Finding the Positives from Never Events Judith Connor






- Slides: 29
Finding the Positives from Never Events Judith Connor Assistant Director Quality Assurance South Tees Hospitals NHS FT Delcy Wells Patient Safety Lead County Durham & Darlington NHS FT
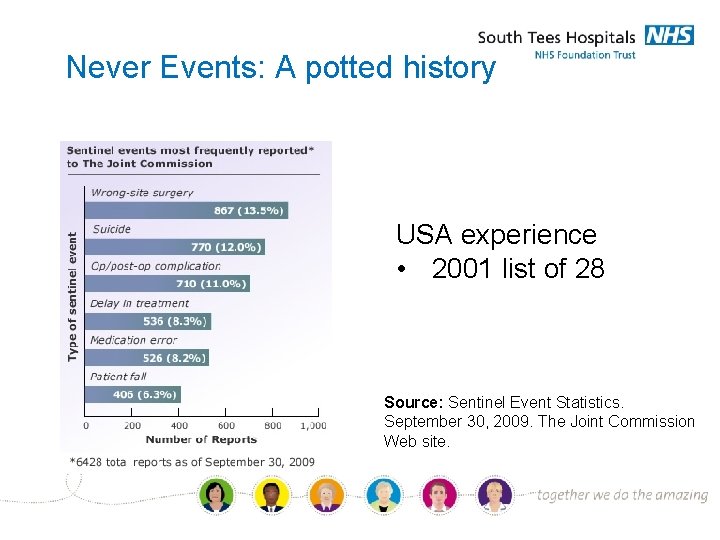
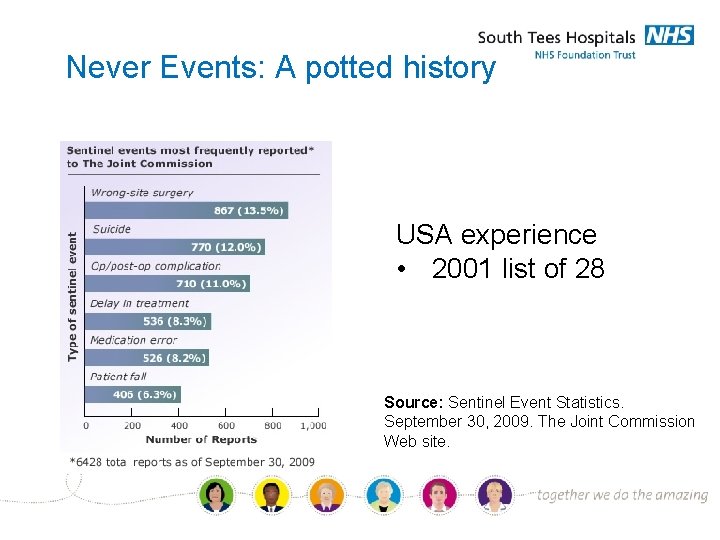
Never Events: A potted history USA experience • 2001 list of 28 Source: Sentinel Event Statistics. September 30, 2009. The Joint Commission Web site.
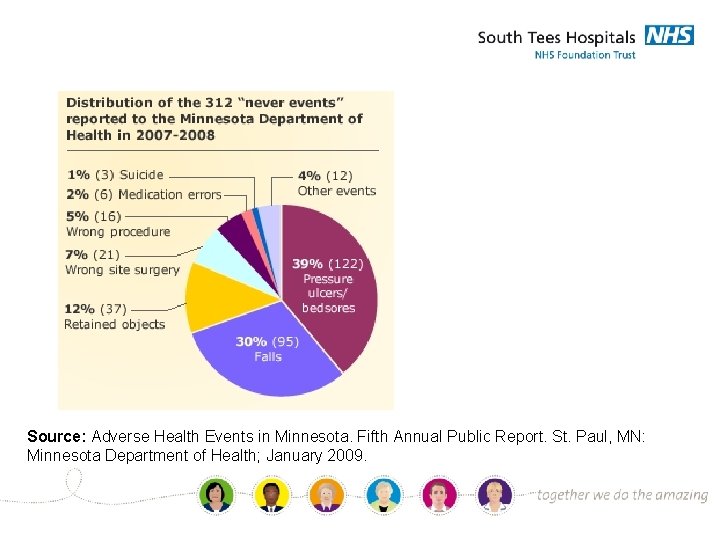
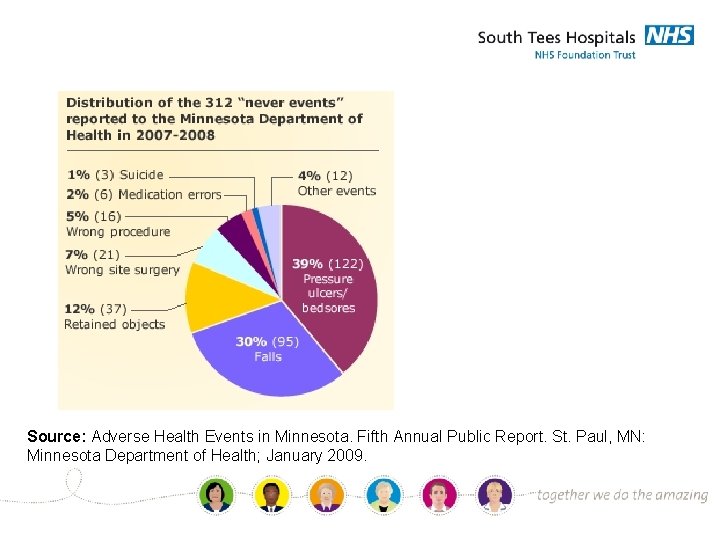
Source: Adverse Health Events in Minnesota. Fifth Annual Public Report. St. Paul, MN: Minnesota Department of Health; January 2009.
