Overcoming Specialists Apathy Toward Family Medicine Chris Jenkins


- Slides: 22
Overcoming Specialist’s Apathy Toward Family Medicine Chris Jenkins, M. D. Family Medicine global Health Workshop September 8 -10, 2010
The Problem (Consultants Need to Recognize It) • Specialists are often apathetic or resistant to the specialty of family medicine* • Need to win the active support and acceptance of specialists for FM • Goals of this talk – – Give historical context Identify reasons for specialist's apathy A few country specific examples and suggestions Formulate ideas for winning specialists cooperation and support of family medicine * ‘General practice’ is the term most commonly used outside the US
The Situation: Historical Context • Countries with specialty based medical systems – Historically • Priority was training specialists • Salaries low for all doctors but on par with salaries in other sectors • Medical profession seen as prestigious because of level of training/education • Lacked a well trained generalist. Generalists were – “Feltchers, ” bare foot doctors, etc, not seen as prestigious • Health care providers who did not specialize were poorly trained and gave low level care
The Situation: Current Circumstances • Countries with specialty based medical systems – Present • Persuaded that primary care is important – Alma-Ata Declaration of 1978 – Prevention, management of care, care of common illness, etc. • Trying to include generalists with higher levels of training into their medical systems – – Retraining programs Post-graduate residency training programs IMF and others willing to fund these efforts Transitioning to balance between primary care and specialty care • Economies changing – Government control verses private sector – Primary care seen as an economical way to provide care for many people
The Situation : Current Circumstances • Countries with specialty based medical systems – Economics • Salaries changing: – business people can make much more now – Wide gap between specialty salaries and salaries of primary care doctors » Official GP salaries often higher » Unofficial GP salaries in reality much lower • Often no jobs available for GPs – Attitudes, perceptions, values • Specialty training remains prestigious • GPs associated with low lever trained “bare foot” doctors • Other specialists do not respect GP’s training or skills
The Situation • Countries with specialty based medical systems – GP models • Poor models of general practice lead to professional dissatisfaction • Lower level of training than necessary to accomplish assigned tasks • Unattractive to medical students – Patient perceptions and attitudes • Lack accurate knowledge of specialty • Lack confidence in specialty • Under utilize services
The Situation: Specialist’s Apathy • Do not understand the role and concept of family medicine • Do not understand not convinced of the need for a well trained generalist • General practice associated with low level “feltchers” and “bare foot doctors” – Consider GPs poorly trained – “They don’t know as much as I do about my specialty. What use are they? ” • May see GPs as competition for patients
The Situation: Specialist’s Apathy • Reluctance to teach – Turf: Specialty faculty often feel GPs/FPs don’t need depth of knowledge – or shouldn’t be in their specialty teaching service at all – Specialists do not understand their role in teaching GPs • GPs trained to manage common conditions in many specialty areas and to know when to refer – Usually do not know how to teach GP residents • How to select information from their body of knowledge • How to design curriculum
The Situation: Specialist’s Apathy • Reluctance to teach, cont. – Specialists may not be reimbursed for teaching GPs but it requires more work on their part – Economics: Students represent future competition • Specialists don’t understand referral systems – Drafted from their own specialty to head GP departments and be faculty • Specialists not involved – Neglected by national planners – Not adequately involved in planning the training of the new specialty – They don’t “own” their role in the new specialty
Specialty Apathy: What to Do? • No perfect solution yet • Most countries have not dealt with the problem adequately • Some have alienated other specialists • Catch 22: – specialists must be involved because there are no fully trained family doctors to begin with – Specialists usually do not want to be involved
Some Examples: China • Huge country, huge medical system • Decided in 1999 that GP would be part of medical system • Capital Medical University – write policy and design training for GP in China • Experienced the common reactions from specialists – Went slow: did not make a large scale initial attempt

