Ipswich and East Suffolk CCG North East Essex


- Slides: 15
Ipswich and East Suffolk CCG North East Essex CCG West Suffolk CCG Aerosol Generating Procedures (AGPs) and Personal Protective Equipment (PPE) including the fit testing and use of FFP 3 masks Developed by Jane Beckford Infection Prevention and Control Adviser On behalf of Suffolk and North East Essex Infection Prevention and Control Team Guidance correct August 2020 at a time of sustained COVID-19 transmission in the UK
Learning Outcomes 1. To understand the role of Aerosol Generating Procedures (AGPs) in increasing the risk of occupational transmission of COVID-19 2. To be able to undertake an AGP risk assessment 3. To understand the enhanced infection prevention and control (IPC) precautions and personal protective equipment (PPE) that may be indicated 4. To understand how to access fit testing and further guidance and support
Introduction and Rationale The highest risk of transmission of respiratory viruses such as COVID-19 is during AGPs of the respiratory tract - these procedures may cause the virus to become aerosolised and more likely to be inhaled by those delivering care – there may be a shift from droplet to airborne transmission The use of enhanced personal protective equipment (PPE) is indicated for health and social care workers performing or assisting in such procedures This enhanced PPE is recommended during AGPs on possible and confirmed cases of COVID-19 all patients in the context of sustained COVID-19 transmission (this is subject to local risk assessment and advice from Public Health England)