The National Patient Safety Agency produced a list of 8 core never events in March 2009: • • wrong site surgery; retained instrument post-operation; wrong route administration of chemotherapy; misplaced naso or orogastric tube not detected prior to use; inpatient suicide using non-collapsible rails; escape from within the secure perimeter of medium or high security mental health services by patients who are transferred prisoners; in-hospital maternal death from post-partum haemorrhage after elective caesarean section; Intravenous administration of mis-selected concentrated potassium chloride. Guidance on implementing the never events framework. Health Service Journal. 15 May 2009
Context • 4. 6 million hospital admissions that lead to surgical • • care every year in England 500, 000 non-Caesarian births also tens of thousands of other interventional procedures like internal radiology and cardiology catheter procedures that are also classified as “surgical” in terms of never events. incidence rate is less than 0. 005% or 1 never event in every 20, 000 procedures.
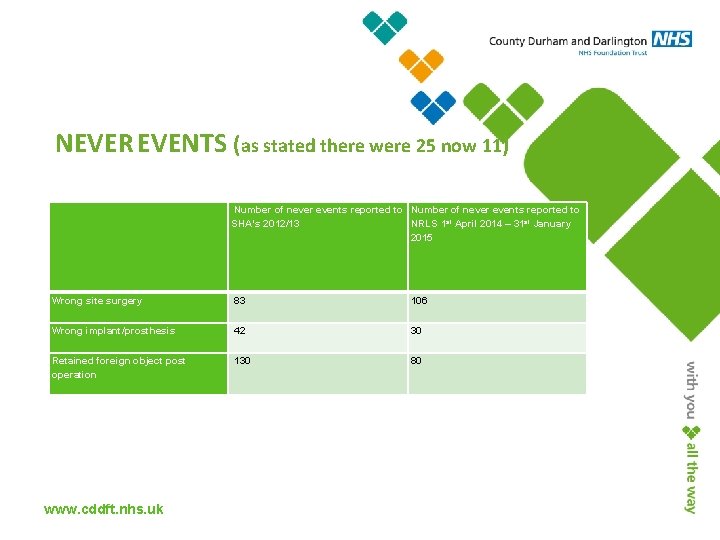
Never Events in England • List increased to 25 in 2013 • Surgical Never events task force Feb • • 2014 New Never Events Policy and Framework published March 27 th 2015 List decreased to 11 categories.
