Health Promotion of the School Aged Child Presented

- Slides: 29
Health Promotion of the School Aged Child Presented by: Jaime Callaghan (Family Nurse Practitioner student), Samantha Moyer (Physical Therapist student), and Sandra Bragg (Counselor student)
Overview • The goals of health maintenance in school-aged children are to promote health, detect any presence of disease, and to prevent adverse health problems or injuries in the future.
The Nurse Practitioner Role • Performs periodically scheduled well visit checks to assess mental and physical development. • Ensures immunizations are up to date. • Provides counseling and guidance to parents and children in areas of physical, behavioral, and emotional development. • Ensures the safety of the school-aged child and contacts proper authorities in cases of abuse or violence. • Reviews the daily habits of this age group such as: nutritional intake, quality of physical activity, time spent watching TV, sleeping habits, and difficulties at school.
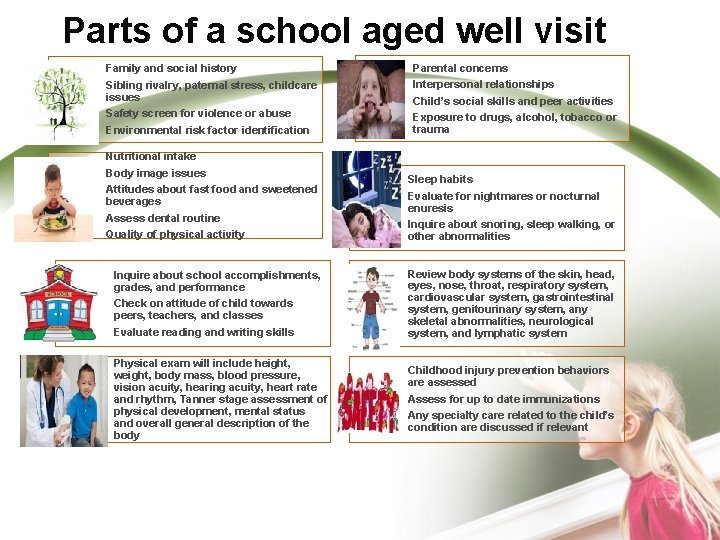
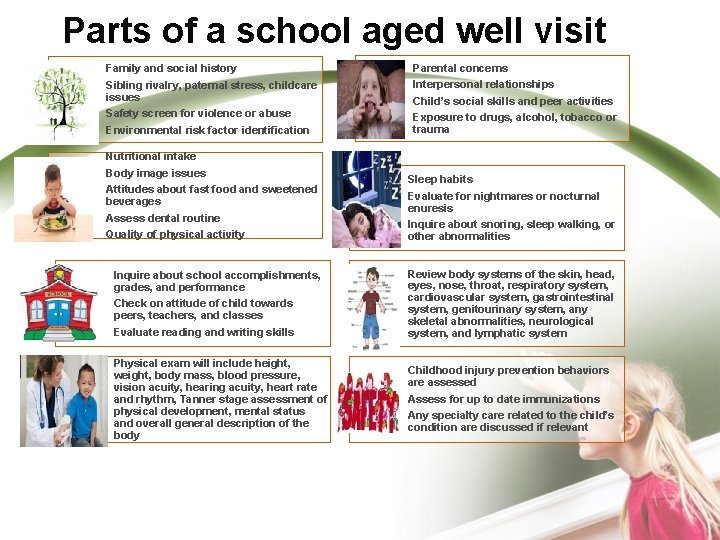
Parts of a school aged well visit Family and social history Sibling rivalry, paternal stress, childcare issues Safety screen for violence or abuse Environmental risk factor identification Nutritional intake Body image issues Attitudes about fast food and sweetened beverages Assess dental routine Quality of physical activity Parental concerns Interpersonal relationships Child’s social skills and peer activities Exposure to drugs, alcohol, tobacco or trauma Sleep habits Evaluate for nightmares or nocturnal enuresis Inquire about snoring, sleep walking, or other abnormalities Inquire about school accomplishments, grades, and performance Check on attitude of child towards peers, teachers, and classes Evaluate reading and writing skills Review body systems of the skin, head, eyes, nose, throat, respiratory system, cardiovascular system, gastrointestinal system, genitourinary system, any skeletal abnormalities, neurological system, and lymphatic system Physical exam will include height, weight, body mass, blood pressure, vision acuity, hearing acuity, heart rate and rhythm, Tanner stage assessment of physical development, mental status and overall general description of the body Childhood injury prevention behaviors are assessed Assess for up to date immunizations Any specialty care related to the child’s condition are discussed if relevant
