Immunotherapy Cancer therapy with TCells Sania Munir 12

- Slides: 17
Immunotherapy (Cancer therapy with T-Cells) Sania Munir 12 -10235 BIOT- 412
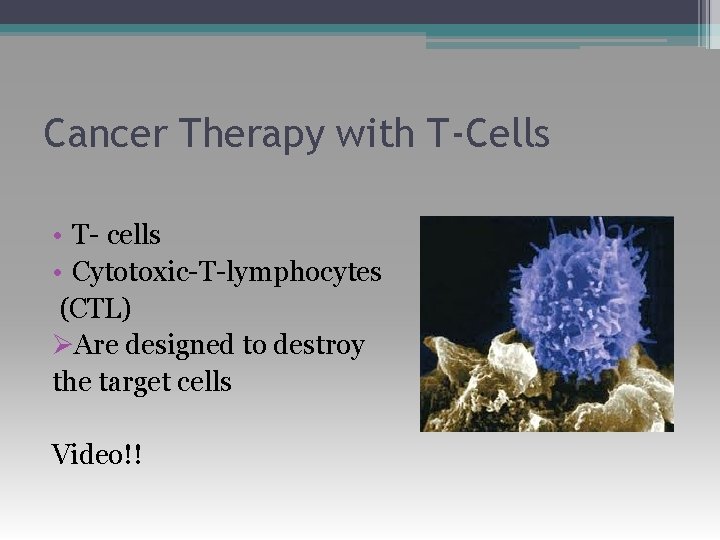
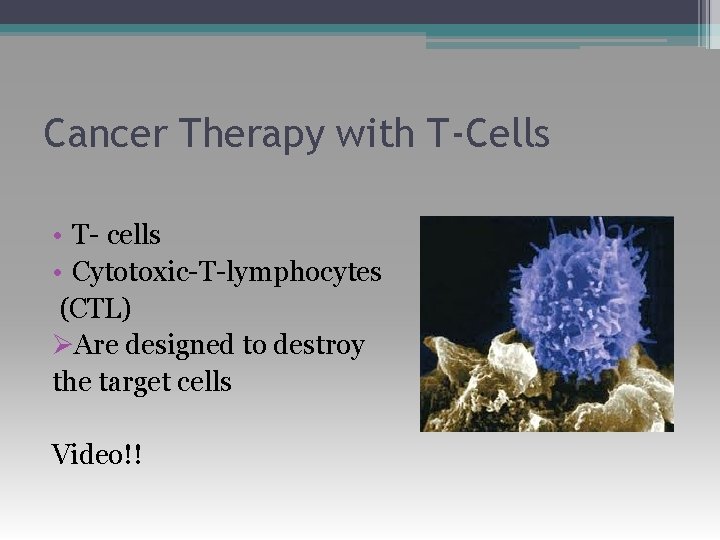
Cancer Therapy with T-Cells • T- cells • Cytotoxic-T-lymphocytes (CTL) ØAre designed to destroy the target cells Video!!
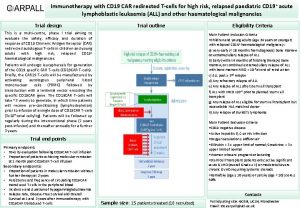
Using a Bispecific Monoclonal Antibody • Blinatumomab is a synthetic monoclonal antibody, carries binding sites. • One arm binds to CD 19 (B-Cells lymphomas) • Other arm binds to CD 3, a cell surface molecule on T cells (CTLs) • Form a bridge b/w CD 3 and CD 19, attaches Tcells to B-cells and activate T-cells to kill B-cells.
Allografts of T-Cells • After total destruction of the pateint’s own white blood cells (myeloablative conditioning) • To cure leukemia (and some other cancers)→high doses of chemotherapy and radiation →patient's bone marrow is destroyed. • If the patient is to survive the treatment, he or she must be given a transplant of hematopoietic stem cells.
The stem cells can be • an autograft; that is, from bone marrow harvested from the patient and stored before treatment begins. • an allograft; that is, cells harvested from another person, usually a family member sharing the same major histocompatibility molecules.
• Allografted hematopoietic stem cells also sometimes fail to cure. But…. ? ? ? • graft-versus-leukemia effect. • Most of the donor T cells are probably attacking normal cell surface molecules, not tumorspecific ones. • The patient may also suffer from graft-versushost disease (GVHD).