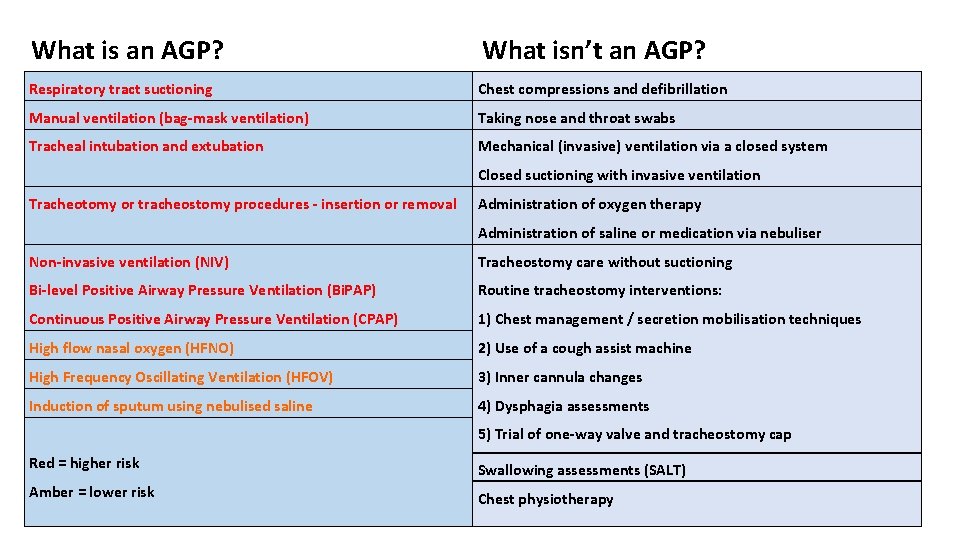
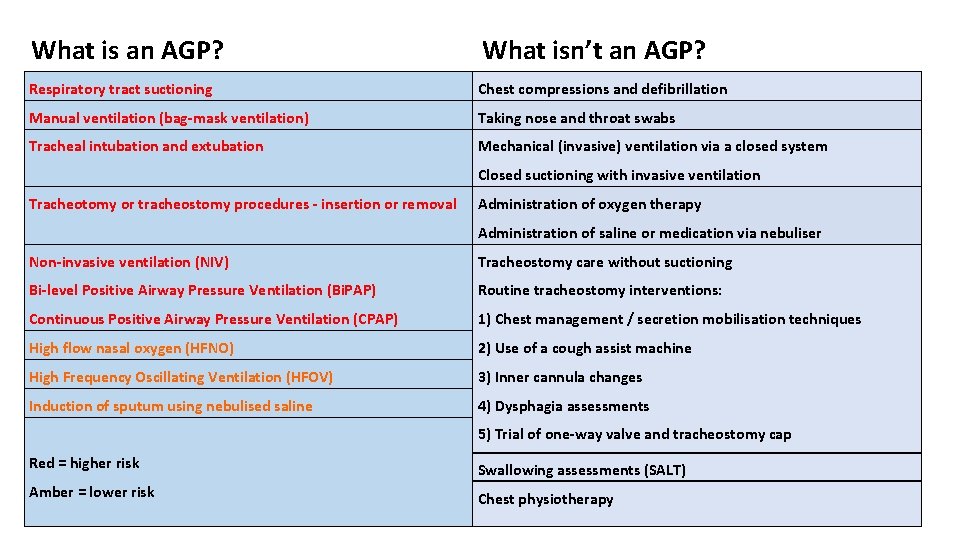
What is an AGP? What isn’t an AGP? Respiratory tract suctioning Chest compressions and defibrillation Manual ventilation (bag-mask ventilation) Taking nose and throat swabs Tracheal intubation and extubation Mechanical (invasive) ventilation via a closed system Closed suctioning with invasive ventilation Tracheotomy or tracheostomy procedures - insertion or removal Administration of oxygen therapy Administration of saline or medication via nebuliser Non-invasive ventilation (NIV) Tracheostomy care without suctioning Bi-level Positive Airway Pressure Ventilation (Bi. PAP) Routine tracheostomy interventions: Continuous Positive Airway Pressure Ventilation (CPAP) 1) Chest management / secretion mobilisation techniques High flow nasal oxygen (HFNO) 2) Use of a cough assist machine High Frequency Oscillating Ventilation (HFOV) 3) Inner cannula changes Induction of sputum using nebulised saline 4) Dysphagia assessments 5) Trial of one-way valve and tracheostomy cap Red = higher risk Swallowing assessments (SALT) Amber = lower risk Chest physiotherapy
Points to Note • The extensive assessment of AGPs was carried out by Health Protection Scotland has been accepted by PHE and NERVTAG – AGPs are defined as medical procedures that generate aerosols and are consistently associated with an increased risk of pathogen transmission • Chest