Preoperative Medical Assessment Eric E Leonheart DPM Primary

- Slides: 30
Preoperative Medical Assessment Eric E. Leonheart DPM
Primary Assessment History (Detailed) Physical Exam Review of Rx Medication Review of Non-Rx Medication Evaluation of Organ Systems Advanced Directives
Other considerations Functional status Risk level of the surgery Expected blood loss Anesthesia type and duration
History HPI (NLDOCAT) PMH PSH Medications Family History Social History Review of systems
Cardiac Evaluation American College of Cardiology & American Heart Association published guidelines in 1996
Cardiac Evaluation Phase 1 – Emergent or elective If emergent and the patient’s life is in danger proceed with surgery – Undergone revascularization within 5 years – Received a recent coronary evaluation
Cardiac Evaluation Elective workup – PMH, functional status, ECG Abnormal findings non-invasive testing (exercise stress test, thallium stress, dobutamine stress ) If abnormal results are found on stress test may proceed to invasive testing (angiogram, catheterization If abnormal results are found may require coronary artery bypass graft (CABG) prior to elective procedure
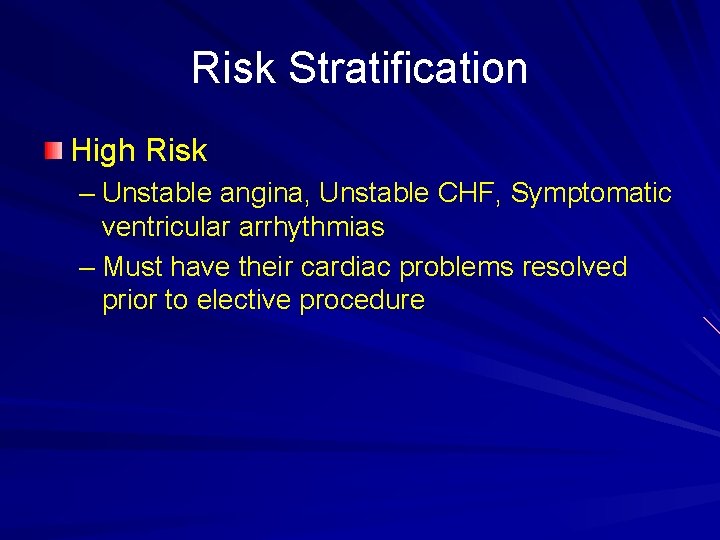
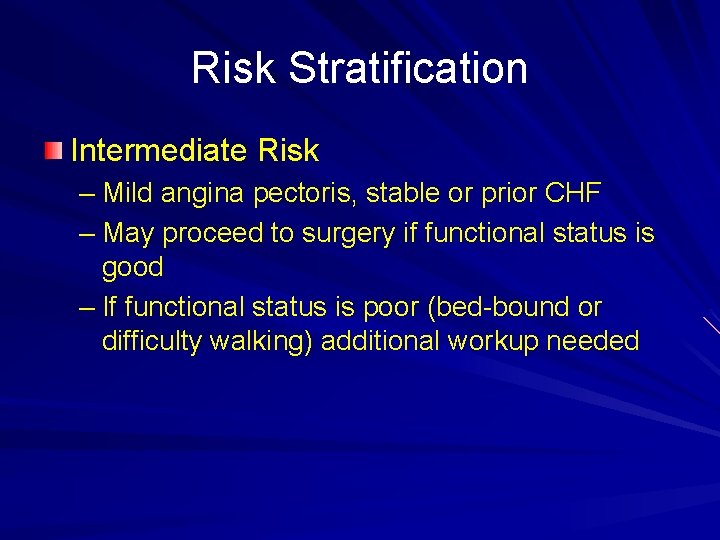
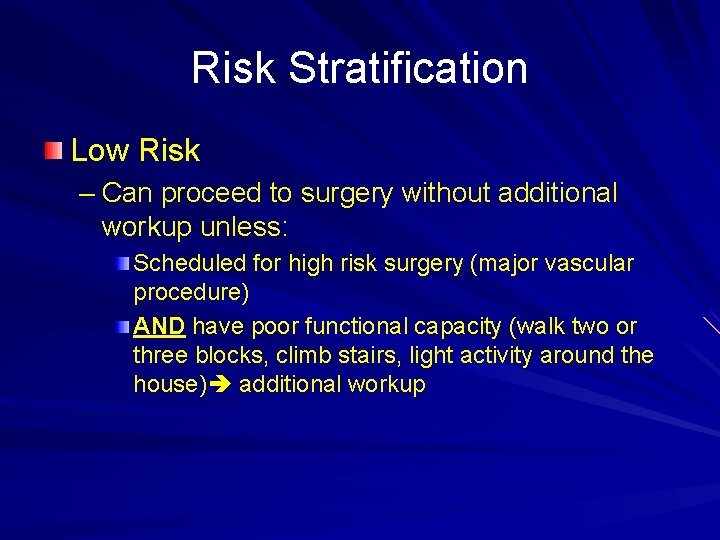
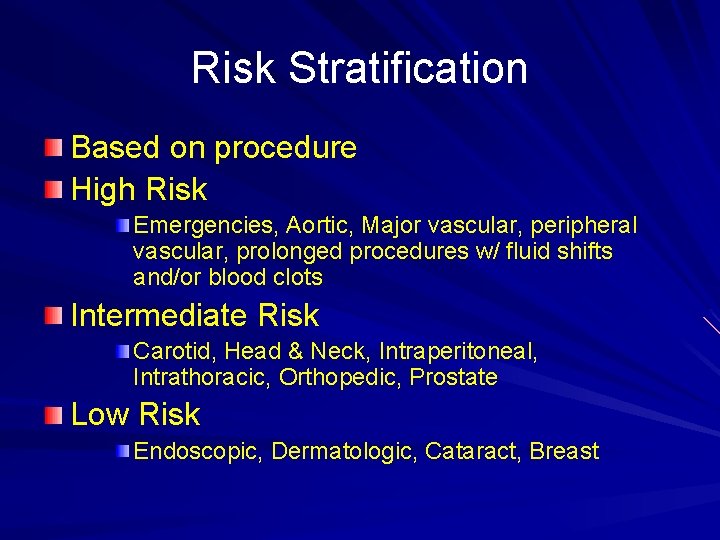
Cardiac Evaluation Risk stratification – Helps to determine the necessary work up based on the risk inherent to the procedure, patient’s PMH and functional status
Risk Stratification High Risk – Unstable angina, Unstable CHF, Symptomatic ventricular arrhythmias – Must have their cardiac problems resolved prior to elective procedure