Screening and secondary prevention tests • Hearing test • Vision test • Lead poisoning blood level for recent immigrants, foreign adoptees, and refugee children between 6 months and 16 years old. • Dental routinely done every six months • Tuberculosis screening for high risk children • Lipid assessment routinely at 2, 4, 6, 8, and 10 years of age or if risk factors indicate additional testing • X-rays for suspicion of injury or voiced concern by parent
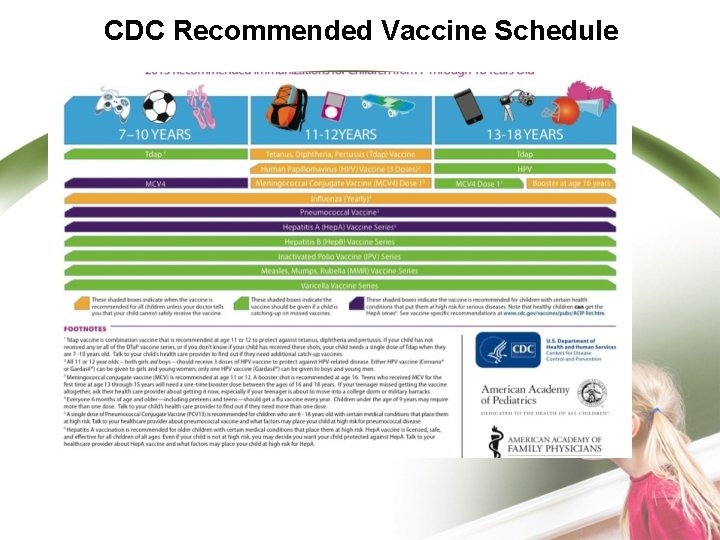
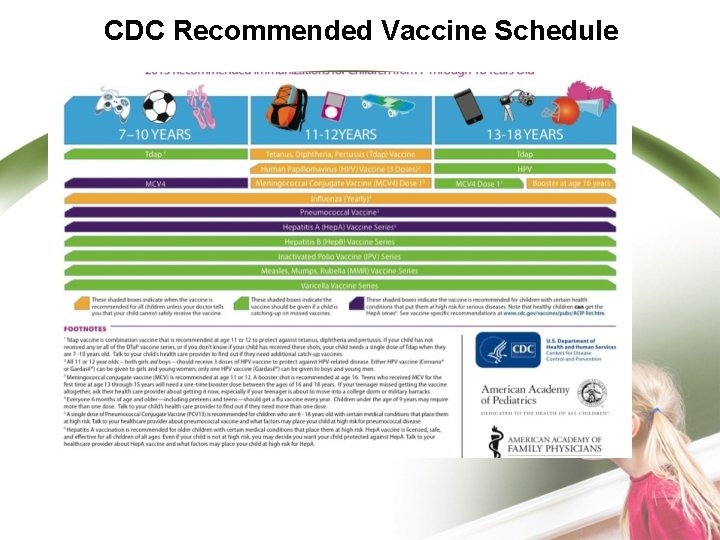
CDC Recommended Vaccine Schedule
How is the media effecting children? • If “screen time” is controlled by responsible parents or caregivers then children can be enhanced cognitively and socially. If watching or engaging in screen time together the experience can even bond interpersonal relationships. • Negative physical effects: promotes sedentary lifestyle, decreases imaginative play, encourages the use of unhealthy products such as beer from stimulating commercials, arouses aggressive impulses Negative cognitive effects: interferes with ability to creatively think, promotes short attention spans, teaches stereotypes of men and women, stimulates consumerism Negative behavioral effects: keeps child occupied if parents or babysitter is avoiding responsibility, promotes social isolation, competes with forming interpersonal relationships with others Negative emotional effects: reduces interest in school or home activities, can increase fear or anxiety, promotes passive aggressive acceptance of violent behavior Negative moral effects: confuses values and value system, fosters attitude of dominance of others, emphasizes sexuality and instant gratification. • •
Incidence of Childhood Obesity • • • About 12. 5 million children and adolescents aged 2 -19 are obese o 1 in 3 children are overweight or obese Prevalence of childhood obesity has tripled since 1980 Obese children have 70% chance of remaining obese in adult years
Consequences of Childhood Obesity • Health Risks Now o o o • o High blood pressure and high cholesterol Impaired glucose tolerance, insulin resistance, type 2 diabetes Breathing problems Joint and musculoskeletal problems Fatty liver disease, gallstones and GERD Social and psychological issues Future Health Risks o Adulthood obesity associated with heart disease, diabetes, and some cancers
Role of the Physical Therapist • Able to relief pain and help children resume daily activities • Can teach children exercises designed to help them regain strength and range of motion. • Can be beneficial to helping improve daily activity in the following children: those with sports injuries, developmental delays, head injuries, muscle disease, cardiac disease, those suffering from acute trauma, and many more.