compressions and defibrillation are not considered AGPs and can be carried out without the need for AGP-PPE whilst awaiting the arrival of paramedics to undertake airway manoeuvres - it is strongly advised that there is no delay in delivering this life saving intervention • During nebulisation, the aerosol derives from a non-patient source (fluid in the nebuliser chamber) and does not carry patient-derived viral particles - staff should use hand hygiene when helping patients to remove nebulisers and oxygen masks • There additional surgical, endoscopic, dental, and post-mortem procedures which are defined as AGPs but are not listed here, as they are unlikely to be carried out in community health and social care settings
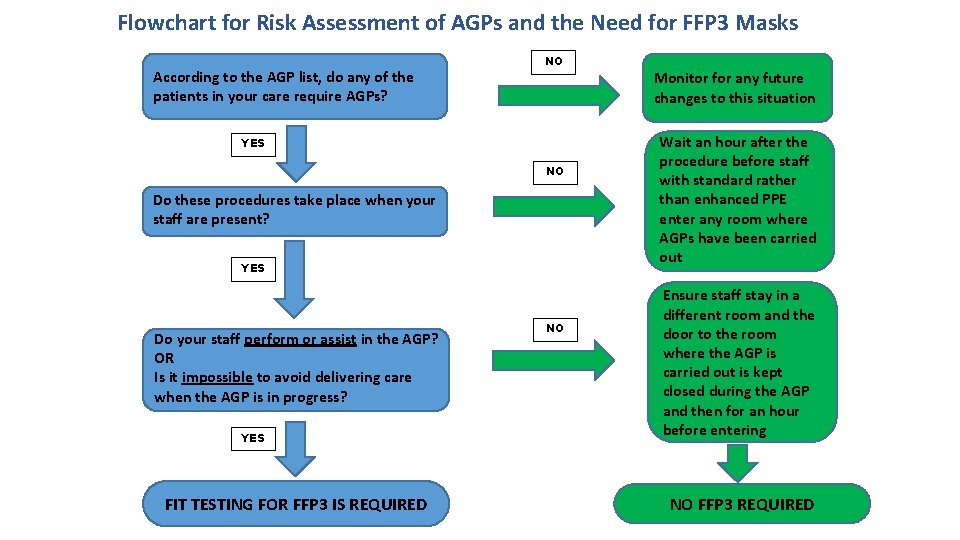
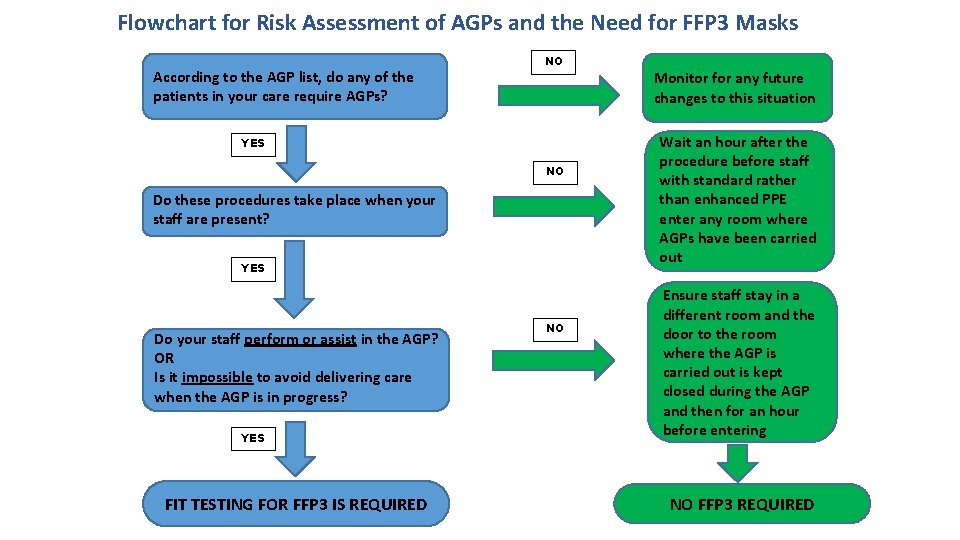
Flowchart for Risk Assessment of AGPs and the Need for FFP 3 Masks According to the AGP list, do any of the patients in your care require AGPs? NO YES NO Do these procedures take place when your staff are present? YES Do your staff perform or assist in the AGP? OR Is it impossible to avoid delivering care when the AGP is in progress? YES FIT TESTING FOR FFP 3 IS REQUIRED NO Monitor for any future changes to this situation Wait an hour after the procedure before staff with standard rather than enhanced PPE enter any room where AGPs have been carried out Ensure staff stay in a different room and the door to the room where the AGP is carried out is kept closed during the AGP and then for an hour before entering NO FFP 3 REQUIRED