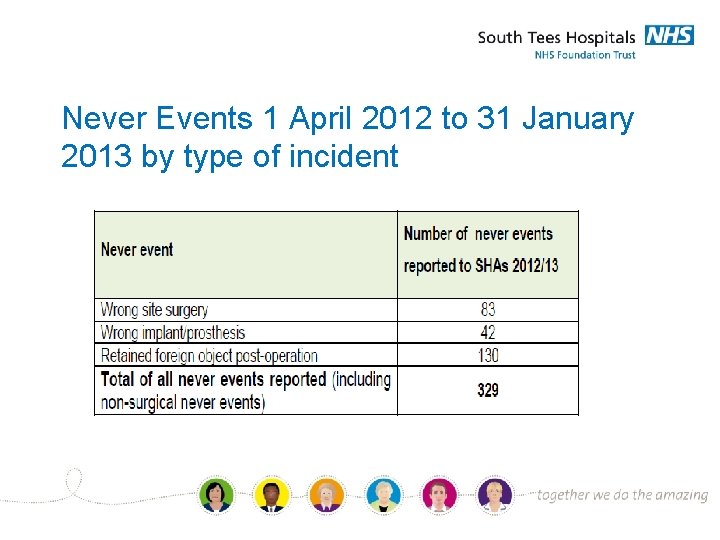
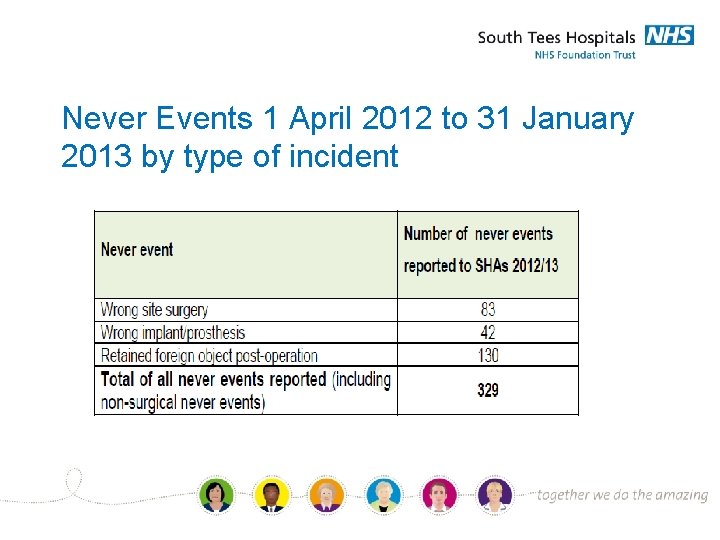
Never Events 1 April 2012 to 31 January 2013 by type of incident
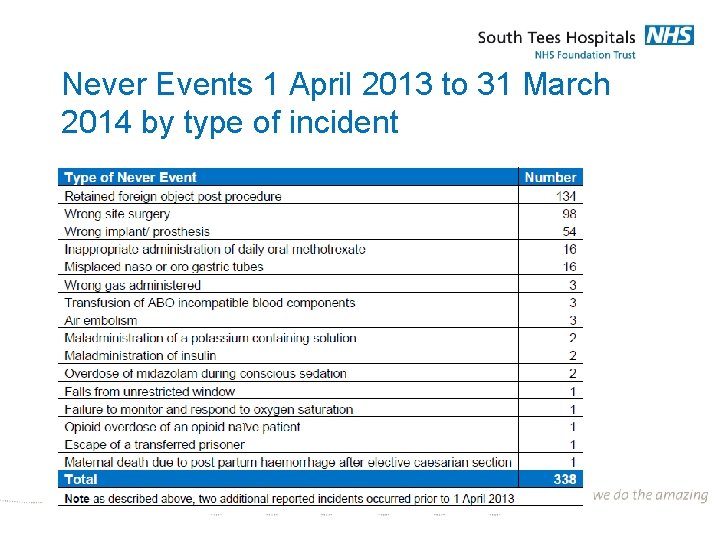
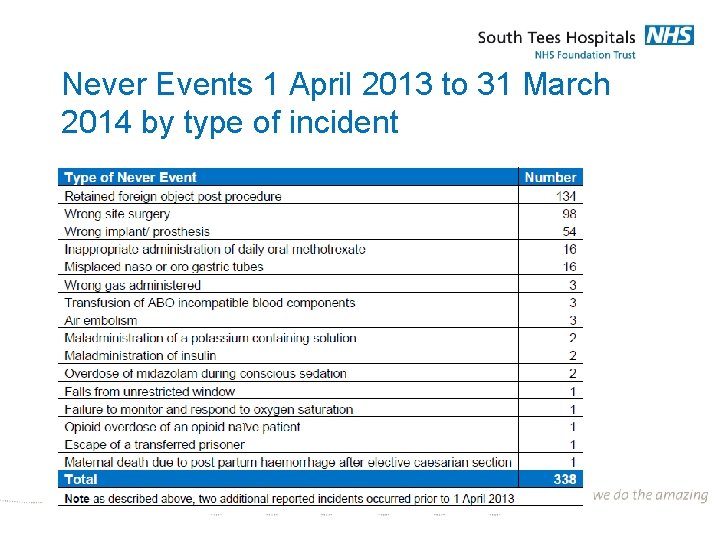
Never Events 1 April 2013 to 31 March 2014 by type of incident
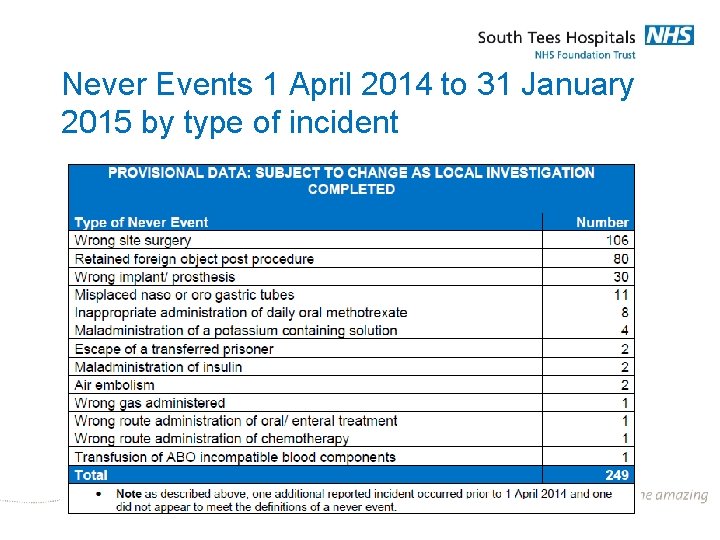
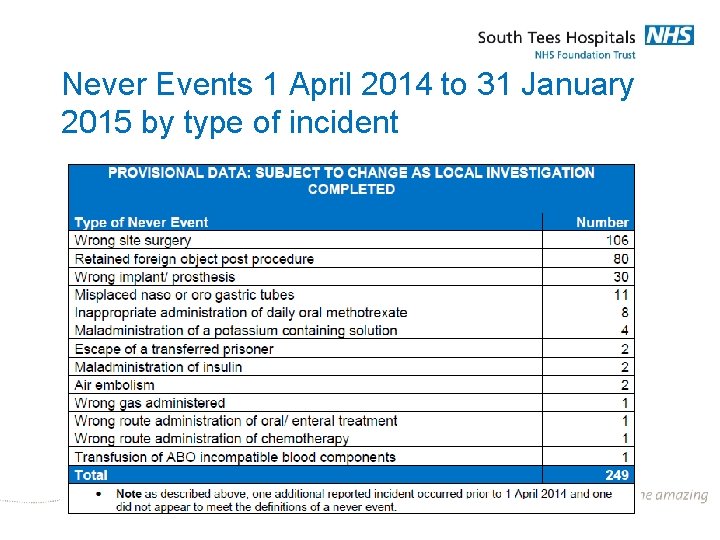
Never Events 1 April 2014 to 31 January 2015 by type of incident
Number of never events relating to surgical error • 12/13 255 • 13/14 286 • 14/15 216 What are we learning?
Insertion of wrong size intraocular lens Never Event Category: Wrong Implant Previous Medical History • The patient has type II diabetes resulting in co-existing diabetic retinopathy. • Previous left cataract surgery, rationale for surgery relates to intermittent pain and blurs, poor vision - right eye. Reason for admission • Right cataract surgery with intraocular lens implant. What happened • The wrong size diopter lens was inserted into the right eye. This was recognised before the patient left theatre and the lens was removed. No other lens was inserted due to the cornea being cloudy.
Impact on the individual The patient was temporarily left with poor vision due to no alternative lens inserted which would impact on their day to day activities. Patient requires further surgery to right eye to insert correct size diopter lens. Prognosis It is anticipated following insertion of correct lens that the prognosis would be as previously expected.
