Joint Strategic Needs Assessment Workshop Crawley and Horsham


- Slides: 40
Joint Strategic Needs Assessment Workshop Crawley and Horsham & Mid Sussex CCGs May 2012 Catherine Scott Consultant in Public Health
Aims of workshop • Share information on health needs of the population • Identify key priorities for each locality to inform commissioning intentions 2012/13 • Identify areas where the JSNA needs to be developed to support CCGs • JSNA document for each CCG to be used for authorisation process
The process of Joint Strategic Needs Assessment (JSNA)
JSNA – what it is • The overarching primary evidence base on factors that influence the health of a population including the social, environmental, economic determinants of health • Support for decision making – – What are the gaps? What evidence is there that we could do better? What do we want to achieve? What are the most effective and cost effective interventions? • A dynamic and flexible process • A range of products IDEA
Why do we need it? • Statutory responsibility for CCGs and LAs • Demand is not the same as need • Partnership working is the only way to address some issues • A single agreed picture of needs is essential for strategic planning
JSNA framework • Data collection – – Routine data Local research eg surveys Professional views Public/patient views • Data analysis – – – – Ad hoc query based analysis Surveillance for unexpected Modelling Area based analysis Benchmarking Evaluation Cost benefit analysis • Interpretation in context – Statistical and methodological issues – Evidence from research – Experience of practice – Local knowledge – National policy • Communication – – Website Reports Presentations Briefings
What do we need to know? • What are the outcomes and why? • What do we expect to happen in future? • What evidence is there that we could achieve better outcomes? • What evidence is there that we could commission more effective and/or cost effective services without getting poorer outcomes? • If we change one part of the system what impact will it have?
High level priorities for West Sussex • Children and families – Child poverty – Education • Working age – Cardiovascular disease – Fair employment • Older people – Independence/Frail elderly – Dementia • Cross cutting issues – – – Inequalities Housing Early intervention Carers Ageing population Mental health
