Preventing Falls Interventions in Geriatric Psychiatry Patients an
- Slides: 13
Preventing Falls – Interventions in Geriatric Psychiatry Patients an Overview of Current Literature Samantha Beckwith BSN, RN, PMH-BC October 23, 2020
Background • Estimated fall rates in acute care hospitals range from 1. 3 to 8. 9 per 1000 patient days (Greely et al. , 2020) • Fall rates on geriatric psychiatry units have been reported to be as high as 13. 66 per 1000 patient days (Struble Fitzsimmons et al. , 2019) • Falls are the leading cause of injury related deaths among people aged 65 years and older (Quigly et al. , 2014) • Serious fall related injuries result in increased length of stay, loss of function, loss of life, and financial burden (Khurshid & Lantz, 2016) • Odds of fall related injury among patients with cognitive disorders such as Alzheimer's disease and other dementias were found to be at least 3 times greater than those among the general elderly population (Quigley et al. , 2014) • As the mobility of geriatric psychiatry patients deteriorates, so does their ability to recognize, judge, and avoid hazards (Neyens et al. , 2009) 2
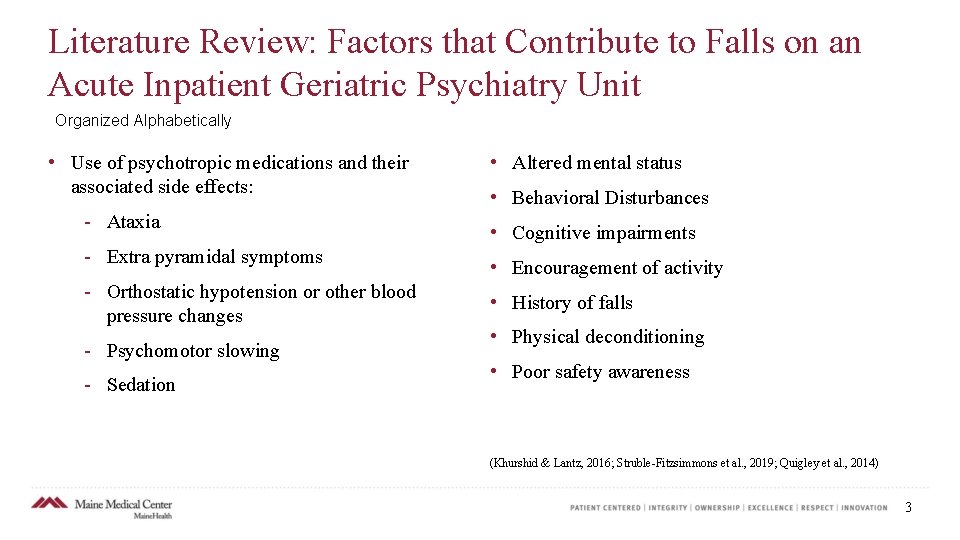
Literature Review: Factors that Contribute to Falls on an Acute Inpatient Geriatric Psychiatry Unit Organized Alphabetically • Use of psychotropic medications and their associated side effects: Ataxia Extra pyramidal symptoms Orthostatic hypotension or other blood pressure changes Psychomotor slowing Sedation • Altered mental status • Behavioral Disturbances • Cognitive impairments • Encouragement of activity • History of falls • Physical deconditioning • Poor safety awareness (Khurshid & Lantz, 2016; Struble Fitzsimmons et al. , 2019; Quigley et al. , 2014) 3
