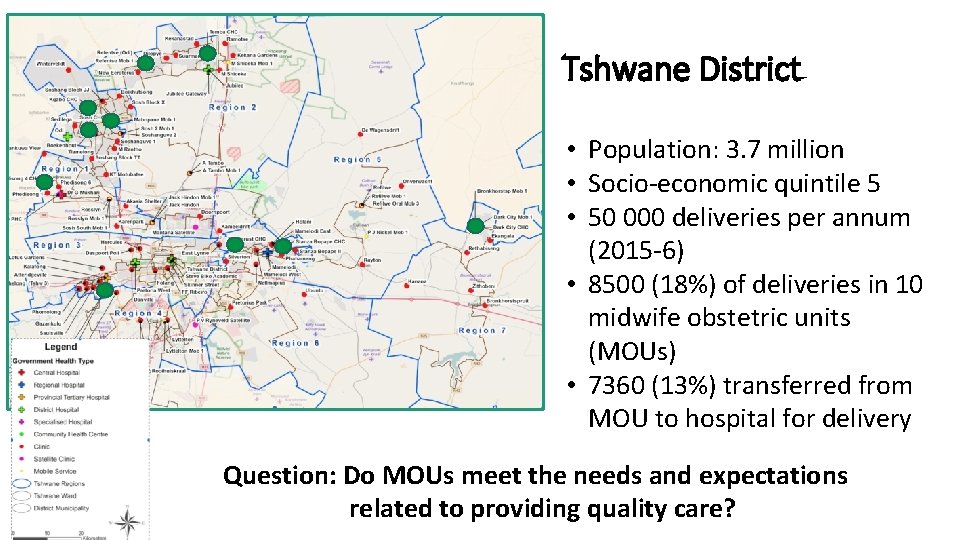
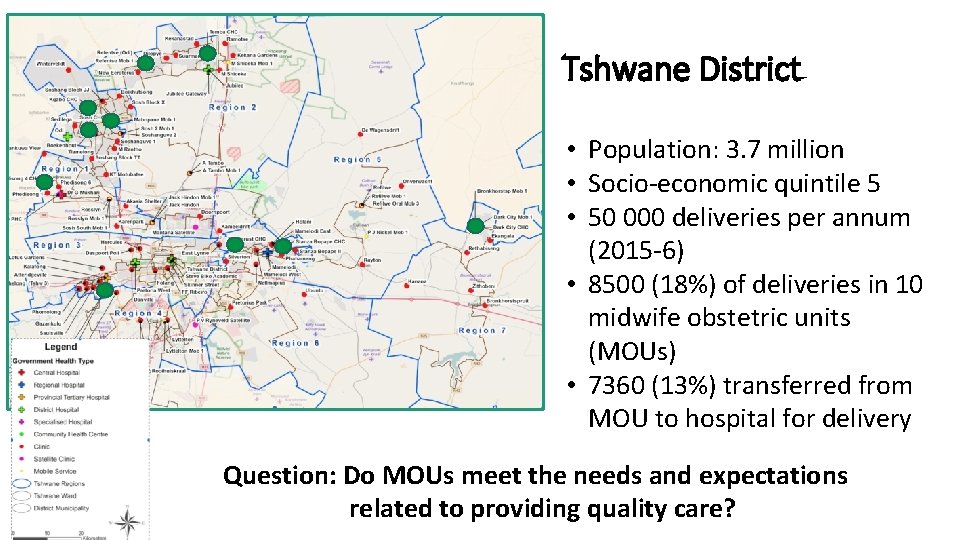
Tshwane District • Population: 3. 7 million • Socio-economic quintile 5 • 50 000 deliveries per annum (2015 -6) • 8500 (18%) of deliveries in 10 midwife obstetric units (MOUs) • 7360 (13%) transferred from MOU to hospital for delivery Question: Do MOUs meet the needs and expectations related to providing quality care?