The population
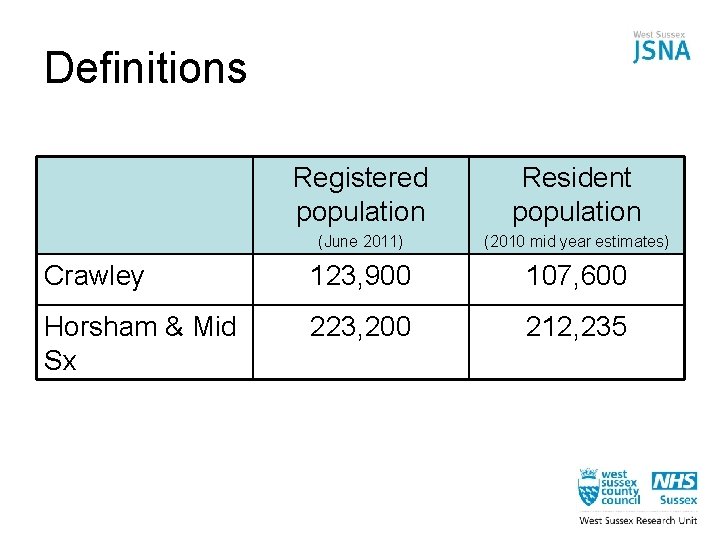
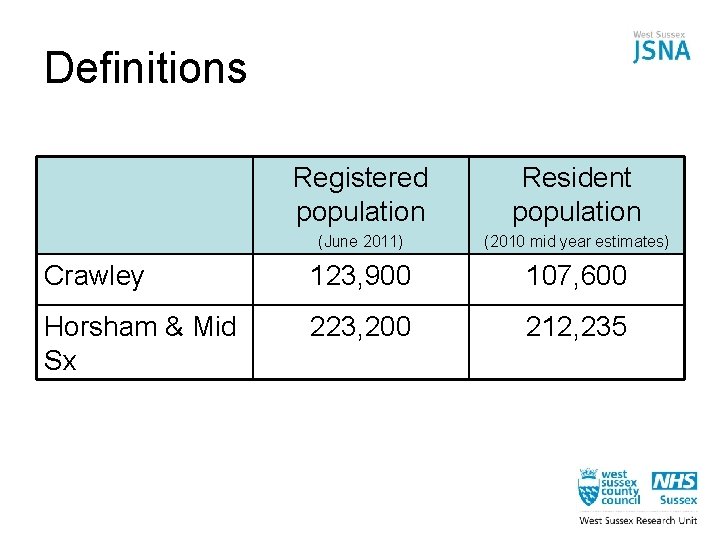
Definitions Registered population Resident population (June 2011) (2010 mid year estimates) Crawley 123, 900 107, 600 Horsham & Mid Sx 223, 200 212, 235
High level health outcomes
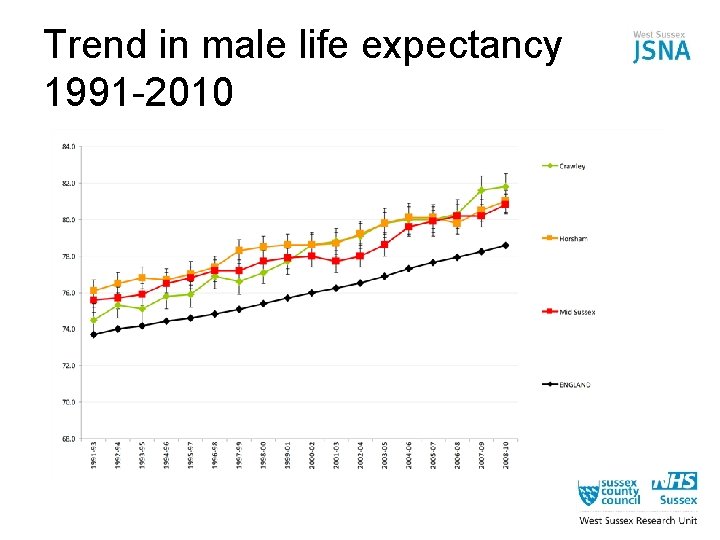
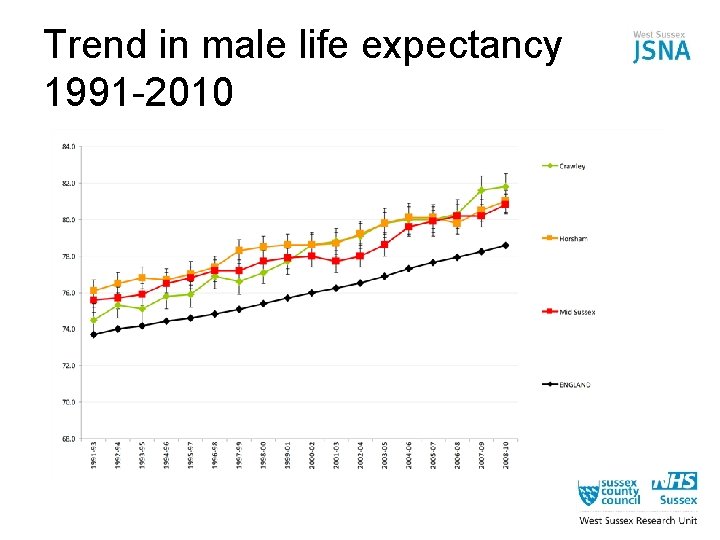
Trend in male life expectancy 1991 -2010
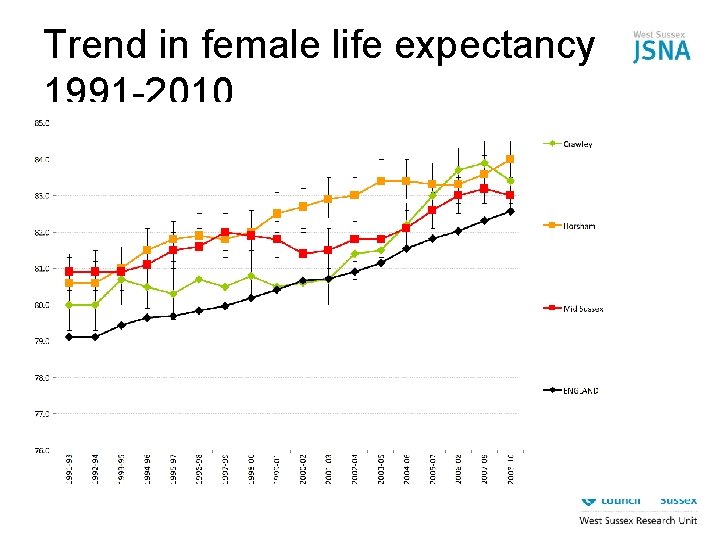
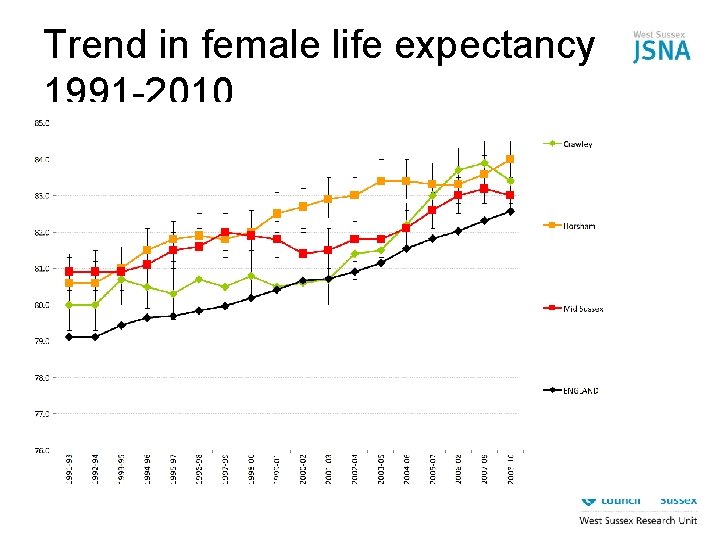
Trend in female life expectancy 1991 -2010
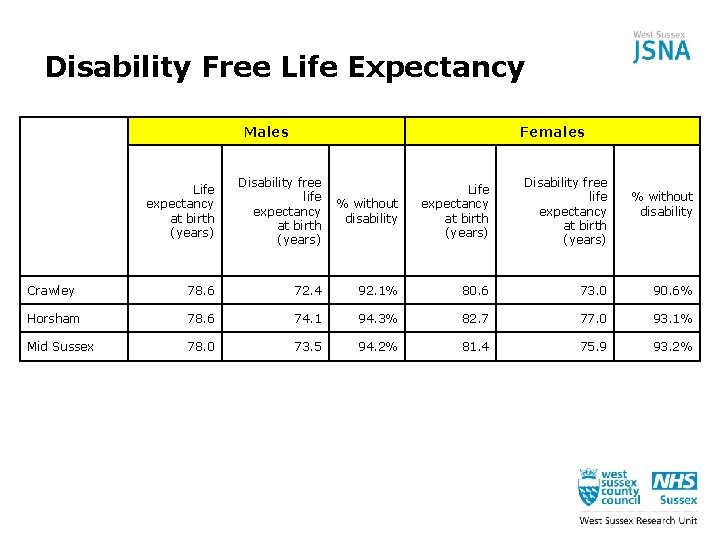
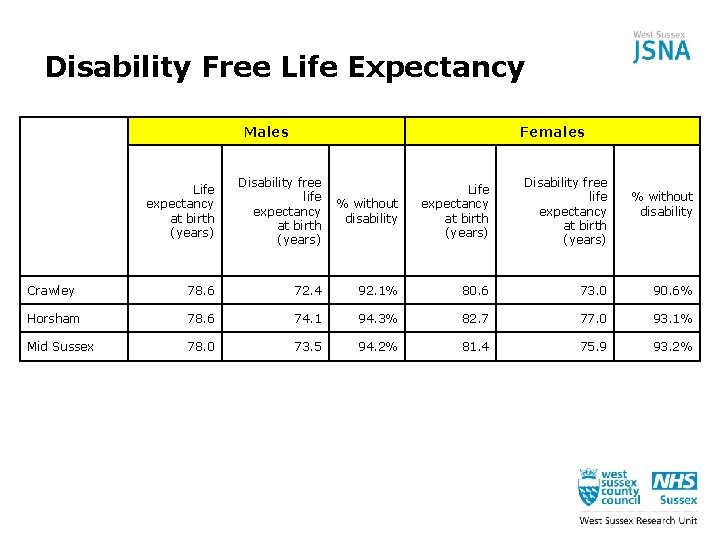
Disability Free Life Expectancy Males Females Life expectancy at birth (years) Disability free life expectancy at birth (years) % without disability Life expectancy at birth (years) Disability free life expectancy at birth (years) Crawley 78. 6 72. 4 92. 1% 80. 6 73. 0 90. 6% Horsham 78. 6 74. 1 94. 3% 82. 7 77. 0 93. 1% Mid Sussex 78. 0 73. 5 94. 2% 81. 4 75. 9 93. 2% % without disability