Some Examples: China • The first 8 -10 years: Retraining programs – 600 hour (later reduced to 500 hours) program – Second-tier medical school graduates put through retraining – Mixed results • The next phase – residency trained GPs • Currently about 40 pilot GP programs across the country – Three years – Includes hospital training and specialty departments – Teaching specialists from these programs brought to Beijing for training
Some Examples: China • Annual national conference for specialists teaching at pilot programs, cont. – Four day conference • Two days led by faculty of CMU: government policy, national direction of GP, finances, etcetera • Two days by foreign experts in general practice: – Philosophy of GP, role in health care system, scope of practice – Role of specialists in teaching GP residents » Why they are needed » How to decide curriculum » Common conditions » Recognition of disease requiring referral » Cooperation with GPs: referrals, more interesting cases for specialists and common ones treated by GPs
Some Examples: China • Annual national conference for specialists teaching at pilot programs, cont. – Four day conference, cont. • Faculty development: how to teach – Teaching analytical thinking skills – Current adult learning theory and teaching methodologies – Precepting – Teaching in the hospital and in the clinic – Etcetera • Whole person care • Other
Some Examples: China • Annual national conference for specialists teaching at pilot programs, cont. – Four day conference, cont. – Approximately 130/year, annually for four years • Basically the same material each year with new specialists from new and older programs • New knowledge and changed attitudes • Return to programs with new appreciation for general practice, a new understanding of their role in training GPs and the complementary nature of primary care and subspecialists and some new teaching skills • A big country – 520 specialists is a small beginning but they are in strategic centers
Some Examples: China Comments from Other Programs • Relationship building with specialists is key – Invite specialists to lecture to GP residents in GP clinics – Have occasional specialty clinic for selected patients – Attend hospital and specialists sponsored CME and make one-on-one contacts – Teach English at government hospitals – the GPs become the specialists

Some Examples: China Comments from Other Programs • Money – salary is very important – Often determining factor in medical student’s specialty choice – Higher salary for residents attracts better students which improves GP reputation • Shenzhen paid GP residents 3 x what others got • Program very competitive: 1 in 5 accepted; excellent students – “Higher salary for GP jobs would make even the specialists take notice” • US example typical – primary care seen as money saver. Save more by paying FPs less – Medical students no longer want to go into FM
Some Examples: Afghanistan • A job description: outlines responsibilities with respect to the training program • Involve them in morning report and AA • Involve them in faculty meetings and decision making • Working alongside of them in medical staff committee work, e. g. , QA, infection control, etc. Thus we all serve on the medical staff, and work together to make the hospital better • Intentionally doing faculty development • “The onus is on us to prove it works”
Some Examples: Central Asia (Local Level) • Mixed efforts, mixed results – Kyrgyzstan • System made a very good effort t o train and incorporate GPs into the system • Considered the best trained GPs in Central Asia • MOH – started GP training programs in medical schools • Trained faculty to understand teach general practice • Initially recruited good students to be trained • currently – Salary problems – Emigration – Low student interest » Less qualified students now applying and fewer of them
Some Examples: Central Asia (Local Level) • Mixed efforts, mixed results – Kazakhstan • Had support of MOH but never won the minds of leaders • Had conferences for specialists to explain specialty • Medical conferences in schools by foreigners for students to promote and explain the concept and scope of practice • Failed to – – Make adequate model Create jobs for those going into general practice Pay well enough to enable practitioners to live on salary Generate enthusiasm except in a few advocates • Limping along now • However, it has received post graduate training programs with other specialties so may succeed in the long run
Summary: Gaining Specialist Cooperation • No perfect answers - a long term project • Relationships are key • Communication and doctor education is critical – Systematic program of informing and training specialists – Philosophy, role, need, practice of new specialty – New specialty not competition but collaboration • Generate referrals • Specialists do cases they trained for • GPs help them care for patients they were not trained for • Involvement in planning from beginning • Help them understand their role in training – Help develop curriculum – High level training in primary care – Reimburse for time spent in training GPs • Encourage planners to pay GPs adequately
Questions?
 Apathy
Apathy Apathy word origin
Apathy word origin Employee apathy
Employee apathy Apathy in a sentence
Apathy in a sentence Cyan medical term example
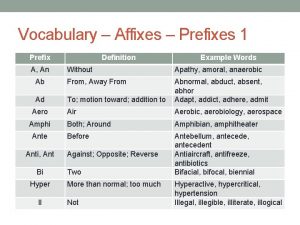
Cyan medical term example The prefix “a” or “an” means:
The prefix “a” or “an” means: Apathy etymology
Apathy etymology Etymology of apathy
Etymology of apathy Apathy is the solution
Apathy is the solution Overcoming perfectionism roz shafran
Overcoming perfectionism roz shafran A technique for overcoming internal fragmentation
A technique for overcoming internal fragmentation Knowledge2practice
Knowledge2practice Barriers of communication in pharmacy
Barriers of communication in pharmacy Overcoming life issues
Overcoming life issues Overcoming the dark side of leadership
Overcoming the dark side of leadership Booker seven basic plots
Booker seven basic plots Overcoming hindrances to spiritual development
Overcoming hindrances to spiritual development Overcoming trials and temptations
Overcoming trials and temptations Overcoming
Overcoming Overcoming barriers to employment
Overcoming barriers to employment All the blocks you want
All the blocks you want Dram refresh failure
Dram refresh failure Scripture about overcoming adversity
Scripture about overcoming adversity