Enhanced Medical Assistant Role Implementing an Expanded Role
- Slides: 43
Enhanced Medical Assistant Role – Implementing an Expanded Role in an Emerging Model of Care Peter Harper, MD, MPH Kristi Van Riper, MPH, CHES
Objectives and a little about us Objectives Verbalize the journey we have taking to develop this emerging model of care Verbalize the new rooming components medical assistants complete for each patient office visit Recognize the improvement methodology used to build this emerging model of care Minneapolis/St. Paul – 4 residency clinics, underserved population and many interpreted visits; Epic is our EMR 2 2
Why is the Enhanced Medical Assistant Role Important? Physician Burnout Family Medicine Capacity Joy of Practice – Sinsky Team-based Care – Bodenheimer Ann Fam Med May/June 2013 vol. 11 no. 3 272 -278 Ann Fam Med March/April 2014 vol. 12 no. 2 166 -171 • • • 3 Unplanned visits Inadequate support Documentation burden EMR push work to physician Poor team function • • • Teamlets – MA/Provider dyad Share the care Standing orders 3
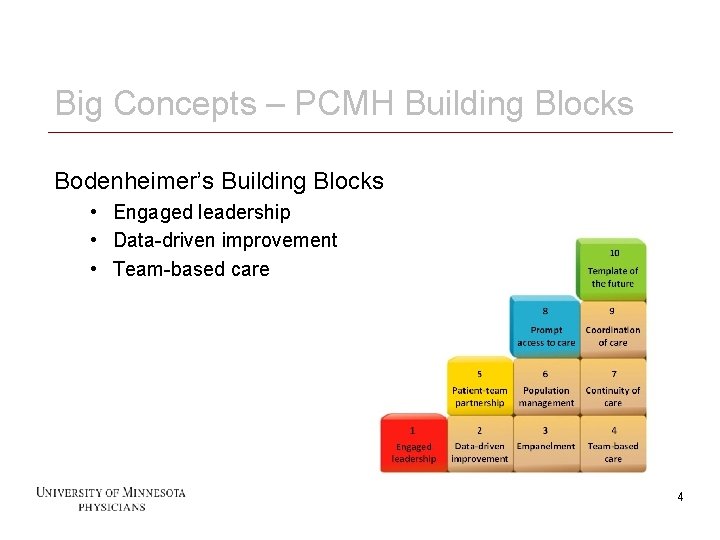
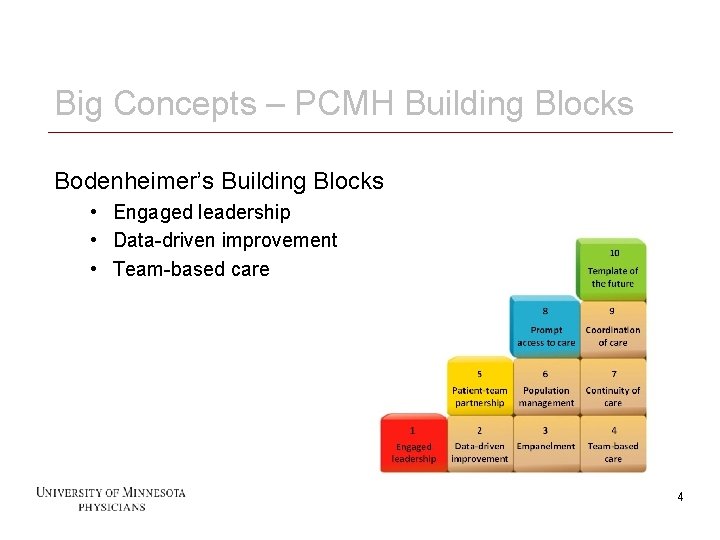
Big Concepts – PCMH Building Blocks Bodenheimer’s Building Blocks • Engaged leadership • Data-driven improvement • Team-based care 4 4
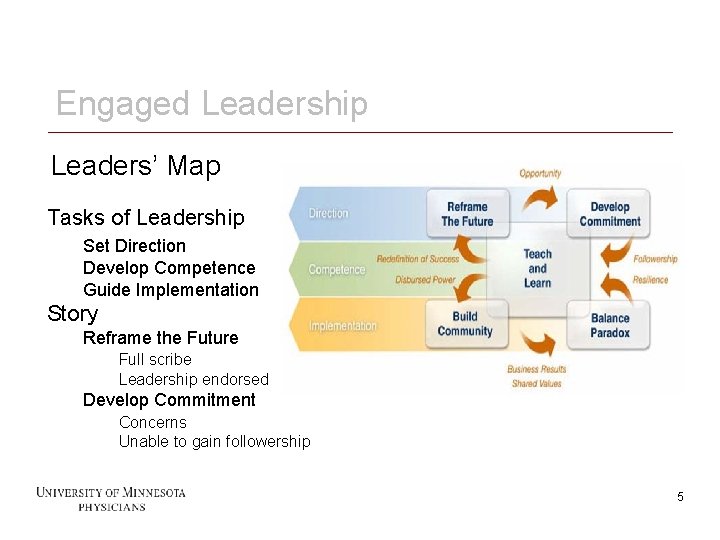
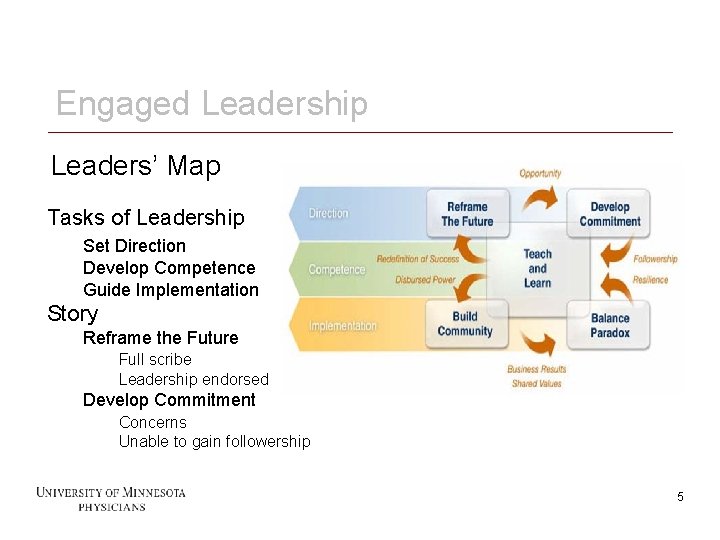
Engaged Leadership Leaders’ Map Tasks of Leadership Set Direction Develop Competence Guide Implementation Story Reframe the Future Full scribe Leadership endorsed Develop Commitment Concerns Unable to gain followership 5 5
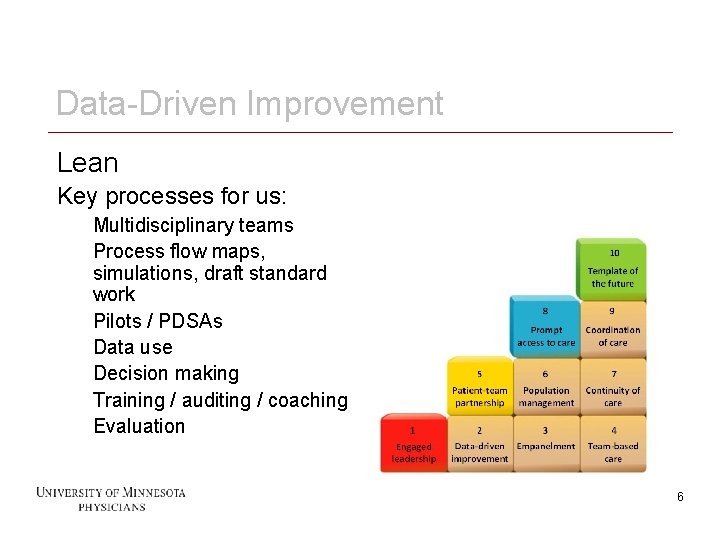
Data-Driven Improvement Lean Key processes for us: Multidisciplinary teams Process flow maps, simulations, draft standard work Pilots / PDSAs Data use Decision making Training / auditing / coaching Evaluation 6 6
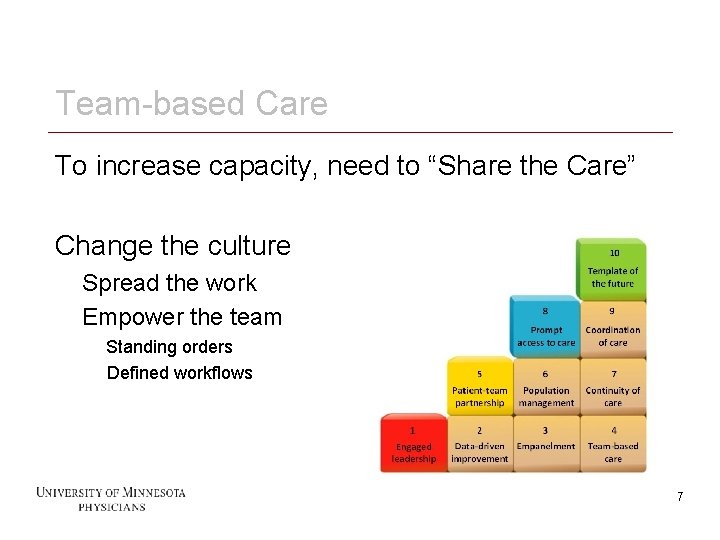