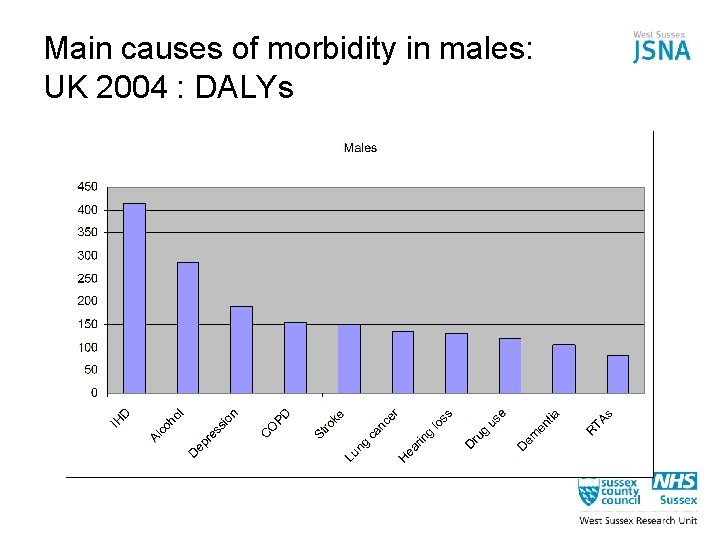
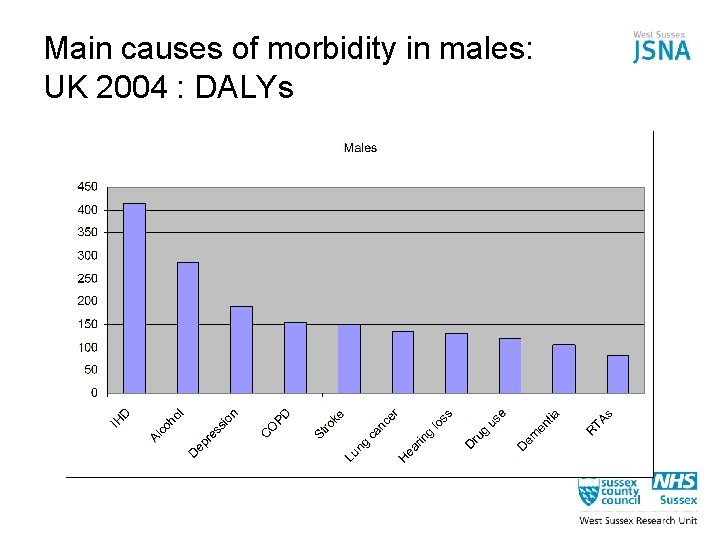
Main causes of morbidity in males: UK 2004 : DALYs
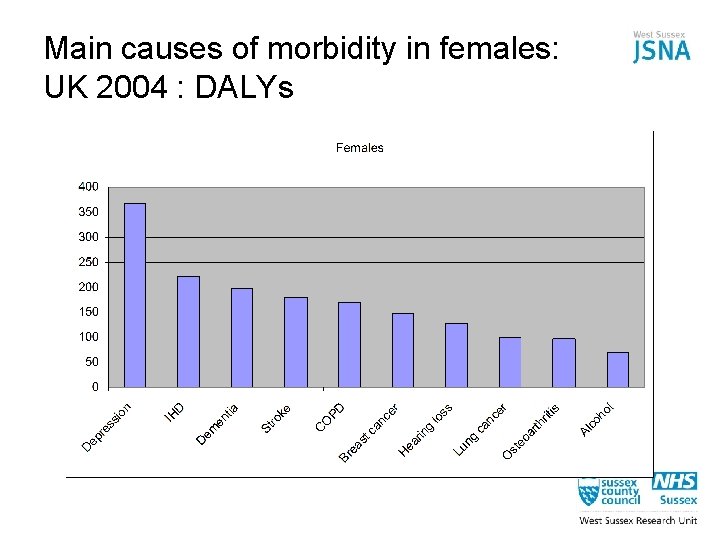
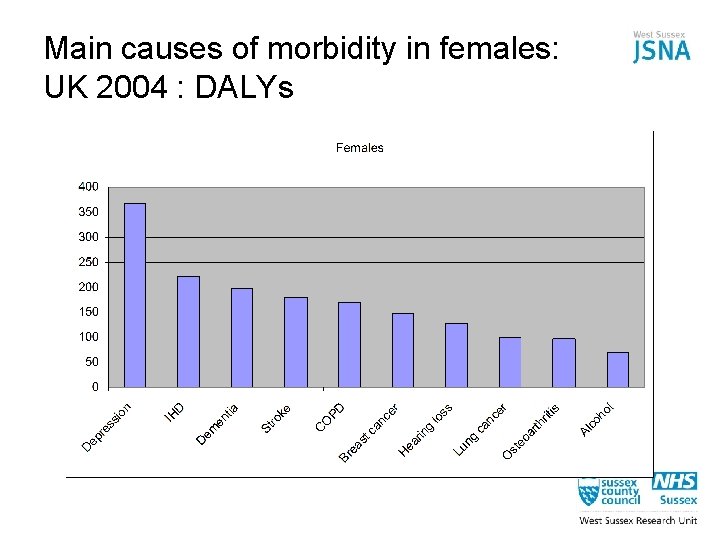
Main causes of morbidity in females: UK 2004 : DALYs
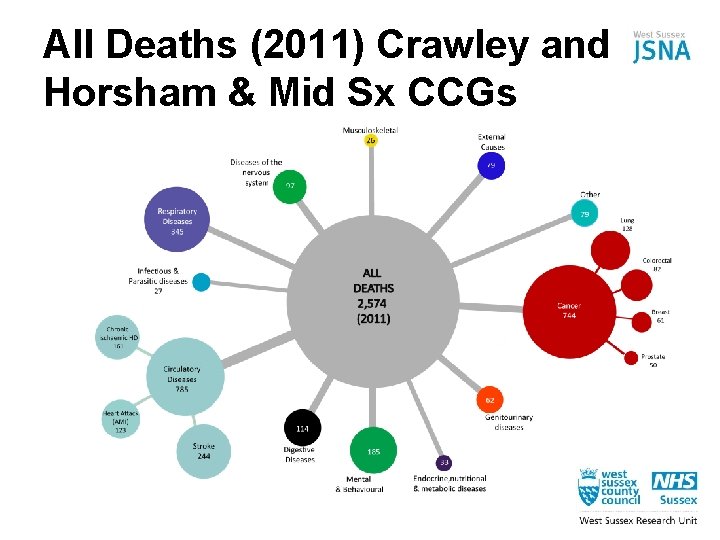
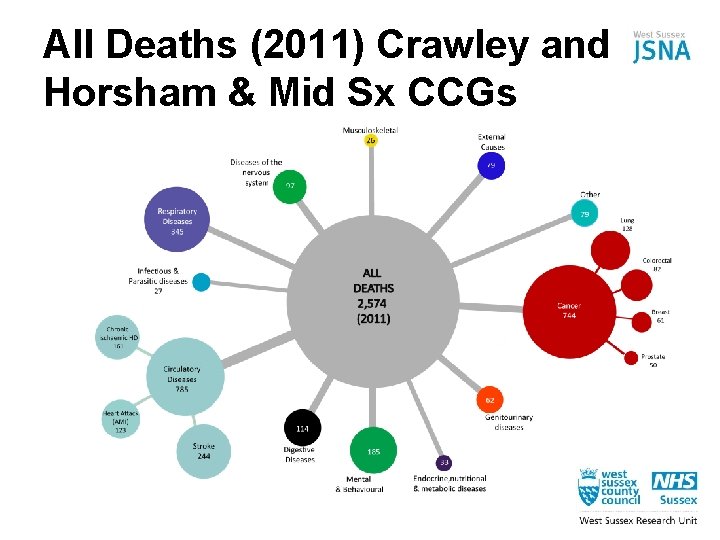
All Deaths (2011) Crawley and Horsham & Mid Sx CCGs
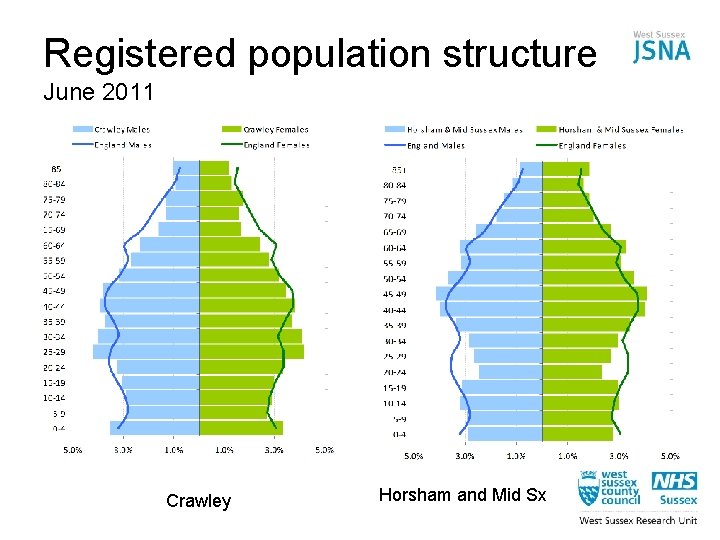
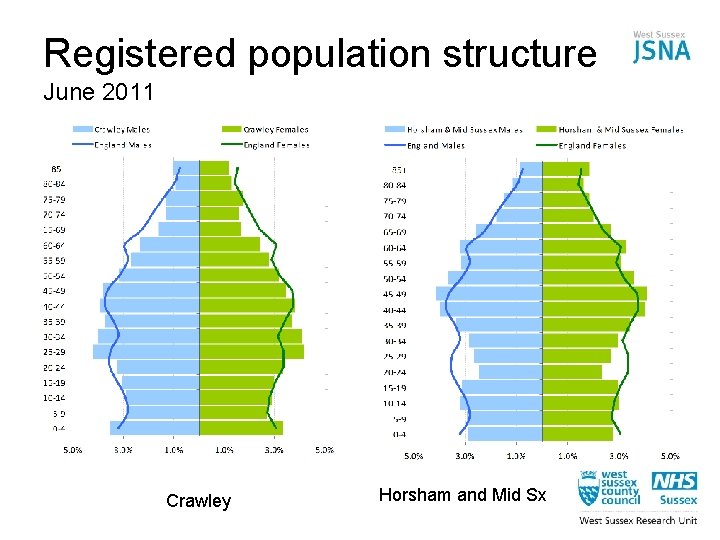
Registered population structure June 2011 Crawley Horsham and Mid Sx
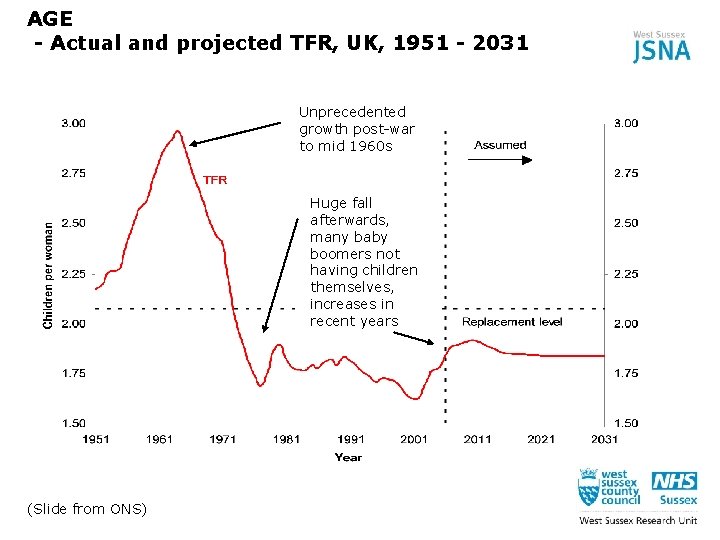
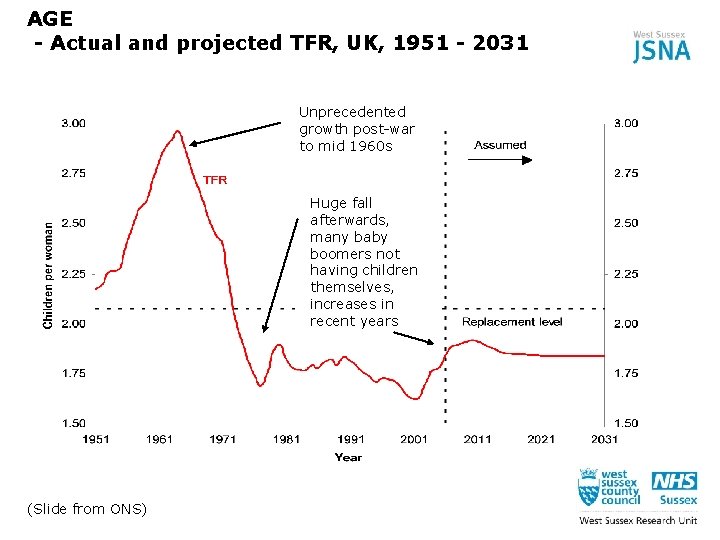
AGE - Actual and projected TFR, UK, 1951 - 2031 Unprecedented growth post-war to mid 1960 s Huge fall afterwards, many baby boomers not having children themselves, increases in recent years (Slide from ONS)
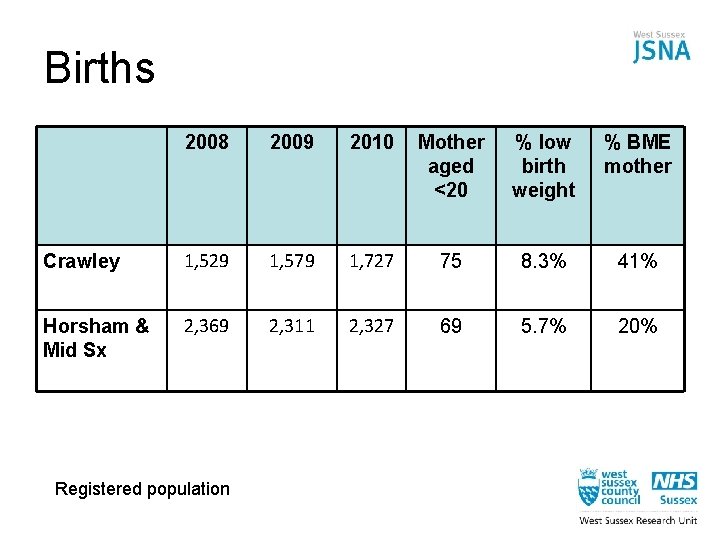
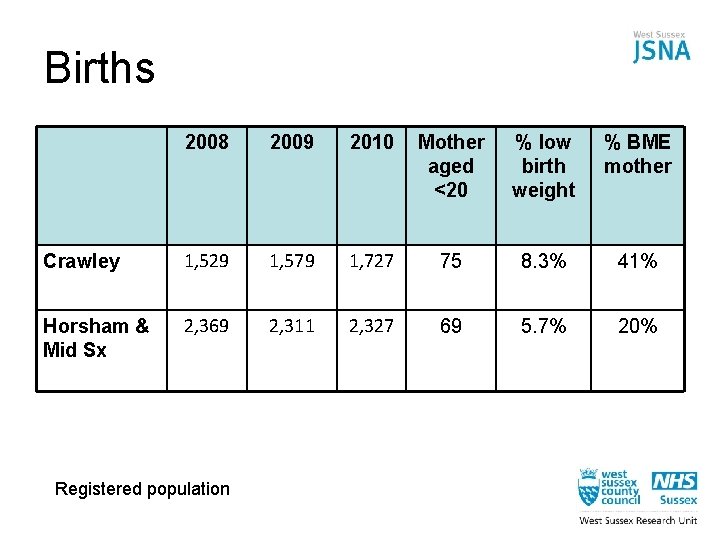
Births 2008 2009 2010 Mother aged <20 % low birth weight % BME mother Crawley 1, 529 1, 579 1, 727 75 8. 3% 41% Horsham & Mid Sx 2, 369 2, 311 2, 327 69 5. 7% 20% Registered population

Behavioural risk factors