Action Taken Immediately Following Incident Operating consultant sought further advice from a consultant colleague who attended to assist with removal of the lens. The lens was removed from the patient’s right eye. The correct lens was not inserted because the cornea was cloudy. The plan of action was to review the patient in outpatients and arrange for further surgery when appropriate. Proposed actions included: • Ophthalmic Surgical Safety Checklist – draft amendments made for approval and subsequent implementation on both sites. • Standard Operating Procedure has been produced in draft format for approval and subsequent implementation on both sites.
Root causes: • Misinterpretation of the surgeon’s handwriting in the patient’s notes by the nursing staff • Failure to cross check IOL power gleaned from notes with information on theatre list. • Lack of pre-operative briefing which inhibited an opportunity to confirm the diopter size. • lack of written IOL power and style on whiteboard
Lessons learned • The surgeon delegated the identification of the power of the IOL in the case records to a circulating nurse • Handwritten IOL power can be mis-interpreted especially if read by a third party • The IOL power and style was not transferred to theatre whiteboard • Theatre nursing staff did not cross-check the IOL power with the printed theatre list
• Because it was not written on theatre whiteboard, there was no immediate way to check the IOL power immediately prior to insertion. • There was no pre-operative briefing prior to this procedure. • Staff did not challenge practice which they felt was not conducive to their working environment/practice (dimming of lights throughout the procedure, checking patient notes for diopter lens size).
Was this a system error or human error?