Team-based Care To increase capacity, need to “Share the Care” Change the culture Spread the work Empower the team Standing orders Defined workflows 7 7
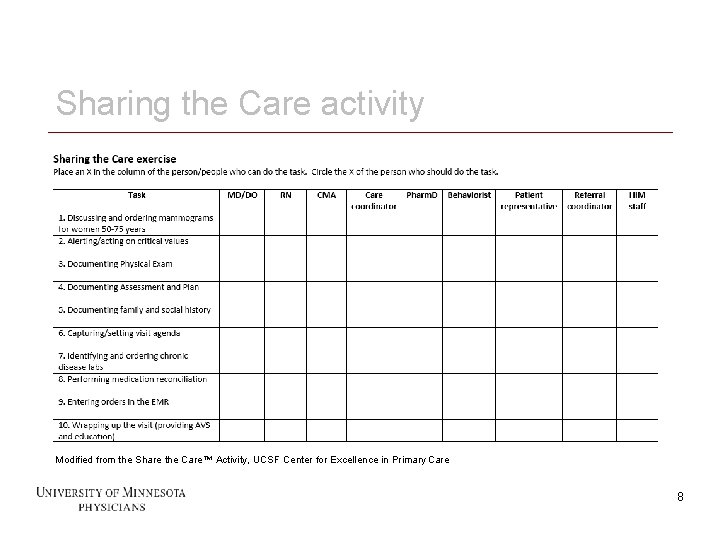
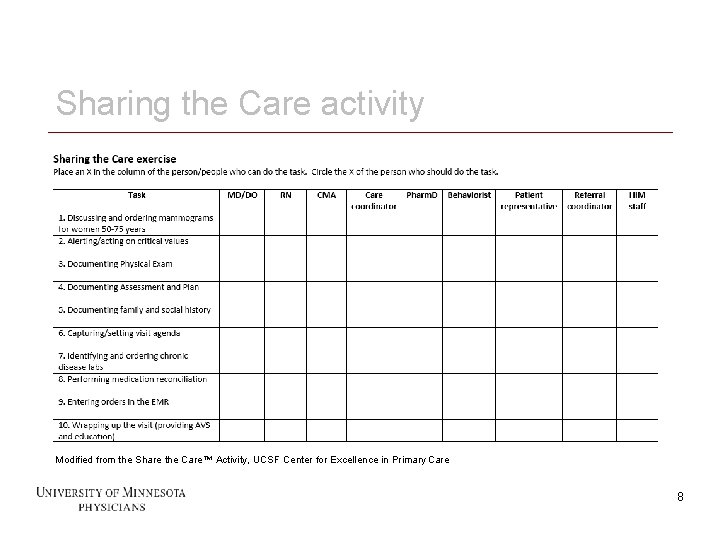
Sharing the Care activity Modified from the Share the Care™ Activity, UCSF Center for Excellence in Primary Care 8 8
What’s next? What did you learn from doing that exercise? Our next step Offload work from providers Shift some ownership to CMA’s 9 9
Enhanced Medical Assistant Role Final model Divided into two sections Step #1: enhanced rooming process Step #2: visit assistant 10 10
Step #1: enhanced rooming process Vitals Family/social history Immunizations Preventive health needs Chronic disease labs Medication reconciliation Agenda capture My. Chart sign-up Hand-off to provider 11 11
Step #2: visit assistant Stay in room for entire visit Upon callout, place orders (with read back) Upon callout, write patient instructions (with read back) **Document portions of visit with templates** **Upon callout, document ROS and PE** Assist with scheduling follow-up/referrals Complete visit wrap-up (after-visit summary) 12 12