Study objectives 1. Determine status of respectful birthing care in midwife obstetric units in Tshwane District 2. Design and implement a participatory research intervention in a selected group of MOUs 3. Monitor: process and progress of implementation 4. Evaluate: Outcomes of intervention Impact of intervention
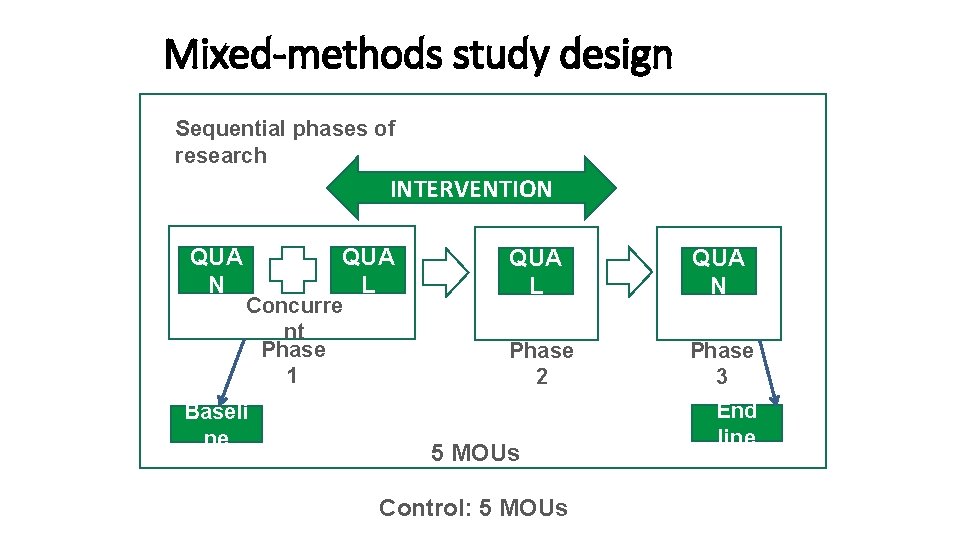
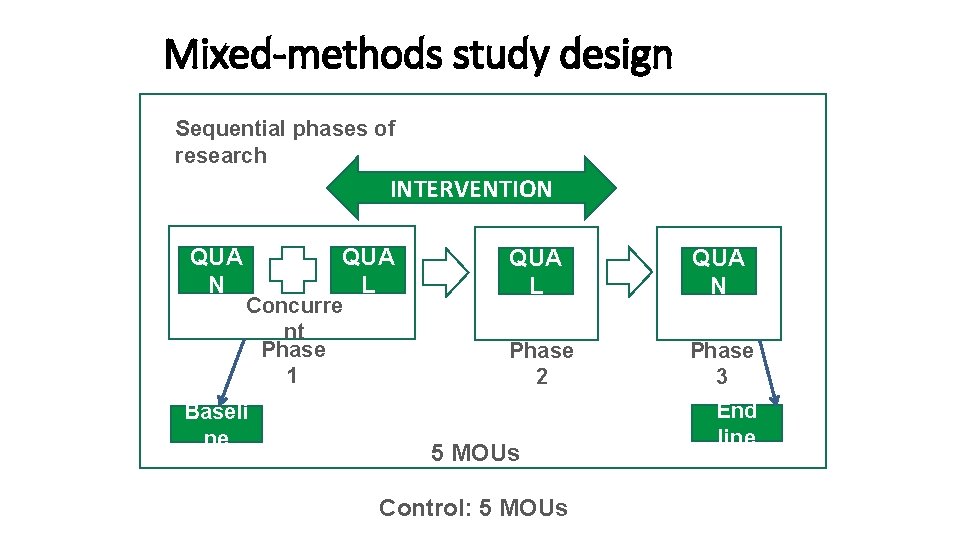
Mixed-methods study design Sequential phases of research INTERVENTION QUA L Concurre nt Phase 1 Baseli ne QUA L QUA N Phase 2 Phase 3 5 MOUs Control: 5 MOUs End line
Phase 1: Baseline assessment
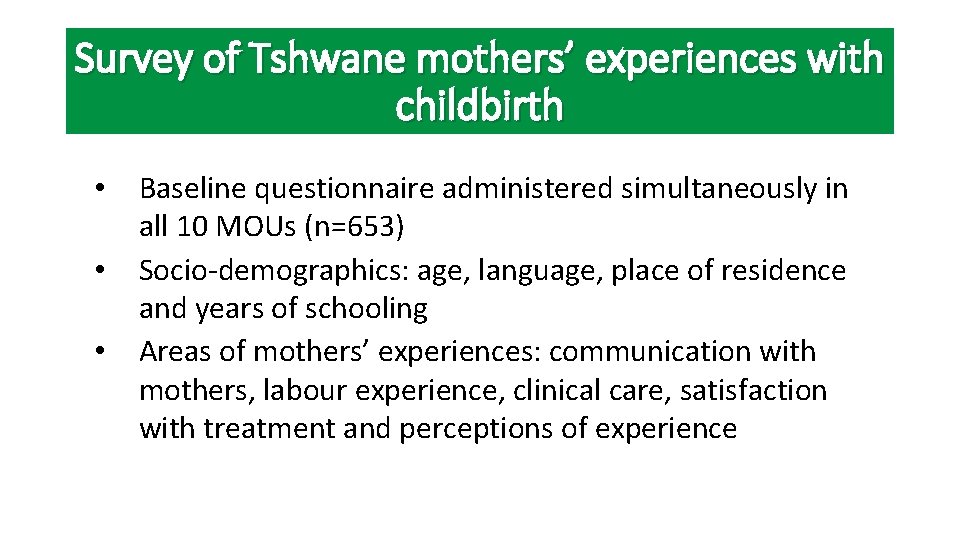
Survey of Tshwane mothers’ experiences with childbirth • • • Baseline questionnaire administered simultaneously in all 10 MOUs (n=653) Socio-demographics: age, language, place of residence and years of schooling Areas of mothers’ experiences: communication with mothers, labour experience, clinical care, satisfaction with treatment and perceptions of experience
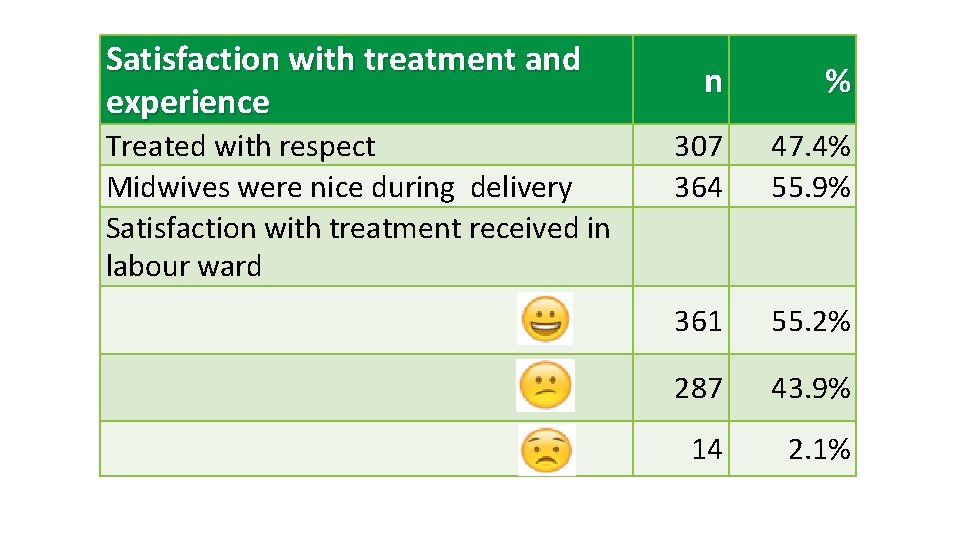
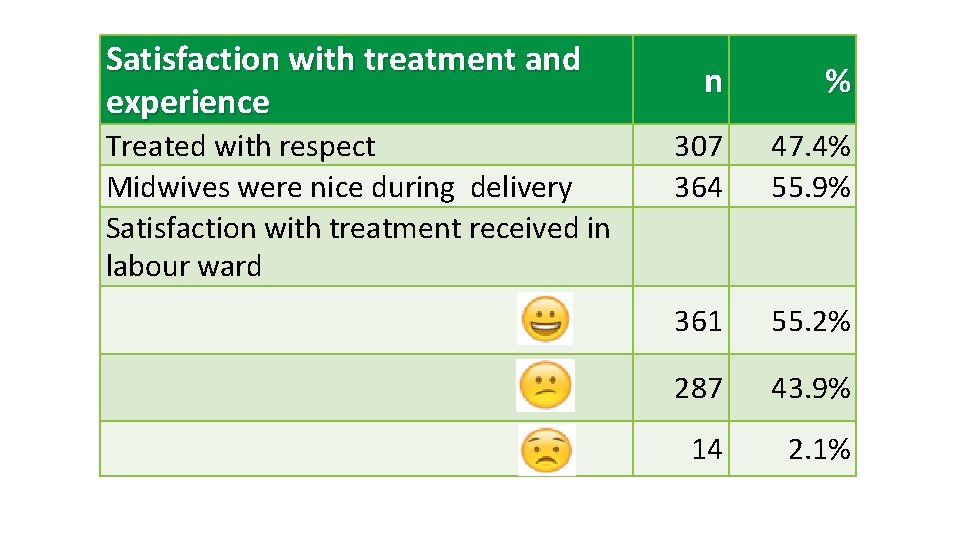
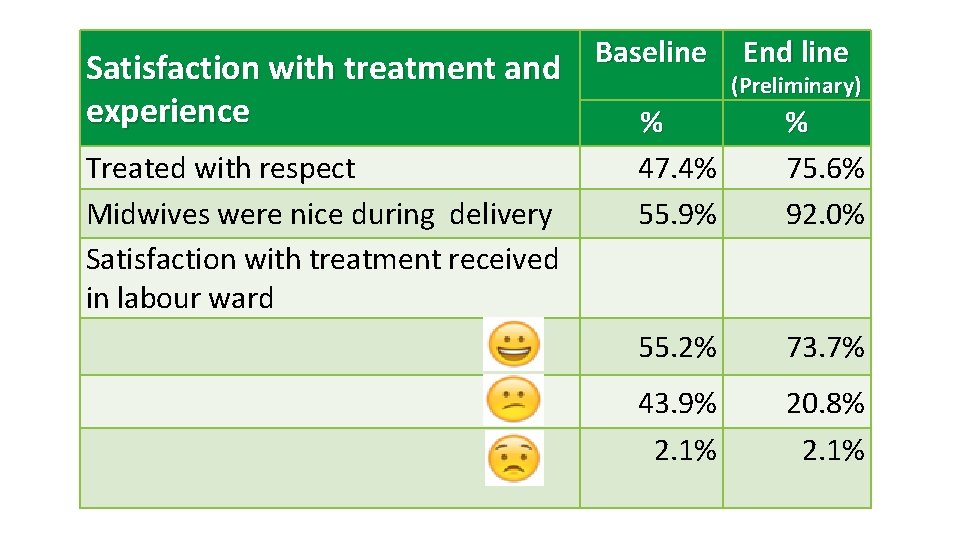
Satisfaction with treatment and experience Treated with respect Midwives were nice during delivery Satisfaction with treatment received in labour ward n % 307 364 47. 4% 55. 9% 361 55. 2% 287 43. 9% 14 2. 1%
