Principles of surgical sterilisation and disinfection Dr Ali
- Slides: 15
Principles of surgical sterilisation and disinfection Dr. Ali Jaffer Upper GI surgeon
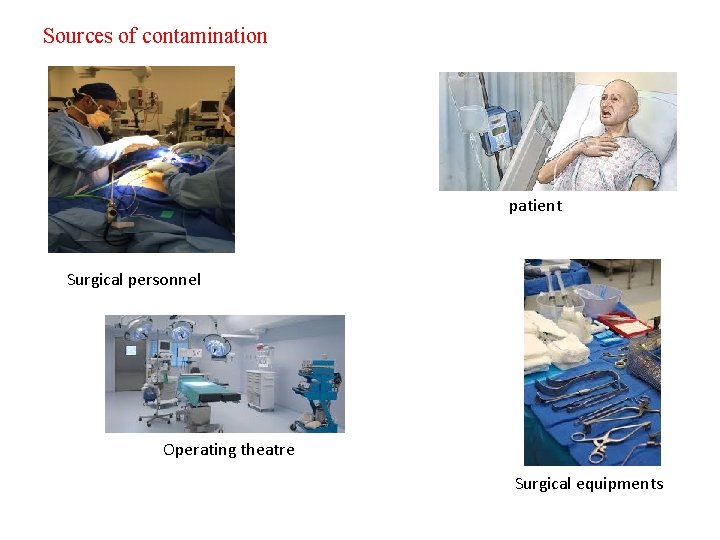
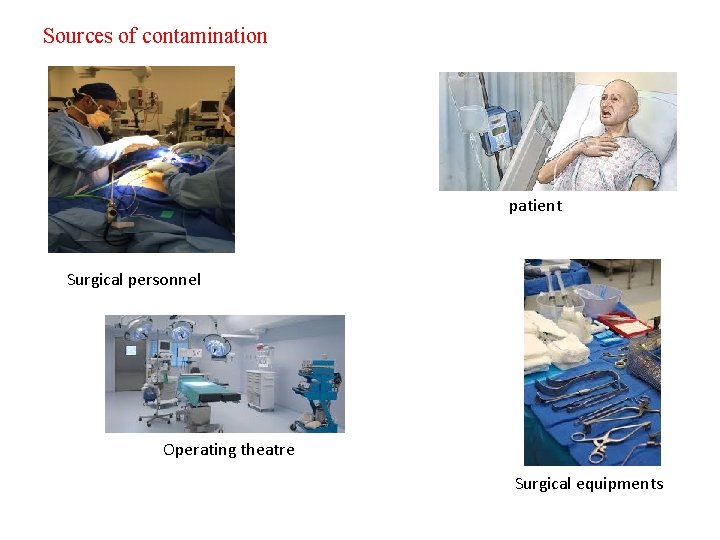
Sources of contamination patient Surgical personnel Operating theatre Surgical equipments
Definition of Terms Sterilization describes a process that destroys or eliminates all forms of microbial life and is carried out in health-care facilities by physical or chemical methods. Disinfection describes a process that eliminates many or all pathogenic microorganisms, except bacterial spores. Cleaning is the removal of visible soil (e. g. , organic and inorganic material) from objects and surfaces and normally is accomplished manually or mechanically using water with detergents or enzymatic products. Thorough cleaning is essential before high-level disinfection and sterilization because inorganic and organic materials that remain on the surfaces of instruments interfere with the effectiveness of these processes. Critical items confer a high risk for infection if they are contaminated with any microorganism. This category includes surgical instruments, cardiac and urinary catheters, implants, and ultrasound probes used in sterile body cavities. Semicritical items contact mucous membranes or nonintact skin. Ex respiratory therapy and anesthesia equipment, some endoscopes and others. These medical devices should be free from all microorganisms; however, small numbers of bacterial spores are permissible. Noncritical items are those that come in contact with intact skin but not mucous membranes. Examples of noncritical patient-care items are bedpans, blood pressure cuffs, crutches and computers.