Physical Activity Guidelines • Children should engage in at least 60 minutes of physical activity daily o Aerobic activity - majority of time § Either moderate or vigorous intensity o Muscle strengthening - at least 3 days/week § Gymnastics, tree climbing o Bone strengthening - at least 3 days/week § Running, Jump rope
Benefits of Physical Activity • • • Weight control Reduces the risk of cardiovascular disease, type 2 Diabetes, some cancers Strengthens bones and muscles Improves mental health and mood Can increase life expectancy
Increasing Activity Levels • • Encourage an active lifestyle through leading by example Make physical activity part of the family's daily routine o Family walks or playing games together Give children equipment that encourages physical activity. Take children to public parks, community fields or courts Positive attitudes Make physical activity fun o Team sports, running, skating, bicycling, swimming, playground activities or freetime play Limit television time. Encourage children to find fun activities to do by themselves, with friends or family o Bike riding, sports

Healthy Children Initiatives
Ethnic Considerations • • • For some cultures respect for your elders is ingrained into the adolescent thought process Some cultures have strong influences over the direction a school aged child takes their life. Be careful in addressing the child specifically without taking culture into consideration…. . this might be seen as a sign of disrespect if the head of the household is not the one properly addressed.
Does this child need a referral? • • • Dental- Any dental abnormality such as caries, gingivitis, or need for orthodontic care. Parents should be encouraged to take their child to the dentist every six months Physical therapy- Any injury whether it be sports related or not. Chronic illnesses such as cystic fibrosis or cerebral palsy may benefit from a physical therapy referral. Counseling- Economic issues at home, students at risk for dropping out of school, disruptive interpersonal relationships at home or in the community. Psychiatric- suicidal or homicidal tendencies expressed by patient, mental disturbances outside the scope of therapeutic counseling with trained professionals. Nutritionist- If body mass index falls outside of normal limitations for age, lack of dietary knowledge, abnormal lipid panel.
Role of the Counselor • Gains insight and knowledge to make valuable contributions to the school aged child’s treatment. • Provides support and positive role modeling. • Supervises and structures interpersonal relationships • Actively participates in group and individual meetings.
