Fluency Clinic Standardized Formal Unstandardized Other Test of











- Slides: 25
Fluency Clinic





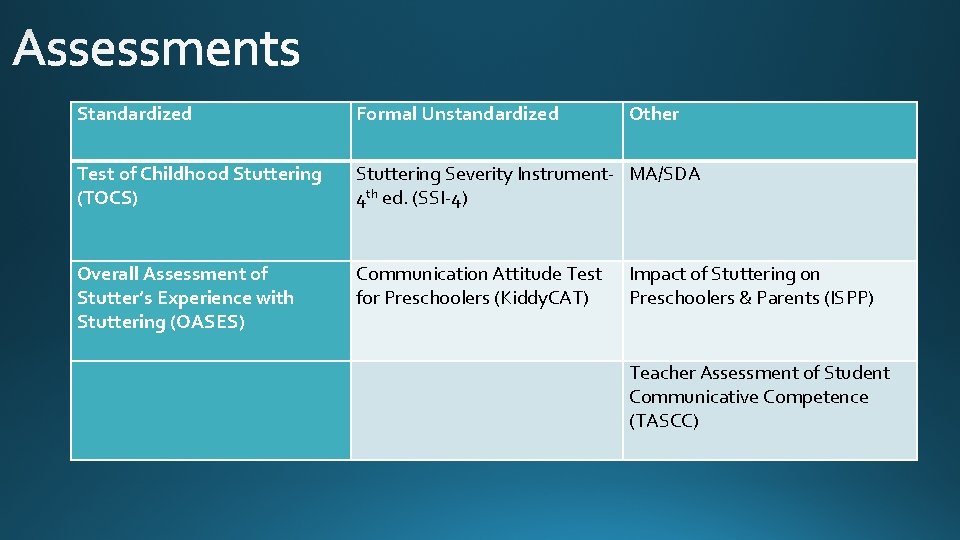
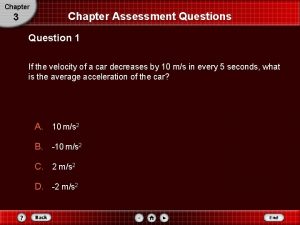
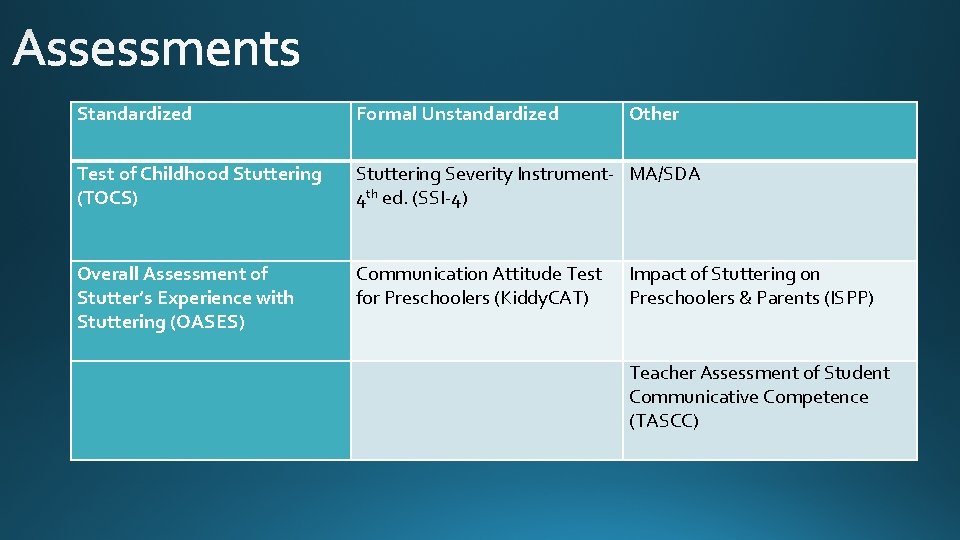
Standardized Formal Unstandardized Other Test of Childhood Stuttering (TOCS) Stuttering Severity Instrument- MA/SDA 4 th ed. (SSI-4) Overall Assessment of Stutter’s Experience with Stuttering (OASES) Communication Attitude Test for Preschoolers (Kiddy. CAT) Impact of Stuttering on Preschoolers & Parents (ISPP) Teacher Assessment of Student Communicative Competence (TASCC)
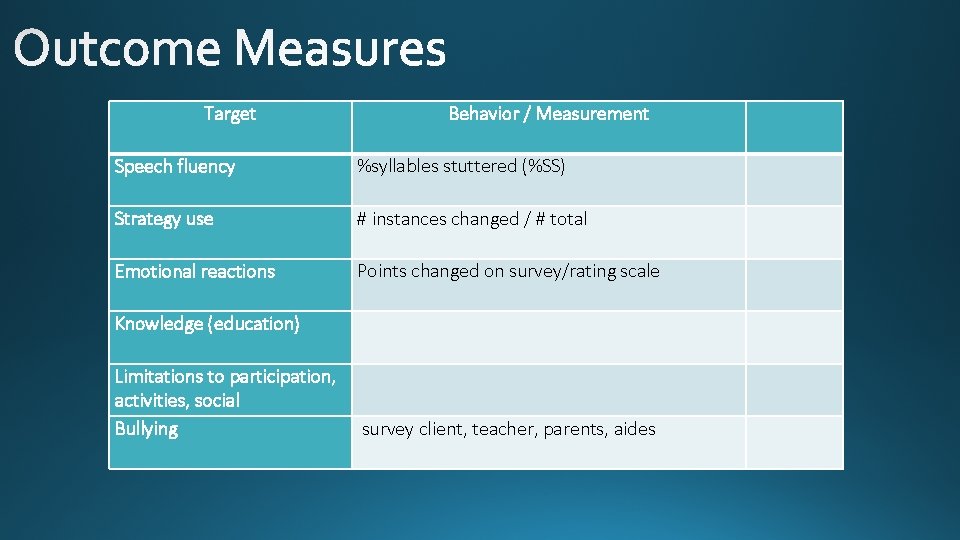
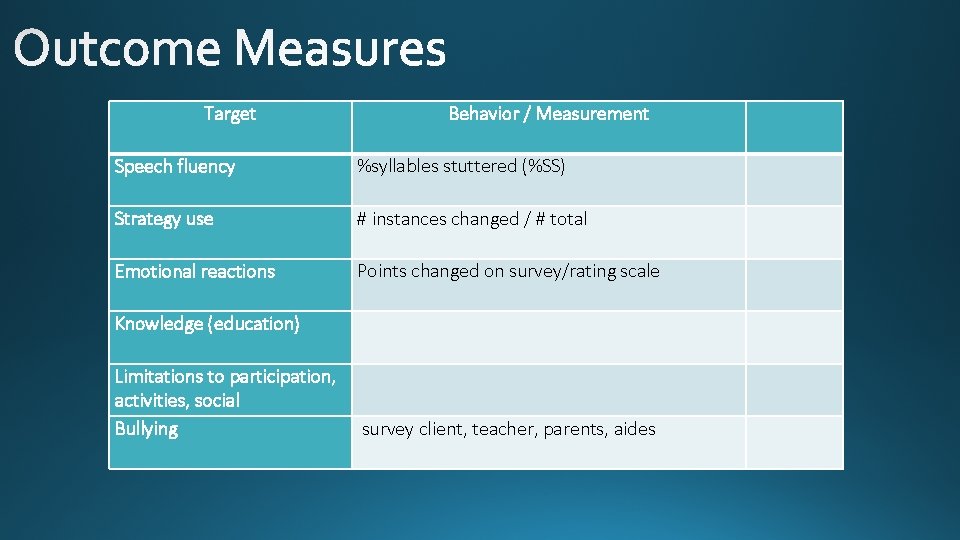
Target Behavior / Measurement Speech fluency %syllables stuttered (%SS) Strategy use # instances changed / # total Emotional reactions Points changed on survey/rating scale Knowledge (education) Limitations to participation, activities, social Bullying survey client, teacher, parents, aides
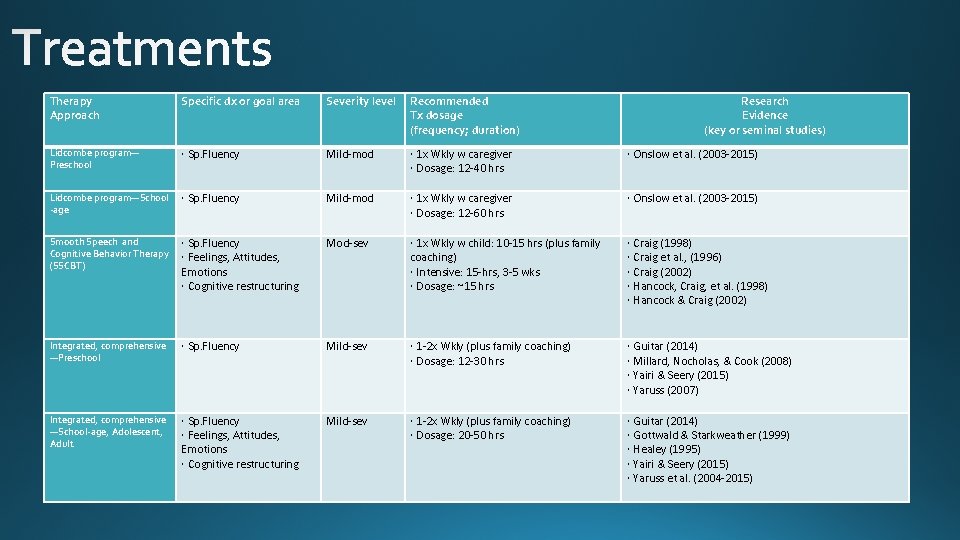
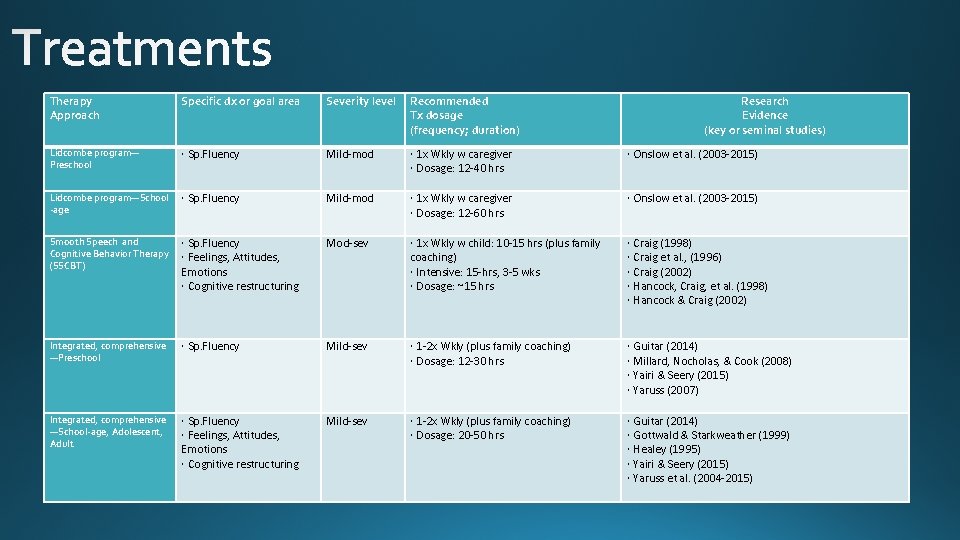
Therapy Approach Specific dx or goal area Severity level Recommended Tx dosage (frequency; duration) Research Evidence (key or seminal studies) Lidcombe program— Preschool Sp. Fluency Mild-mod 1 x Wkly w caregiver Dosage: 12 -40 hrs Onslow et al. (2003 -2015) Lidcombe program—School -age Sp. Fluency Mild-mod 1 x Wkly w caregiver Dosage: 12 -60 hrs Onslow et al. (2003 -2015) Smooth Speech and Cognitive Behavior Therapy (SSCBT) Sp. Fluency Feelings, Attitudes, Emotions Cognitive restructuring Mod-sev 1 x Wkly w child: 10 -15 hrs (plus family coaching) Intensive: 15 -hrs, 3 -5 wks Dosage: ~15 hrs Integrated, comprehensive —Preschool Sp. Fluency Mild-sev 1 -2 x Wkly (plus family coaching) Dosage: 12 -30 hrs