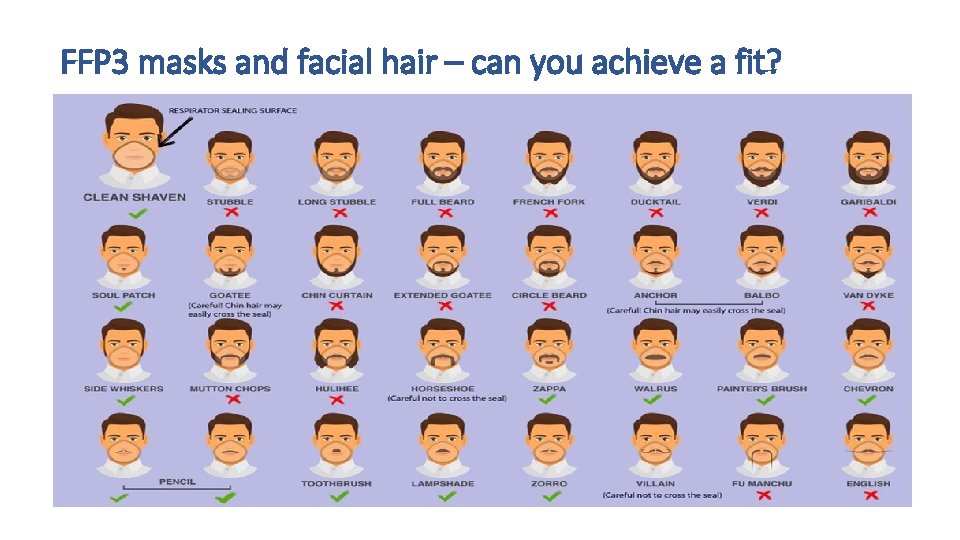
If fit testing is required, what does the manager need to do next? Select the staff to be fit tested – choose a core team of regular (not agency) staff, exclude any who cannot wear FFP 3 masks for medical reasons or any who may not achieve a good fit due to facial hair – see next slide Contact one of the fit testing companies (see slide after next) and arrange a fit testing session Once fit testing is completed - with full reports from the company, compile a register of the staff who have been fit tested and the make, model and size of mask for which each achieved a fit – this mask must then be supplied for them Maintain and update the register when there are staff changes - arrange fit testing for new staff Provide each employee with details of the mask they should be using
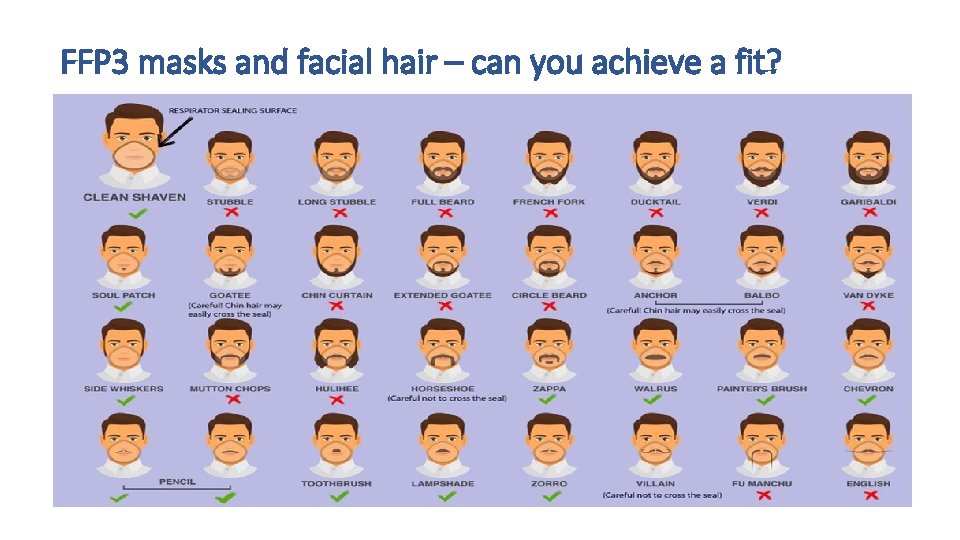
FFP 3 masks and facial hair – can you achieve a fit?

Fit Testing Companies Commissioned by Suffolk CCGs Wherever possible please bring together a group of individuals for fit testing or arrange for more than one provider in a locality to be scheduled for the same morning or afternoon You will need to provide the masks for which you wish staff to be fit tested The invoice will be presented to the CCG for validation so please complete the registration provided by the tester If individuals do not turn up to a booked test, then your organisation may be liable for the cost of the missed test - the CCG