Context – P 6 • The Inpatient Psychiatry unit at Maine Medical Center (P 6) is a 21 bed unit specializing in geriatric and medical psychiatry • The majority of patients have a primary diagnosis of Dementia with Behavioral Disturbance • The unit features 12 double occupancy rooms and one single occupancy room, as well as a large activity room • Patients participate in a therapeutic milieu in which they are encouraged to interact with other patients in common areas and ambulate around the unit • Average number of patients: 19. 6 (FY 2020) • Average length of stay: 27. 2 days (FY 2020) • Targeted nurse to patient ratio: 1: 5. 3 (0700 2300), 1: 8 (2300 0700) 4
Context – How Does P 6 Mitigate Falls Currently • On admission to P 6 each patient receives a comprehensive interdisciplinary fall risk assessment including Fall Injury Risk Level per the New York Presbyterian Fall/Injury Risk Assessment Tool by nursing (this is also completed once a shift and following a fall), a rating on the Bedside Mobility Assessment Tool (BMAT) by nursing, and a score/fall risk level via the Get Up and Go Fall Risk Assessment by OT. • Each patient’s fall risk level is discussed each morning in our interdisciplinary treatment team meeting • Based on nursing assessments, nurses deploy fall risk interventions based on the MMC Policy “Fall Risk Identification and Management” • Yellow Shirt Program: If a patient is found to be a Very High Fall Risk based on the interdisciplinary fall risk assessment they are placed in a yellow shirt or Johnny Provides visual cue to all members of the treatment team that the patient should not be ambulating alone 5
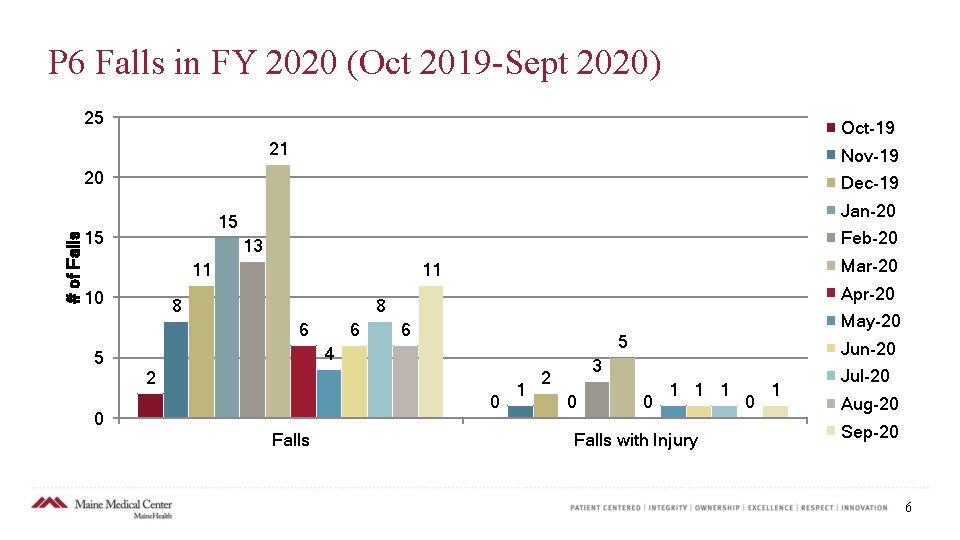
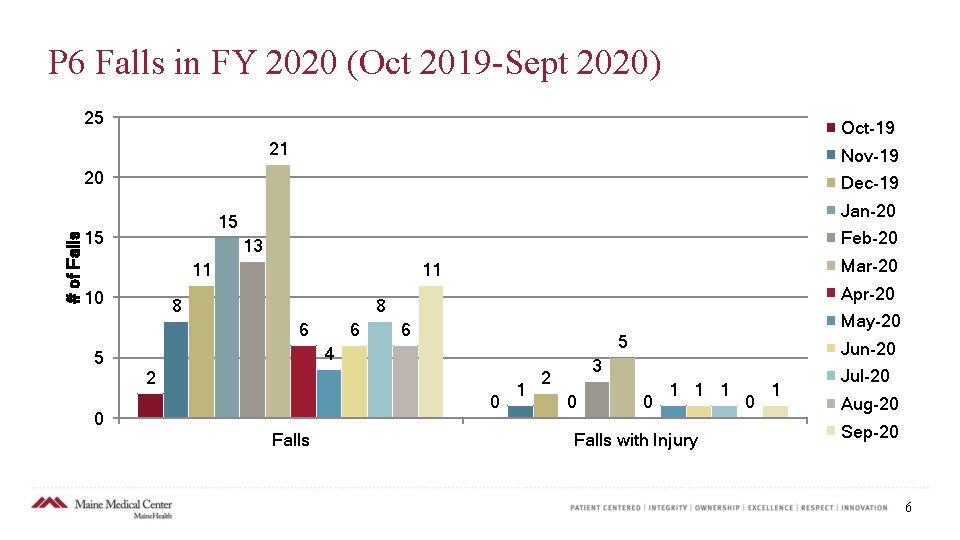
P 6 Falls in FY 2020 (Oct 2019 Sept 2020) 25 Oct-19 21 Nov-19 # of Falls 20 Dec-19 Jan-20 15 15 Feb-20 13 11 10 8 Apr-20 8 6 5 Mar-20 11 6 May-20 6 5 4 2 0 0 Falls 1 Jun-20 3 2 0 0 1 1 1 Falls with Injury 0 1 Jul-20 Aug-20 Sep-20 6