‘Most non-communicable diseases are strongly associated and causally linked with four behaviours: tobacco use, unhealthy diet, physical inactivity and the harmful use of tobacco. ’ - WHO 2010
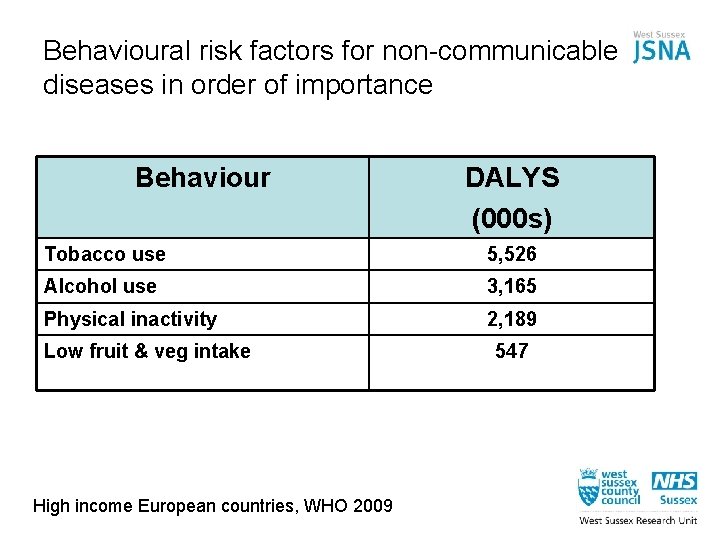
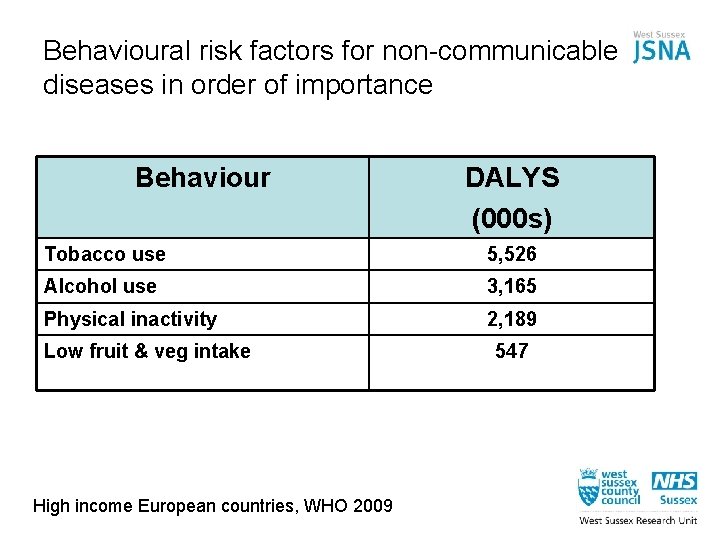
Behavioural risk factors for non-communicable diseases in order of importance Behaviour DALYS (000 s) Tobacco use 5, 526 Alcohol use 3, 165 Physical inactivity 2, 189 Low fruit & veg intake High income European countries, WHO 2009 547
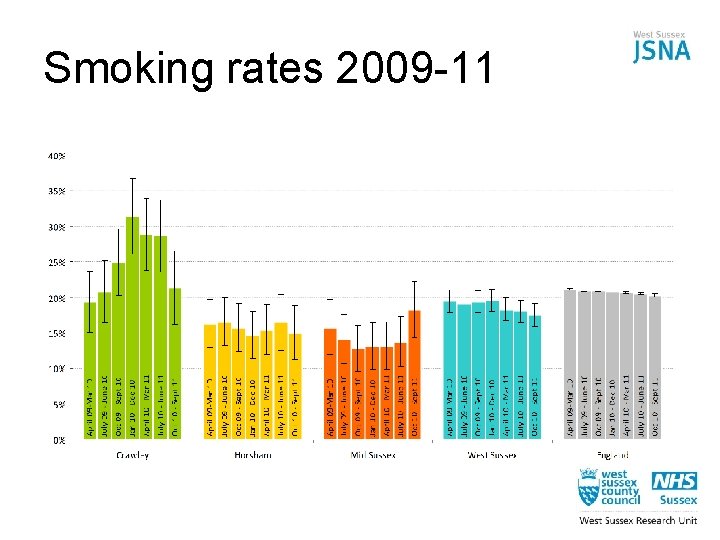
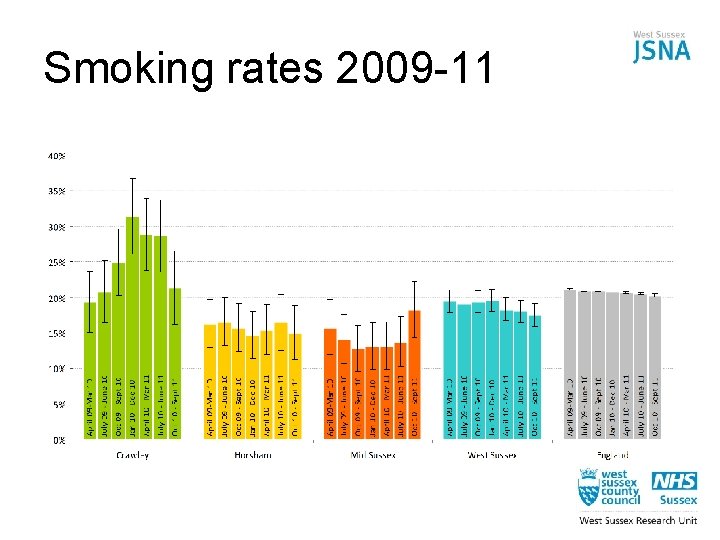
Smoking rates 2009 -11
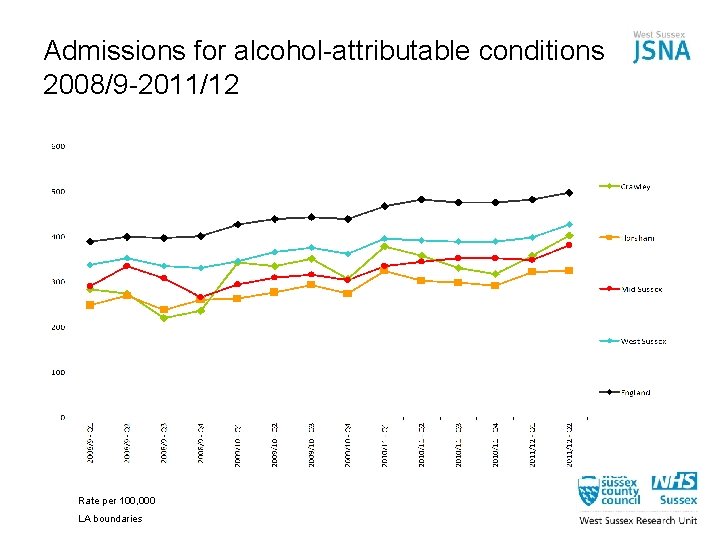
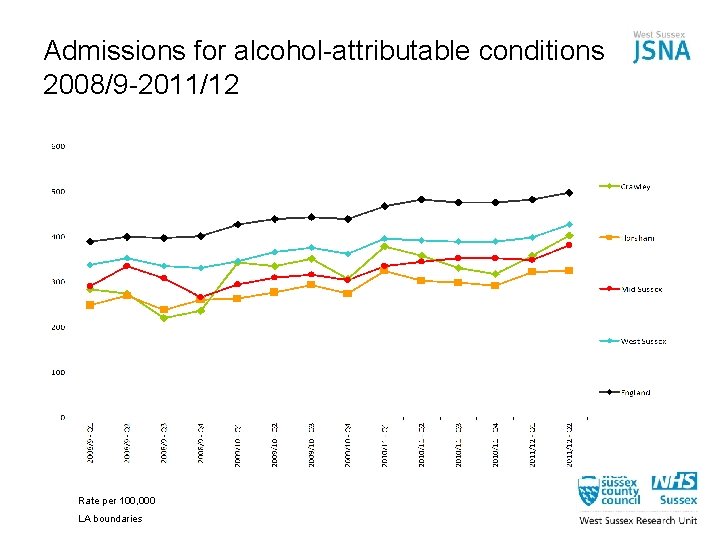
Admissions for alcohol-attributable conditions 2008/9 -2011/12 Rate per 100, 000 LA boundaries
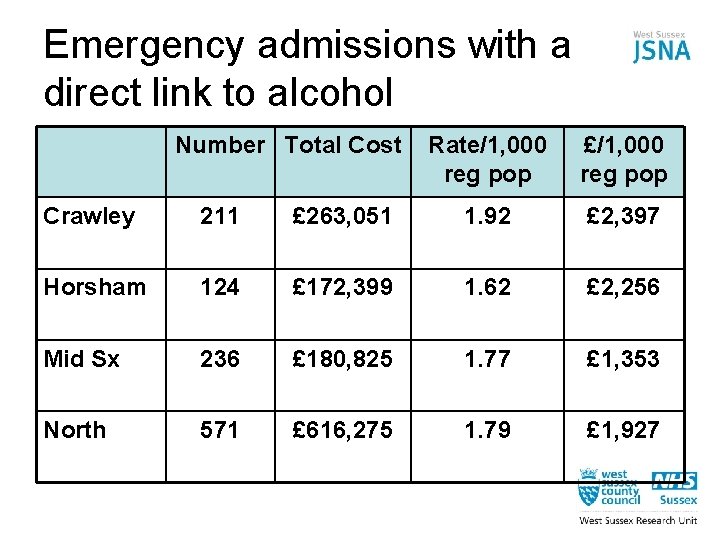
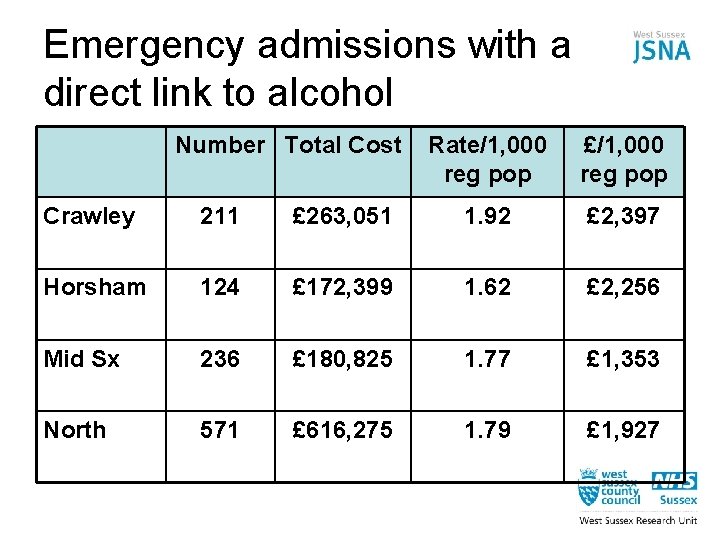
Emergency admissions with a direct link to alcohol Number Total Cost Rate/1, 000 reg pop £/1, 000 reg pop Crawley 211 £ 263, 051 1. 92 £ 2, 397 Horsham 124 £ 172, 399 1. 62 £ 2, 256 Mid Sx 236 £ 180, 825 1. 77 £ 1, 353 North 571 £ 616, 275 1. 79 £ 1, 927
Metabolic/physiological changes
