PACE Guidance Why implement PACE To support delivery

- Slides: 20

PACE Guidance
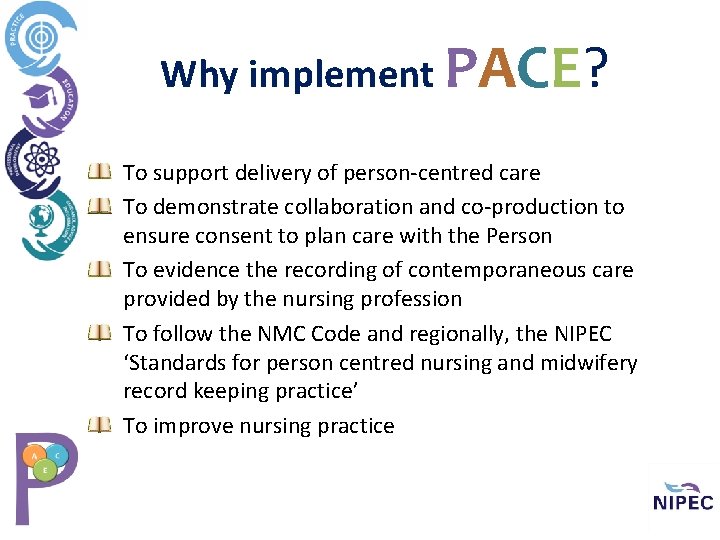
Why implement PACE? To support delivery of person-centred care To demonstrate collaboration and co-production to ensure consent to plan care with the Person To evidence the recording of contemporaneous care provided by the nursing profession To follow the NMC Code and regionally, the NIPEC ‘Standards for person centred nursing and midwifery record keeping practice’ To improve nursing practice
“Good record keeping is an integral part of nursing and midwifery practice and is an essential component of safe, effective and person centred care provision” (NIPEC, 2017, p. 5). Nurses and Midwives MUST ‘Prioritise people’ and ensure “their needs are recognised, assessed and responded to” (NMC, 2018, p. 6. )
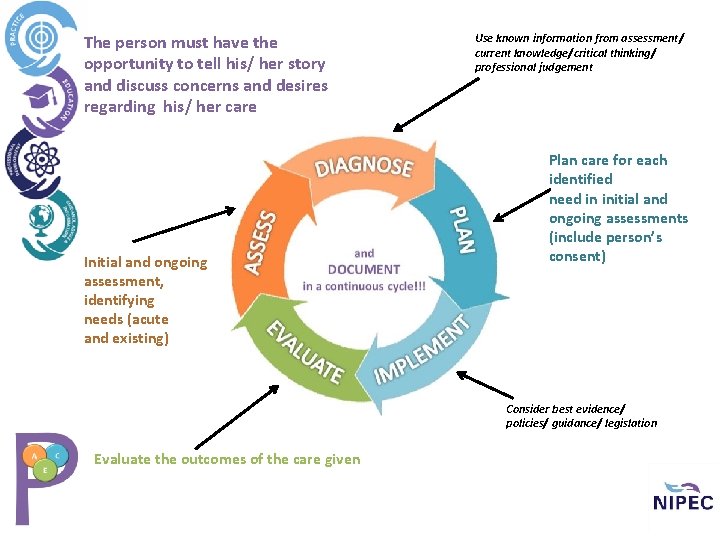
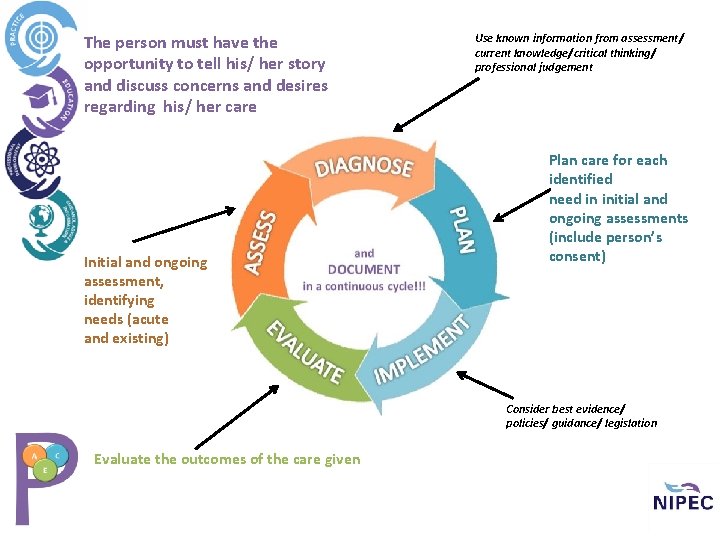
The person must have the opportunity to tell his/ her story and discuss concerns and desires regarding his/ her care Initial and ongoing assessment, identifying needs (acute and existing) Use known information from assessment/ current knowledge/critical thinking/ professional judgement Plan care for each identified need in initial and ongoing assessments (include person’s consent) Consider best evidence/ policies/ guidance/ legislation Evaluate the outcomes of the care given