Integrated, comprehensive —School-age, Adolescent, Adult Sp. Fluency Feelings, Attitudes, Emotions Cognitive restructuring Mild-sev 1 -2 x Wkly (plus family coaching) Dosage: 20 -50 hrs Craig (1998) Craig et al. , (1996) Craig (2002) Hancock, Craig, et al. (1998) Hancock & Craig (2002) Guitar (2014) Millard, Nocholas, & Cook (2008) Yairi & Seery (2015) Yaruss (2007) Guitar (2014) Gottwald & Starkweather (1999) Healey (1995) Yairi & Seery (2015) Yaruss et al. (2004 -2015)

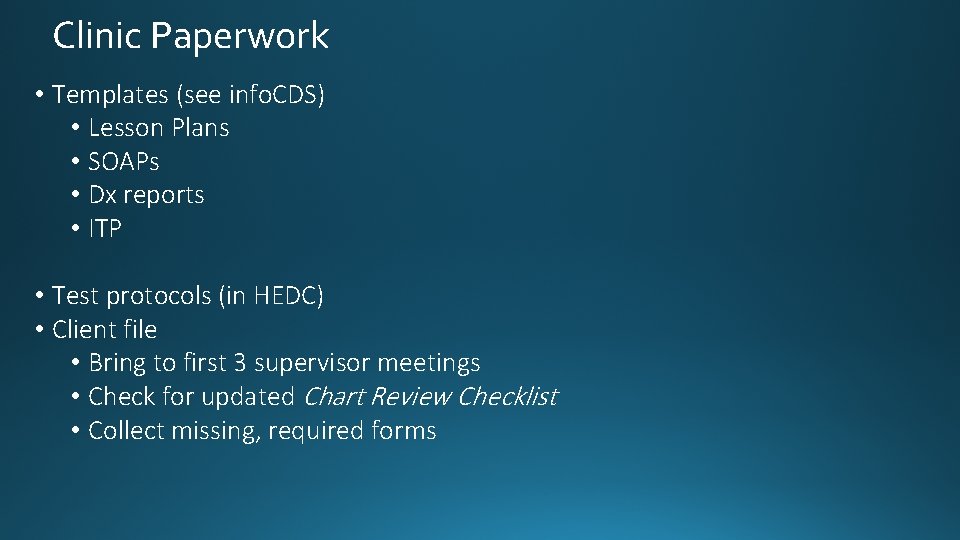
Clinic Paperwork • Templates (see info. CDS) • Lesson Plans • SOAPs • Dx reports • ITP • Test protocols (in HEDC) • Client file • Bring to first 3 supervisor meetings • Check for updated Chart Review Checklist • Collect missing, required forms


CHARTRs • Review CHARTR’s started last week in Clinical Methods • Work with PM to complete second CHARTR • See PM checklist for timelines for clinical documents to be submitted to supervisor

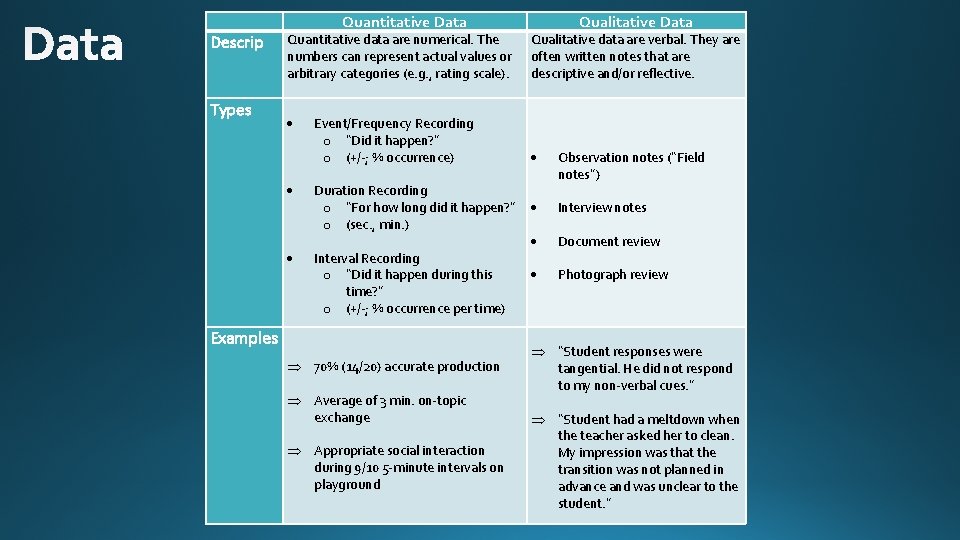
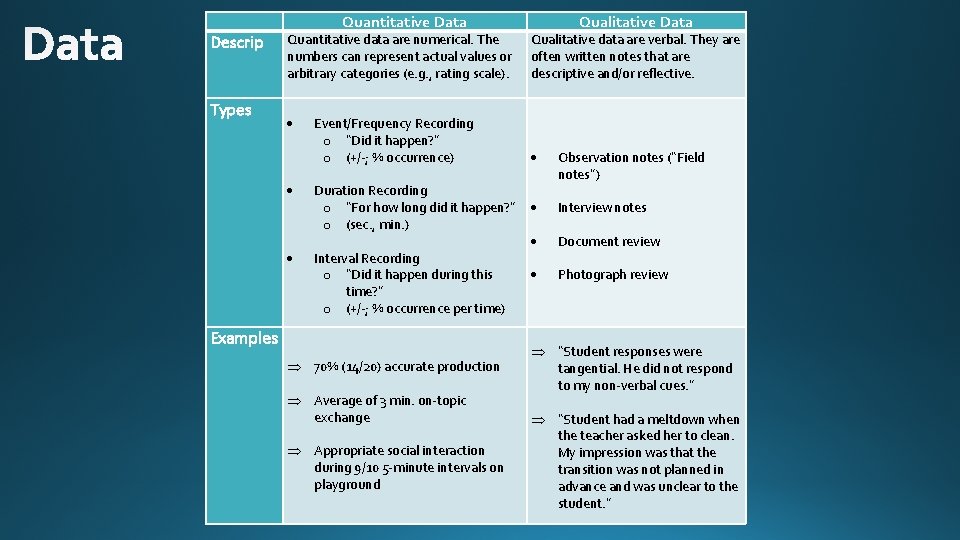
Descrip Types Quantitative Data Quantitative data are numerical. The numbers can represent actual values or arbitrary categories (e. g. , rating scale). Event/Frequency Recording o “Did it happen? ” o (+/-; % occurrence) Duration Recording o “For how long did it happen? ” o (sec. , min. ) Interval Recording o “Did it happen during this time? ” o (+/-; % occurrence per time) Examples 70% (14/20) accurate production Average of 3 min. on-topic exchange Appropriate social interaction during 9/10 5 -minute intervals on playground Qualitative Data Qualitative data are verbal. They are often written notes that are descriptive and/or reflective. Observation notes (“Field notes”) Interview notes Document review Photograph review “Student responses were tangential. He did not respond to my non-verbal cues. ” “Student had a meltdown when the teacher asked her to clean. My impression was that the transition was not planned in advance and was unclear to the student. ”
