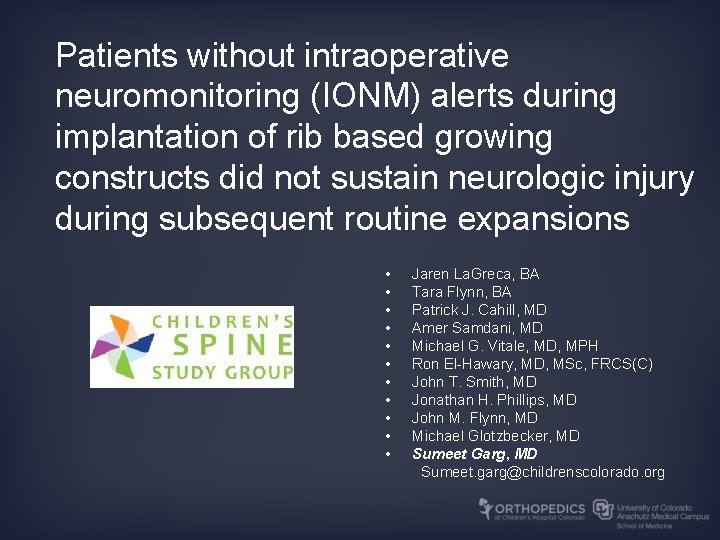
Patients without intraoperative neuromonitoring IONM alerts during implantation

- Slides: 12
Patients without intraoperative neuromonitoring (IONM) alerts during implantation of rib based growing constructs did not sustain neurologic injury during subsequent routine expansions • • • Jaren La. Greca, BA Tara Flynn, BA Patrick J. Cahill, MD Amer Samdani, MD Michael G. Vitale, MD, MPH Ron El-Hawary, MD, MSc, FRCS(C) John T. Smith, MD Jonathan H. Phillips, MD John M. Flynn, MD Michael Glotzbecker, MD Sumeet Garg, MD Sumeet. garg@childrenscolorado. org
Introduction • Skaggs JBJS 2009 • 1736 rib based growing surgery procedures – 0. 5% overall neurologic injury rate – 0% (1185 procedures) – expansions • Neuromonitoring – 1 alert during expansion • Child with history of alert at implant
Study Questions • If a patient has no neuromonitoring (IONM) alerts during implant of rib based growing construct, is monitoring necessary during expansion procedures? • Describe the rate of IONM alerts and neurologic injury
Hypothesis • Monitoring does not identify new neurologic injury during expansion of rib based growing constructs in children without monitoring alerts during initial implantation
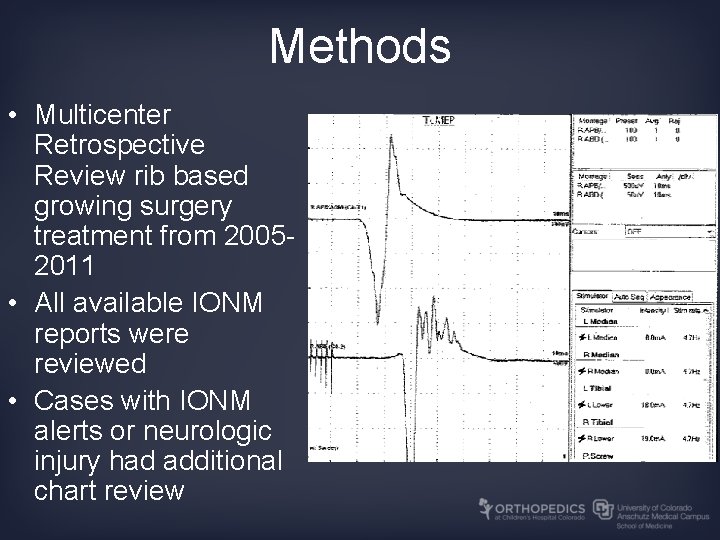
Methods • Multicenter Retrospective Review rib based growing surgery treatment from 20052011 • All available IONM reports were reviewed • Cases with IONM alerts or neurologic injury had additional chart review