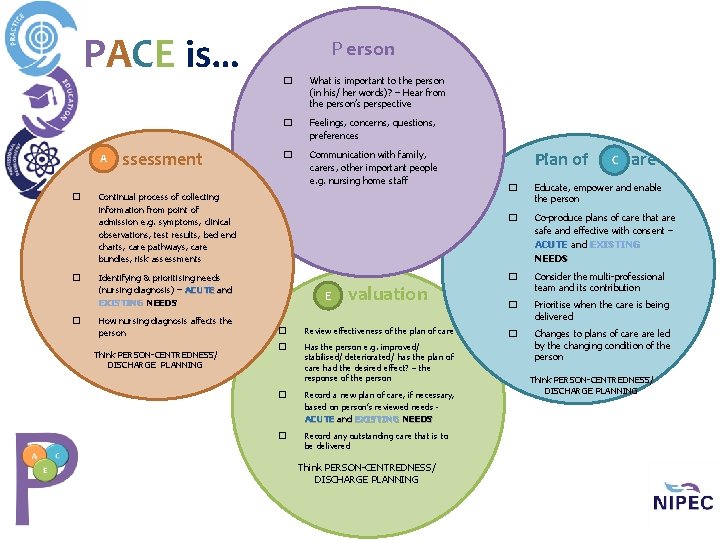
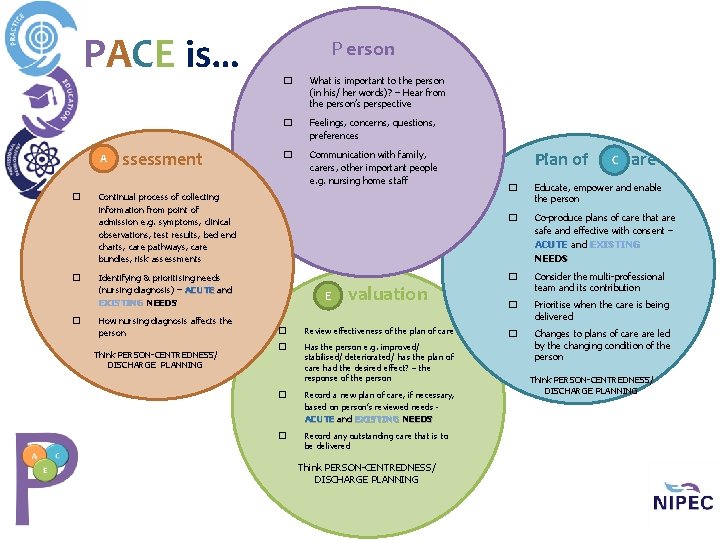
PACE is… A � � � ssessment P erson � What is important to the person (in his/ her words)? – Hear from the person’s perspective � Feelings, concerns, questions, preferences � Communication with family, carers, other important people e. g. nursing home staff Continual process of collecting information from point of admission e. g. symptoms, clinical observations, test results, bed end charts, care pathways, care bundles, risk assessments Think PERSON-CENTREDNESS/ DISCHARGE PLANNING C are � Educate, empower and enable the person � Co-produce plans of care that are safe and effective with consent – ACUTE and EXISTING NEEDS Identifying & prioritising needs (nursing diagnosis) – ACUTE and EXISTING NEEDS How nursing diagnosis affects the person Plan of E valuation � Review effectiveness of the plan of care � Has the person e. g. improved/ stabilised/ deteriorated/ has the plan of care had the desired effect? – the response of the person � Record a new plan of care, if necessary, based on person’s reviewed needs - ACUTE and EXISTING NEEDS � Record any outstanding care that is to be delivered Think PERSON-CENTREDNESS/ DISCHARGE PLANNING � Consider the multi-professional team and its contribution � Prioritise when the care is being delivered � Changes to plans of care led by the changing condition of the person Think PERSON-CENTREDNESS/ DISCHARGE PLANNING