After Non-myeloablative Conditioning • The patient is treated to kill some bone marrow cells. • Instead of using high doses of radiation to the entire body and chemotherapy, only the lymphoid organs are irradiated. • Antithymocyte globulin can also be given. • Even though this leaves some cancer cells, it makes it possible for allogeneic bone marrow stem cells to take up long-term residence in the recipient.
• This is followed by an infusion of T cells from the same donor. • Once again they will also attack normal cells of the recipient usually causing graft-versus-host disease (GVHD). But this it would be milder than that following myeloablative conditioning — perhaps because repeated small doses of radiation favors the survival of natural killer (NK) cells, and these appear to protect against GVHD.
Autografts of T cells: Tumor. Infiltrating Lymphocytes (TIL) The procedure: ØIsolate T cells — both CD 4+and CD 8+ from samples of the tumor (melanoma) ØIn-vitro testing Ø Grow large numbers of them in culture (using the powerful T-cell growth factor IL-2) ØTreat the patient with modest doses of cytotoxic drugs to reduce — but not destroy — the bone marrow ØReintroduce the mix of Th cells (CD 4+) and CTL (CD 8+) into the patient (along with IL-2).

The results: • The infused cells usually took up long-term residence. • In 10 of 13 patients, their melanoma cells — including all metastases — regressed either partially or completely. • In a few cases, the TIL seemed to be reacting to tumor-specific antigens, but in most the target seems to have been antigens expressed by all melanin-containing cells. Evidence: • Four patients lost normal melanocytes from their skin leaving white patches. • One patient developed inflammation of the uvea. Video!!
Gene Therapy: Autografts of genetically-modified T cells • On April 20, 2006, the Rosenberg group reported some success with melanoma patients using a modification of the TIL procedure. • The patient's T cells were removed and treated with a retroviral vector containing the αβ TCR specific for a melanoma antigen. • Large numbers of these were grown in culture. • After partial myeloablative conditioning, the genetically-modified lymphocytes were infused into the patient.
Cont. • This application of gene therapy succeeded in eliminating the metastases and providing a disease-free period of two years in two patients. • Video!!
Autografts of a clone of tumorantigen-specific T cells • The 19 June 2008 issue of the New England Journal of Medicine (Naomi Hunder et al) carried a report describing the successful treatment of a man with metastasized melanoma using his own T cells. The procedure: • His leukocytes were harvested and a mixed culture was prepared containing ▫ antigen-presenting dendritic cells. ▫ a peptide from the antigen NY-ESO-1. ▫ The patient's own T cells. • After repeated stimulation with the antigen, responding cells were cloned by limiting dilution.
• One (of four) antigen-reactive cells was then expanded in culture until 5 billion (5 x 109) identical anti-NY-ESO-1 CD 4+ T cells were available to infuse into the patient. The result: • Complete regression of each metastatic clump of melanoma cells, and the patient has remained free of this lethal cancer for two years since this treatment.
“One swallow does not make a summer”, but this result give hope that in time immunotherapy will become an effective weapon against cancer.
Thank you!!
 What are the 5 stages of rostow's model
What are the 5 stages of rostow's model Ukons immunotherapy guidelines
Ukons immunotherapy guidelines Initinib
Initinib Immunotherapy
Immunotherapy Matematika diskrit rinaldi munir revisi 6
Matematika diskrit rinaldi munir revisi 6 Anggur emir
Anggur emir Kriptografi rinaldi munir
Kriptografi rinaldi munir Rinaldi munir kriptografi
Rinaldi munir kriptografi Rinaldi munir
Rinaldi munir Proton therapy for breast cancer after mastectomy
Proton therapy for breast cancer after mastectomy Psychoanalytic vs humanistic
Psychoanalytic vs humanistic Bioness bits cost
Bioness bits cost Humanistic therapies aim to boost
Humanistic therapies aim to boost Immune checkpoint inhibitors mechanism of action
Immune checkpoint inhibitors mechanism of action Primary bone vs secondary bone
Primary bone vs secondary bone Optimal lung cancer pathway
Optimal lung cancer pathway Asterias rubens materia medica
Asterias rubens materia medica Cleopatra view mammography
Cleopatra view mammography