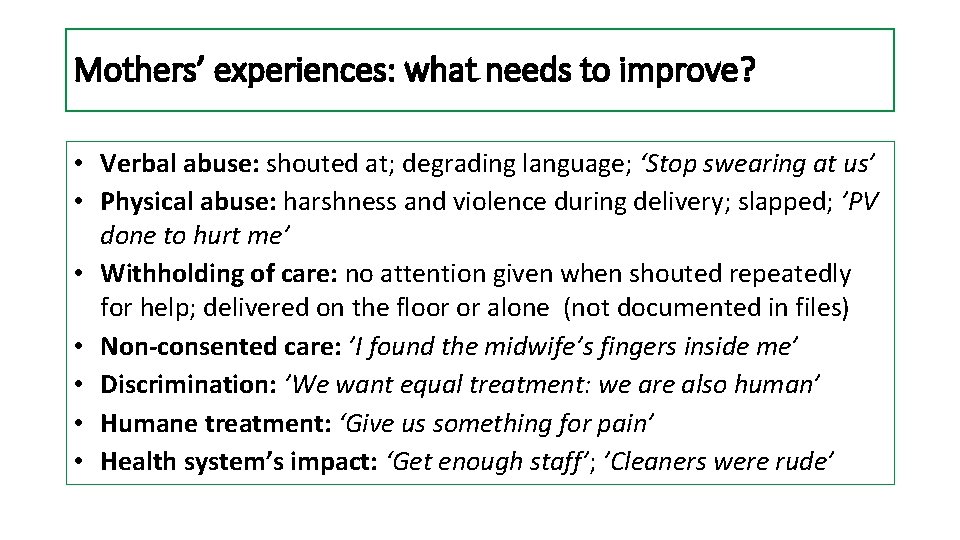
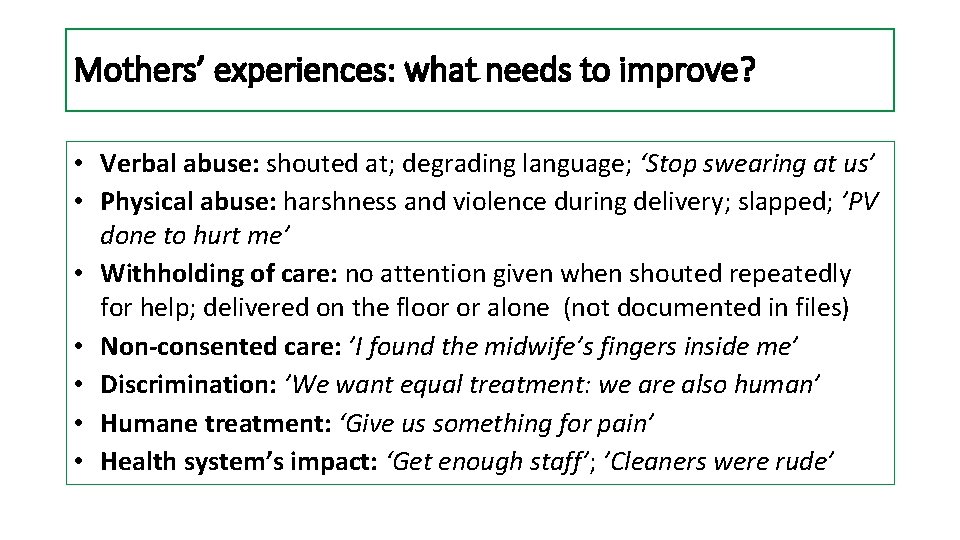
Mothers’ experiences: what needs to improve? • Verbal abuse: shouted at; degrading language; ‘Stop swearing at us’ • Physical abuse: harshness and violence during delivery; slapped; ’PV done to hurt me’ • Withholding of care: no attention given when shouted repeatedly for help; delivered on the floor or alone (not documented in files) • Non-consented care: ’I found the midwife’s fingers inside me’ • Discrimination: ’We want equal treatment: we are also human’ • Humane treatment: ‘Give us something for pain’ • Health system’s impact: ‘Get enough staff’; ’Cleaners were rude’
Conclusion • Midwife obstetric units did not meet the needs and expectations of birthing women • Interventions should address changes in the context of respectful relationships, cognitive care and attention to maternal needs • Respectful care and communication should be linked with midwife competence and quality clinical care
Phase 2: The CLEVER intervention package
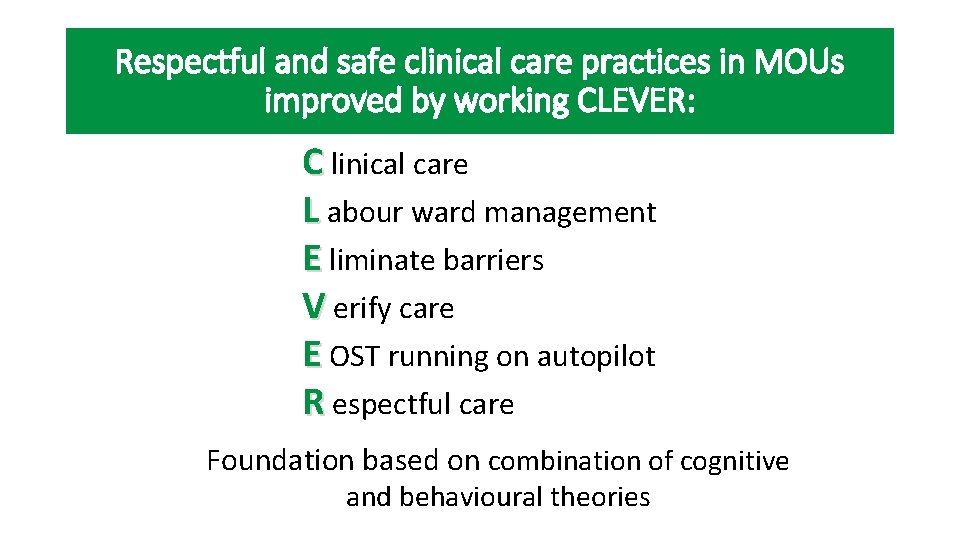
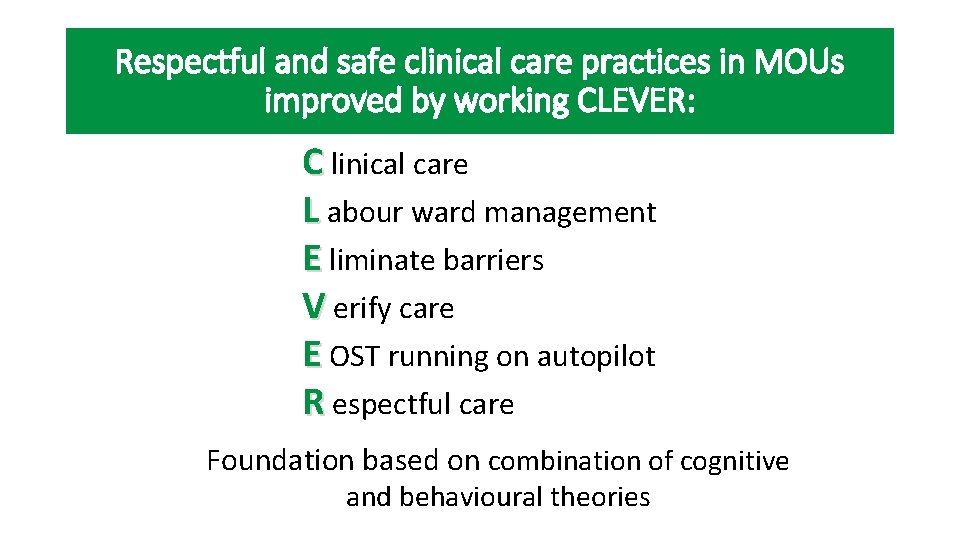
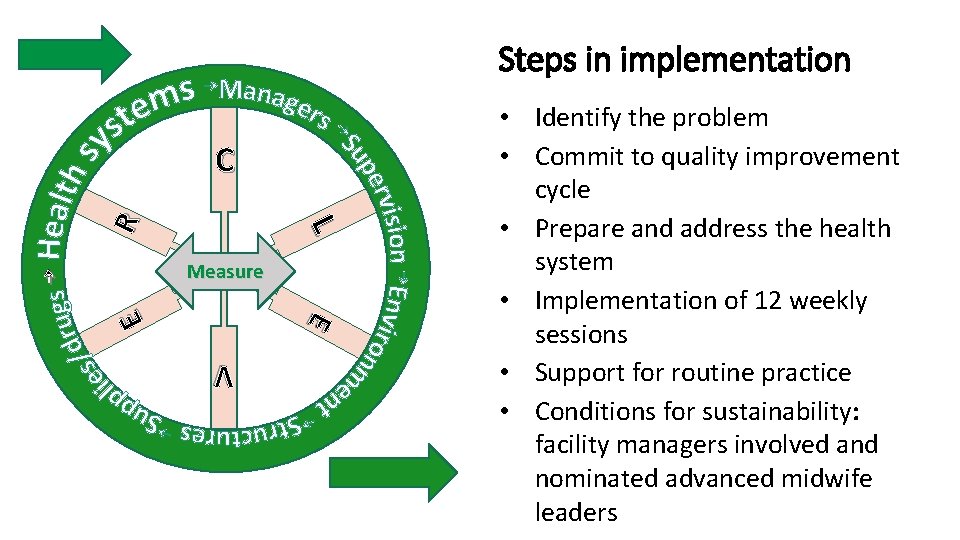
