Group 5 Provision and Improvement of Clinical Care
- Slides: 19
Group 5 Provision and Improvement of Clinical Care for Joint TB/HIV Activities
1. What steps are required for strengthening of diagnostic processes for TB and HIV/AIDS? – General health services – TB treatment sites – HIV/AIDS treatment sites
General Features • Strengthening Health System • Community level • Remove barriers to access to health care facilities • Improve human resources at health care facilities • Specific tools/commodities
Strengthening Health System • Collaboration between medical and multisectoral sectors • Increase involvement of district health management authorities • Strengthen interaction between laboratory and health system and other social services (if not the same)
Community Level • Increase community awareness of signs/symptoms of HIV/TB to improve seeking of health services • Include traditional healers, shops • In doing this, liason between medical and multisectoral sectors • Work to reduce stigma related to both diseases
Remove Barriers to Access to TB/HIV Diagnostic Services • Identified barriers – Cost – Distance – Perception that no treatment is available (esp. for HIV)
Strengthen Human Resources at Health Care Facilities • Increase the numbers of health care workers (paid—not volunteer) – Determine numbers of staff needed to provide services – Address IMF recommendation to reduce numbers of government workers • Improve training regarding recognition of sx/suspecting TB/HIV – Update clinicians trained previously – Incorporate TB/HIV information into current curriculae at medical/nursing schools etc.
Improve Human Resources at Health Care Facilities (cont. ) • Provide counseling training for all involved health care workers • Train lab technicians regarding the importance of the results to patients • Cross training – Train laboratory workers currently performing AFB smears to do rapid tests for HIV – Consider training lower level health care workers or counsellors to perform rapid tests for HIV – Consider having staff from TB clinic seconded to HIV clinics
Improve Human Resources at Health Care Facilities (cont. ) • Consider prioritizing treatment of HCWs (losing valuable trained staff to HIV/TB) – Incentive to work as a health care worker
Specific practices/ commodities • Develop joint guidelines that address both HIV and TB (and other needs) – Simple – Wall charts • Increase access to privacy (esp. HIV) • Consider adjustment of diagnostic criteria – Consider more empiric therapy – Consider “diagnostic” trials of anti-TB rx (without rifamycins) – ? Expand access to TB culture facilities – Reduce turn around time for results of diagnostic tests (esp. TB)
Specific practices/ commodities (cont. ) • Reduce turnaround time for results of TB diagnostic tests – Facilitate transport of specimens to laboratories – Facilitate transmission of results to clinicians (phone) • Strengthen procurement of HIV test kits (ensure quality)
Entry Point-Specific Interventions • To improve diagnosis in general medical settings – Develop training materials that address altered presentation of TB in the context of HIV • At TB treatment sites – Incorporate VCT services on site at TB treatment sites • At VCT sites – Conduct active case finding at VCT sites
2. How Can Referral Between TB and HIV Services be Strengthened ? • Ensure information about where to refer is available at relevant sites • Clarify specific roles of referring sites, sites being referred to • Consider provide services for both at the same location • Use of referral forms • Build network referral system in community (with community ownership)
How Can Referral Between TB and HIV Services be Strengthened (cont) • Involve district health managers at initial stage (build into system)
3. What Elements of TB/HIV Programs Need to be in Place Prior to ARVs? • • Need to have infrastructure Need functional health delivery system Boost laboratory services Have drugs and supplies in place for management of TB, HIV (other than ARVs) • Ability to conduct ongoing counselling for TB and HIV • Clear idea of eligibility criteria, ethical considerations
Necessary Elements (cont. ) • Consider implementation of ARV services in areas with strong TB programs…because of experience with: – Long term follow-up of patients/support of medication adherence – Supply chain for drugs – Training • But…. consider implementing HIV programs in areas with weak health systems and using treatment programs for HIV to strengthen the health system.
4. When/How Should ARVs be Implemented to Patients on TB therapy • Begin ARV treatment after completion of initiation phase (include in guidelines) • Consider implementing ARVs after completion of TB therapy (perhaps by the same HCWs, in the same setting) – Continuing adherence support from accompanateur – May improve management of interactions/co-toxicities
When/How Should ARVs be Implemented to Patients on TB therapy • But caution because: – Some infection control issues related to offering both services in the same site – May overburden already stressed TB programs
When/How to Give ARVs to TB Patients Cont. • Also consider closely related program and have patients move from TB to ARV program an included program that is a distinct component
 The provision of a public good generates a
The provision of a public good generates a Hip fracture care clinical care standard
Hip fracture care clinical care standard Independent service provision
Independent service provision Outpatient clinical documentation improvement
Outpatient clinical documentation improvement Clinical documentation improvement for cardiology
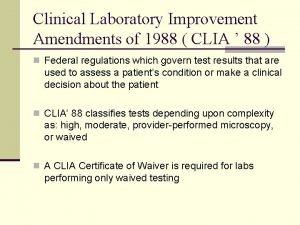
Clinical documentation improvement for cardiology Clinical laboratory improvement amendments of 1988
Clinical laboratory improvement amendments of 1988 Primary secondary tertiary health care definition
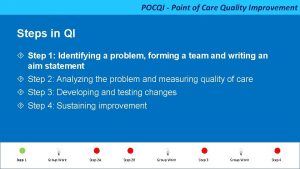
Primary secondary tertiary health care definition Pocqi ppt
Pocqi ppt Qi 101: introduction to health care improvement
Qi 101: introduction to health care improvement Catering provision meaning
Catering provision meaning The provision and use of work equipment regulations 1998
The provision and use of work equipment regulations 1998 Closing off the year
Closing off the year The foundry mft
The foundry mft Whole health clinical group
Whole health clinical group Dr nicola burbidge
Dr nicola burbidge Croydon clinical commissioning group
Croydon clinical commissioning group Costed provision map template
Costed provision map template Samba ad domain controller
Samba ad domain controller Summarise types of early years provision
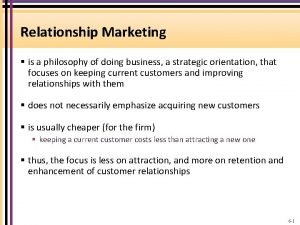
Summarise types of early years provision Relationship marketing philosophy
Relationship marketing philosophy