Factors Affecting the Efficacy of Disinfection and Sterilization Number and Location of Microorganisms The larger the number of microbes, the more time a germicide needs to destroy all of them. Medical instruments with multiple pieces must be disassembled and equipment such as endoscopes that have crevices, joints, and channels are more difficult to disinfect than are flatsurface equipment because penetration of the disinfectant of all parts of the equipment is more difficult. Innate Resistance of Microorganisms For example, spores are resistant to disinfectants because the spore coat and cortex act as a barrier. Concentration and Potency of Disinfectants Several physical and chemical factors also influence disinfectant procedures: temperature, p. H, relative humidity, and water hardness. For example, the activity of most disinfectants increases as the temperature increases, but some exceptions exist. Furthermore, too great an increase in temperature causes the disinfectant to degrade and weakens its germicidal activity and thus might produce a potential health hazard. An increase in p. H improves the antimicrobial activity of some disinfectants (e. g. , glutaraldehyde, quaternary ammonium compounds) but decreases the antimicrobial activity of others (e. g. , phenols, hypochlorites, and iodine). Relative humidity is the single most important factor influencing the activity of gaseous disinfectants/sterilants, such as ETO, chlorine dioxide, and formaldehyde.
Factors Affecting the Efficacy of Disinfection and Sterilization Organic and Inorganic Matter Organic matter in the form of serum, blood, pus, or fecal or lubricant material can interfere with the antimicrobial activity of disinfectants. Most commonly, interference occurs by a chemical reaction between the germicide and the organic matter resulting in a complex that is less germicidal or nongermicidal, leaving less of the active germicide available for attacking microorganisms. Chlorine and iodine disinfectants, in particular, are prone to such interaction Duration of Exposure
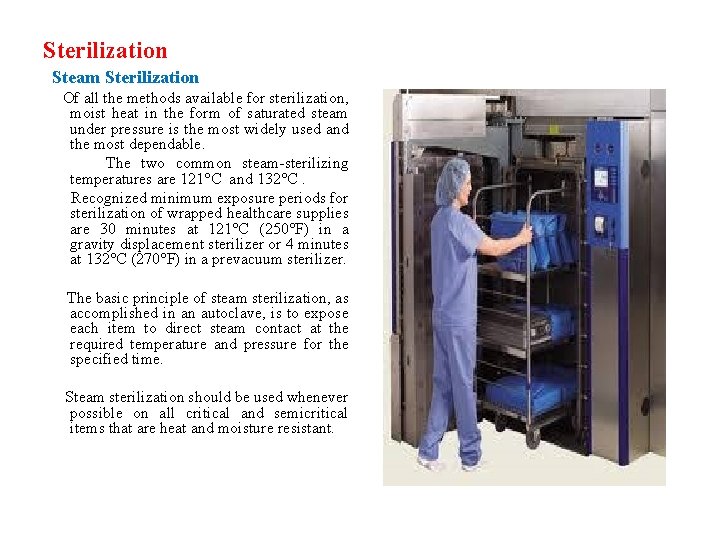
Sterilization Steam Sterilization Of all the methods available for sterilization, moist heat in the form of saturated steam under pressure is the most widely used and the most dependable. The two common steam-sterilizing temperatures are 121°C and 132°C. Recognized minimum exposure periods for sterilization of wrapped healthcare supplies are 30 minutes at 121°C (250°F) in a gravity displacement sterilizer or 4 minutes at 132°C (270°F) in a prevacuum sterilizer. The basic principle of steam sterilization, as accomplished in an autoclave, is to expose each item to direct steam contact at the required temperature and pressure for the specified time. Steam sterilization should be used whenever possible on all critical and semicritical items that are heat and moisture resistant.
Flash Sterilization It is a modification of conventional steam sterilization in which the flashed item is placed in an open tray or is placed in a specially designed, covered, rigid container to allow for rapid penetration of steam. Adverse events have been associated with flash sterilization. Less effective in comparison with steam sterilisation. It may cause clinical burns so it is need to develop policies and educate staff to prevent the use of instruments hot enough to cause such injuries.