Purpose • The purpose of this project was to search and review the current literature for interventions to prevent falls in geriatric psychiatry patients. PICOT: In geriatric psychiatry patients, are there specific fall interventions that decrease fall rates that P 6 is not currently utilizing? 7
Design/Methods • Databases Used: CINAHL, Pub. Med • MMC Librarians also completed search and provided articles • Key Words Used: Falls, Geriatric, Psychiatry, Psychiatric, Geripsych, Fall Interventions • Articles Found: 15 • Articles Used: 9 8
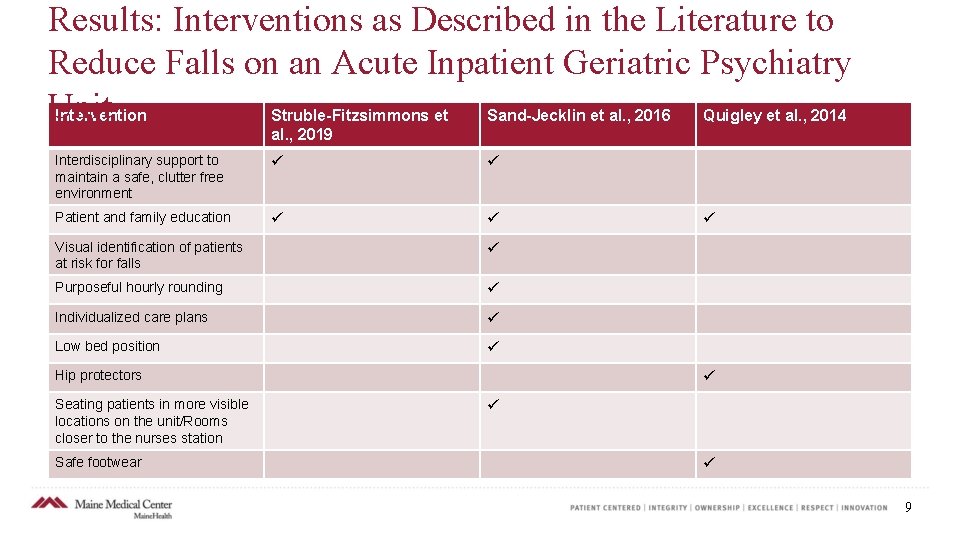
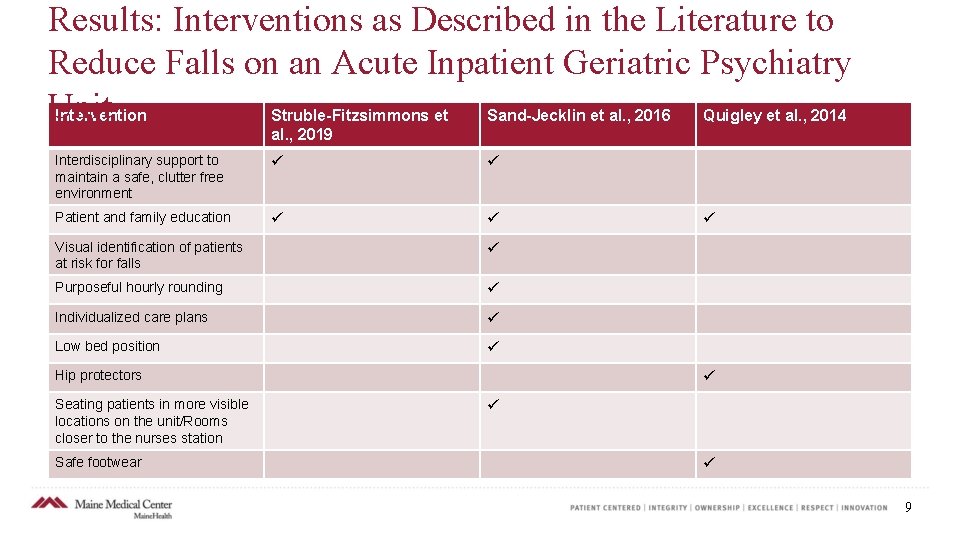
Results: Interventions as Described in the Literature to Reduce Falls on an Acute Inpatient Geriatric Psychiatry Unit Intervention Struble-Fitzsimmons et Sand-Jecklin et al. , 2016 Quigley et al. , 2014 al. , 2019 Interdisciplinary support to maintain a safe, clutter free environment Patient and family education Visual identification of patients at risk for falls Purposeful hourly rounding Individualized care plans Low bed position Hip protectors Seating patients in more visible locations on the unit/Rooms closer to the nurses station Safe footwear 9
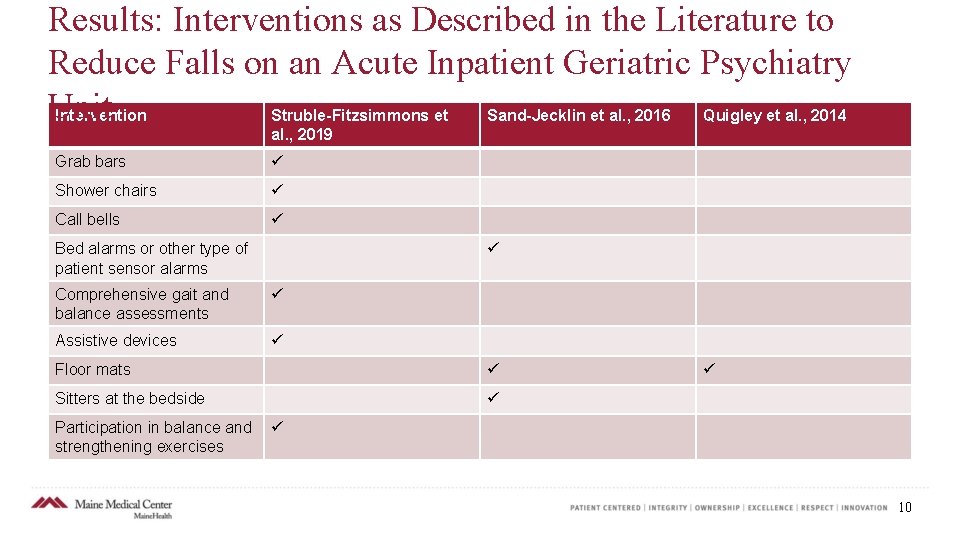
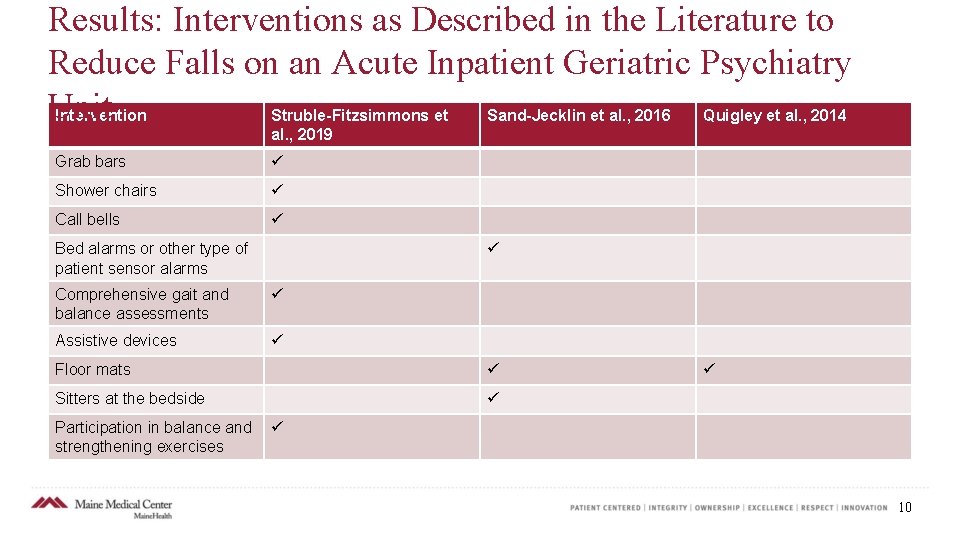
Results: Interventions as Described in the Literature to Reduce Falls on an Acute Inpatient Geriatric Psychiatry Unit Intervention Struble-Fitzsimmons et Sand-Jecklin et al. , 2016 Quigley et al. , 2014 al. , 2019 Grab bars Shower chairs Call bells Bed alarms or other type of patient sensor alarms Comprehensive gait and balance assessments Assistive devices Floor mats Sitters at the bedside Participation in balance and strengthening exercises 10