Mental Health Issues Involving the Schoolchild • There are many mental health issues that affect hundreds of thousands of school-age children every year • According to the DSM-IV-TR some common disorders onset during childhood are often not diagnosed until adulthood • Common mental illnesses seen in childhood – Anxiety disorders – ADD/ADHD – Autism spectrum disorders – Bipolar disorder – Depression – Eating disorders – Schizophrenia
Startling Statistics: Children and Adolescents • • • 5% to 9 % of children in the US have a serious emotional disturbance Only 21 % of children in the US who need mental health services actually receive services Approximately 13% of children ages 9 -17 have an anxiety disorder About 4% of school-aged children have Attention Deficit Hyperactivity Disorder Almost 4% of boys and 6% of girls have symptoms of Post. Traumatic Stress Disorder caused violence they have witnessed or endured • • • 2 out of 3 boys and 3 out of 4 girls in juvenile detention centers have a psychiatric disorder Students who have been bullied are 50% more likely to bring weapons to school campuses A young person commits suicide about every 2 hours 3 million teens have considered or attempted suicide in the past year Suicide is the 3 rd leading cause of death of the under 24 population only after accidents and homicides
• Screening and Assessment There are many screening. Tools and assessment tools used by mental health professionals – Child and Adolescent Functional Assessment Scale (CAFAS) ages 5 -19 – Children’s Depression Inventory-2 (CDI-2) ages 7 -17 – Reynold’s Child Depression Scale 2 (RCDS-2) ages 713 – Millon Clinical Multiaxial Inventory, 3 rd Edition (MCMIIII) – Minnesota Multiphasic Personality Inventory, 2 nd Edition (MMPI-A: ages 14 -18 – MACI (ages 13 -19) – The Achenbach Child Behavior Checklist (CBCL) • One test: ages 2 -3 • One test: ages 4 -18
Children’s Depression Inventory 2 nd edition • http: //downloads. mhs. com/masc/MASC 2_U S_Info. Sheet. pdf