Ethylene Oxide "Gas" Sterilization ETO is used in healthcare facilities to sterilize critical items (and sometimes semicritical items) that are moisture or heat sensitive and cannot be sterilized by steam sterilization. Ionizing Radiation. Sterilization by ionizing radiation, primarily by cobalt 60 gamma rays or electron accelerators, is a low-temperature sterilization method that has been used for a number of medical products (e. g. , tissue for transplantation, pharmaceuticals, medical devices). Dry-Heat Sterilizers. This method should be used only for materials that might be damaged by moist heat or that are impenetrable to moist heat (e. g. , powders, petroleum products, sharp instruments).
Disinfection • Chlorhexidine gluconate has a residual effect and is effective for more than 4 hours. It has potent antiseptic activity against Grampositive and Gram-negative organisms and some viruses but only moderate activity against the tubercle bacillus. • Iodine (povidone-iodine) has some residual effects but these are not sustained for more than 4 hours. “Free” iodine (I 2) contributes to the bactericidal activity of iodophors and dilutions of iodophors demonstrate more rapid bactericidal action than does a full-strength povidoneiodine solution. It is highly bactericidal, fungicidal and viricidal. There is some activity against bacterial spores and good activity against the tubercle bacillus. The iodine agents penetrate cell walls to produce anti-microbial effects. They may be irritating to the skin or cause allergic reactions. • The alcohols are highly effective, rapidly acting anti-microbial agents with broad-spectrum activity. They are effective in destroying Gram-positive and Gram-negative bacteria, fungi, viruses and tubercle bacilli, but are not sporicidal. Alcohol is an inexpensive anti-microbial agent and one of the most widely used skin antiseptics, especially preceding subcutaneous and intramuscular injections and venepunctures; a 10 -s drying after application enhances its effectiveness.
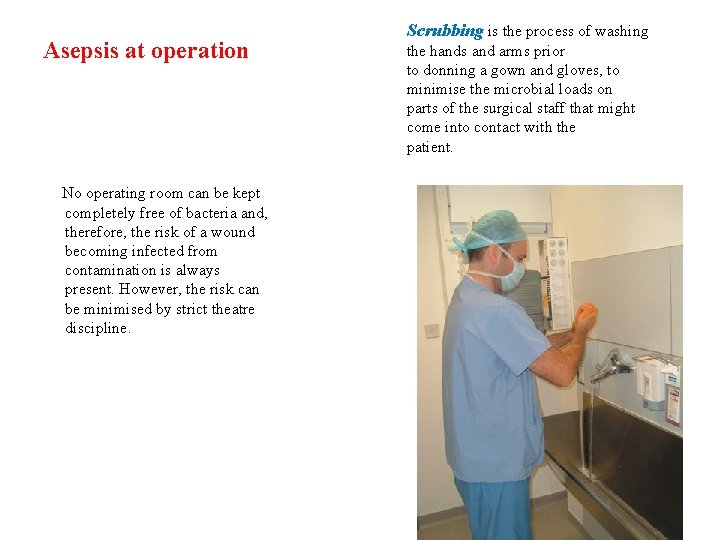
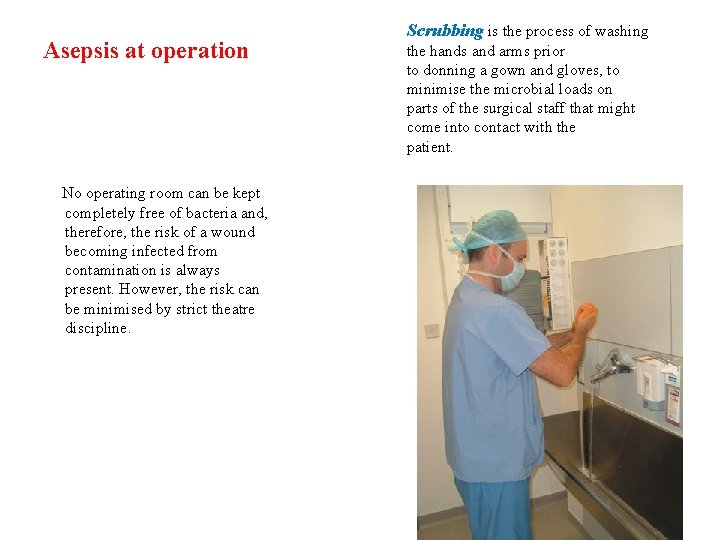
Asepsis at operation No operating room can be kept completely free of bacteria and, therefore, the risk of a wound becoming infected from contamination is always present. However, the risk can be minimised by strict theatre discipline. Scrubbing is the process of washing the hands and arms prior to donning a gown and gloves, to minimise the microbial loads on parts of the surgical staff that might come into contact with the patient.