will be funding this service on your behalf and will receive detailed invoices Safescope Dr Khalid Bhutto – csr@safescope. com – 01473 407020 C&C Training Ltd Andrew Bishton – andrew@cctraining. uk. com – 01525 851752 Gipping Occupational Health (fit testing only, no training) Amanda Heavens – adminteam@gipping. co. uk – 01449 766913
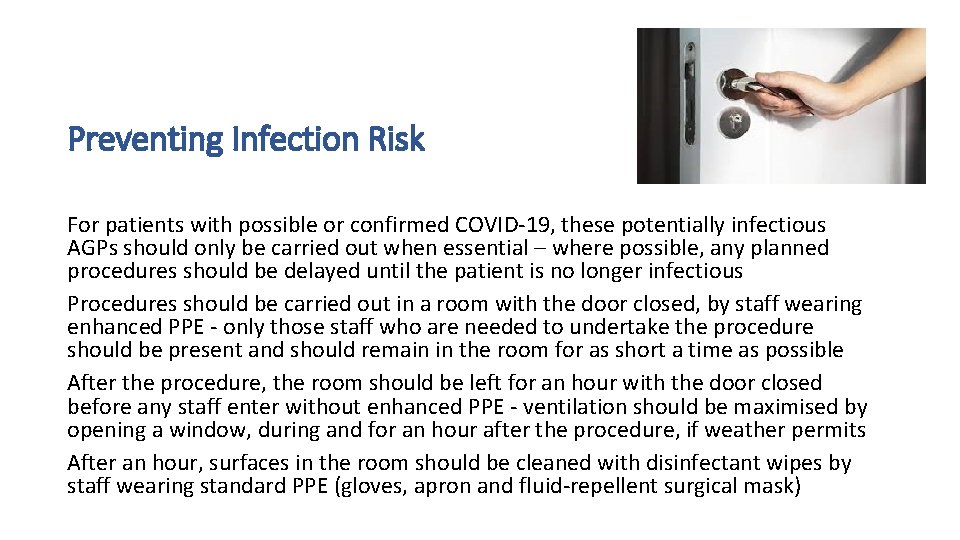
Preventing Infection Risk For patients with possible or confirmed COVID-19, these potentially infectious AGPs should only be carried out when essential – where possible, any planned procedures should be delayed until the patient is no longer infectious Procedures should be carried out in a room with the door closed, by staff wearing enhanced PPE - only those staff who are needed to undertake the procedure should be present and should remain in the room for as short a time as possible After the procedure, the room should be left for an hour with the door closed before any staff enter without enhanced PPE - ventilation should be maximised by opening a window, during and for an hour after the procedure, if weather permits After an hour, surfaces in the room should be cleaned with disinfectant wipes by staff wearing standard PPE (gloves, apron and fluid-repellent surgical mask)
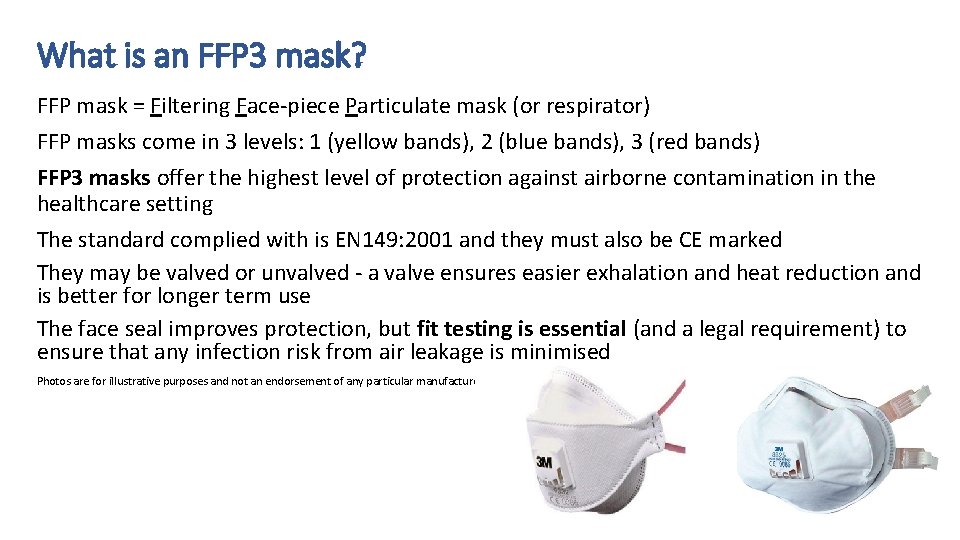
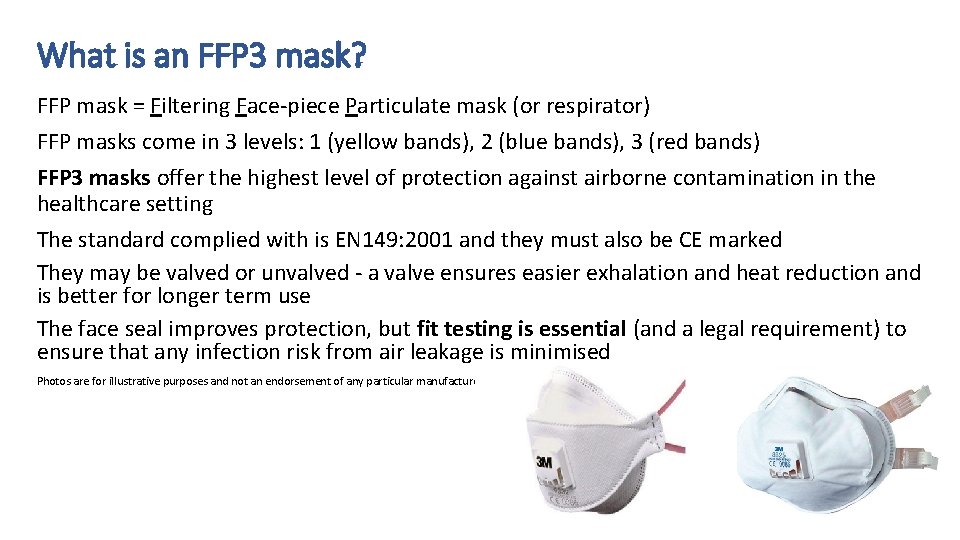