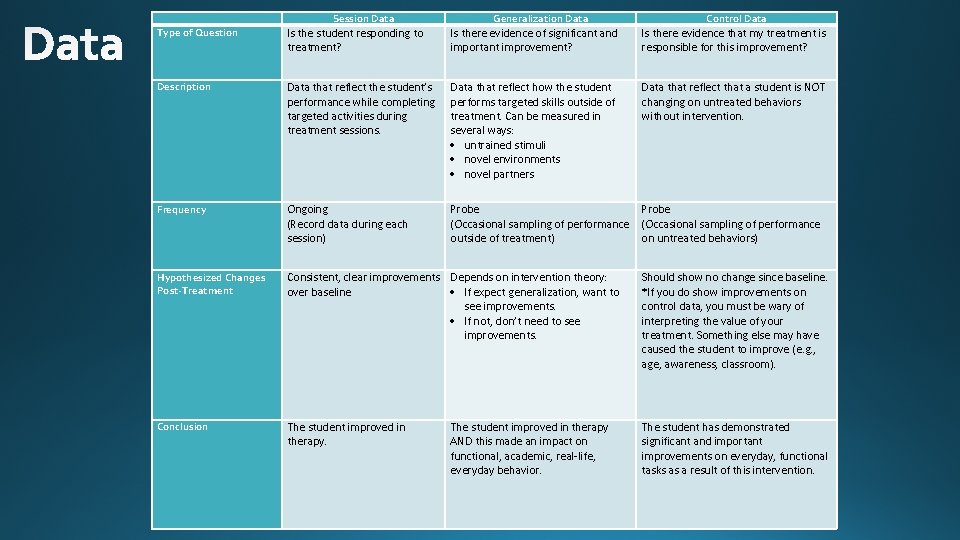
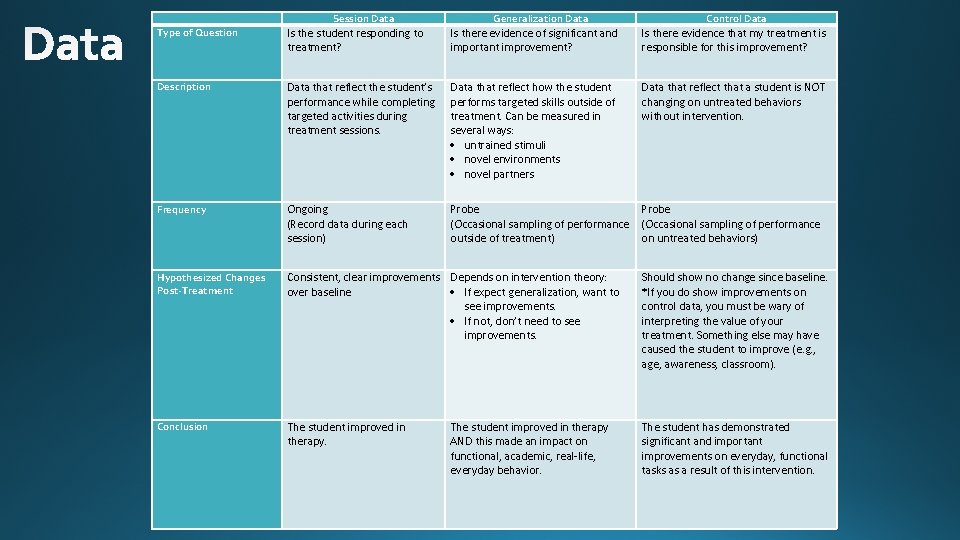
Type of Question Session Data Generalization Data Control Data Is the student responding to treatment? Is there evidence of significant and important improvement? Is there evidence that my treatment is responsible for this improvement? Description Data that reflect the student’s performance while completing targeted activities during treatment sessions. Data that reflect how the student performs targeted skills outside of treatment. Can be measured in several ways: untrained stimuli novel environments novel partners Data that reflect that a student is NOT changing on untreated behaviors without intervention. Frequency Ongoing (Record data during each session) Probe (Occasional sampling of performance outside of treatment) on untreated behaviors) Hypothesized Changes Post-Treatment Consistent, clear improvements Depends on intervention theory: over baseline If expect generalization, want to see improvements. If not, don’t need to see improvements. Should show no change since baseline. *If you do show improvements on control data, you must be wary of interpreting the value of your treatment. Something else may have caused the student to improve (e. g. , age, awareness, classroom). Conclusion The student improved in therapy. The student has demonstrated significant and important improvements on everyday, functional tasks as a result of this intervention. The student improved in therapy AND this made an impact on functional, academic, real-life, everyday behavior.