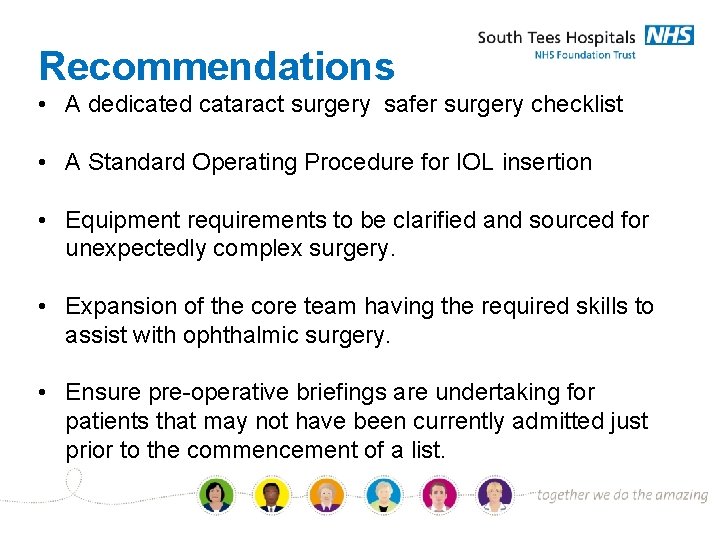
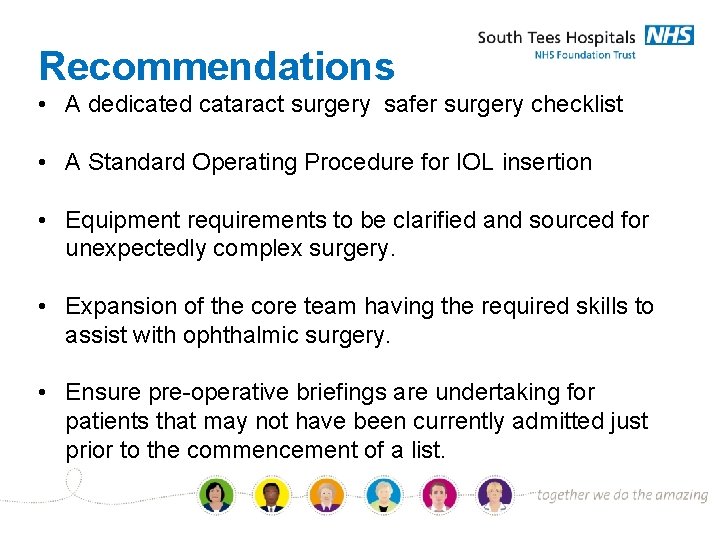
Recommendations • A dedicated cataract surgery safer surgery checklist • A Standard Operating Procedure for IOL insertion • Equipment requirements to be clarified and sourced for unexpectedly complex surgery. • Expansion of the core team having the required skills to assist with ophthalmic surgery. • Ensure pre-operative briefings are undertaking for patients that may not have been currently admitted just prior to the commencement of a list.
Solutions: Human vs System Will they address the issues?
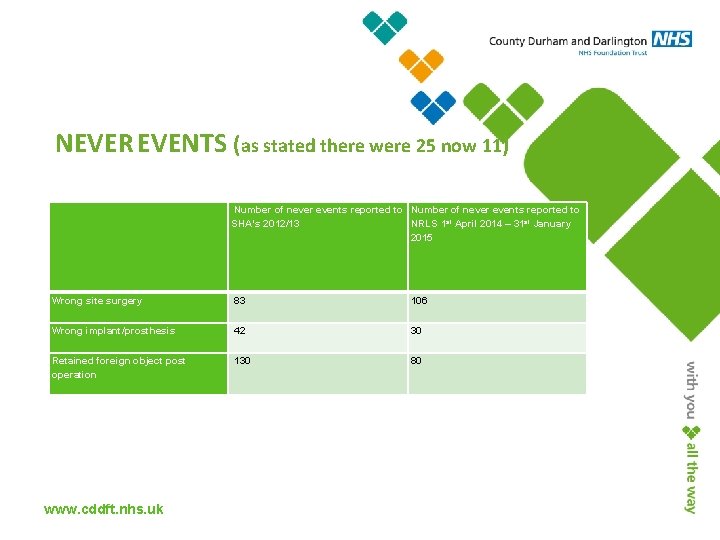
NEVER EVENTS (as stated there were 25 now 11) Number of never events reported to SHA’s 2012/13 NRLS 1 st April 2014 – 31 st January 2015 Wrong site surgery 83 106 Wrong implant/prosthesis 42 30 Retained foreign object post operation 130 80 The Clinical & Quality Strategy www. cddft. nhs. uk

Never Events The Trust had 1 never event for 2013/14 (guidewire) reported on STEIS 22/11/2013 and then 3 never events for 2014/15 Focus on retained foreign objects post procedure as we had 2 from maternity services reported on STEIS 29/8/2014 and 5/3/2015. Our 3 rd was similar to South Tees as it was an ophthalmic lens never event that was in the patient for 7 minutes before being removed as it was the wrong lens for this patient reported on STEIS 12/6/2014. www. cddft. nhs. uk
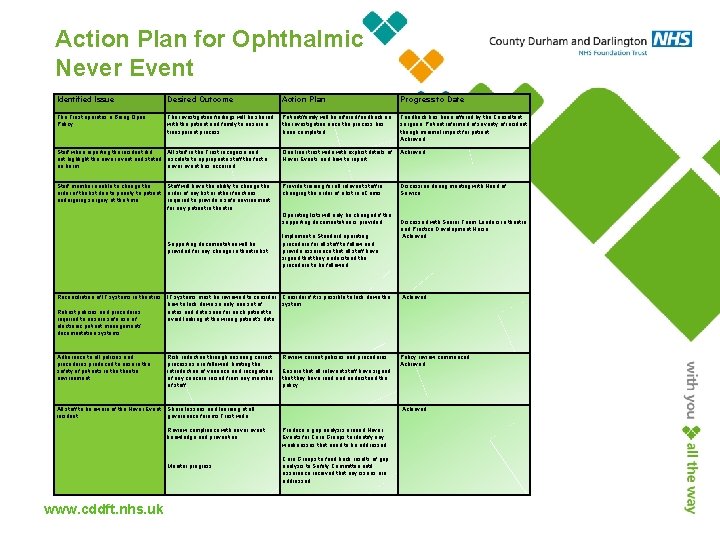
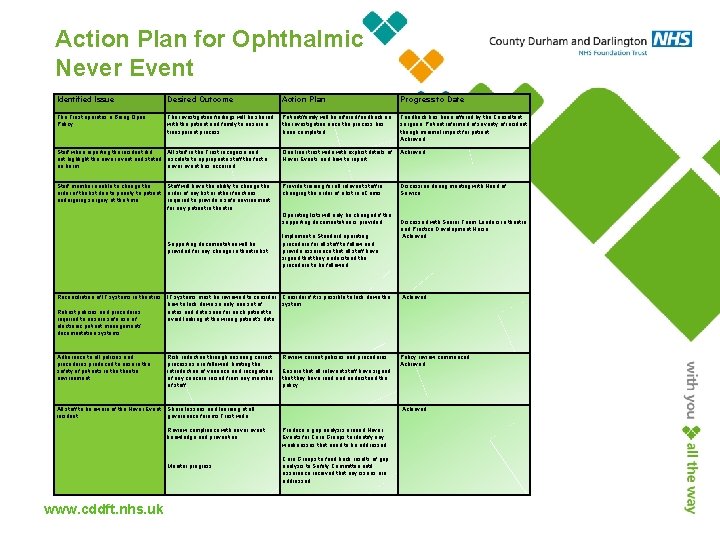
Action Plan for Ophthalmic Never Event Identified Issue Desired Outcome Action Plan Progress to Date The Trust operates a Being Open Policy The investigation findings will be shared with the patient and family to ensure a transparent process. Patient/family will be offered feedback on the investigation once the process has been completed. Feedback has been offered by the Consultant surgeon. Patient informed of severity of incident though minimal impact for patient. Achieved Staff when reporting the incident did All staff in the Trust recognise and not highlight the never event and stated escalate to appropriate staff the fact a no harm never event has occurred. One liner trust wide with explicit details of Never Events and how to report. Achieved Staff member