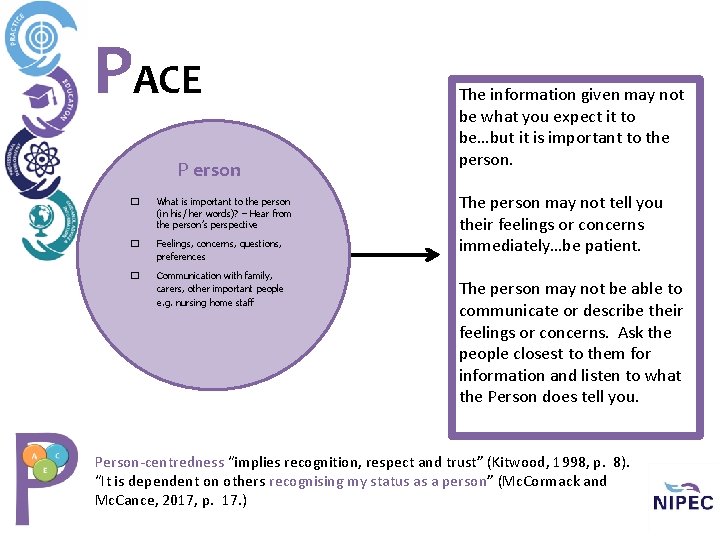
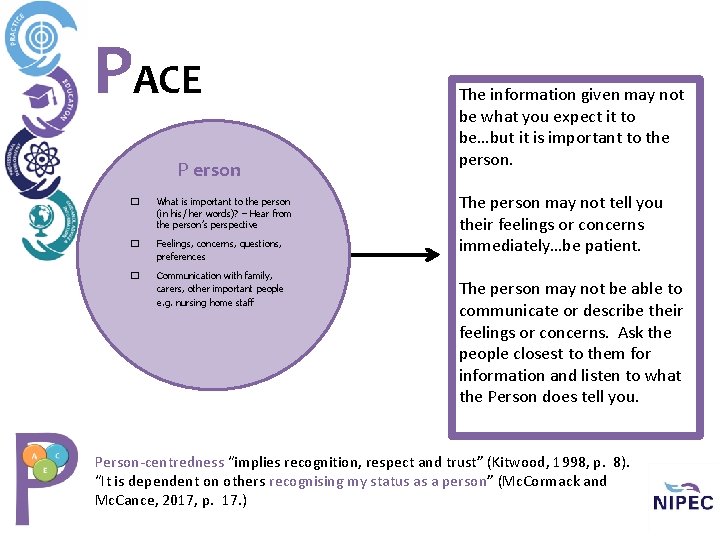
PACE P erson � What is important to the person (in his/ her words)? – Hear from the person’s perspective � Feelings, concerns, questions, preferences � Communication with family, carers, other important people e. g. nursing home staff The information given may not be what you expect it to be…but it is important to the person. The person may not tell you their feelings or concerns immediately…be patient. The person may not be able to communicate or describe their feelings or concerns. Ask the people closest to them for information and listen to what the Person does tell you. Person-centredness “implies recognition, respect and trust” (Kitwood, 1998, p. 8). “It is dependent on others recognising my status as a person” (Mc. Cormack and Mc. Cance, 2017, p. 17. )
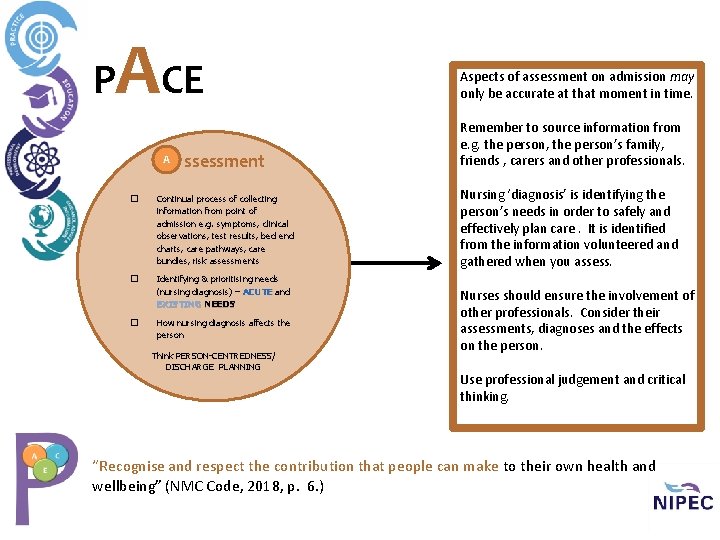
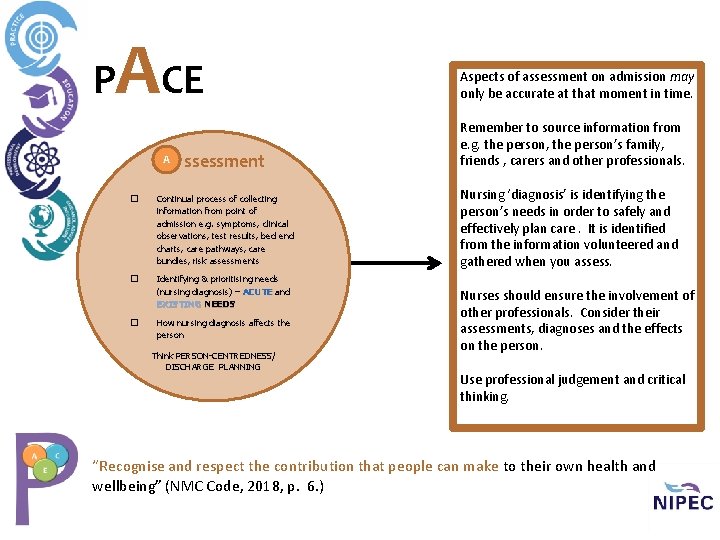
P ACE A ssessment � Continual process of collecting information from point of admission e. g. symptoms, clinical observations, test results, bed end charts, care pathways, care bundles, risk assessments � Identifying & prioritising needs (nursing diagnosis) – ACUTE and EXISTING NEEDS � How nursing diagnosis affects the person Think PERSON-CENTREDNESS/ DISCHARGE PLANNING Aspects of assessment on admission may only be accurate at that moment in