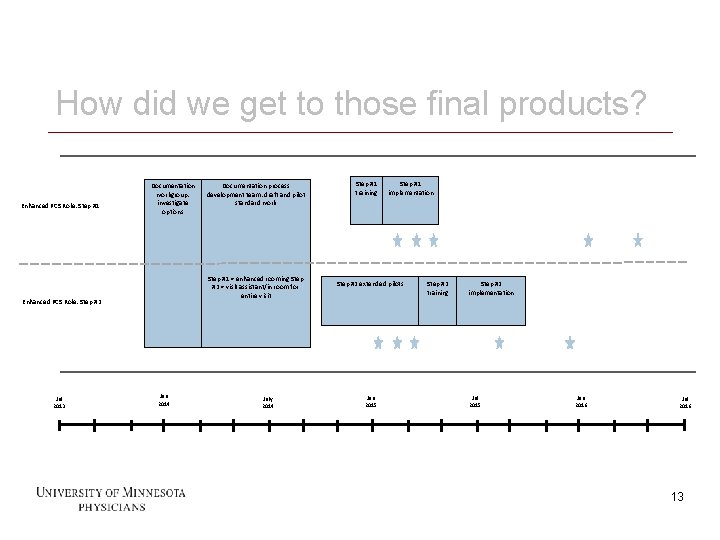
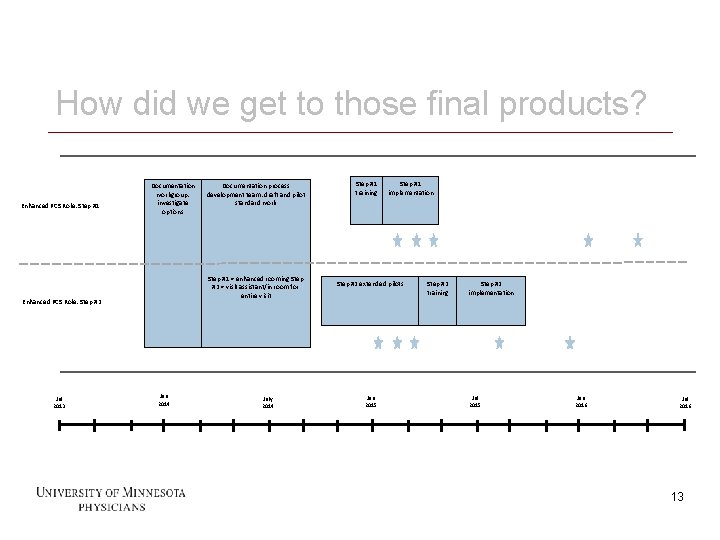
How did we get to those final products? Enhanced PCS Role: Step #1 Documentation workgroup: investigate options Step #1 = enhanced rooming Step #2 = visit assistant/in room for entire visit Enhanced PCS Role: Step #2 Jul 2013 13 Documentation process development team: draft and pilot standard work Jan 2014 July 2014 Step #1 training Step #1 implementation Step #2 extended pilots Jan 2015 Step #2 training Step #2 implementation Jul 2015 Jan 2016 Jul 2016 13
Documentation workgroup Multidisciplinary leadership team to review the 4 options for documentation assistance Pushback from providers about scribing Ultimately decided to proceed with assisting providers with orders and patient instructions 14 14