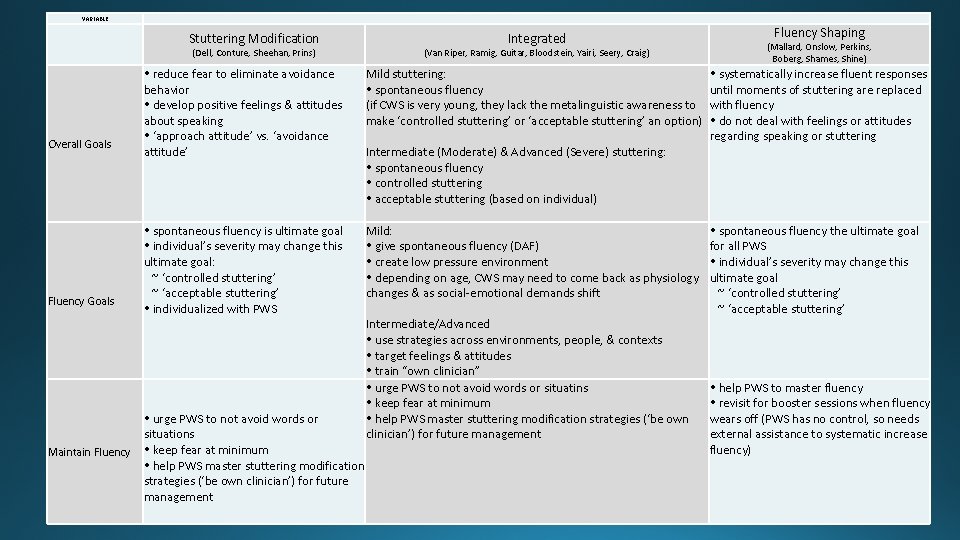
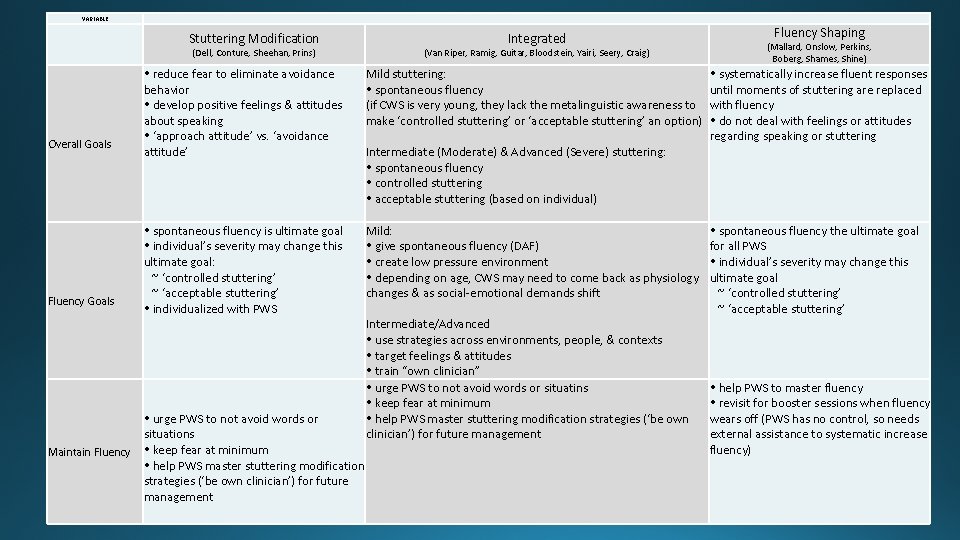
VARIABLE Overall Goals Fluency Goals Maintain Fluency Stuttering Modification Integrated (Dell, Conture, Sheehan, Prins) reduce fear to eliminate avoidance behavior develop positive feelings & attitudes about speaking ‘approach attitude’ vs. ‘avoidance attitude’ spontaneous fluency is ultimate goal individual’s severity may change this ultimate goal: ~ ‘controlled stuttering’ ~ ‘acceptable stuttering’ individualized with PWS (Van Riper, Ramig, Guitar, Bloodstein, Yairi, Seery, Craig) Mild stuttering: spontaneous fluency (if CWS is very young, they lack the metalinguistic awareness to make ‘controlled stuttering’ or ‘acceptable stuttering’ an option) Intermediate (Moderate) & Advanced (Severe) stuttering: spontaneous fluency controlled stuttering acceptable stuttering (based on individual) Mild: give spontaneous fluency (DAF) create low pressure environment depending on age, CWS may need to come back as physiology changes & as social-emotional demands shift Intermediate/Advanced use strategies across environments, people, & contexts target feelings & attitudes train “own clinician” urge PWS to not avoid words or situatins keep fear at minimum help PWS master stuttering modification strategies (‘be own clinician’) for future management urge PWS to not avoid words or situations keep fear at minimum help PWS master stuttering modification strategies (‘be own clinician’) for future management Fluency Shaping (Mallard, Onslow, Perkins, Boberg, Shames, Shine) systematically increase fluent responses until moments of stuttering are replaced with fluency do not deal with feelings or attitudes regarding speaking or stuttering spontaneous fluency the ultimate goal for all PWS individual’s severity may change this ultimate goal ~ ‘controlled stuttering’ ~ ‘acceptable stuttering’ help PWS to master fluency revisit for booster sessions when fluency wears off (PWS has no control, so needs external assistance to systematic increase fluency)
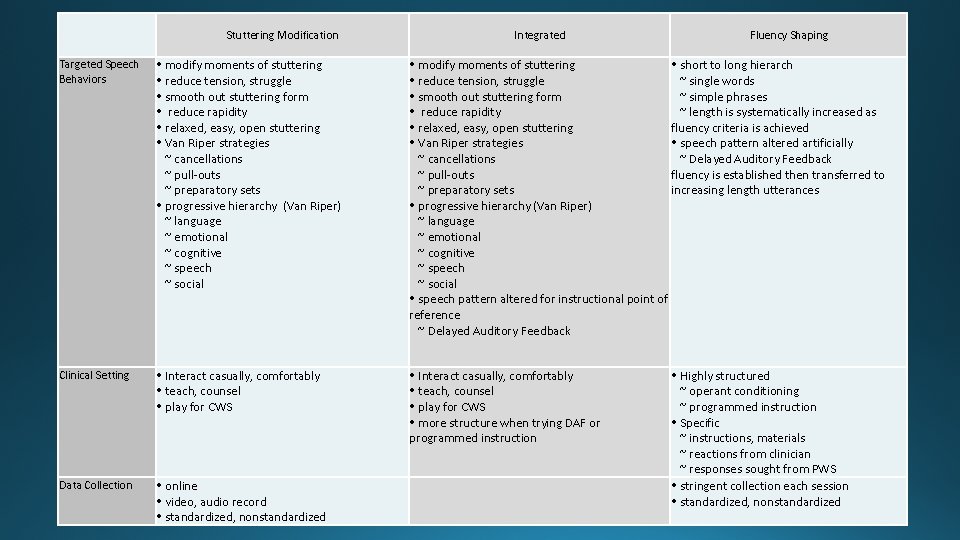
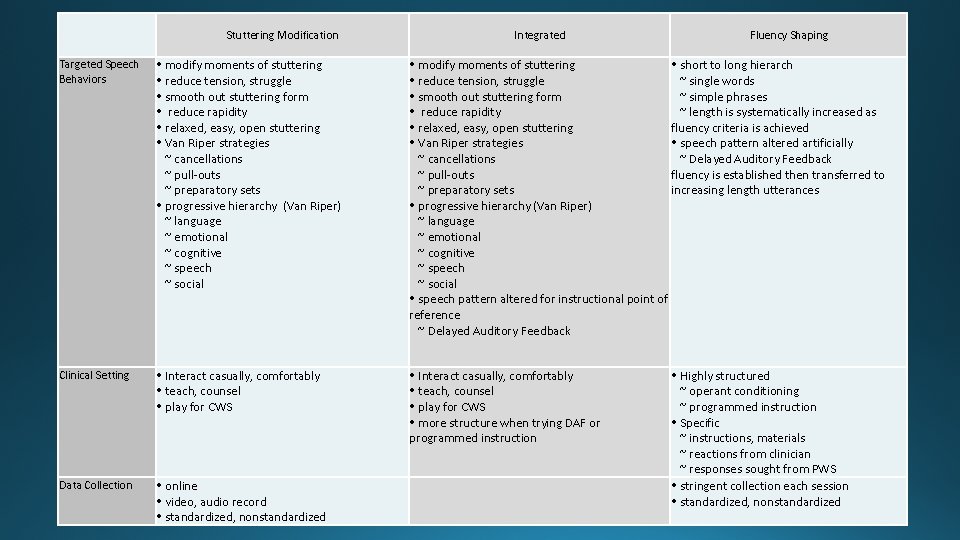
Stuttering Modification Integrated Fluency Shaping Targeted Speech Behaviors modify moments of stuttering reduce tension, struggle smooth out stuttering form reduce rapidity relaxed, easy, open stuttering Van Riper strategies ~ cancellations ~ pull-outs ~ preparatory sets progressive hierarchy (Van Riper) ~ language ~ emotional ~ cognitive ~ speech ~ social modify moments of stuttering short to long hierarch reduce tension, struggle ~ single words smooth out stuttering form ~ simple phrases reduce rapidity ~ length is systematically increased as relaxed, easy, open stuttering fluency criteria is achieved Van Riper strategies speech pattern altered artificially ~ cancellations ~ Delayed Auditory Feedback ~ pull-outs fluency is established then transferred to ~ preparatory sets increasing length utterances progressive hierarchy (Van Riper) ~ language ~ emotional ~ cognitive ~ speech ~ social speech pattern altered for instructional point of reference ~ Delayed Auditory Feedback Clinical Setting Interact casually, comfortably teach, counsel play for CWS more structure when trying DAF or programmed instruction Data Collection online video, audio record standardized, nonstandardized Highly structured ~ operant conditioning ~ programmed instruction Specific ~ instructions, materials ~ reactions from clinician ~ responses sought from PWS stringent collection each session standardized, nonstandardized
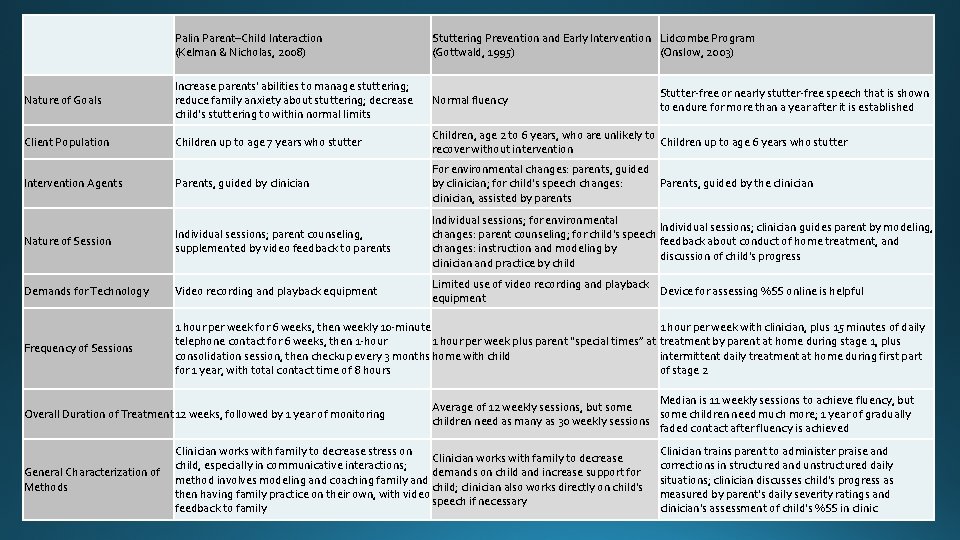