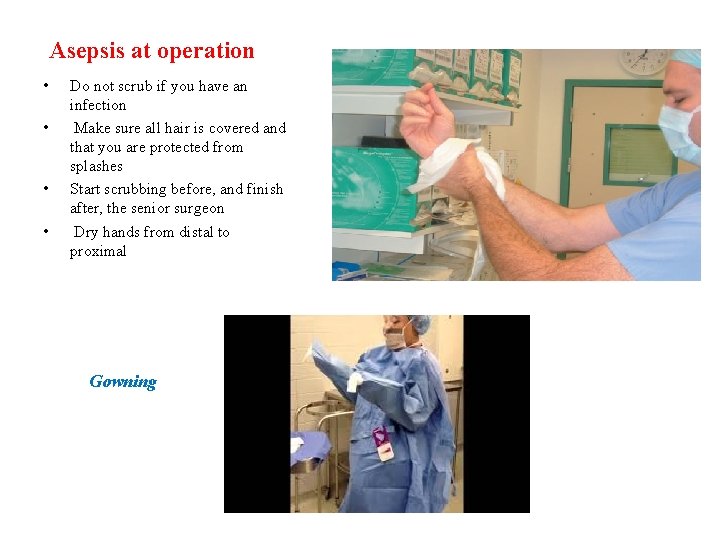
Asepsis at operation • • Do not scrub if you have an infection Make sure all hair is covered and that you are protected from splashes Start scrubbing before, and finish after, the senior surgeon Dry hands from distal to proximal Gowning
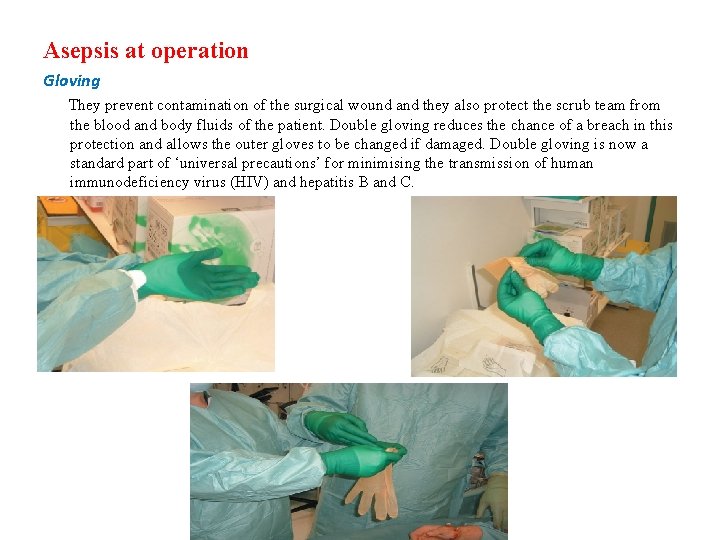
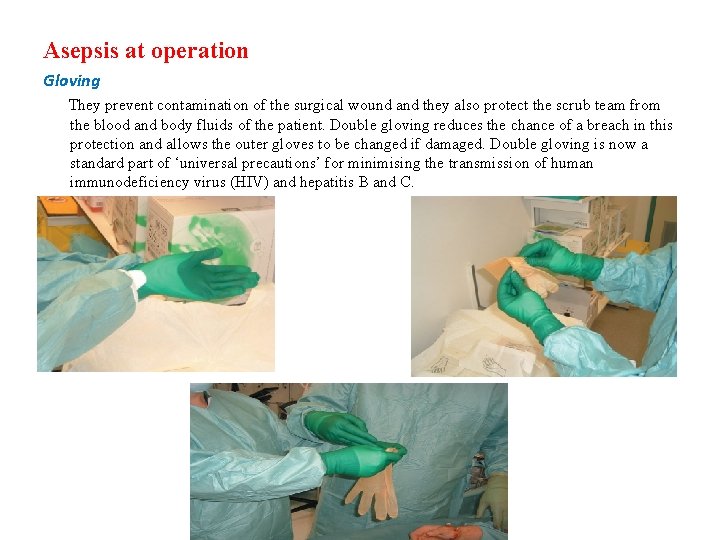
Asepsis at operation Gloving They prevent contamination of the surgical wound and they also protect the scrub team from the blood and body fluids of the patient. Double gloving reduces the chance of a breach in this protection and allows the outer gloves to be changed if damaged. Double gloving is now a standard part of ‘universal precautions’ for minimising the transmission of human immunodeficiency virus (HIV) and hepatitis B and C.