Documentation process development team One dyad (MD/CMA) from each clinic Drafted, simulated, and revised standard work Piloted it with individual patients Revised standard work again Trained additional PCS and provider (2 PCS working with 1 provider) Piloted with all patients during a clinic shift (1/2 day) PCS = patient care staff (CMA, LPN, RN) 15 15
Outcomes of pilot Divide the standard work into two sections (Step #1 and Step #2) Roll out Step #1 to all immediately Continue extended pilots for Step #2 (spread to more PCS and providers) – hire temps to fill in for PCS doing pilots 16 16
Step #1 implementation (December 2014) Trained all PCS in person Trained providers via written communication Conducted standard work audits Self Peer Supervisor Conducted satisfaction surveys 17 17
Step #2 extended pilot outcomes Mixed satisfaction Do more and will get better Central Leadership Team – spread! 18 18
Step #2 implementation (Summer 2015) Trained all PCS Trained all faculty and Nurse Practitioners Shadow shifts Shifts with already trained Conducted standard work audits Conducted satisfaction surveys 19 19
DATA AND MEASUREMENT 20 20
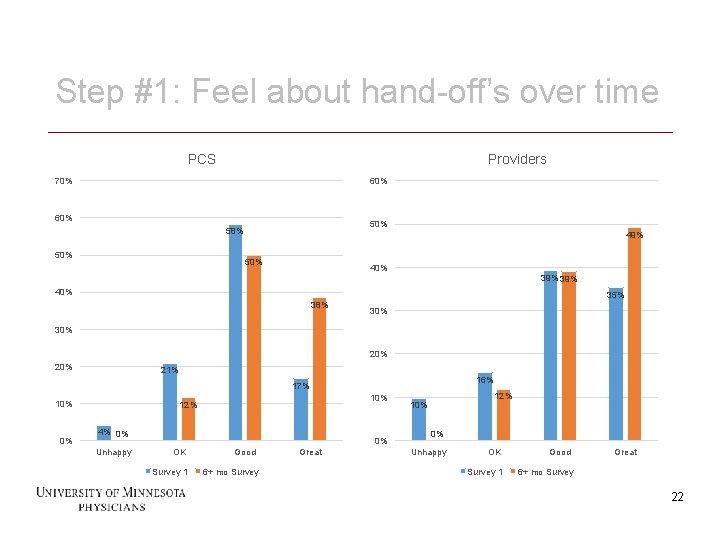
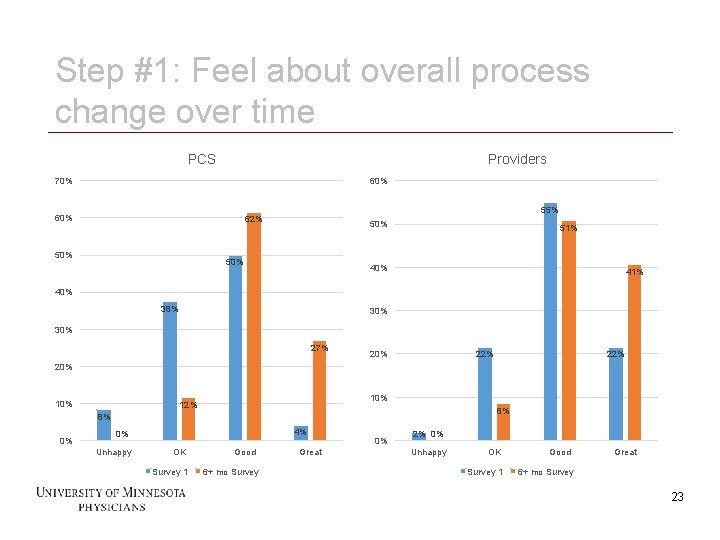
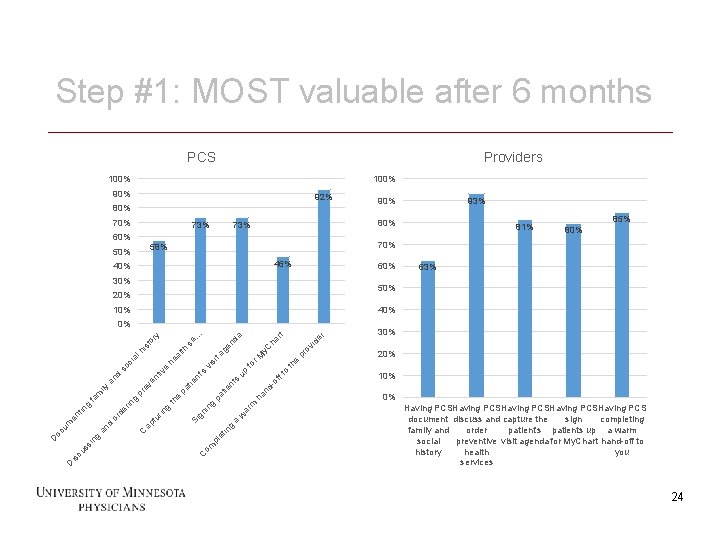
Step #1: Staff/provider satisfaction Feel about hand-off’s (over time) Feel about overall process change (over time) Most valuable (after 6 months) 21 21
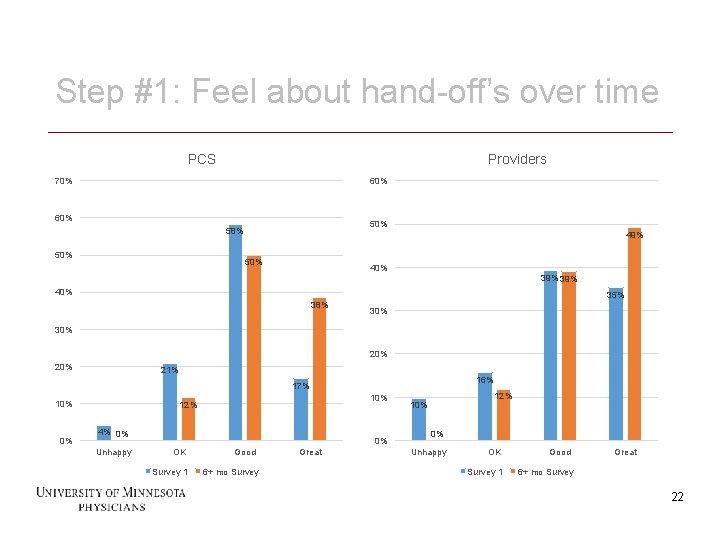
Step #1: Feel about hand-off’s over time PCS Providers 70% 60% 58% 50% 49% 50% 40% 39% 40% 35% 38% 30% 20% 21% 16% 17% 10% 0% 4% 0% Unhappy 0% OK Survey 1 22 10% 12% Good 6+ mo Survey Great 12% 10% 0% Unhappy OK Survey 1 Good Great 6+ mo Survey 22
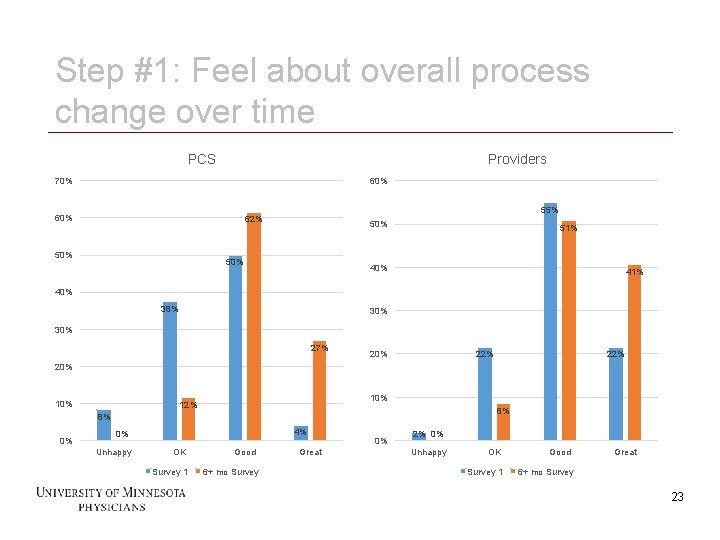
Step #1: Feel about overall process change over time PCS Providers 70% 60% 55% 62% 50% 50% 51% 40% 41% 40% 38% 30% 27% 20% 22% 20% 10% 12% 8% 8% 0% 4% 0% Unhappy OK Survey 1 23 Good 6+ mo Survey Great 0% 2% 0% Unhappy OK Survey 1 Good Great 6+ mo Survey 23