When to assess for mental, emotional or behavioral issues • Problem behaviors in a variety of settings – Home, School, Peers, Daycare • Changes in appetite and/or sleep patterns • Social withdrawal, or new fearful behaviors • Returning to previous younger child behaviors for an extended period of time: – bedwetting, thumb sucking • Sadness and/or tearfulness • Self-destructive behaviors – Head banging, getting hurt often • Increased or repeated thoughts of death
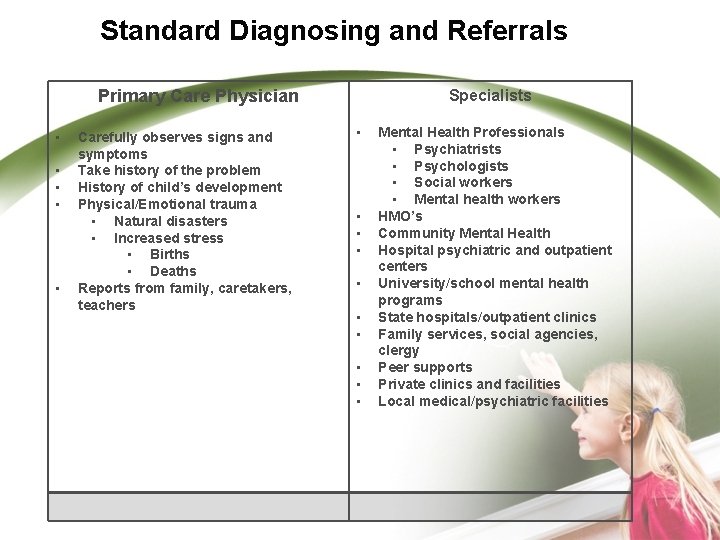
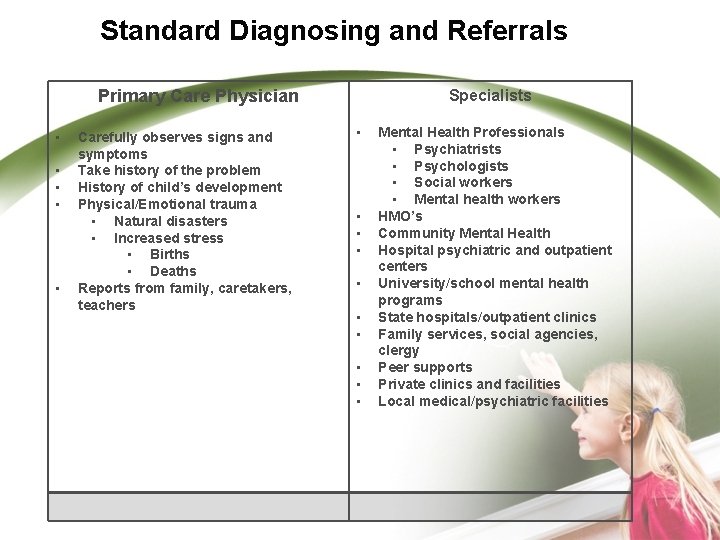
Standard Diagnosing and Referrals Specialists Primary Care Physician • • • Carefully observes signs and symptoms Take history of the problem History of child’s development Physical/Emotional trauma • Natural disasters • Increased stress • Births • Deaths Reports from family, caretakers, teachers • • • Mental Health Professionals • Psychiatrists • Psychologists • Social workers • Mental health workers HMO’s Community Mental Health Hospital psychiatric and outpatient centers University/school mental health programs State hospitals/outpatient clinics Family services, social agencies, clergy Peer supports Private clinics and facilities Local medical/psychiatric facilities
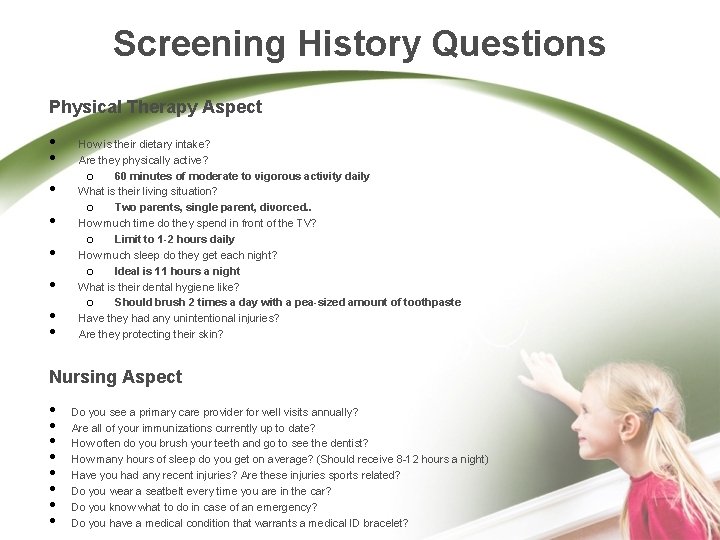
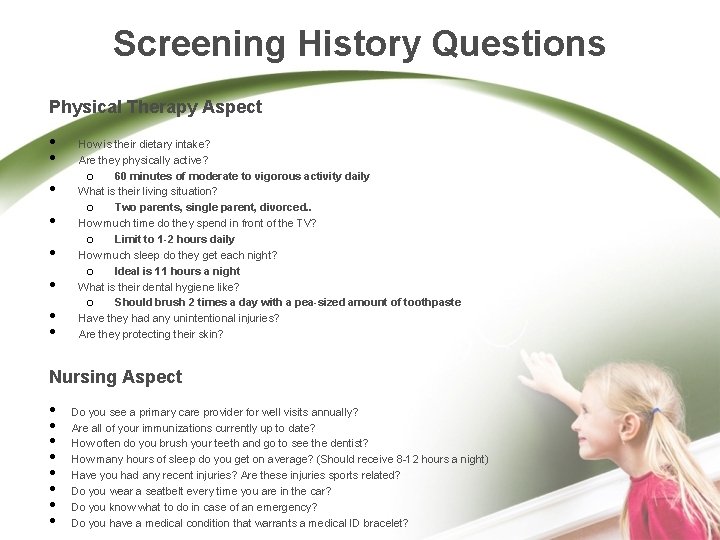
Screening History Questions Physical Therapy Aspect • • How is their dietary intake? Are they physically active? o 60 minutes of moderate to vigorous activity daily What is their living situation? o Two parents, single parent, divorced. . How much time do they spend in front of the TV? o Limit to 1 -2 hours daily How much sleep do they get each night? o Ideal is 11 hours a night What is their dental hygiene like? o Should brush 2 times a day with a pea-sized amount of toothpaste Have they had any unintentional injuries? Are they protecting their skin? Nursing Aspect • • Do you see a primary care provider for well visits annually? Are all of your immunizations currently up to date? How often do you brush your teeth and go to see the dentist? How many hours of sleep do you get on average? (Should receive 8 -12 hours a night) Have you had any recent injuries? Are these injuries sports related? Do you wear a seatbelt every time you are in the car? Do you know what to do in case of an emergency? Do you have a medical condition that warrants a medical ID bracelet?