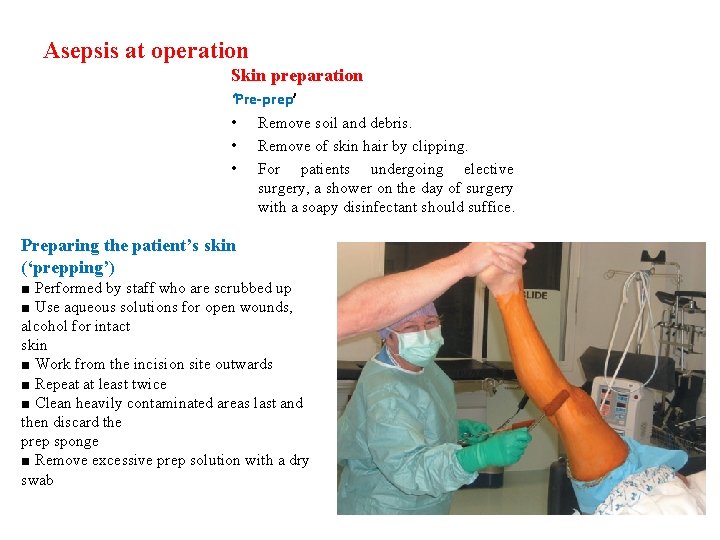
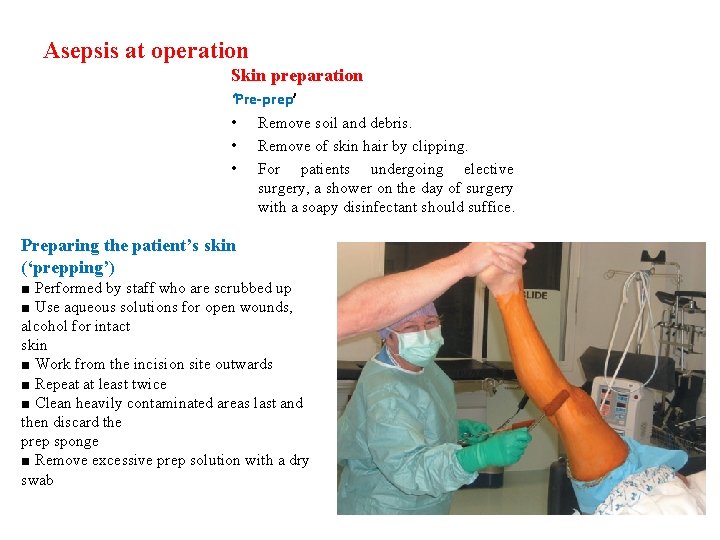
Asepsis at operation Skin preparation ‘Pre-prep’ • Remove soil and debris. • Remove of skin hair by clipping. • For patients undergoing elective surgery, a shower on the day of surgery with a soapy disinfectant should suffice. Preparing the patient’s skin (‘prepping’) ■ Performed by staff who are scrubbed up ■ Use aqueous solutions for open wounds, alcohol for intact skin ■ Work from the incision site outwards ■ Repeat at least twice ■ Clean heavily contaminated areas last and then discard the prep sponge ■ Remove excessive prep solution with a dry swab
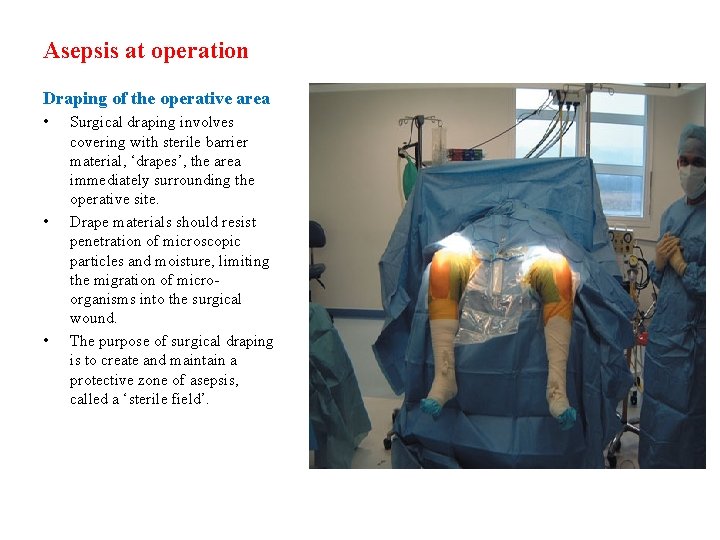
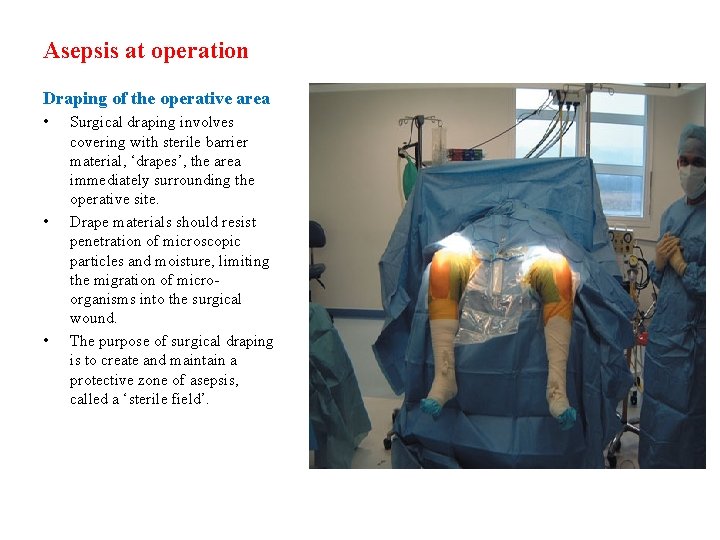
Asepsis at operation Draping of the operative area • • • Surgical draping involves covering with sterile barrier material, ‘drapes’, the area immediately surrounding the operative site. Drape materials should resist penetration of microscopic particles and moisture, limiting the migration of microorganisms into the surgical wound. The purpose of surgical draping is to create and maintain a protective zone of asepsis, called a ‘sterile field’.
Good Luck
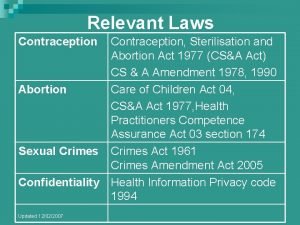
 Contraception sterilisation and abortion act 1977
Contraception sterilisation and abortion act 1977 Validierung rdg zahnarztpraxis
Validierung rdg zahnarztpraxis Circuit du linge definition
Circuit du linge definition Double emballage stérilisation
Double emballage stérilisation Pliage enveloppe stérilisation
Pliage enveloppe stérilisation Central lean
Central lean Pliage pasteur stérilisation
Pliage pasteur stérilisation Browne sterilisation indicators
Browne sterilisation indicators Sekretmetoden
Sekretmetoden Stérilisation chaleur humide
Stérilisation chaleur humide Low level disinfectant
Low level disinfectant Sterilization and disinfection
Sterilization and disinfection Sterilization and disinfection
Sterilization and disinfection Sterilization and disinfection
Sterilization and disinfection Sterilization and disinfection
Sterilization and disinfection Nurses responsibility in sterilization
Nurses responsibility in sterilization