unable to change the Staff will have the ability to change the order of the list due to priority to patient order of any list or other functions undergoing surgery at the time. required to provide a safe environment for any patient in theatre. Supporting documentation will be provided for any change in theatre list Provide training for all relevant staff in changing the order of a list in e. Camis. Operating lists will only be changed if the supporting documentation is provided Implement a Standard operating procedure for all staff to follow and provide assurance that all staff have signed that they understand the procedure to be followed Discussion during meeting with Head of Service. Discussed with Senior Team Leaders in theatre and Practice Development Nurse. Achieved Reconciliation of IT systems in theatres Robust policies and procedures required to ensure safe use of electronic patient management/ documentation systems IT systems must be reviewed to consider Consider if it is possible to lock down the how to lock down so only one set of system notes and data seen for each patient to avoid looking at the wrong patient’s data. Achieved Adherence to all policies and procedures produced to ensure the safety of patients in theatre environment. Risk reduction through ensuring correct processes are followed, limiting the introduction of variance and recognition of any concern raised from any member of staff. Review current policies and procedures. Ensure that all relevant staff have signed that they have read and understood the policy Policy review commenced. Achieved All staff to be aware of the Never Event incident. Share lessons and learning at all governance forums Trust wide Review compliance with never event knowledge and prevention Monitor progress Produce a gap analysis around Never Events for Care Groups to identify any weaknesses that need to be addressed Care Groups to feed back results of gap analysis to Safety Committee until assurance received that any issues are addressed Achieved www. cddft. nhs. uk
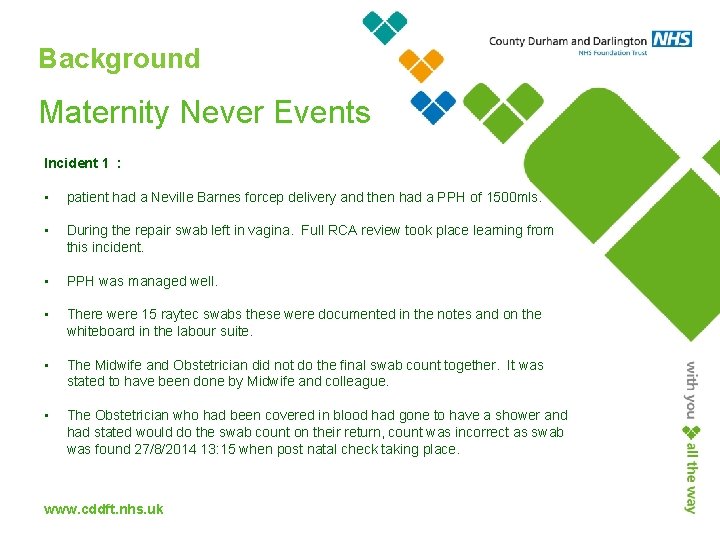
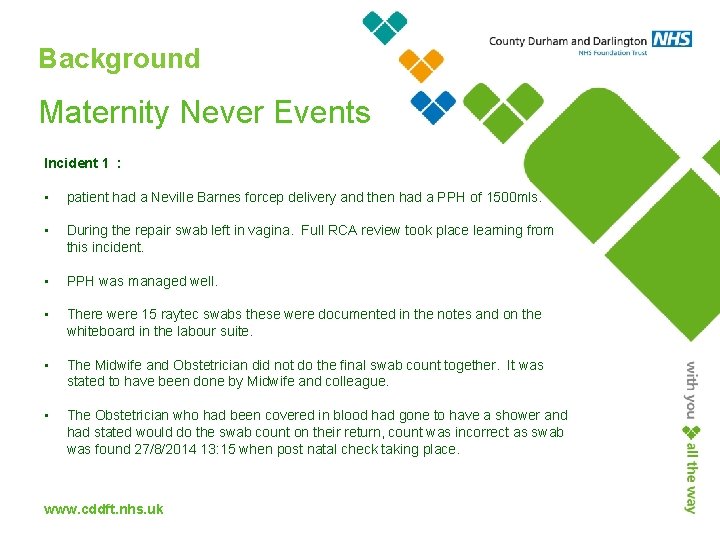