What is an FFP 3 mask? FFP mask = Filtering Face-piece Particulate mask (or respirator) FFP masks come in 3 levels: 1 (yellow bands), 2 (blue bands), 3 (red bands) FFP 3 masks offer the highest level of protection against airborne contamination in the healthcare setting The standard complied with is EN 149: 2001 and they must also be CE marked They may be valved or unvalved - a valve ensures easier exhalation and heat reduction and is better for longer term use The face seal improves protection, but fit testing is essential (and a legal requirement) to ensure that any infection risk from air leakage is minimised Photos are for illustrative purposes and not an endorsement of any particular manufacturer
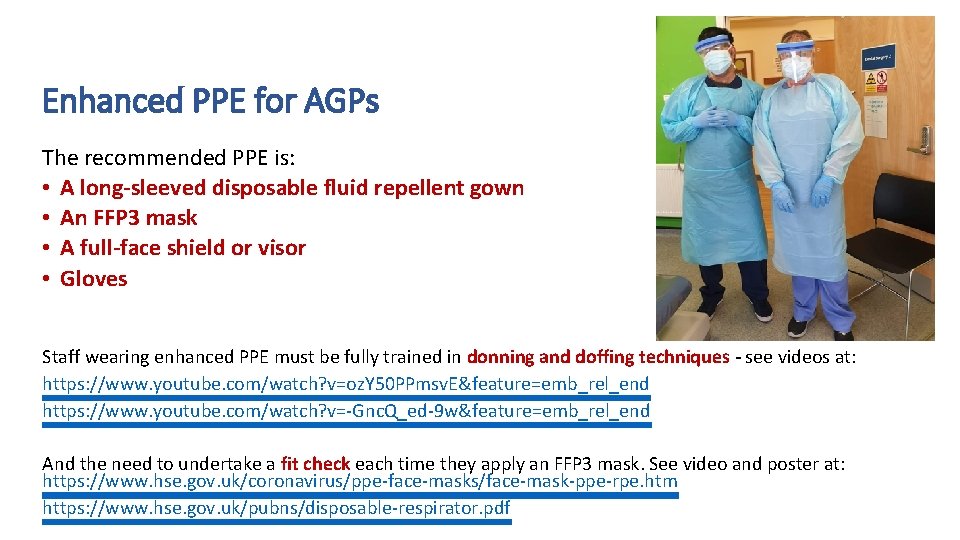
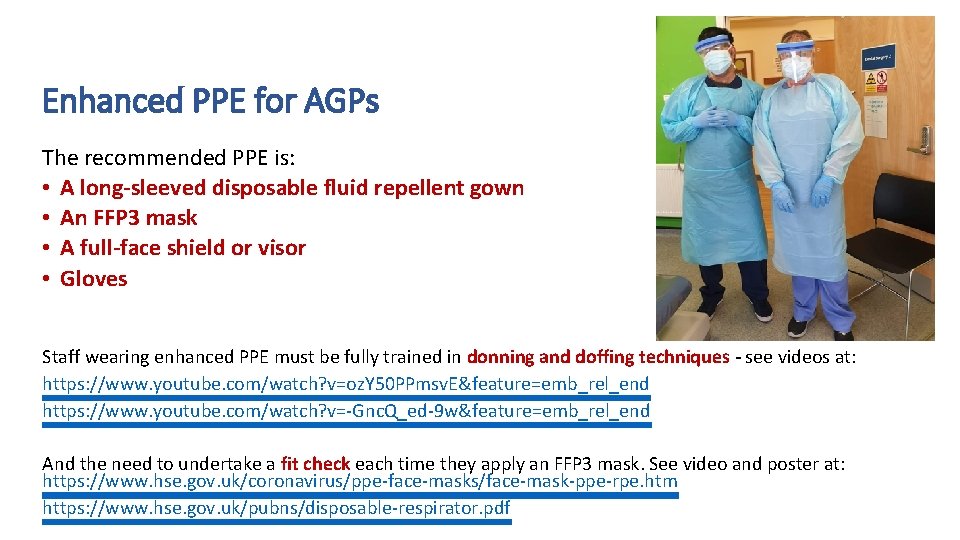
Enhanced PPE for AGPs The recommended PPE is: • A long-sleeved disposable fluid repellent gown • An FFP 3 mask • A full-face shield or visor • Gloves Staff wearing enhanced PPE must be fully trained in donning and doffing techniques - see videos at: https: //www. youtube. com/watch? v=oz. Y 50 PPmsv. E&feature=emb_rel_end https: //www. youtube. com/watch? v=-Gnc. Q_ed-9 w&feature=emb_rel_end And the need to undertake a fit check each time they apply an FFP 3 mask. See video and poster at: https: //www. hse. gov. uk/coronavirus/ppe-face-masks/face-mask-ppe-rpe. htm https: //www. hse. gov. uk/pubns/disposable-respirator. pdf
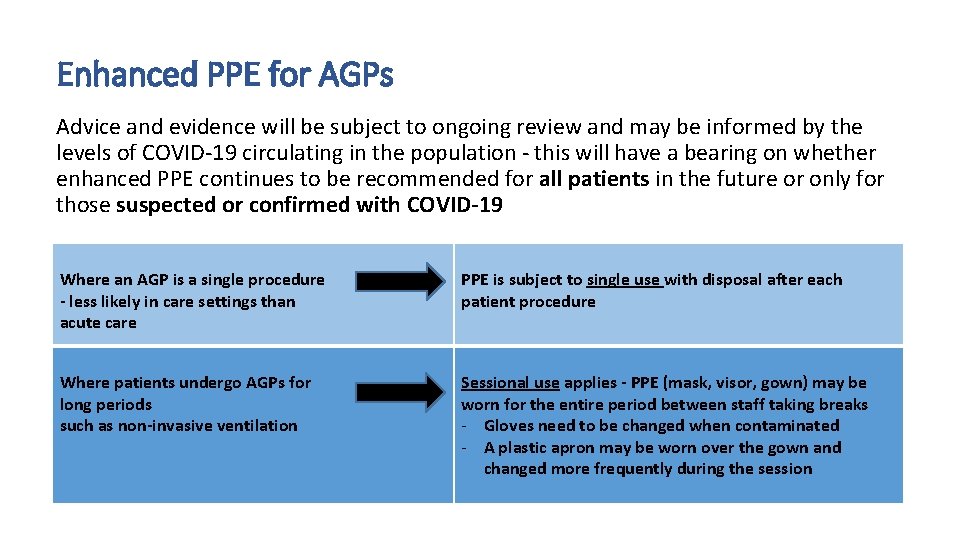
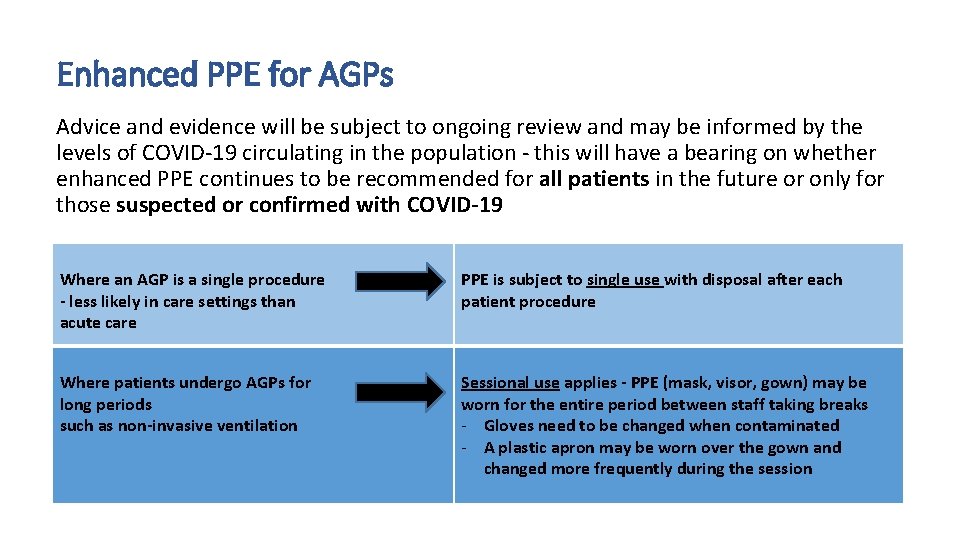