Risk Stratification Intermediate Risk – Mild angina pectoris, stable or prior CHF – May proceed to surgery if functional status is good – If functional status is poor (bed-bound or difficulty walking) additional workup needed
Risk Stratification Low Risk – Can proceed to surgery without additional workup unless: Scheduled for high risk surgery (major vascular procedure) AND have poor functional capacity (walk two or three blocks, climb stairs, light activity around the house) additional workup
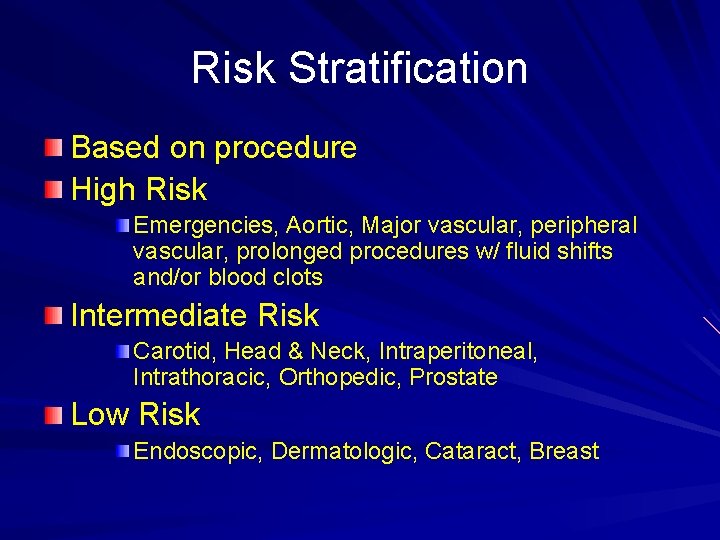
Risk Stratification Based on procedure High Risk Emergencies, Aortic, Major vascular, peripheral vascular, prolonged procedures w/ fluid shifts and/or blood clots Intermediate Risk Carotid, Head & Neck, Intraperitoneal, Intrathoracic, Orthopedic, Prostate Low Risk Endoscopic, Dermatologic, Cataract, Breast
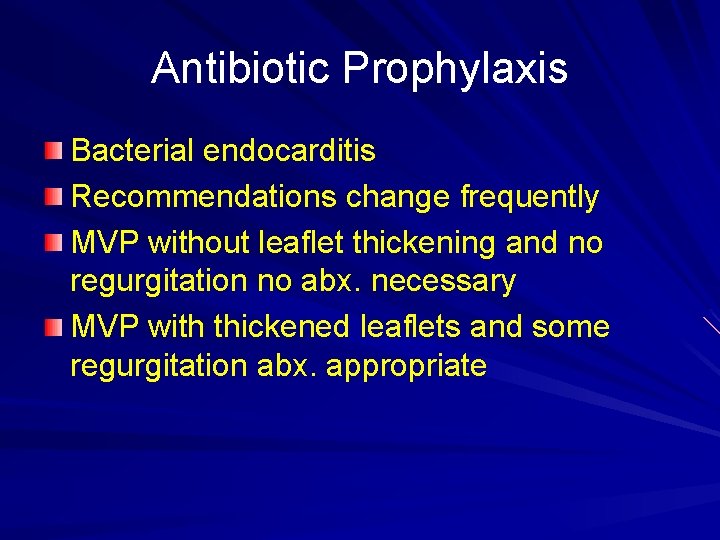
Antibiotic Prophylaxis Bacterial endocarditis Recommendations change frequently MVP without leaflet thickening and no regurgitation no abx. necessary MVP with thickened leaflets and some regurgitation abx. appropriate
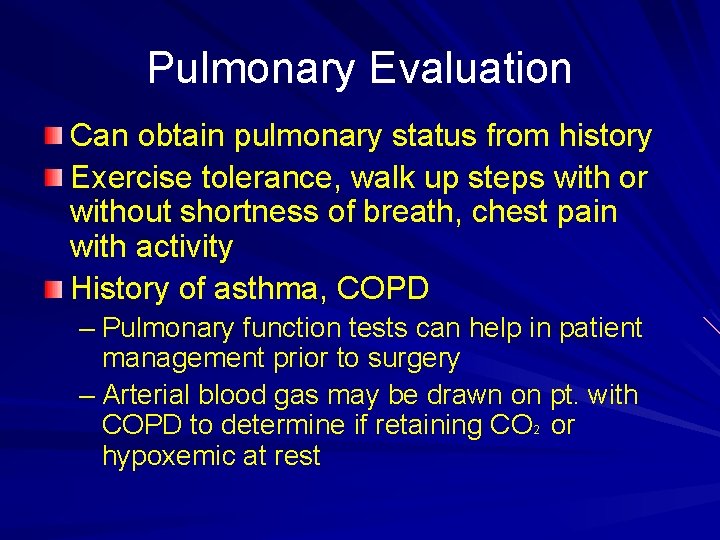
Pulmonary Evaluation Can obtain pulmonary status from history Exercise tolerance, walk up steps with or without shortness of breath, chest pain with activity History of asthma, COPD – Pulmonary function tests can help in patient management prior to surgery – Arterial blood gas may be drawn on pt. with COPD to determine if retaining CO 2 or hypoxemic at rest
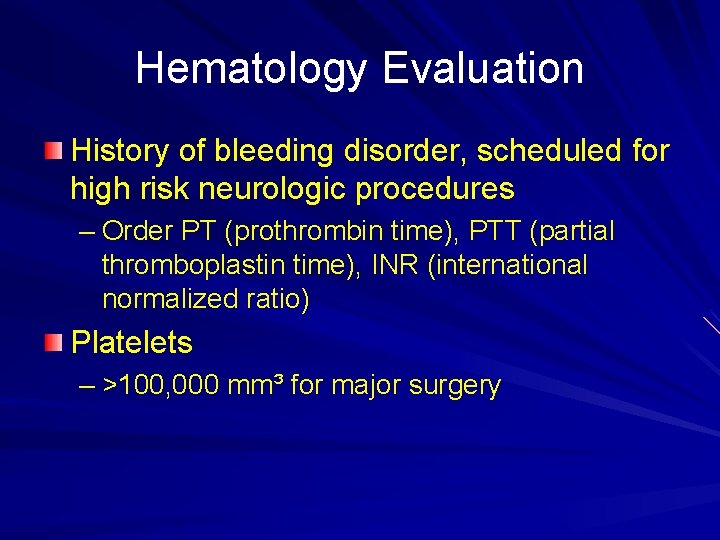