Participating Sites
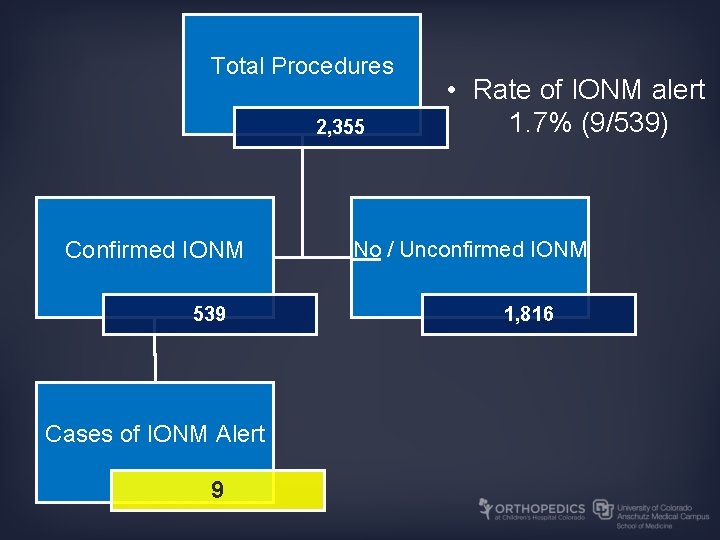
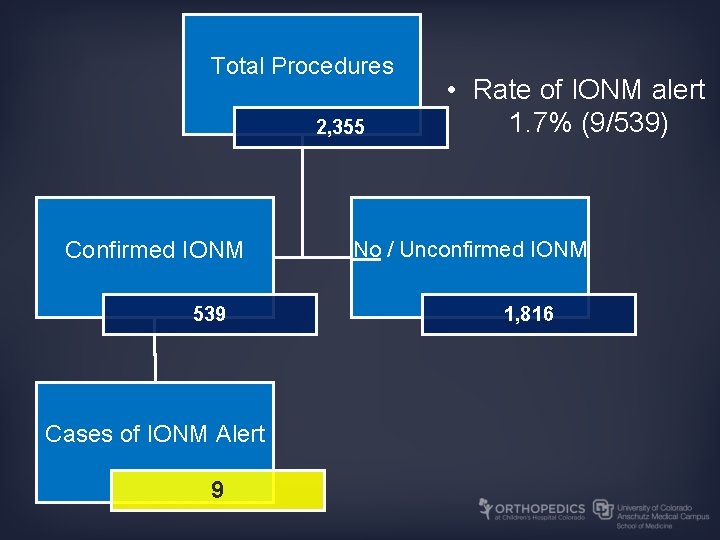
Total Procedures 2, 355 Confirmed IONM 539 Cases of IONM Alert 9 • Rate of IONM alert 1. 7% (9/539) No / Unconfirmed IONM 1, 816
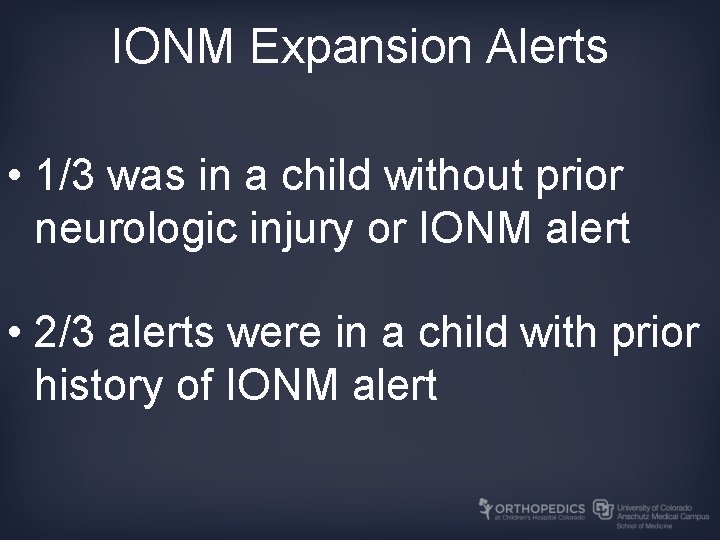
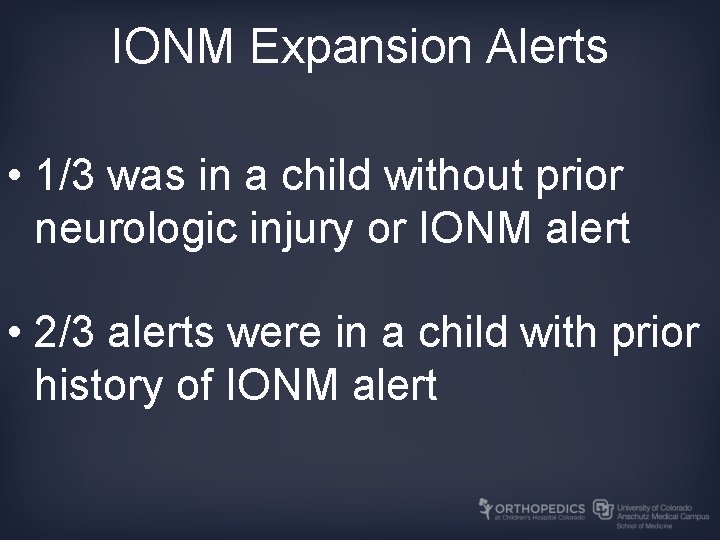
IONM Expansion Alerts • 1/3 was in a child without prior neurologic injury or IONM alert • 2/3 alerts were in a child with prior history of IONM alert
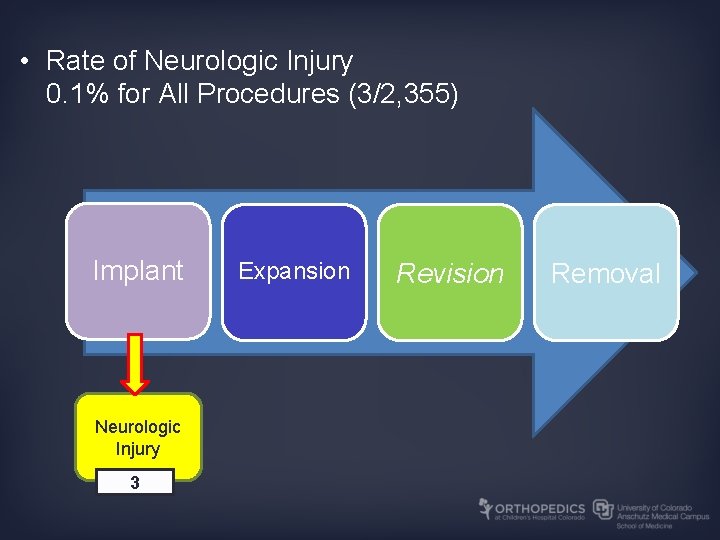
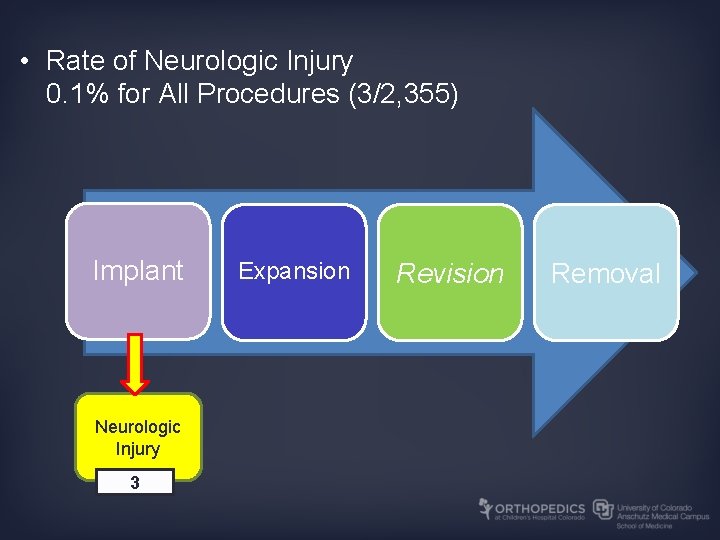
• Rate of Neurologic Injury 0. 1% for All Procedures (3/2, 355) Implant Neurologic Injury 3 Expansion Revision Removal
Conclusions • IONM did not identify new neurologic injuries during rib based growing surgery expansion procedures in patients without a history of IONM alert or neurologic injury • The highest rate of neurologic injury was during implant procedures • There were no instances of neurologic injury during expansion, revision, or removal procedures
Significance • IONM may not be necessary in patients undergoing rib based growing surgery expansion procedures who have not previously had IONM alerts or neurologic injury
References • • • 1. Campbell RM, Smith MD, Mayes TC, et al. The effect of opening wedge thoracostomy on thoracic insufficiency syndrome associated with fused ribs and congenital scoliosis. J Bone Joint Surg Am. Aug 2004; 86 -A(8): 1659 -1674. 