time. Remember to source information from e. g. the person, the person’s family, friends , carers and other professionals. Nursing ‘diagnosis’ is identifying the person’s needs in order to safely and effectively plan care. It is identified from the information volunteered and gathered when you assess. Nurses should ensure the involvement of other professionals. Consider their assessments, diagnoses and the effects on the person. Use professional judgement and critical thinking. “Recognise and respect the contribution that people can make to their own health and wellbeing” (NMC Code, 2018, p. 6. )
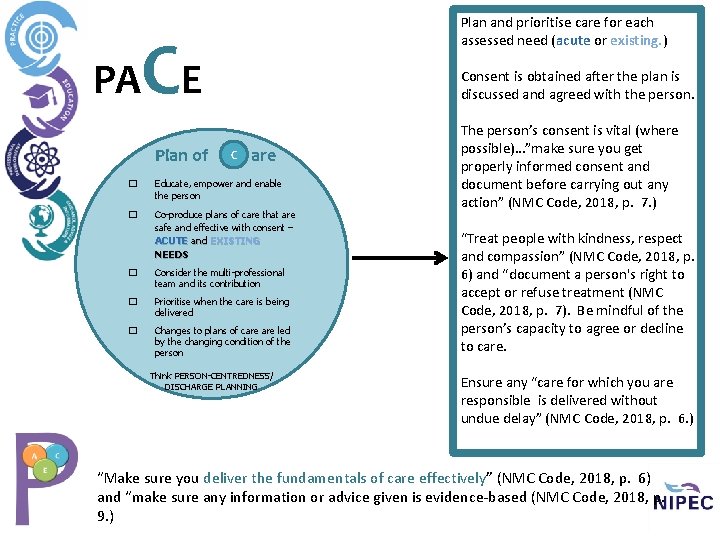
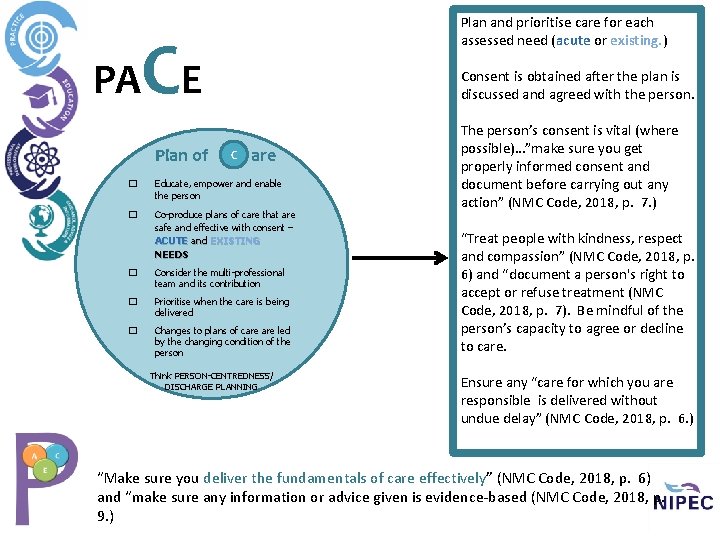
Plan and prioritise care for each assessed need (acute or existing. ) C PA E Plan of Consent is obtained after the plan is discussed and agreed with the person. C are � Educate, empower and enable the person � Co-produce plans of care that are safe and effective with consent – ACUTE and EXISTING NEEDS � Consider the multi-professional team and its contribution � Prioritise when the care is being delivered � Changes to plans of care led by the changing condition of the person Think PERSON-CENTREDNESS/ DISCHARGE PLANNING The person’s consent is vital (where possible)…”make sure you get properly informed consent and document before carrying out any action” (NMC Code, 2018, p. 7. ) “Treat people with kindness, respect and