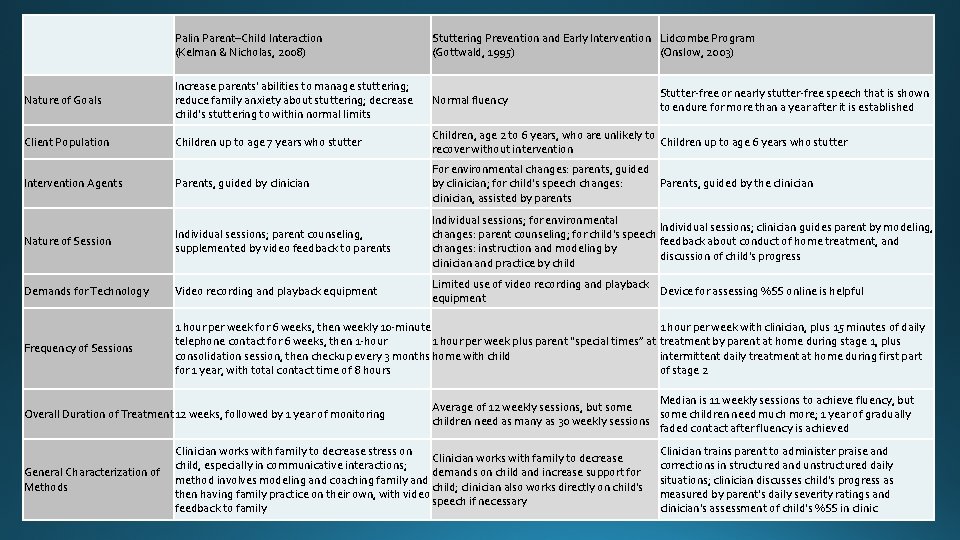
Palin Parent–Child Interaction (Kelman & Nicholas, 2008) Stuttering Prevention and Early Intervention Lidcombe Program (Gottwald, 1995) (Onslow, 2003) Nature of Goals Increase parents' abilities to manage stuttering; reduce family anxiety about stuttering; decrease child's stuttering to within normal limits Normal fluency Client Population Children up to age 7 years who stutter Children, age 2 to 6 years, who are unlikely to Children up to age 6 years who stutter recover without intervention Intervention Agents Parents, guided by clinician For environmental changes: parents, guided Parents, guided by the clinician by clinician; for child's speech changes: clinician, assisted by parents Nature of Session Individual sessions; parent counseling, supplemented by video feedback to parents Individual sessions; for environmental Individual sessions; clinician guides parent by modeling, changes: parent counseling; for child's speech feedback about conduct of home treatment, and changes: instruction and modeling by discussion of child's progress clinician and practice by child Demands for Technology Video recording and playback equipment Limited use of video recording and playback Device for assessing %SS online is helpful equipment Frequency of Sessions 1 hour per week for 6 weeks, then weekly 10 -minute 1 hour per week with clinician, plus 15 minutes of daily telephone contact for 6 weeks, then 1 -hour 1 hour per week plus parent “special times” at treatment by parent at home during stage 1, plus consolidation session, then checkup every 3 months home with child intermittent daily treatment at home during first part for 1 year, with total contact time of 8 hours of stage 2 Overall Duration of Treatment 12 weeks, followed by 1 year of monitoring General Characterization of Methods Stutter-free or nearly stutter-free speech that is shown to endure for more than a year after it is established Median is 11 weekly sessions to achieve fluency, but Average of 12 weekly sessions, but some children need much more; 1 year of gradually children need as many as 30 weekly sessions faded contact after fluency is achieved Clinician works with family to decrease stress on Clinician works with family to decrease child, especially in communicative interactions; demands on child and increase support for method involves modeling and coaching family and child; clinician also works directly on child's then having family practice on their own, with video speech if necessary feedback to family Clinician trains parent to administer praise and corrections in structured and unstructured daily situations; clinician discusses child's progress as measured by parent's daily severity ratings and clinician's assessment of child's %SS in clinic
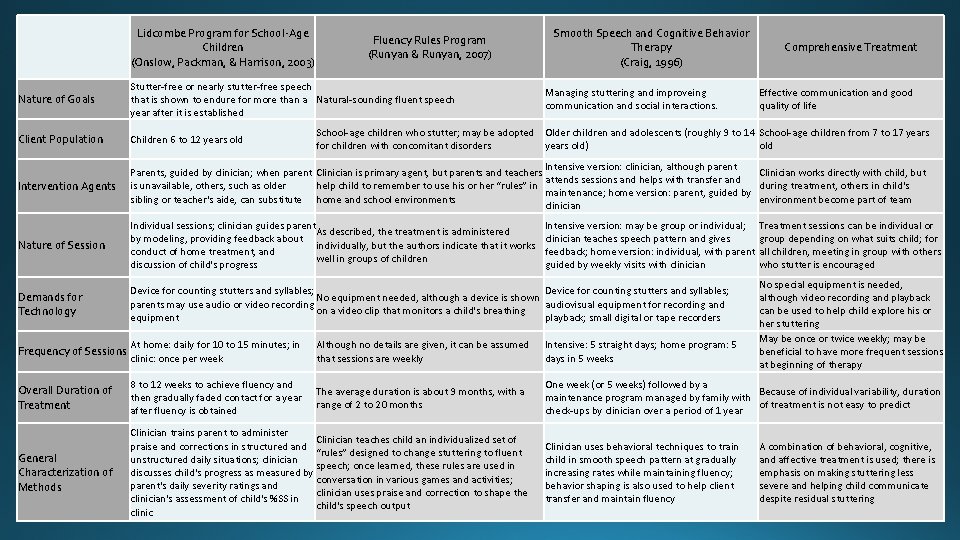
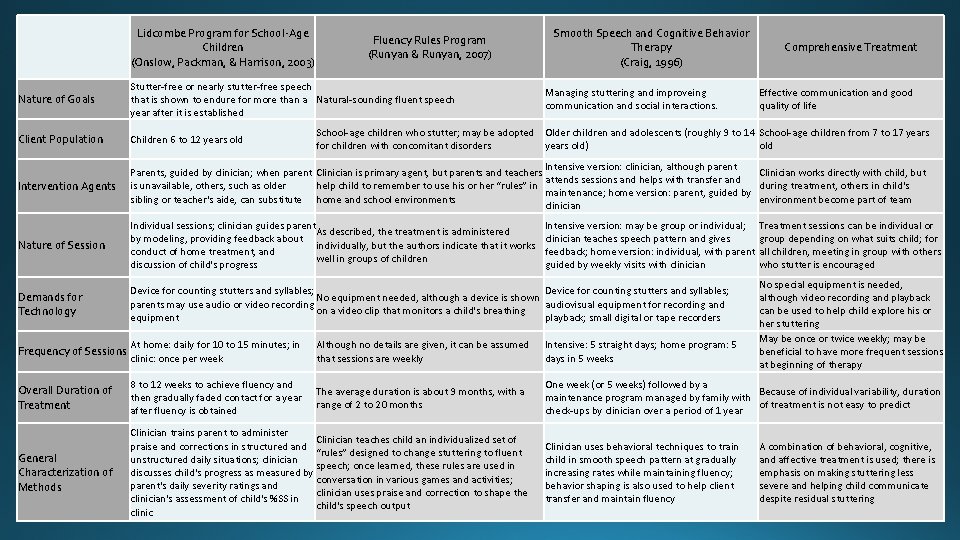
Lidcombe Program for School-Age Children (Onslow, Packman, & Harrison, 2003) Fluency Rules Program (Runyan & Runyan, 2007) Smooth Speech and Cognitive Behavior Therapy (Craig, 1996) Comprehensive Treatment Nature of Goals Stutter-free or nearly stutter-free speech that is shown to endure for more than a Natural-sounding fluent speech year after it is established Client Population Children 6 to 12 years old Intervention Agents Intensive version: clinician, although parent Parents, guided by clinician; when parent Clinician is primary agent, but parents and teachers Clinician works directly with child, but attends sessions and helps with transfer and is unavailable, others, such as older help