Hematology Evaluation History of bleeding disorder, scheduled for high risk neurologic procedures – Order PT (prothrombin time), PTT (partial thromboplastin time), INR (international normalized ratio) Platelets – >100, 000 mm³ for major surgery
Hematology Evaluation Medications – Anticoagulant held 48 -72 hours prior to surgery – Antiplatelet (aspirin) held 5 -7 days prior to surgery – If patient requires continuous anticoagulation IV heparin
Endocrine Evaluation Objective – Is to rule out diabetes or thyroid disease – Evaluate control of blood sugar – Determine whether the patient is experiencing adrenal suppression
Endocrine Evaluation Diabetes Fasting blood sugar < 200 mg/d. L If elevated must gain control with oral hypoglycemics or insulin prior to surgery
Endocrine Evaluation Thyroid disorders – Common symptoms, fatigue and constipation – TSH testing, possibly T 3 or T 4 – Regulation of TSH is needed prior to surgery
Endocrine Evaluation Adrenal insufficiency – Common in older patients – Even 5 mg q. d. for a year can cause adrenal suppression – Require perioperative supplementation of corticosteroids – RA patients need C spine x-rays, subluxation of atlantoaxial joint, hyperextension of the neck severed spinal cord
Endocrine Evaluation Normal supplement of hydrocortisone is 20 -30 mg/day Perioperatively increase to 200 -300 mg/day usually IV and can taper down if patient is afebrile and improving on day 4 or 5 postoperative