Respectful and safe clinical care practices in MOUs improved by working CLEVER: C linical care L abour ward management E liminate barriers V erify care E OST running on autopilot R espectful care Foundation based on combination of cognitive and behavioural theories
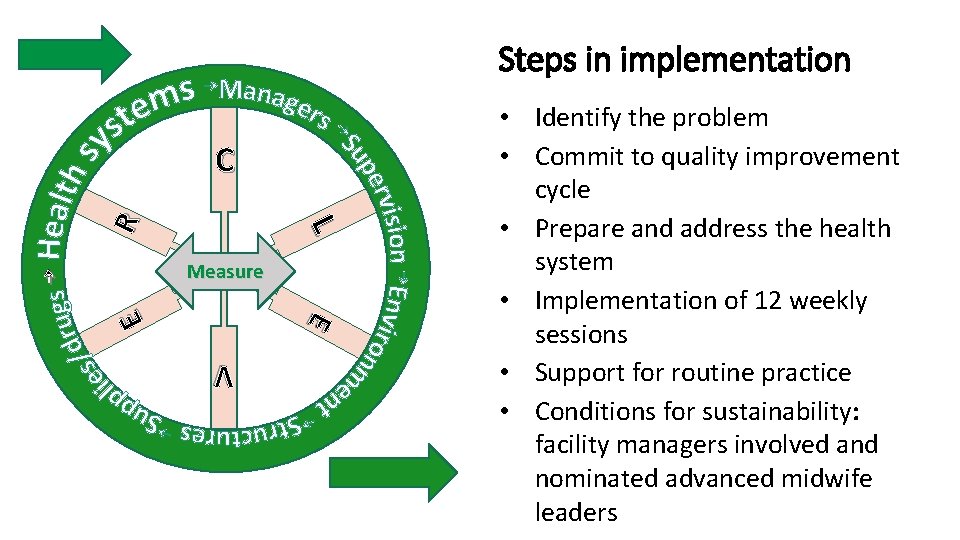
Steps in implementation L R C E E Measure • Identify the problem • Commit to quality improvement cycle • Prepare and address the health system • Implementation of 12 weekly sessions • Support for routine practice • Conditions for sustainability: facility managers involved and nominated advanced midwife leaders V
Clinical care: obstetric admission and triage with urgency • Handover rounds at change of each shift at the mother’s bed to eliminate care delays and blind spots, midwives sign notes • Risk evaluation with management plan, next observation time visibly documented in maternity file (reduce litigation) • Intrapartum monitoring on partogram and continuation of care • Guidelines and flow charts available at triage/admission bed • Discussions with night staff, reviewing cases and debriefing • Team work; support to take over from each other and mandatory support during emergencies