‘These behaviours lead to four metabolic/physiological changes: hypertension, overweight/obesity, hyperglycaemia and hyperlipidaemia. ’ - WHO 2010
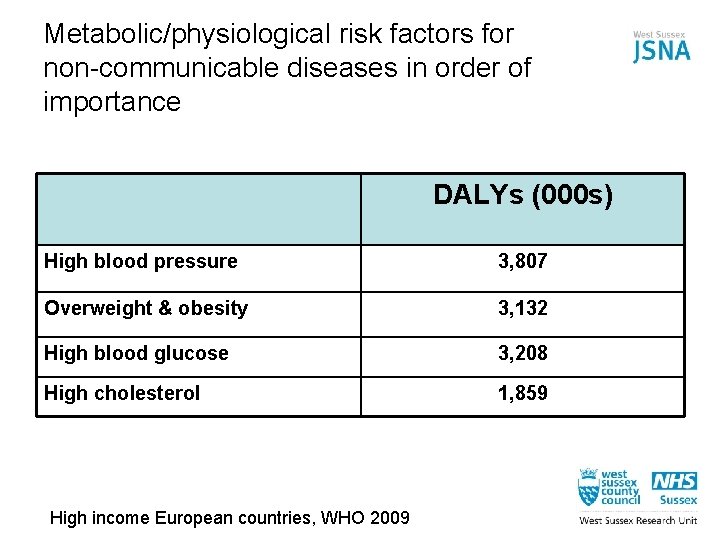
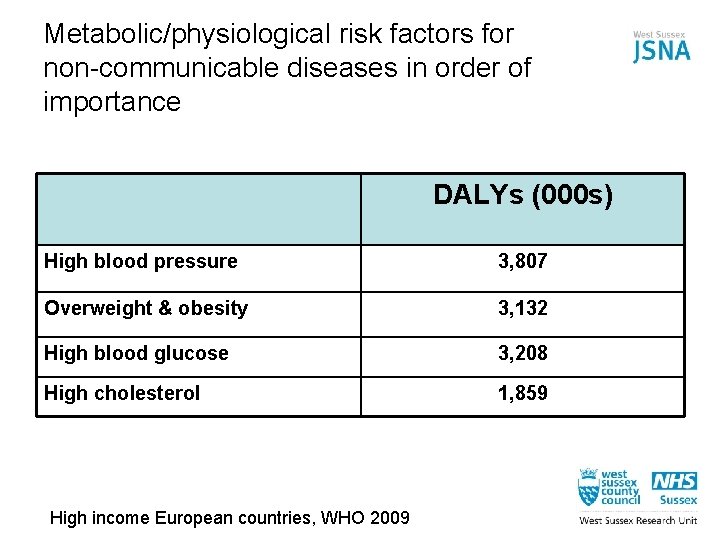
Metabolic/physiological risk factors for non-communicable diseases in order of importance DALYs (000 s) High blood pressure 3, 807 Overweight & obesity 3, 132 High blood glucose 3, 208 High cholesterol 1, 859 High income European countries, WHO 2009
Diabetes: what evidence is there that we can do better?
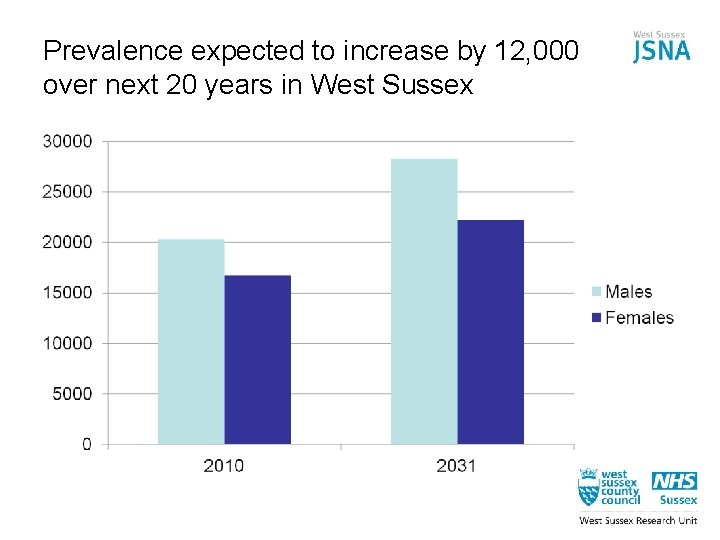
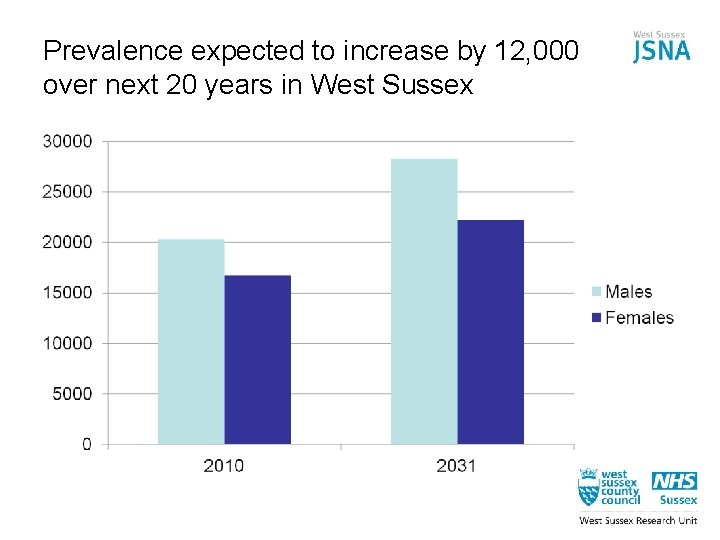
Prevalence expected to increase by 12, 000 over next 20 years in West Sussex
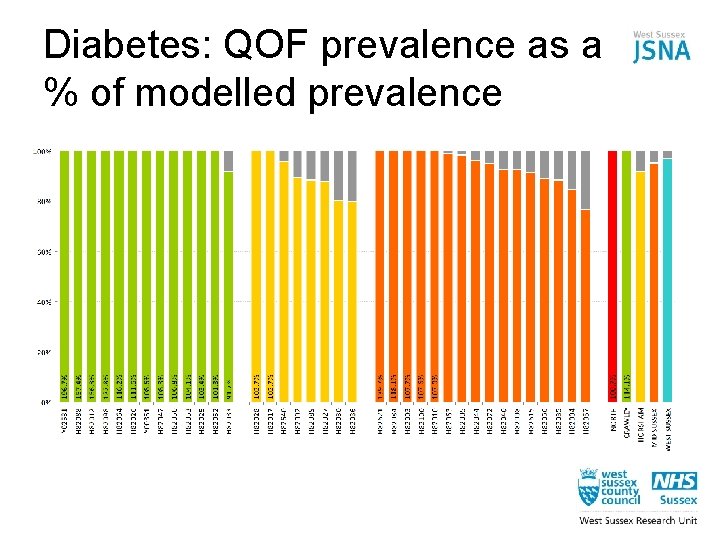
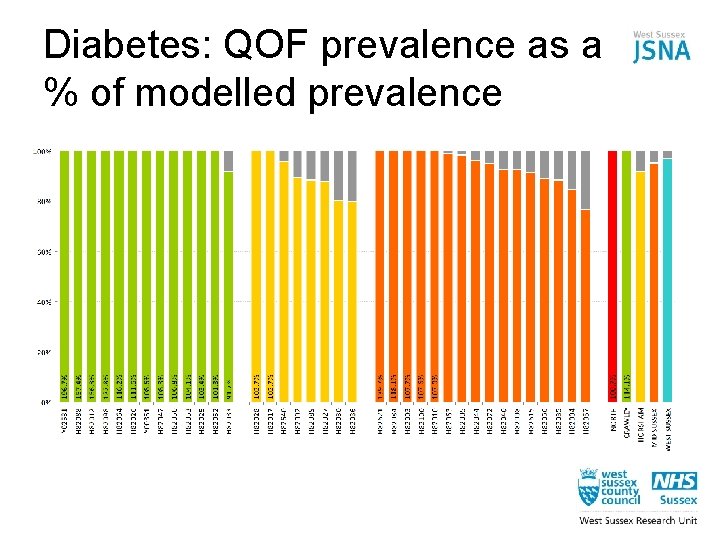
Diabetes: QOF prevalence as a % of modelled prevalence
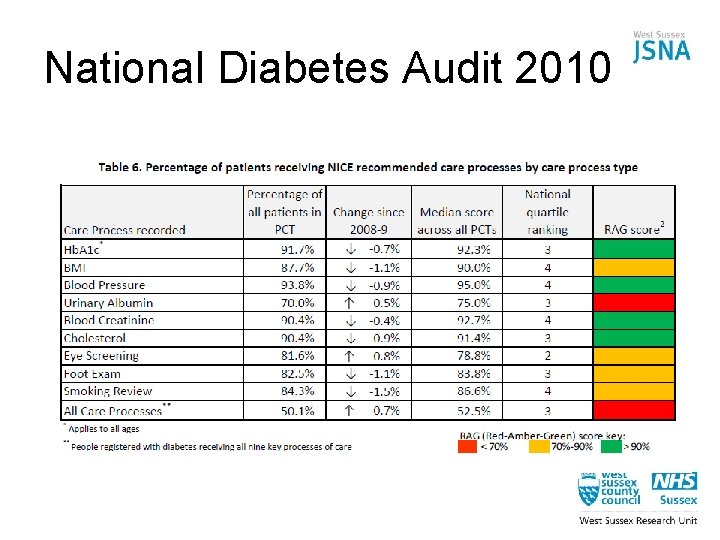
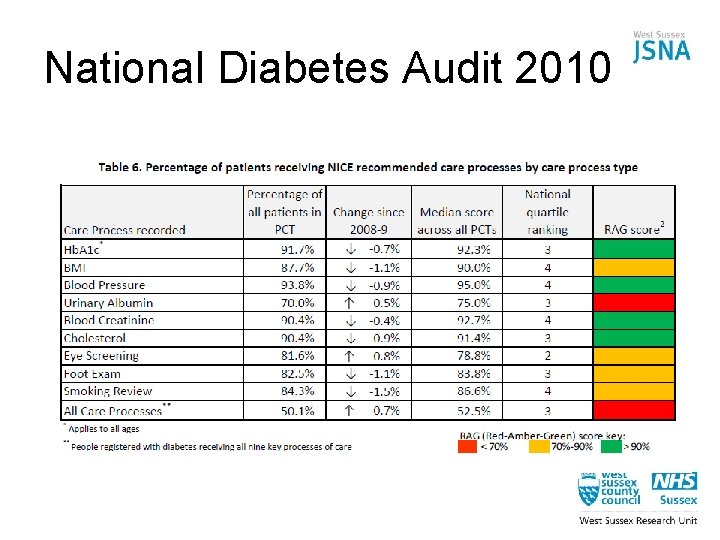
National Diabetes Audit 2010
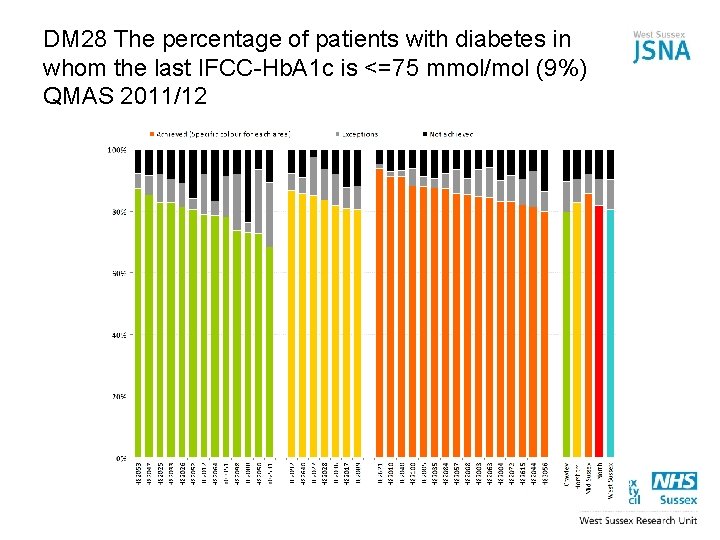
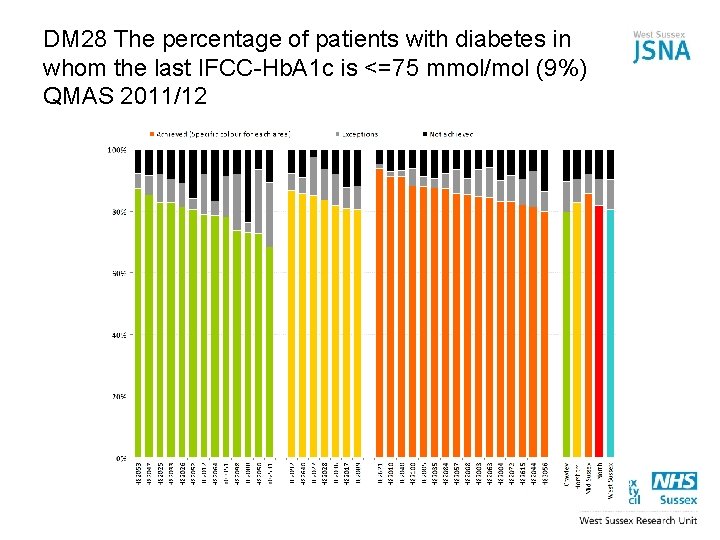
DM 28 The percentage of patients with diabetes in whom the last IFCC-Hb. A 1 c is <=75 mmol/mol (9%) QMAS 2011/12