Background Maternity Never Events Incident 1 : • • patient had a Neville Barnes forcep delivery and then had a PPH of 1500 mls. • PPH was managed well. • There were 15 raytec swabs these were documented in the notes and on the whiteboard in the labour suite. • The Midwife and Obstetrician did not do the final swab count together. It was stated to have been done by Midwife and colleague. • The Obstetrician who had been covered in blood had gone to have a shower and had stated would do the swab count on their return, count was incorrect as swab was found 27/8/2014 13: 15 when post natal check taking place. During the repair swab left in vagina. Full RCA review took place learning from this incident. www. cddft. nhs. uk

Maternity Never Events Incident 2 : • patient had a forcep delivery in theatre and sustained a 3 rd degree tear during suturing stated 2 swabs placed in vagina to stop bleeding - the full RCA has not been completed as yet so full outcome cannot be shared. www. cddft. nhs. uk
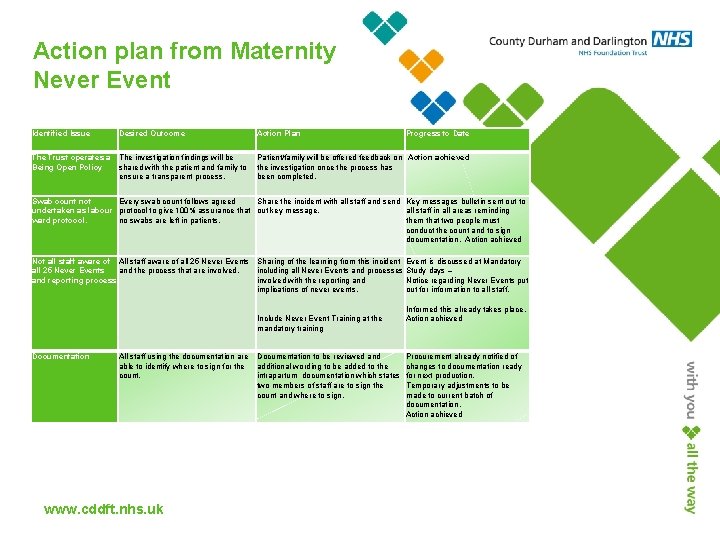
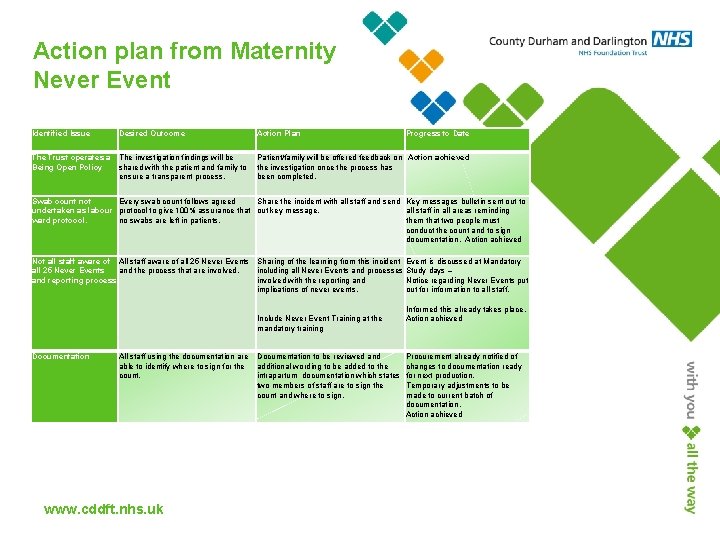
Action plan from Maternity Never Event Identified Issue Desired Outcome Action Plan Progress to Date The Trust operates a The investigation findings will be Patient/family will be offered feedback on Action achieved Being Open Policy shared with the patient and family to the investigation once the process has ensure a transparent process. been completed. Swab count not Every swab count follows agreed Share the incident with all staff and send Key messages bulletin sent out to undertaken as labour protocol to give 100% assurance that out key message. all staff in all areas reminding ward protocol. no swabs are left in patients. them that two people must conduct the count and to sign documentation. Action achieved Not all staff aware of All staff aware of all 25 Never Events Sharing of the learning from this incident Event is discussed at Mandatory all 25 Never Events and the process that are involved. including all Never Events and processes Study days – and reporting process involved with the reporting and Notice regarding Never Events put implications of never events. out for information to all staff. Informed this already takes place. Include Never Event Training at the Action achieved mandatory training Documentation All staff using the documentation are