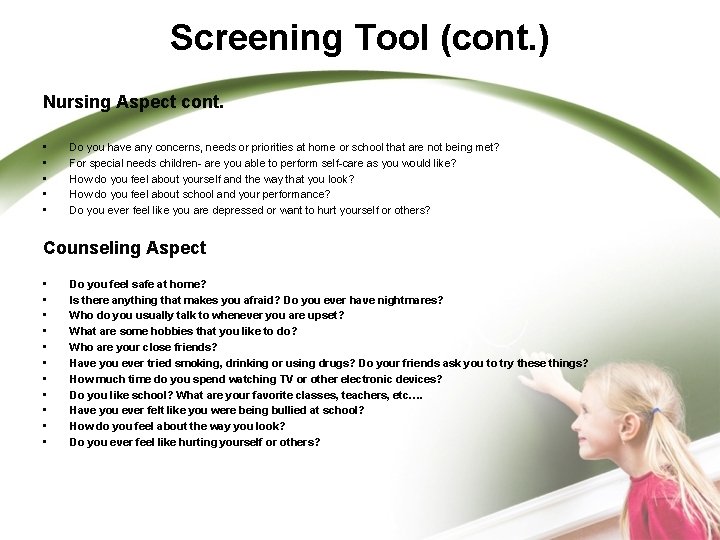
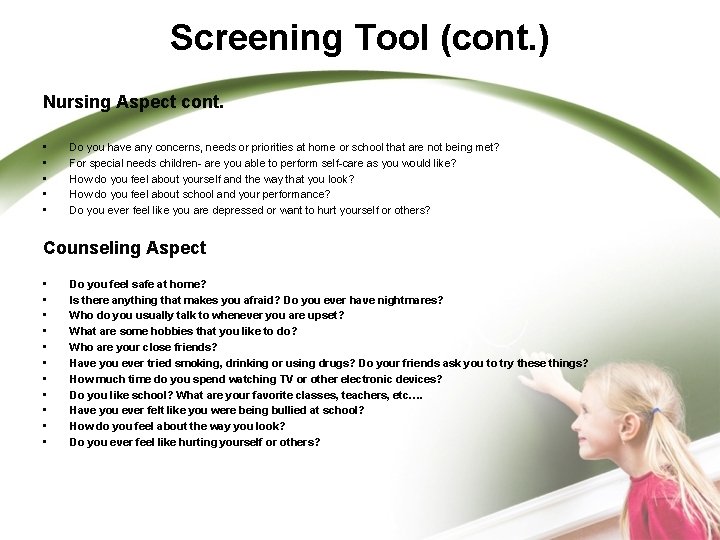
Screening Tool (cont. ) Nursing Aspect cont. • • • Do you have any concerns, needs or priorities at home or school that are not being met? For special needs children- are you able to perform self-care as you would like? How do you feel about yourself and the way that you look? How do you feel about school and your performance? Do you ever feel like you are depressed or want to hurt yourself or others? Counseling Aspect • • • Do you feel safe at home? Is there anything that makes you afraid? Do you ever have nightmares? Who do you usually talk to whenever you are upset? What are some hobbies that you like to do? Who are your close friends? Have you ever tried smoking, drinking or using drugs? Do your friends ask you to try these things? How much time do you spend watching TV or other electronic devices? Do you like school? What are your favorite classes, teachers, etc…. Have you ever felt like you were being bullied at school? How do you feel about the way you look? Do you ever feel like hurting yourself or others?