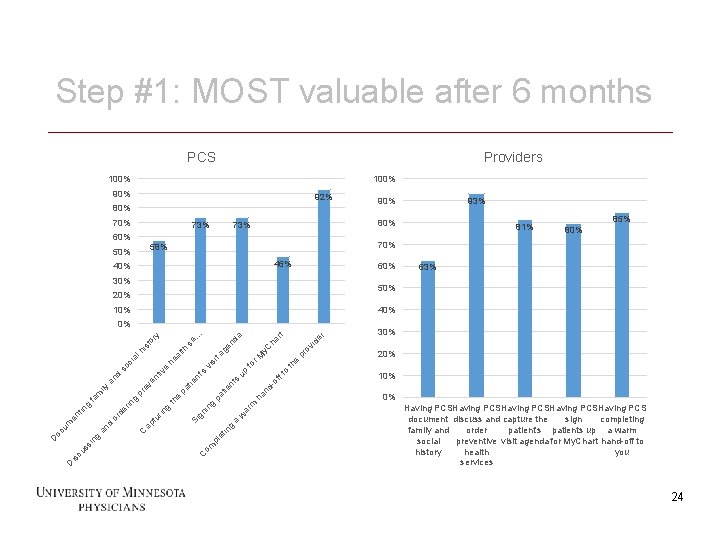
Step #1: MOST valuable after 6 months PCS Providers 100% 90% 92% 80% 73% 60% 46% 40% 60% 30% 10% ov i pr 20% e nd -o ha ar m w a g in et pl om C 30% th ff to up s nt tie pa g gn in Si de r ha rt r. M fo si vi 's nt tie pa e th g rin tu ap C g in ss cu is y. C ge n ta th he al e tiv en ev pr g de rin or d an da se. . . or y st hi al so ci d an ily m fa g tin en um oc D 63% 40% 0% D 85% 80% 50% 24 81% 70% 58% 50% 93% 90% 10% 0% Having PCSHaving PCS document discuss and capture the sign completing family and order patient's patients up a warm social preventive visit agenda for My. Chart hand-off to history health you services 24
Data activity Two groups 25 25
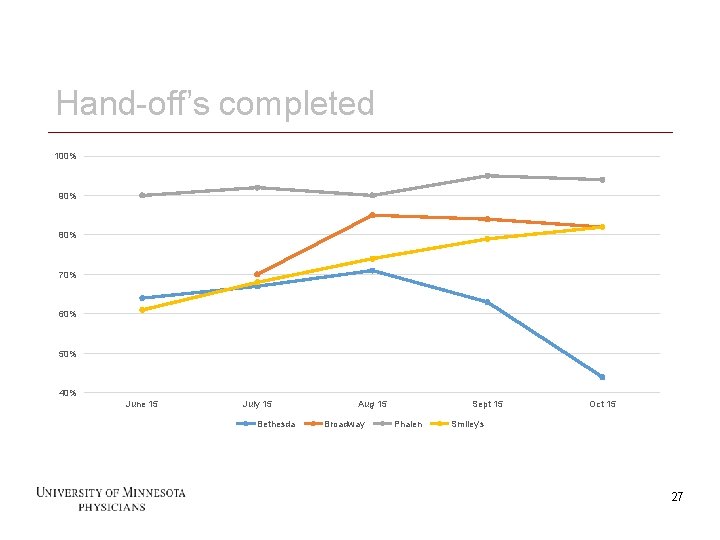
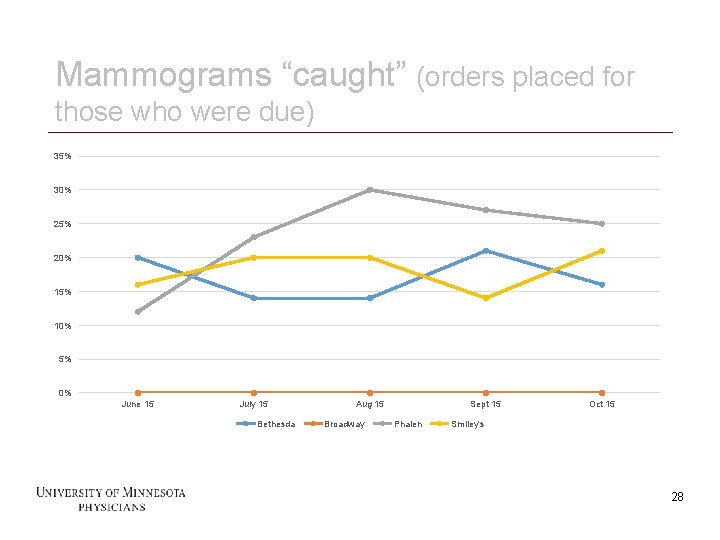
Step #1: Process measures Hand-off’s Mammograms Family/social history – cannot get good data! 26 26
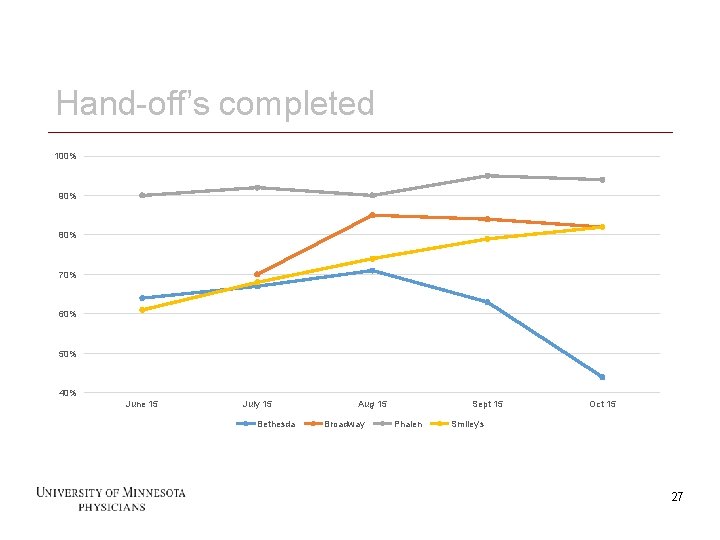