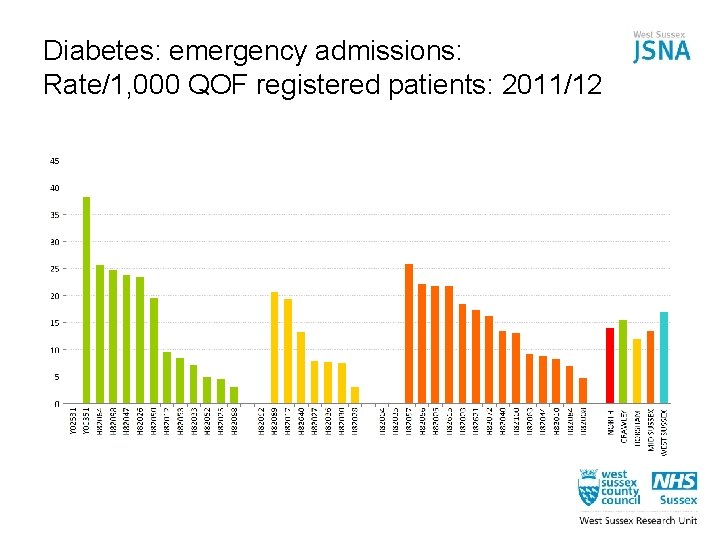
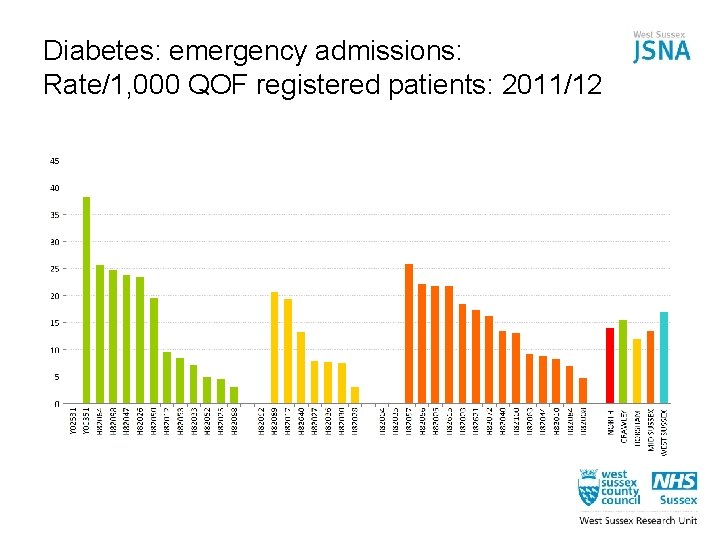
Diabetes: emergency admissions: Rate/1, 000 QOF registered patients: 2011/12
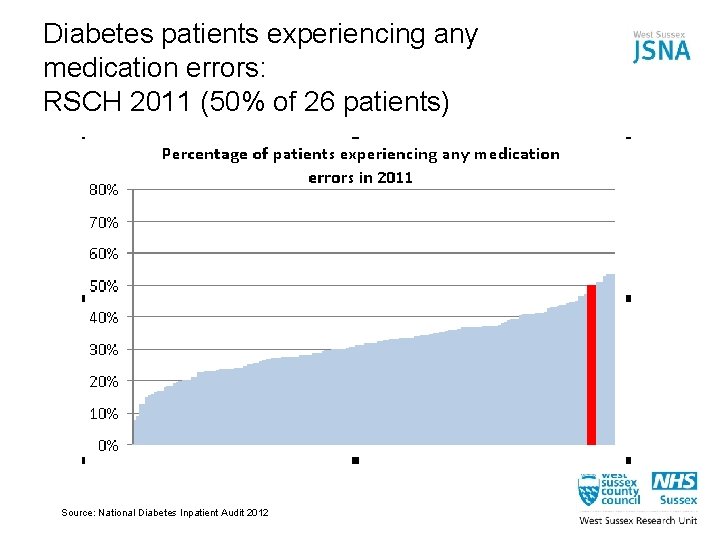
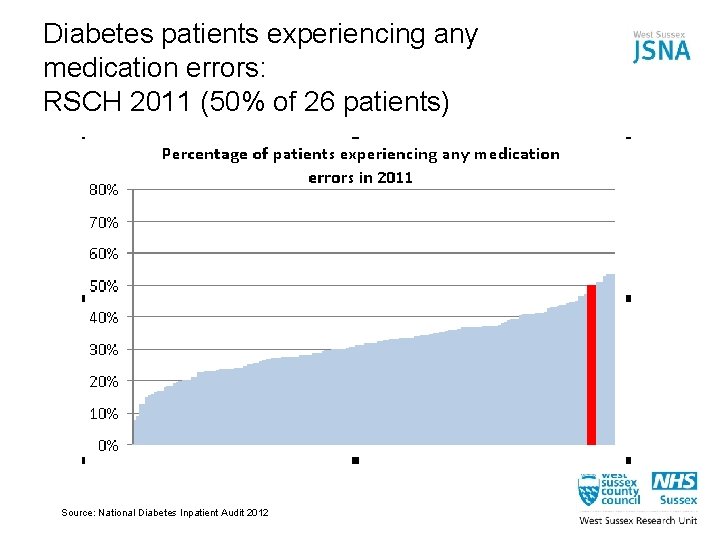
Diabetes patients experiencing any medication errors: RSCH 2011 (50% of 26 patients) Source: National Diabetes Inpatient Audit 2012
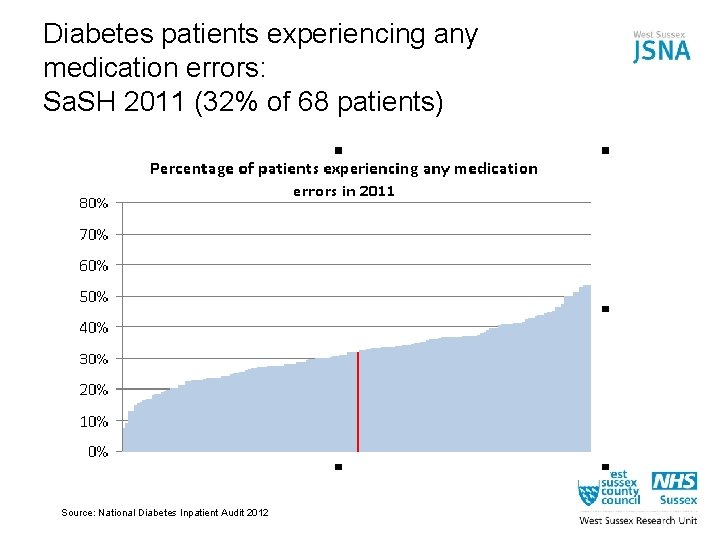
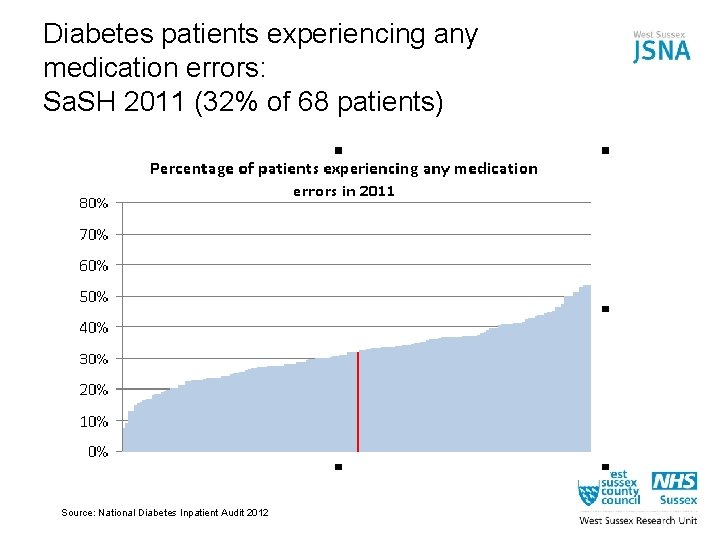
Diabetes patients experiencing any medication errors: Sa. SH 2011 (32% of 68 patients) Source: National Diabetes Inpatient Audit 2012
Evidence-based actions for CCGs on diabetes 1. Set targets to tackle risk factors in primary care to reduce future prevalence (eg brief interventions, referral to weight management services, Health Checks) 2. Local audits of patients receiving all 9 care processes with defined standards 3. Improve hospital care by specifying in contracts that diabetes care should be delivered by appropriately trained professionals 4. Local audits of medication errors in Sa. SH and BSUH 5. Clarify local costs of treating patients with diabetes and consider whether they can be reduced without compromising outcomes 6. Ensure patients receive education and support to manage their condition effectively 7. Systematically seek patient views to ensure services (primary, community and secondary care) are accessible, culturally appropriate and acceptable
Questions to consider • • • • What needs to change, and is it something we control, something we can influence, or something we can do nothing about? What outcome do we want? Is it an important health issue (mortality, morbidity, quality of life)? Will it have a big effect on a few or a small effect on many? Does an adequate treatment/pathway already exist? What’s the level of public/patient support? Will healthcare colleagues and partners support it? What impact will it have on inequalities? How quickly will we see the benefit? Do we know what to do (evidence base) or are we innovating? If we’re innovating how soon will we know whether it’s worked? And what would be the consequences of failure? Is it a national priority? Is it cost saving, cost neutral or cost effective? What’s the opportunity cost?