Gastrointestinal Evaluation History liver disease – – PT, INR evaluate coagulation Albumin testing May change anesthesia due to metabolism of agent History of ulcers or GI bleeds, may change post-op oral meds – Opiates can decrease peristalsis and lead to post-op constipation – Constipation can actually lead to delirium in patients with mild dementia
Urologic Evaluation Appropriate for; – Frequency, urgency, incontinence, hesitancy – May be signs of UTI – Patients with recent UTI should have U/A repeated if undergoing orthopedic procedures – BPH may lead to urinary retention post-op leading to UTI, pain, and the necessity for catheterization
Neurologic Evaluation Conditions of concern – Myasthenia gravis – Amyotrophic lateral sclerosis – Parkinson’s – CVA – Seizures – Dementia
Neurologic Evaluation MG, ALS neuromuscular disorders – Increased complications with general anesthesia – Greater difficulty with function post-op CVA – > incidents of clot formation, take perioperative precautions – SCD, anti-coagulate (LMH), ROM, no tourniquet
Neurologic Evaluation Seizures – Inherent risk to themselves during and after surgery Delirium – > incident with; age, MI, hypoxia, hypotension. dementia, CVA, electrolyte abnormalities, ulcer, bleeding, constipation, urinary retention, infection, hypoalbuminemia, medications (opiates), trauma, pain
Psychiatric Issues High incident of ETOH abuse Benzodiazepine abuse is common Smoking history Must manage withdrawal
Functional Status Home environment Help at home Ability to engage in the duties of daily living Discharge planning Need for nursing care, SNF placement Ability to be NWB or PWB
Conclusion Varying levels of risk Imperative for the surgeon to be aware of at risk issues Work with PCP or other specialists