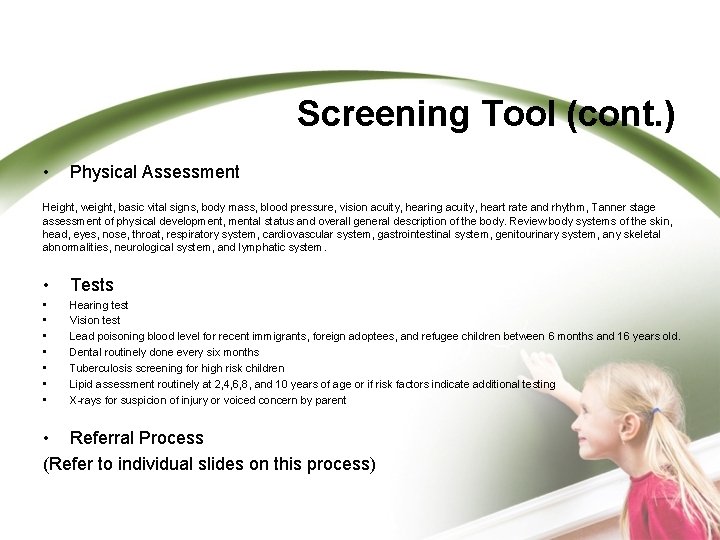
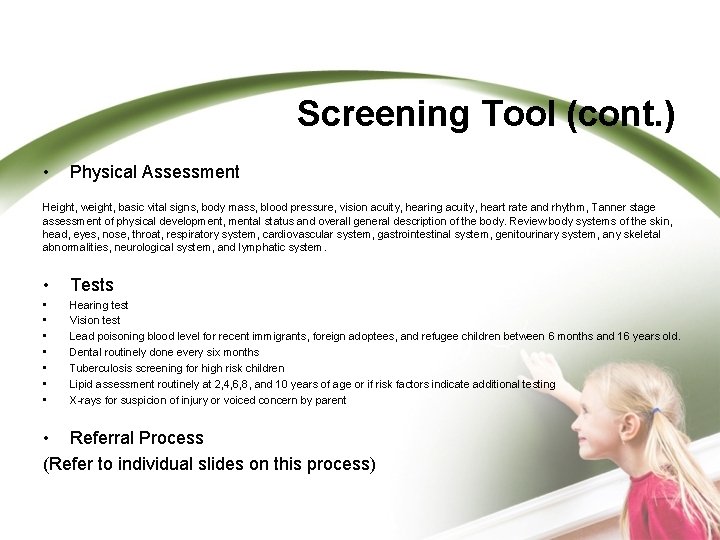
Screening Tool (cont. ) • Physical Assessment Height, weight, basic vital signs, body mass, blood pressure, vision acuity, hearing acuity, heart rate and rhythm, Tanner stage assessment of physical development, mental status and overall general description of the body. Review body systems of the skin, head, eyes, nose, throat, respiratory system, cardiovascular system, gastrointestinal system, genitourinary system, any skeletal abnormalities, neurological system, and lymphatic system. • Tests • • Hearing test Vision test Lead poisoning blood level for recent immigrants, foreign adoptees, and refugee children between 6 months and 16 years old. Dental routinely done every six months Tuberculosis screening for high risk children Lipid assessment routinely at 2, 4, 6, 8, and 10 years of age or if risk factors indicate additional testing X-rays for suspicion of injury or voiced concern by parent • Referral Process (Refer to individual slides on this process)
References • Anderson, D. , Keith, J, Novak, P. & Elliot, M. (2002). Mosby’s Medical, Nursing & Allied Health Dictionary (6 th ed. ). St. Louis, Missouri: Mosby. • Center for Disease Control and prevention (2013). Recommended Immunizations for Preteens and Teens (7 -18 years). Retrieved from www. cdc. gov/vaccines/schedules • Collins-bride, G. & Saxe, J. (2013). Clinical guidelines for advanced practice nursing (2 nd ed. ). Burlington, MA: Jones & Bartlett Learning. • Murray, R. , Zentner, J. , & Yakimo, R. (2009). Health Promotion Strategies Through the Life Span (8 th ed. ). Upper Saddle River, NJ: Pearson Education, Inc.