child to remember to use his or her “rules” in during treatment, others in child's maintenance; home version: parent, guided by sibling or teacher's aide, can substitute home and school environments environment become part of team clinician Nature of Session Individual sessions; clinician guides parent As described, the treatment is administered by modeling, providing feedback about individually, but the authors indicate that it works conduct of home treatment, and well in groups of children discussion of child's progress Demands for Technology Device for counting stutters and syllables; No equipment needed, although a device is shown parents may use audio or video recording audiovisual equipment for recording and on a video clip that monitors a child's breathing equipment playback; small digital or tape recorders Frequency of Sessions At home: daily for 10 to 15 minutes; in clinic: once per week Although no details are given, it can be assumed that sessions are weekly Intensive: 5 straight days; home program: 5 days in 5 weeks Overall Duration of Treatment 8 to 12 weeks to achieve fluency and then gradually faded contact for a year after fluency is obtained The average duration is about 9 months, with a range of 2 to 20 months One week (or 5 weeks) followed by a Because of individual variability, duration maintenance program managed by family with of treatment is not easy to predict check-ups by clinician over a period of 1 year General Characterization of Methods Clinician trains parent to administer Clinician teaches child an individualized set of praise and corrections in structured and “rules” designed to change stuttering to fluent unstructured daily situations; clinician speech; once learned, these rules are used in discusses child's progress as measured by conversation in various games and activities; parent's daily severity ratings and clinician uses praise and correction to shape the clinician's assessment of child's %SS in child's speech output clinic Managing stuttering and improveing communication and social interactions. Effective communication and good quality of life School-age children who stutter; may be adopted Older children and adolescents (roughly 9 to 14 School-age children from 7 to 17 years for children with concomitant disorders years old) old Intensive version: may be group or individual; Treatment sessions can be individual or clinician teaches speech pattern and gives group depending on what suits child; for feedback; home version: individual, with parent all children, meeting in group with others guided by weekly visits with clinician who stutter is encouraged Clinician uses behavioral techniques to train child in smooth speech pattern at gradually increasing rates while maintaining fluency; behavior shaping is also used to help client transfer and maintain fluency No special equipment is needed, although video recording and playback can be used to help child explore his or her stuttering May be once or twice weekly; may be beneficial to have more frequent sessions at beginning of therapy A combination of behavioral, cognitive, and affective treatment is used; there is emphasis on making stuttering less severe and helping child communicate despite residual stuttering
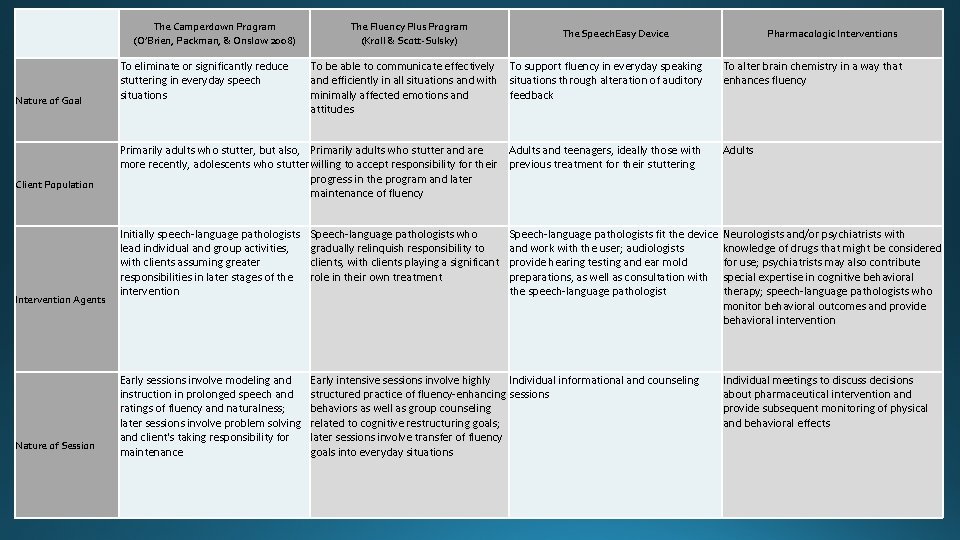
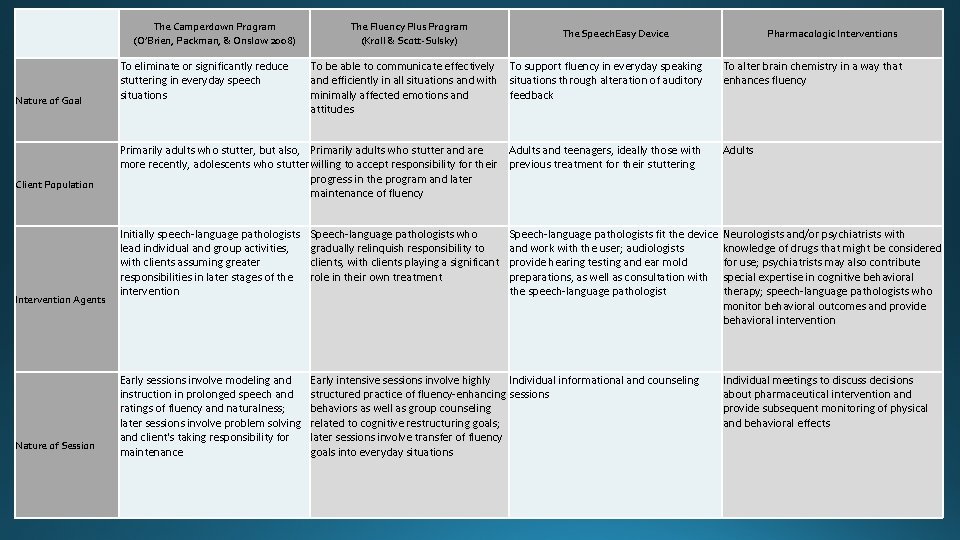