Documentation to be reviewed and able to identify where to sign for the additional wording to be added to the count. intrapartum documentation which states two members of staff are to sign the count and where to sign. www. cddft. nhs. uk Procurement already notified of changes to documentation ready for next production. Temporary adjustments to be made to current batch of documentation. Action achieved

Sign up to Safety Pledges Never Event All never events have been reviewed and extra controls put in place with the aim to prevent them taking place. Discussion at team meetings, governance meetings across the whole Trust has taken place to highlight what a never event is, how to report and consider how or what further controls need to be in place to prevent. Under collaboration this Trust stated it would share lessons learnt with regional workstreams. www. cddft. nhs. uk

From 1 st April 2015 new never event list 2015/16 and new SI policy – please go to the website and read. All staff should remember there are financial penalties, damage of Trust reputation as well as the risk of harming a patient when a never event takes place. www. cddft. nhs. uk

County Durham & Darlington have agreed to take part in national research with the aim to prevent retained swabs from maternity cases. Discussed was the use of separate theatre staff to maternity as behavioural and culture different within obstetric theatres and main theatres. Again solution Human v Systems we can have all the policies and SOPs but if humans don’t follow them we could have another Never Event. Integrating Human Factors into Healthcare should be mandatory as optimising human performance by better understanding the behaviour of individuals, their interactions with each other and within the environment. In November 2013 the National Quality Board raised a concordat which aims to provide leadership and oversight for embedding Human Factors principles and practices into the healthcare system. www. cddft. nhs. uk

Finding the Positive from Never Events Improvements are being made and reductions occurring. Transparency and Duty of Candour being followed gives the general public assurance we are aiming to improve quality in the NHS all the time. www. cddft. nhs. uk