References (cont. ) • • Moses, Scott. Pediatric Health Maintenance. Family Practice Notebook. http: //www. fpnotebook. com/Prevent/HME/Pdtrc. Hth. Mntnc. htm. Published February 8, 2013. Accessed February 11, 2013 Basics About Childhood Obesity. Centers for Disease Control and Prevention. http: //www. cdc. gov/obesity/childhood/basics. html. April 27, 2010. Accessed February 7, 2013. Data and Statistics. Centers for Disease Control and Prevention. http: //www. cdc. gov/obesity/data/childhood. html. January 11, 2013. Accessed February 7, 2013. How much physical activity do children need? Centers for Disease Control and Prevention. http: //www. cdc. gov/physicalactivity/everyone/guidelines/children. html. November 9, 2011. Accessed February 7, 2013. Physical Activity and Health. Centers for Disease Control and Prevention. http: //www. cdc. gov/physicalactivity/everyone/health/index. html. February 16, 2011. Accessed February 7, 2013. Making Physical Activity a Part of a Child's Life. Centers for Disease Control and Prevention. http: //www. cdc. gov/physicalactivity/everyone/getactive/children. html. November 9, 2011. Accessed February 7, 2013. Overweight Children in America – Childhood Obesity Statistics. Your Health Community. http: //obesity. ygoy. com/overweight-chidren-in-america-childhoodobesity-statistics/. Accessed February 11, 2013.
References (cont. ) • American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision, Washington, DC, American Psychiatric Association, 2000. • National Institute for Mental Health, retrieved from the world wide web, February 10, 2013: http: //www. nimh. nih. gov/health/publicati ons/treatment-of-children-with-mentalillness-fact-sheet/index. shtml
 Similarities between health education and health promotion
Similarities between health education and health promotion Health maintenance and promotion
Health maintenance and promotion Kinesiology ucf catalog
Kinesiology ucf catalog Open disclosure in aged care
Open disclosure in aged care Nettles poem
Nettles poem Nettles poem annotated
Nettles poem annotated Sarah russell aged care
Sarah russell aged care What are the 5 principles of cultural safety?
What are the 5 principles of cultural safety? My aged care
My aged care A stout middle aged man with enormous
A stout middle aged man with enormous Dignity of risk in aged care
Dignity of risk in aged care Kimberley aged care services
Kimberley aged care services What is cultural safety in aged care
What is cultural safety in aged care Ananda aged care
Ananda aged care National program list
National program list 전위 순회
전위 순회 Pengertian promkes adalah
Pengertian promkes adalah Pender metaparadigm
Pender metaparadigm Health promotion approach
Health promotion approach Health promotion approaches
Health promotion approaches Nola pender health promotion theory
Nola pender health promotion theory 5 levels of prevention leavell and clark
5 levels of prevention leavell and clark Jessica konopka
Jessica konopka Health promotion emblem
Health promotion emblem Ethical issues in health promotion
Ethical issues in health promotion Health promotion and levels of disease prevention
Health promotion and levels of disease prevention Chapter 9 patient education and health promotion
Chapter 9 patient education and health promotion Health promotion and levels of disease prevention
Health promotion and levels of disease prevention Health promotion program in malaysia
Health promotion program in malaysia Caplan and holland model of health promotion
Caplan and holland model of health promotion