Enhanced PPE for AGPs Advice and evidence will be subject to ongoing review and may be informed by the levels of COVID-19 circulating in the population - this will have a bearing on whether enhanced PPE continues to be recommended for all patients in the future or only for those suspected or confirmed with COVID-19 Where an AGP is a single procedure - less likely in care settings than acute care PPE is subject to single use with disposal after each patient procedure Where patients undergo AGPs for long periods such as non-invasive ventilation Sessional use applies - PPE (mask, visor, gown) may be worn for the entire period between staff taking breaks - Gloves need to be changed when contaminated - A plastic apron may be worn over the gown and changed more frequently during the session

Sources of Further Advice Public Health England Website https: //www. gov. uk/government/publications/covid-19 -personal-protective-equipment-use-for-aerosol-generatingprocedures Suffolk County Council Website https: //www. suffolk. gov. uk/coronavirus-covid-19/latest-information/ Suffolk County Council Support ACSContracts. Helpdesk@suffolk. gov. uk Infection Prevention and Control Support Covid-19@Suffolk. gov. uk 01473 296400
References Public Health England. (2020). COVID-19 Personal Protective Equipment (PPE), Section 8. 1: Aerosol Generating Procedures, at: https: //www. gov. uk/government/publications/wuhan-novel-coronavirus-infection-prevention-andcontrol/covid-19 -personal-protective-equipment-ppe Lancashire and South Cumbria Regional Tracheostomy Team. (2020). Covid-19: Acute Tracheostomy Management, April 6, V 1, at: https: //www. acprc. org. uk/Data/Resource_Downloads/Covid 