Results – Interventions on P 6 • Of the 18 interventions supported by the literature, P 6 is utilizing 16 of the supported interventions. • The two interventions not currently utilized on P 6 are: Hip Protectors Floor Mats 11
References Blair E, & Gruman C. (2005). Falls in an inpatient geriatric psychiatric population. Journal of the American Psychiatric Nurses Association, 11(6), 351– 354. Greeley, A. M. , Tanner, E. P. , Mak, S. , Begashaw, M. M. , Miake Lye, I. M. , & Shekelle, P. G. (2020). Sitters as a Patient Safety Strategy to Reduce Hospital Falls: A Systematic Review. Annals of Internal Medicine, 172(5), 317– 324. https: //doi org. mainehealth. idm. oclc. org/10. 7326/M 19 2628 Khurshid, T. , & Lantz, M. S. (2016). Poster Number: EI 24 Falls and Inpatient Geriatric Psychiatry: A Simple Solution to a Chronic and Difficult Problem. American Journal of Geriatric Psychiatry, 24(3), S 90–S 91. https: //doi org. mainehealth. idm. oclc. org/10. 1016/j. jagp. 2016. 01. 089 Neyens, J. C. L. , Dijcks, B. P. J. , Twisk, J. , Schols, J. M. G. A. , van Haastregt, J. C. M. , van den Heuvel, W. J. A. , & de Witte, L. P. (2009). A multifactorial intervention for the prevention of falls in psychogeriatric nursing home patients, a randomised controlled trial (RCT). Age and Ageing, 38(2), 194– 199. https: //doi org. mainehealth. idm. oclc. org/10. 1093/ageing/afn 297 Quigley, P. A. , Barnett, S. D. , Bulat, T. , & Friedman, Y. (2014). Reducing falls and fall related injuries in mental health: a 1 year multihospital falls collaborative. Journal of Nursing Care Quality, 29(1), 51– 59. https: //doi org. mainehealth. idm. oclc. org/10. 1097/01. NCQ. 0000437033. 67042. 63 12