compassion” (NMC Code, 2018, p. 6) and “document a person's right to accept or refuse treatment (NMC Code, 2018, p. 7). Be mindful of the person’s capacity to agree or decline to care. Ensure any “care for which you are responsible is delivered without undue delay” (NMC Code, 2018, p. 6. ) “Make sure you deliver the fundamentals of care effectively” (NMC Code, 2018, p. 6) and “make sure any information or advice given is evidence-based (NMC Code, 2018, p. 9. )
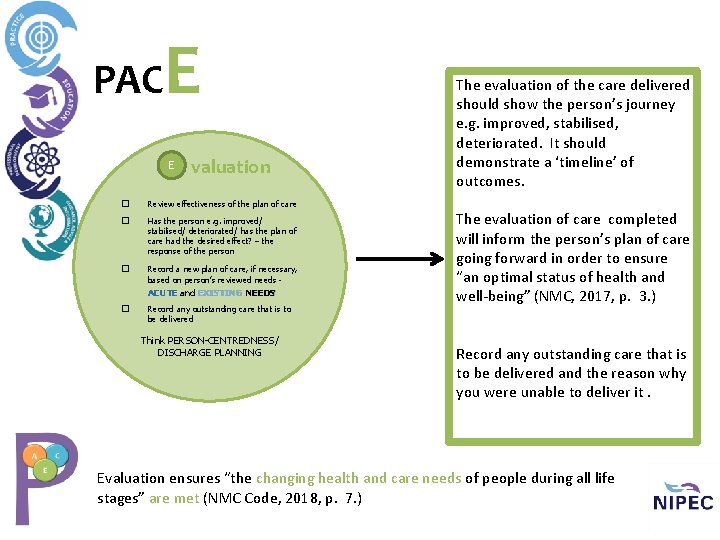
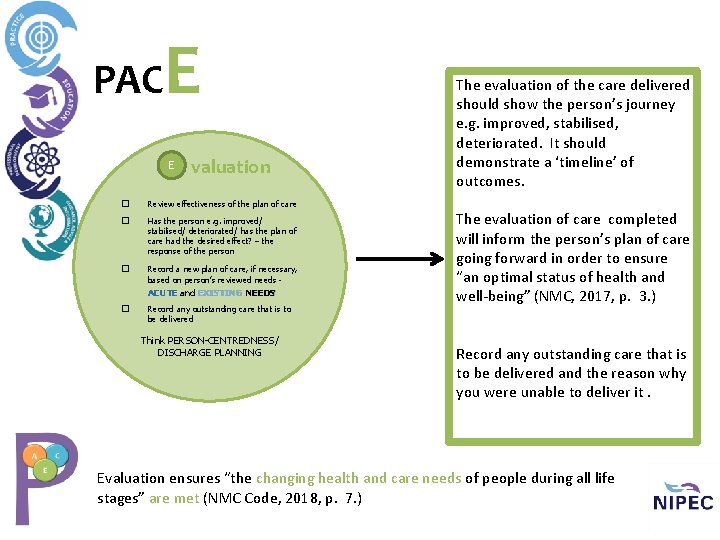
PAC E E valuation � Review effectiveness of the plan of care � Has the person e. g. improved/ stabilised/ deteriorated/ has the plan of care had the desired effect? – the response of the person � Record a new plan of care, if necessary, based on person’s reviewed needs - ACUTE and EXISTING NEEDS � Record any outstanding care that is to be delivered Think PERSON-CENTREDNESS/ DISCHARGE PLANNING The evaluation of the care delivered should show the person’s journey e. g. improved, stabilised, deteriorated. It should demonstrate a ‘timeline’ of outcomes. The evaluation of care completed will inform the person’s plan of care going forward in order to ensure “an optimal status of health and well-being” (NMC, 2017, p. 3. ) Record any outstanding care that is to be delivered and the reason why you were unable to deliver it. Evaluation ensures “the changing health and care needs of people during all life stages” are met (NMC Code, 2018, p. 7. )