The Camperdown Program (O’Brien, Packman, & Onslow 2008) Nature of Goal Client Population Intervention Agents Nature of Session To eliminate or significantly reduce stuttering in everyday speech situations The Fluency Plus Program (Kroll & Scott-Sulsky) The Speech. Easy Device To be able to communicate effectively To support fluency in everyday speaking and efficiently in all situations and with situations through alteration of auditory minimally affected emotions and feedback attitudes Primarily adults who stutter, but also, Primarily adults who stutter and are Adults and teenagers, ideally those with more recently, adolescents who stutter willing to accept responsibility for their previous treatment for their stuttering progress in the program and later maintenance of fluency Initially speech-language pathologists lead individual and group activities, with clients assuming greater responsibilities in later stages of the intervention Speech-language pathologists who gradually relinquish responsibility to clients, with clients playing a significant role in their own treatment Early sessions involve modeling and instruction in prolonged speech and ratings of fluency and naturalness; later sessions involve problem solving and client's taking responsibility for maintenance Early intensive sessions involve highly Individual informational and counseling structured practice of fluency-enhancing sessions behaviors as well as group counseling related to cognitive restructuring goals; later sessions involve transfer of fluency goals into everyday situations Pharmacologic Interventions To alter brain chemistry in a way that enhances fluency Adults Speech-language pathologists fit the device Neurologists and/or psychiatrists with and work with the user; audiologists knowledge of drugs that might be considered provide hearing testing and ear mold for use; psychiatrists may also contribute preparations, as well as consultation with special expertise in cognitive behavioral the speech-language pathologist therapy; speech-language pathologists who monitor behavioral outcomes and provide behavioral intervention Individual meetings to discuss decisions about pharmaceutical intervention and provide subsequent monitoring of physical and behavioral effects
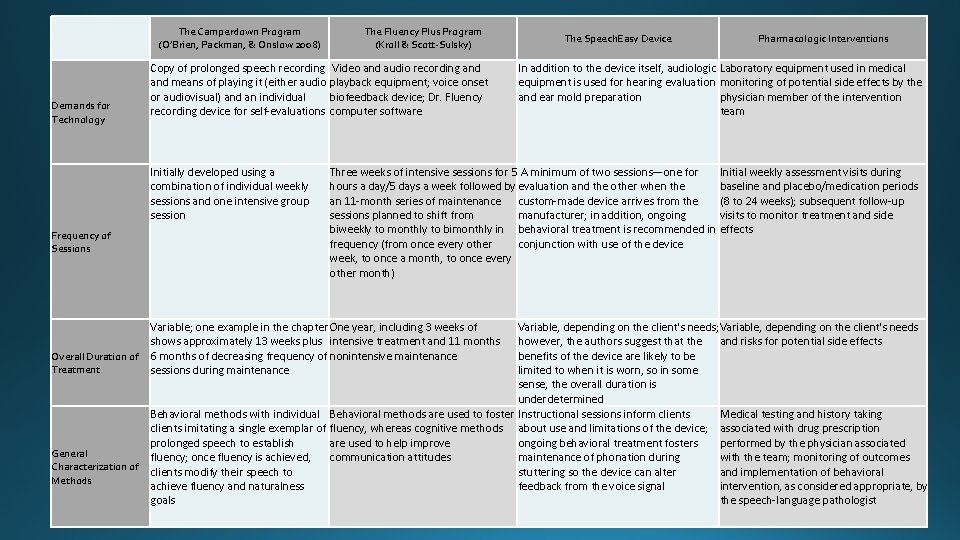
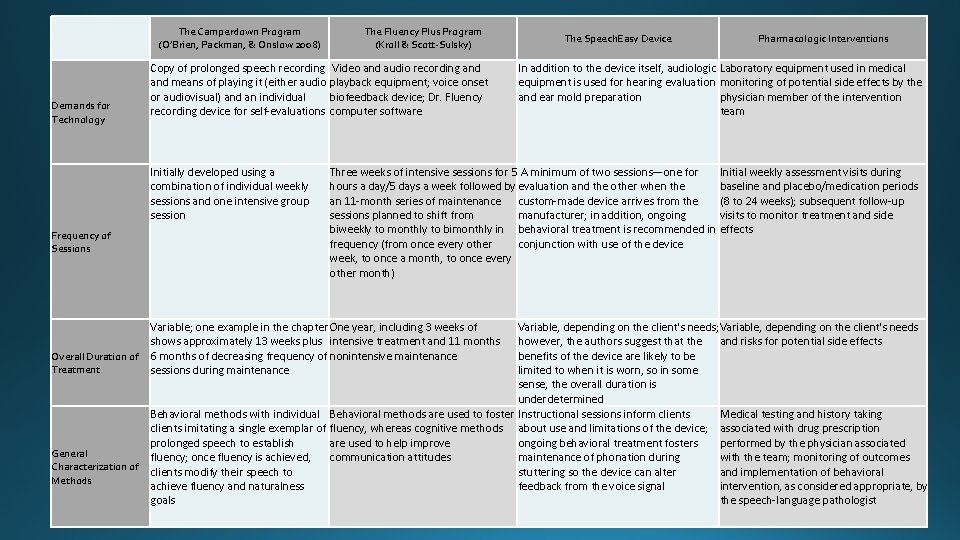
The Camperdown Program (O’Brien, Packman, & Onslow 2008) Demands for Technology Copy of prolonged speech recording Video and audio recording and means of playing it (either audio playback equipment; voice onset or audiovisual) and an individual biofeedback device; Dr. Fluency recording device for self-evaluations computer software Initially developed using a combination of individual weekly sessions and one intensive group session Frequency of Sessions The Fluency Plus Program (Kroll & Scott-Sulsky) The Speech. Easy Device Pharmacologic Interventions In addition to the device itself, audiologic Laboratory equipment used in medical equipment is used for hearing evaluation monitoring of potential side effects by the and ear mold preparation physician member of the intervention team Three weeks of intensive sessions for 5 A minimum of two sessions—one for Initial weekly assessment visits during hours a day/5 days a week followed by evaluation and the other when the baseline and placebo/medication periods an 11 -month series of maintenance custom-made device arrives from the (8 to 24 weeks); subsequent follow-up sessions planned to shift from manufacturer; in addition, ongoing visits to monitor treatment and side biweekly to monthly to bimonthly in behavioral treatment is recommended in effects frequency (from once every other conjunction with use of the device week, to once a month, to once every other month) Variable; one example in the