Labour ward management: Resolve withholding of care • Within 5 -10 min of arrival, mother welcomed by name by a midwife stating her own name • Admission/triage bed with equipment and supplies, flow charts • Allocation of cases: advanced midwife according to experience/skill • Working in teams, taking over when needed • Timeous referral of high risk patients to correct level of care • After initial assessment, document time of next observation • Facility manager with team leader doing weekly rounds in unit to support midwife teams, reaching all midwives during handover of shift
Eliminate barriers: meeting basic human needs • Pain management during labour: pethidine and promethazine with signed protocol • Cultural birthing practices allowed – squatting • Birth partners allowed during labour • Food and drinks offered • Comfortable clean environment – linen and savers, maternity pads
Verify care: monitoring, evaluation and feedback • Team leader reviews care and documentation on partograms • Team leaders visible as role models with emphatic care (don’t allow poor care practices and rude communication) • Measure care by key indicators and tools • Follow mothers’ complaints and experiences during birth • Constant feedback to teams and facility manager on birthing mothers’ needs and expectations • Balance actions with “what would the professional midwife do? ”
Emergency obstetric simulation training (EOST): creating autopilot care in units Reaching all shifts in delivery units • Eliminate thinking during emergencies: ensure that skill is so well ingrained that midwives can deliver breech, shoulder dystocia and handle PPH, eclampsia, sepsis and cord prolapse without stress • Use different teaching methods: simulated training, videos and discussions with flow charts • EOST needs to reach all the teams of midwives in the unit (night and the rotational weekend shifts)
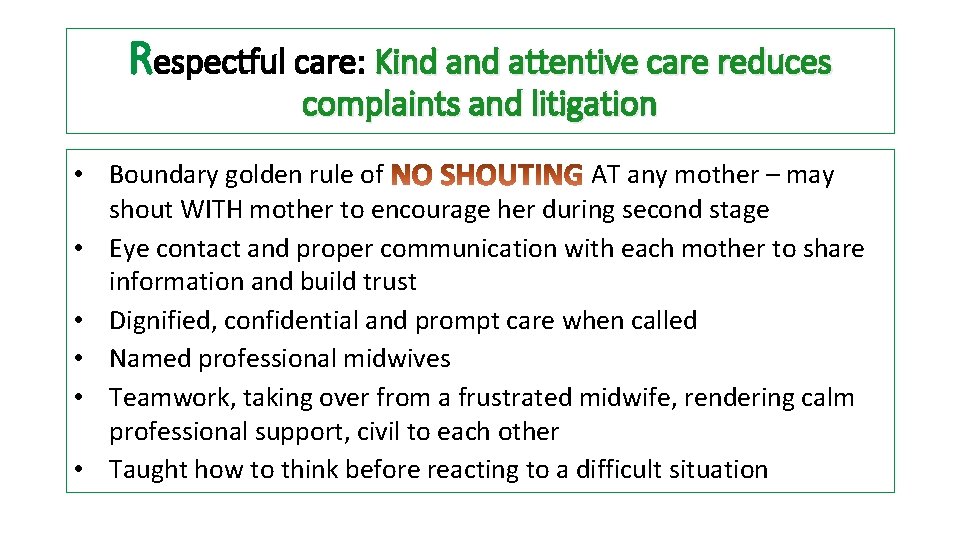
Respectful care: Kind attentive care reduces complaints and litigation • Boundary golden rule of AT any mother – may shout WITH mother to encourage her during second stage • Eye contact and proper communication with each mother to share information and build trust • Dignified, confidential and prompt care when called • Named professional midwives • Teamwork, taking over from a frustrated midwife, rendering calm professional support, civil to each other • Taught how to think before reacting to a difficult situation
Phase 3: End line assessment of working CLEVER
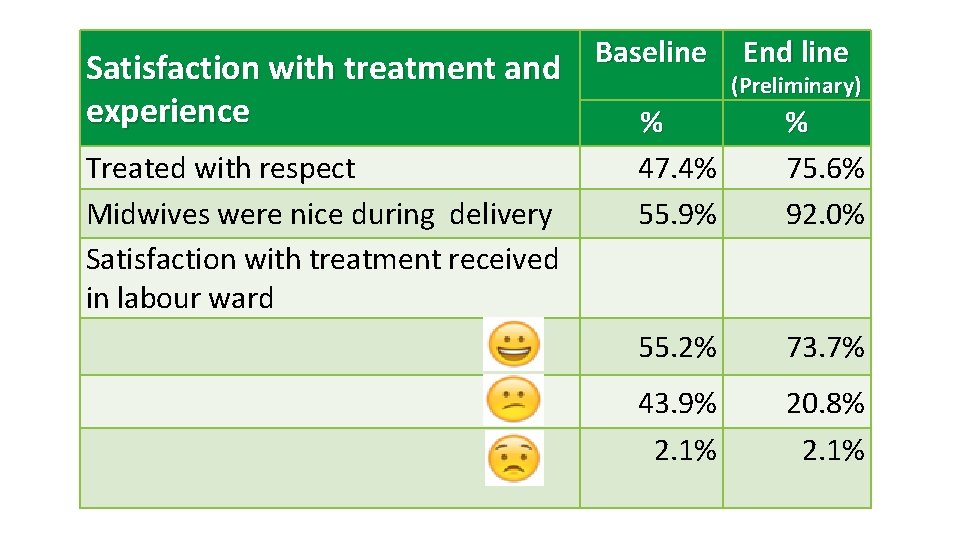