When should I record PACE? As early in the shift as possible, at the bedside!!! As often as is necessary to demonstrate that you have assessed the person, planned care and evaluated the care while considering the person’s opinions, thoughts, feelings, preferences and priorities.
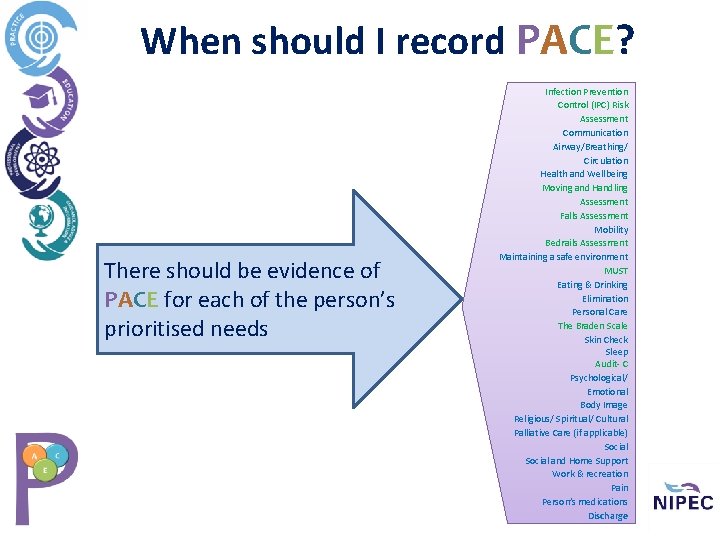
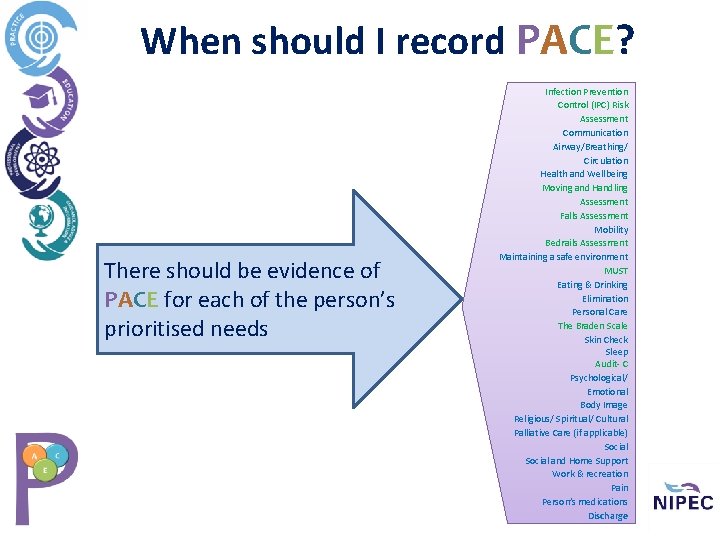
When should I record PACE? There should be evidence of PACE for each of the person’s prioritised needs Infection Prevention Control (IPC) Risk Assessment Communication Airway/Breathing/ Circulation Health and Wellbeing Moving and Handling Assessment Falls Assessment Mobility Bedrails Assessment Maintaining a safe environment MUST Eating & Drinking Elimination Personal Care The Braden Scale Skin Check Sleep Audit- C Psychological/ Emotional Body Image Religious/ Spiritual/ Cultural Palliative Care (if applicable) Social and Home Support Work & recreation Pain Person’s medications Discharge
What should I record ? The first entry in the document (on admission) - there should be reference to P, A and C for care needs in the nursing record. The first entry of each shift and the handover of nursing care- there should be reference to P, A, C and E for care needs in the nursing record. Update record appropriately throughout the shift using the PACE framework.