2. Hell AK, Campbell RM, Hefti F. The vertical expandable prosthetic titanium rib implant for the treatment of thoracic insufficiency syndrome associated with congenital and neuromuscular scoliosis in young children. J Pediatr Orthop B. Jul 2005; 14(4): 287 -293. 3. Joiner ER, Andras LM, Skaggs DL. Mechanisms and risk factors of brachial plexus injury in the treatment of early-onset scoliosis with distraction-based growing implants. J Bone Joint Surg Am. Nov 2013; 95(21): e 161. 4. Devlin VJ, Schwartz DM. Intraoperative neurophysiologic monitoring during spinal surgery. J Am Acad Orthop Surg. Sep 2007; 15(9): 549 -560. 5. Schwartz DM, Auerbach JD, Dormans JP, et al. Neurophysiological detection of impending spinal cord injury during scoliosis surgery. J Bone Joint Surg Am. Nov 2007; 89(11): 2440 -2449. 6. Skaggs DL, Choi PD, Rice C, et al. Efficacy of intraoperative neurologic monitoring in surgery involving a vertical expandable prosthetic titanium rib for early-onset spinal deformity. J Bone Joint Surg Am. Jul 2009; 91(7): 1657 -1663. 7. Sankar WN, Skaggs DL, Emans JB, et al. Neurologic risk in growing rod spine surgery in early onset scoliosis: is neuromonitoring necessary for all cases? Spine (Phila Pa 1976). Aug 2009; 34(18): 1952 -1955. 8. Seyal M, Mull B. Mechanisms of signal change during intraoperative somatosensory evoked potential monitoring of the spinal cord. J Clin Neurophysiol. Oct 2002; 19(5): 409 -415. 