Satisfaction with treatment and experience Treated with respect Midwives were nice during delivery Satisfaction with treatment received in labour ward Baseline End line (Preliminary) % 47. 4% 55. 9% % 75. 6% 92. 0% 55. 2% 73. 7% 43. 9% 2. 1% 20. 8% 2. 1%
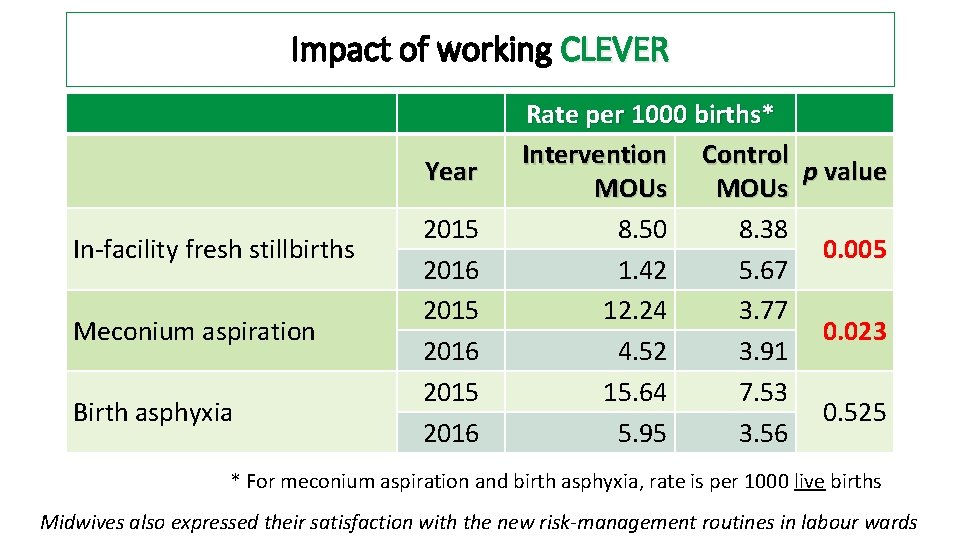
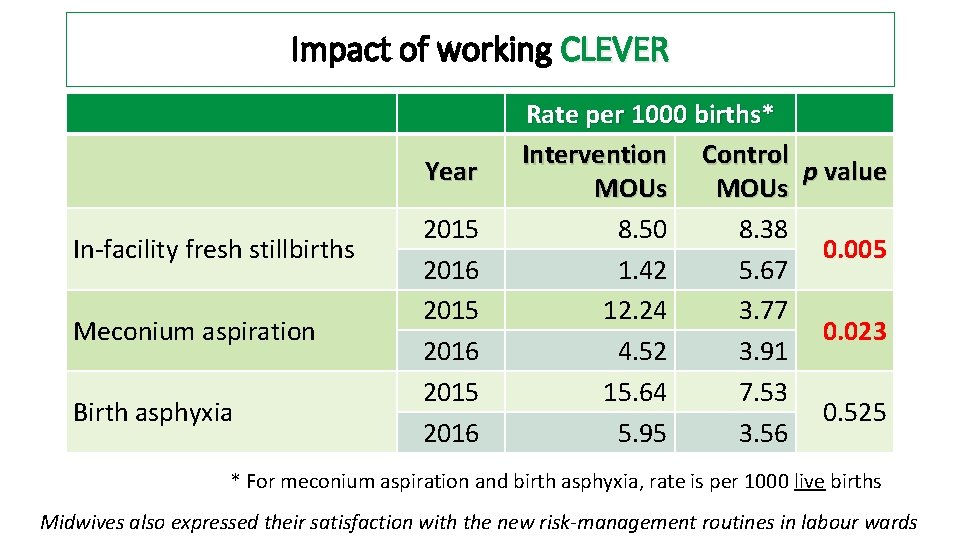
Impact of working CLEVER Year In-facility fresh stillbirths Meconium aspiration Birth asphyxia 2015 2016 Rate per 1000 births* Intervention Control p value MOUs 8. 50 8. 38 0. 005 1. 42 5. 67 12. 24 3. 77 0. 023 4. 52 3. 91 15. 64 7. 53 0. 525 5. 95 3. 56 * For meconium aspiration and birth asphyxia, rate is per 1000 live births Midwives also expressed their satisfaction with the new risk-management routines in labour wards
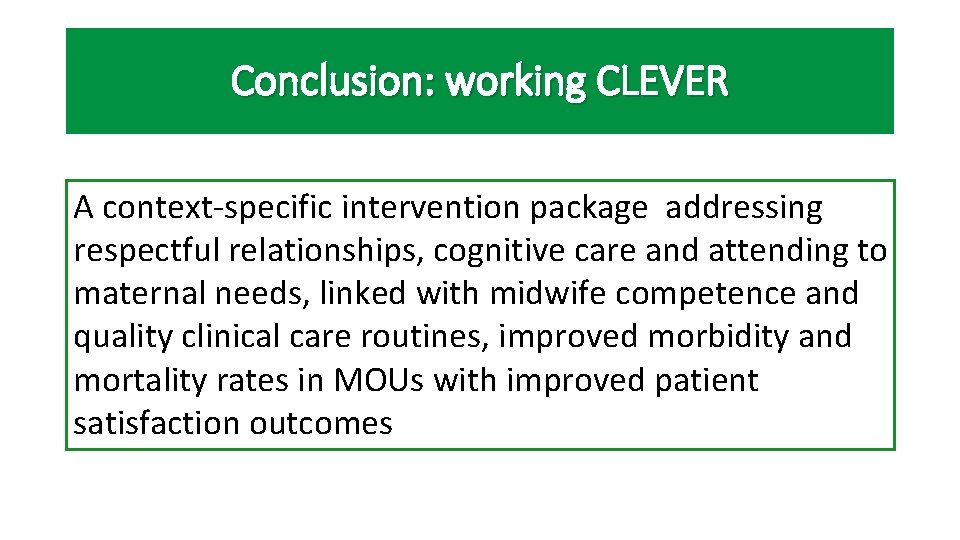
Conclusion: working CLEVER A context-specific intervention package addressing respectful relationships, cognitive care and attending to maternal needs, linked with midwife competence and quality clinical care routines, improved morbidity and mortality rates in MOUs with improved patient satisfaction outcomes
 Ekurhuleni district of education
Ekurhuleni district of education Providing improper or unprofessional treatment or care