How should I record PACE? Identify the nursing care needs i. e. the ‘acute’ (ongoing and changing) or ‘existing’ (ongoing but unchanging. ) If a short- term care need with minimal risk to the person is identified, the P, A, C and E can be documented together in the record.
Acute care needs (ongoing and changing) If person’s need(s) change, a new and complete PACE record must be documented. There may be multiple acute care needs identified. Acute care needs can be ongoing, even when the person is discharged e. g. a community nurse, treatment room nurse, or the person themselves may be delegated the care (with professional community support. )
Existing care needs (ongoing and unchanging) If the person’s care need is stable, unchanging and is not an acute care need, the Assessment and Plan of Care should be rewritten at least weekly. If the person’s: • • • needs change (A) input into his/ her care or plan of care changes (C) condition changes in response to the care being delivered (E, ) weekly revision and rewriting of the PACE record IS NOT APPROPRIATE
Existing care needs (ongoing and unchanging) If a previously documented PACE record is being referenced for an existing care need, a clear timeline and note of the professional’s name should be recorded in the nursing record in order to indicate which Assessment and Plan of Care is being referenced. The Assessment and Plan of Care being referenced MUST be accurate, evidence based, robust and the nursing professional who is referencing it MUST be satisfied that it is appropriate to the PACE framework. A daily Evaluation of the outcomes of care planned and delivered MUST be recorded. Nurses must use professional judgement and critical thinking when considering existing care needs.
Important guidance According to the NMC Code, a nurse should: 10. 1 complete records at the time or as soon as possible after an event, recording if the notes are written some time after the event. Date and time the entry when you are writing it but reference back to a time when e. g. the care was completed.
Important guidance According to the NMC Code, a nurse should: 10. 4 attribute any entries you make in any paper or electronic records to yourself, making sure they are clearly written, dated and timed. If another person carried out care you are documenting, ensure the person’s name is recorded against the care he or she gave. If the care is traceable in other nursing documentation e. g. a fluid balance chart, reference to the chart is satisfactory i. e. document ‘catheter emptied as per fluid balance chart” (this is provided the clinical area ensures that all staff (including bank and agency) sign the register at the end of the person’s record
PACE encourages Registered Nurses to: Prioritise people by involving “the person for whom the care is being provided for” (NIPEC, 2017, p. 6. ) Prioritise people by documenting their person-centred assessment, plan of care and evaluation in a structured, factual and holistic manner, while ensuring the person shares “in decisions about their treatment and care” through “informed consent” (NMC, 2018, p. 7. )
PACE encourages Registered Nurses to: Practise effectively’ by “keeping clear and accurate records” (NMC, 2018, p. 9) to show that safe, effective, compassionate and person - centred care is being given to people and their families/ carers. Practise effectively by “ keeping clear and accurate records” (NMC, 2018, p. 9) to show evidence of decision making processes and professional ability. This should include documentation showing evidence based ways of working in clinical practice. Practise effectively by being “accountable for your decisions to delegate tasks and duties to other people” (NMC, 2018, P. 12. )