References Continued Sand Jecklin, K. , Johnson, J. R. , & Tylka, S. (2016). Protecting Patient Safety: Can Video Monitoring Prevent Falls in High Risk Patient Populations? Journal of Nursing Care Quality, 31(2), 131– 138. https: //doi org. mainehealth. idm. oclc. org/10. 1097/NCQ. 0000000163 Struble Fitzsimmons, D. , Oswald, A. , & Di. Persia, E. (2019). Patient Location and Mobility Factors Associated with Falls on an Inpatient Geriatric Psychiatry Unit. Activities, Adaptation & Aging, 43(4), 276– 283. https: //doi org. mainehealth. idm. oclc. org/10. 1080/01924788. 2018. 1528829 Tängman, S. , Eriksson, S. , Gustafson, Y. , & Lundin Olsson, L. (2010). Precipitating factors for falls among patients with dementia on a psychogeriatric ward. International Psychogeriatrics, 22(4), 641– 649. https: //doi org. mainehealth. idm. oclc. org/10. 1017/S 1041610209991724 Wong, M. M. , & Pang, P. F. (2019). Factors Associated with Falls in Psychogeriatric Inpatients and Comparison of Two Fall Risk Assessment Tools. East Asian Archives of Psychiatry Official Journal of the Hong Kong College of Psychiatrists = Dong Ya Jing Shen Ke Xue Zhi Xianggang Jing Shen Ke Yi Xue Yuan Qi Kan, 29(1), 10– 14. 13
 Community geriatric psychiatry
Community geriatric psychiatry Geriatric psychiatry definition
Geriatric psychiatry definition Ocd ncp
Ocd ncp Cingulate herniation
Cingulate herniation Radical psychiatry sociology
Radical psychiatry sociology Global initiative on psychiatry
Global initiative on psychiatry Step 1 score percentiles 2021
Step 1 score percentiles 2021 National network of child psychiatry access programs
National network of child psychiatry access programs Criminological psychology definition
Criminological psychology definition Mse in psychology
Mse in psychology Cécile hanon
Cécile hanon Asclepiades father of psychiatry
Asclepiades father of psychiatry Addiction expert witnesses
Addiction expert witnesses Forensic psychiatry vs forensic psychology
Forensic psychiatry vs forensic psychology