19 Acutetracheostomyadmissionguidenceversion 2. pdf? date=10/05/2020%2000: 33: 35 British Thoracic Society. (2020). Guidance for community management of patients receiving long-term ventilation (LTV) during and beyond COVID-19, June 26, V 2. 1 Health Protection Scotland. (2020). Assessing the evidence base for medical procedures which create a higher risk of respiratory infection transmission from patient to healthcare worker, May 12, at: https: //hps. scot. nhs. uk/web-resources-container/sbar-assessing-the-evidence-base-for-medicalprocedures-which-create-a-higher-risk-of-respiratory-infection-transmission-from-patient-tohealthcare-worker/
 Nhs north east hampshire and farnham ccg
Nhs north east hampshire and farnham ccg Nottingham north and east ccg
Nottingham north and east ccg Ics north east
Ics north east Southwold council
Southwold council North west surrey ccg
North west surrey ccg Dr nicola burbidge
Dr nicola burbidge Esccg
Esccg Jim lindsay ipswich city council
Jim lindsay ipswich city council Endeavour house ipswich
Endeavour house ipswich Lines that run from north to south but measure is and west
Lines that run from north to south but measure is and west Chapter 14 lesson 4 people of the south
Chapter 14 lesson 4 people of the south West suffolk alliance
West suffolk alliance Ann coyne suffolk university
Ann coyne suffolk university Ovelhas suffolk
Ovelhas suffolk Ambulette service long island
Ambulette service long island It outsourcing suffolk
It outsourcing suffolk