9. Smith JT, Hung M. Is Neuromonitoring necessary for VEPTR expansion and implant exchanges in Early Onset Scoliosis? . ICEOS 2013. Proceedings of the 7 th International Congress on Early Onset Scoliosis and Growing Spine. San Diego, CA 2013. 10. Cole T, Veeravagu A, Zhang M, Li A, Ratliff JK. Intraoperative neuromonitoring in single-level spinal procedures: a retrospective propensity score-matched analysis in a national longitudinal database. Spine (Phila Pa 1976). Nov 2014; 39(23): 1950 -1959. 11. Ayoub C, Zreik T, Sawaya R, Domloj N, Sabbagh A, Skaf G. Significance and cost-effectiveness of somatosensory evoked potential monitoring in cervical spine surgery. Neurol India. 2010 May-Jun 2010; 58(3): 424 -428.
 Intraoperative cholangiogram
Intraoperative cholangiogram Pre op checklist nursing
Pre op checklist nursing What are the 3 phases of perioperative nursing?
What are the 3 phases of perioperative nursing? Percutaneous transhepatic cholangiography
Percutaneous transhepatic cholangiography Site:slidetodoc.com
Site:slidetodoc.com Site:slidetodoc.com
Site:slidetodoc.com Implantation verticale et horizontale
Implantation verticale et horizontale Implantation spotting
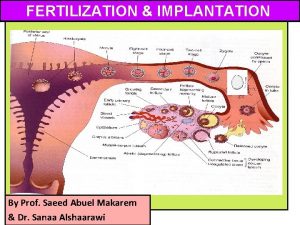
Implantation spotting Lesson 15.4 ovulation fertilization and implantation
Lesson 15.4 ovulation fertilization and implantation Implantation batiment methode
Implantation batiment methode Implantation verticale et horizontale
Implantation verticale et horizontale Subcutaneous pellet implantation
Subcutaneous pellet implantation Grand rendez-vous sst
Grand rendez-vous sst