Providing improper or unprofessional treatment or care Providing improper or unprofessional treatment or care
Providing improper or unprofessional treatment or care Future nurse programme
Future nurse programme Carla morrow midwife
Carla morrow midwife Dallas midwife associates
Dallas midwife associates Ready respectful safe assembly
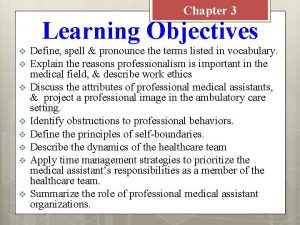
Ready respectful safe assembly Obstructions to professionalism
Obstructions to professionalism Stories of respect
Stories of respect Building respectful families
Building respectful families Dirty jobs dairy cow midwife worksheet
Dirty jobs dairy cow midwife worksheet Cindy morrow midwife
Cindy morrow midwife Respectful
Respectful Respectful samoan greeting
Respectful samoan greeting Vcaa respectful relationships
Vcaa respectful relationships Prefixes kelimeler
Prefixes kelimeler New york certified midwife
New york certified midwife Compassionate respectful and caring
Compassionate respectful and caring Respectful learning environment
Respectful learning environment Kepanjangan sst
Kepanjangan sst Bestwood and sherwood midwifery
Bestwood and sherwood midwifery Considerate prefix
Considerate prefix Respectful communication quotes
Respectful communication quotes