chapter One year, including 3 weeks of shows approximately 13 weeks plus intensive treatment and 11 months Overall Duration of 6 months of decreasing frequency of nonintensive maintenance Treatment sessions during maintenance Variable, depending on the client's needs; Variable, depending on the client's needs however, the authors suggest that the and risks for potential side effects benefits of the device are likely to be limited to when it is worn, so in some sense, the overall duration is underdetermined Behavioral methods with individual Behavioral methods are used to foster Instructional sessions inform clients Medical testing and history taking clients imitating a single exemplar of fluency, whereas cognitive methods about use and limitations of the device; associated with drug prescription prolonged speech to establish are used to help improve ongoing behavioral treatment fosters performed by the physician associated General fluency; once fluency is achieved, communication attitudes maintenance of phonation during with the team; monitoring of outcomes Characterization of clients modify their speech to stuttering so the device can alter and implementation of behavioral Methods achieve fluency and naturalness feedback from the voice signal intervention, as considered appropriate, by goals the speech-language pathologist

 Unstandardized coefficients
Unstandardized coefficients Tes standar adalah
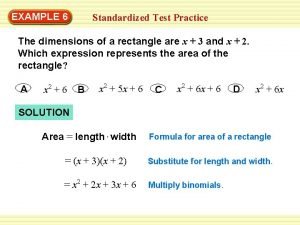
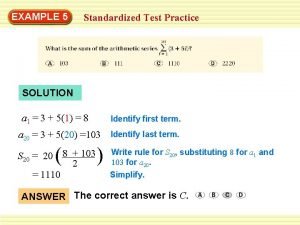
Tes standar adalah Circuit training standardized test prep answers
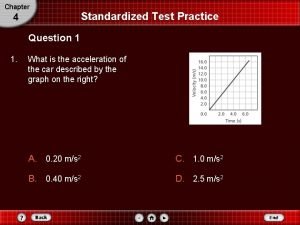
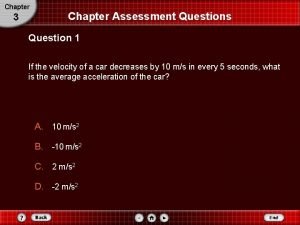
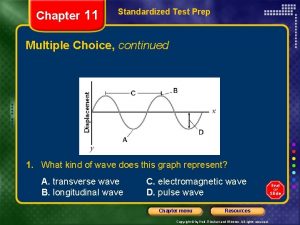
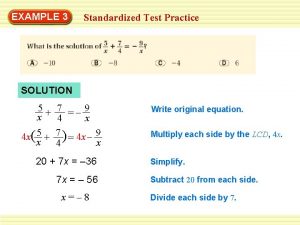
Circuit training standardized test prep answers 4-5 standardized test prep
4-5 standardized test prep A rock climber's shoe loosens a rock and her climbing buddy
A rock climber's shoe loosens a rock and her climbing buddy Chapter 21 standardized test practice answers
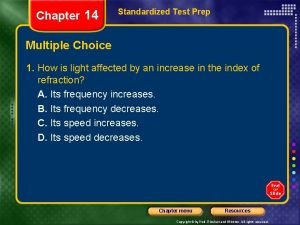
Chapter 21 standardized test practice answers Chapter 14 standardized test practice answers
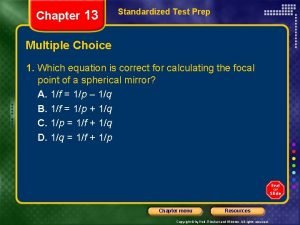
Chapter 14 standardized test practice answers Chapter 13 standardized test practice answers
Chapter 13 standardized test practice answers 10-6 standardized test prep answers
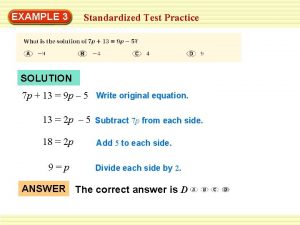
10-6 standardized test prep answers Chapter 2 standardized test practice answers
Chapter 2 standardized test practice answers Chapter 19 standardized test practice answers
Chapter 19 standardized test practice answers Define standardized test
Define standardized test 7-3 standardized test prep
7-3 standardized test prep A rock climber's shoe loosens a rock and her climbing buddy
A rock climber's shoe loosens a rock and her climbing buddy Standardized test characteristics
Standardized test characteristics Non standard test
Non standard test 7-4 standardized test prep
7-4 standardized test prep 6 standardized test practice
6 standardized test practice 5-1 standardized test prep
5-1 standardized test prep 3-5 standardized test prep
3-5 standardized test prep Self initiated other repair
Self initiated other repair Voting districts definition ap human geography
Voting districts definition ap human geography Acquisition, fluency maintenance generalization examples
Acquisition, fluency maintenance generalization examples Stages of language development
Stages of language development Sentence fluency is
Sentence fluency is Woodcock johnson iv subtests
Woodcock johnson iv subtests