Nursing Care Interventions in Clients with PituataryAdrenal Gland


- Slides: 22
Nursing Care & Interventions in Clients with Pituatary/Adrenal Gland Disorders Keith Rischer RN, MA, CEN 1
Today’s Objectives… Ø Ø Ø Compare and contrast pathophysiology & manifestations of pituitary/adrenal gland dysfunction. Identify, nursing priorities, and client education associated with pituitary/adrenal gland dysfunction. Interpret abnormal laboratory test indicators of pituitary/adrenal gland dysfunction. Analyze assessment to determine nursing diagnoses and formulate a plan of care for clients with pituitary and adrenal gland dysfunction. Describe the mechanism of action, side effects and nursing interventions of pharmological management with pituitary and adrenal gland dysfunction. 2

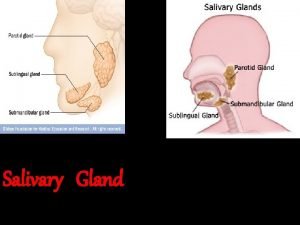
Patho: Endocrine System Ø Endocrine glands • • • Ø Pituitary glands Adrenal glands Thyroid glands Islet cells of pancreas Parathyroid glands Gonads Hormones • Negative feedback mechanism 3
Patho: Pituitary Gland Ø Anterior • • • Ø Growth hormone Thyroid Stimulating Hormone (TSH) Adrenocorticotropic Hormone (ACTH) Follicle Stimulating Hormone (FSH) Luteinizing Hormone (LH) Posterior • Vasopressin ü Antidiuretic hormone (ADH) 4
Anterior Hypo-pituitarism Ø Causes • Tumor ü • • Ø Ø • Ø Anorexia Shock Growth hormone Gonadatropins • Ø Brain or pituitary Women Men TSH ACTH 5
Anterior Hypo-pituitarism Ø Labs • • Ø T 3, T 4 Testerone, estradiol levels Nursing interventions • Replacement of deficient hormones ü Androgen therapy – gynecomastia can occur ü Estrogens and progesterone ü Growth hormone • Assess function of target organ ü thyroid 6
Anterior Hyper-pituitarism Ø Causes • Pituitary tumors or hyperplasia ü Gigantism ü Acromegaly 7

Hypophysectomy Ø Post op Care • Closely monitor neuros • Assess for postnasal drip “halo sign” • Avoid coughing early after the surgery. • Keep HOB elevated • Assess for meningitis • Replace hormones and glucocorticoids as needed • Diabetes insipidus ü Assess I&O closely first 24 hours 8
Posterior Pituitary Gland: Diabetes Insipidus Ø Patho • Antidiuretic hormone ü • deficiency Water unable to be reabsorbed 9
Diabetes Insipidus: Clinical Manifestations Ø CV • • • Ø Renal • Ø Dramatic increased u/o Skin • Ø Tachycardia Hypotension Heme concentration Dry mucous membranes Neuro • • • Thirst Irritable Lethargy to unresponsive 10
Diabetes insipidus: Interventions Ø Nursing Diagnostic Statements • • Ø Priorities • • Ø Deficient fluid volume r/t… Decreased cardiac output r/t… Early detection dehydration Maintain adequate hydration Desmopressin acetate (DDAVP) intranasally • • Synthetic vasopressin I&O-daily weights 11
Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH) Ø Patho • Vasopressin (ADH) ü • Water retained ü Ø Increased Dilutional hyponatremia Causes • • Cancer Infection Chemo agents COPD 12
SAIDH: Clinical Manifestations Ø Fluid retention • Ø Neuro • • • Ø Lethargy HA Altered LOC CV • Ø Hyponatremia Tachycardia Renal • u/o decrease 13
SAIDH: Nursing Interventions Ø Nursing diagnostic priorities • • Ø Ø Fluid restriction Drug therapy • • Ø Decreased cardiac output r/t… Fatigue Diuretics Hypertonic saline (3%) Neurologic assessment • • Orientation Safe environment 14
Adrenal Glands Ø Patho • • • Aldosterone Cortisol Catecholamines ü Epinephrine – Beta receptors ü Norepinephrine – Alpha receptors • Deduced aldosterone levels ü Hyperkalemia – acidosis ü Hyponatremia – hypovolemia 15
Adrenal Glands: Hypofunction Ø Acute adrenal insufficiency • • Addisonian crisis Causes ü Steroids Ø stopped abruptly Clinical manifestations • • Muscle weakness, fatigue, constipation Hypoglycemia ü • • Diaphoresis, tachy, tremors Blood volume depletion Hyperkalemia ü cardiac arrest-rhythm changes 16
Addison’s Disease: Interventions Ø Ø Ø Promote fluid balance and monitor fluid deficit. • Careful I&O • Record weight daily Assess vital signs every 1 to 4 hours, assess for dysrhythmias or postural hypotension. Monitor laboratory values • Na • K • Glucose Cortisol and aldosterone replacement therapy Diet - ↑ sodium, ↓ potassium, ↑ Carbs 17
Adrenal Gland: Hyperfunction Patho Ø Pheochromocytoma Ø Cushing’s syndrome Ø • Causes ü Primary/secondary malignancies ü Steroids • • Lymphocytes Inflammatory/immune response 18
Cushing’s Disease: Clinical Manifestations Ø Obesity • Changes in fat distribution ü Ø Ø Ø Facial hair for women Thin skin Blood vessels fragile Acne Immunosupression HTN • Ø Moon face Water/sodium retention Lab changes • • Glucose WBC Sodium Potassium 19
Nursing Priorities Excess fluid volume r/t… Ø Risk for infection r/t… Ø Deficient knowledge Ø 20
Medical Management Ø Drug therapy • • Mitotane If caused by side effect of medication ü Ø try to decrease or change meds Radiation therapy • Pituitary tumors 21
Cushings: Surgical Management Total hypophysectomy Ø Adrenalectomy Ø Preoperative care Ø • Ø Correct lyte imbalances Postoperative care • • • Prevent skin breakdown Pathologic fractures Education regarding lifelong steroid use ü Take with meals ü Never skip doses ü Weigh daily 22
 Pituitary gland and pineal gland spiritual
Pituitary gland and pineal gland spiritual Thyoid gland
Thyoid gland Nursing process stages
Nursing process stages Examples of implementation in nursing process
Examples of implementation in nursing process Collaborative interventions nursing
Collaborative interventions nursing Nursing care plans examples
Nursing care plans examples Nursing interventions for dvt
Nursing interventions for dvt Explain nursing process
Explain nursing process Example of community health nursing diagnosis statement
Example of community health nursing diagnosis statement Goals and expected outcomes
Goals and expected outcomes Nursing management of rheumatoid arthritis
Nursing management of rheumatoid arthritis Hypertensive crisis management
Hypertensive crisis management Skeletal traction vs skin traction
Skeletal traction vs skin traction Short term goal for anxiety
Short term goal for anxiety Ncp for ocd
Ncp for ocd Independent nursing interventions
Independent nursing interventions Dependent nursing interventions
Dependent nursing interventions Gout nursing care plan
Gout nursing care plan Nwcc nursing
Nwcc nursing Umbilical cord prolapse interventions
Umbilical cord prolapse interventions Nursing management of chronic pancreatitis
Nursing management of chronic pancreatitis Pancreatitis nursing interventions
Pancreatitis nursing interventions Nursing diagnosis for vision impairment
Nursing diagnosis for vision impairment