Hand-off’s completed 100% 90% 80% 70% 60% 50% 40% June 15 July 15 Bethesda 27 Aug 15 Broadway Sept 15 Phalen Oct 15 Smiley's 27
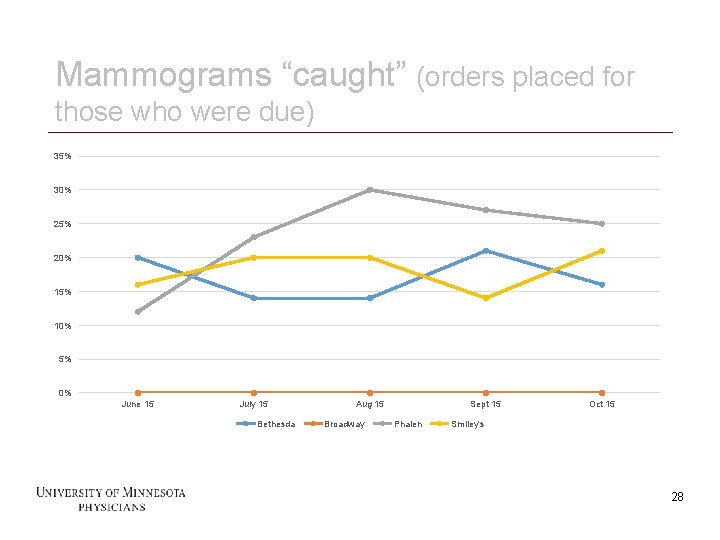
Mammograms “caught” (orders placed for those who were due) 35% 30% 25% 20% 15% 10% 5% 0% June 15 July 15 Bethesda 28 Aug 15 Broadway Sept 15 Phalen Oct 15 Smiley's 28
Step #2: Staff/provider satisfaction Feel about PCS staying in room for visit Feel about PCS completing visit wrap-up Feel about overall process Most valuable after 6 months 29 29
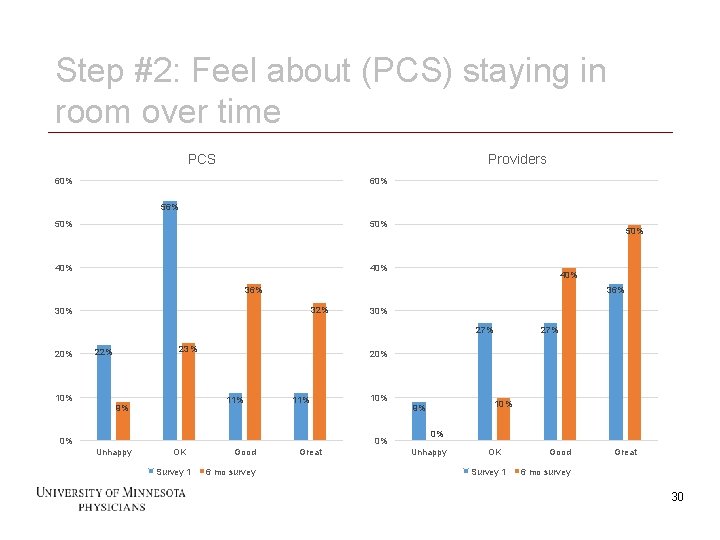
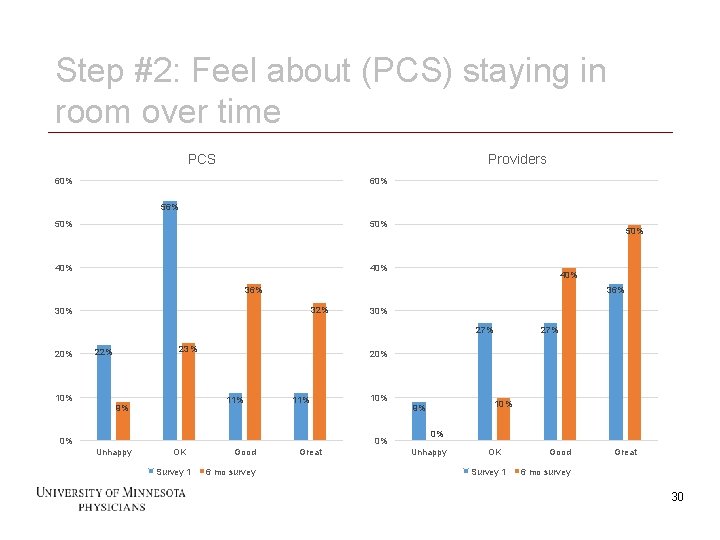
Step #2: Feel about (PCS) staying in room over time PCS Providers 60% 56% 50% 40% 36% 32% 30% 27% 20% 23% 22% 10% 20% 11% 9% 11% 0% OK Survey 1 30 10% Good 6 mo survey Great 10% 9% 0% Unhappy 27% 0% Unhappy OK Survey 1 Good Great 6 mo survey 30
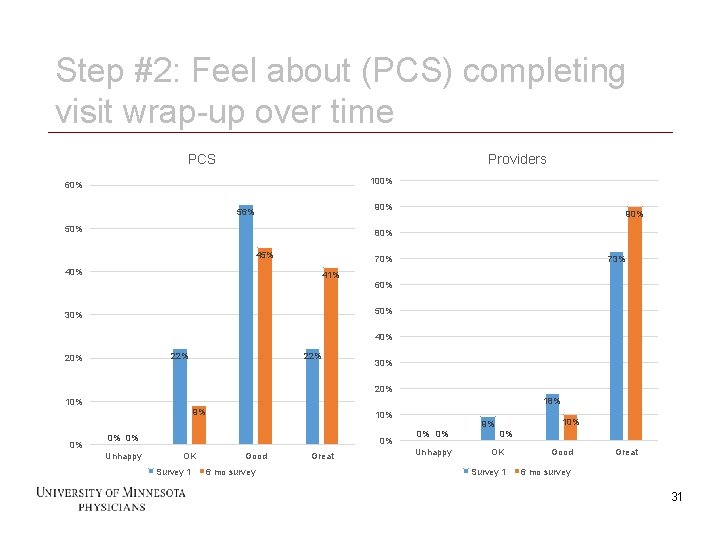
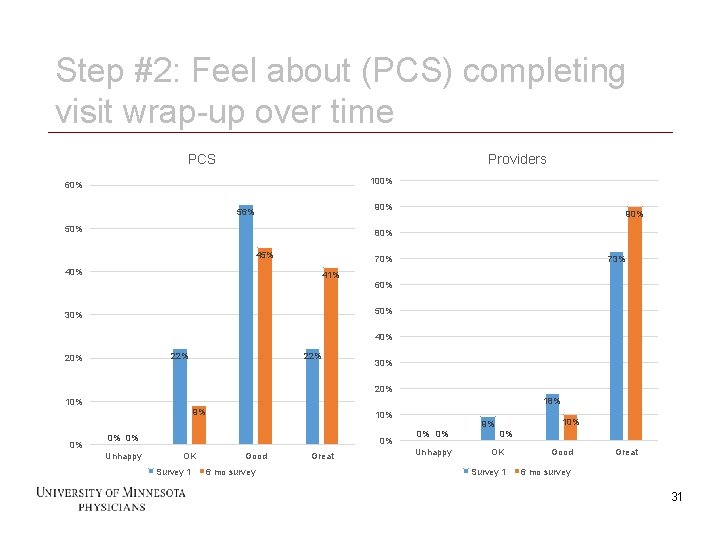
Step #2: Feel about (PCS) completing visit wrap-up over time PCS Providers 100% 60% 90% 56% 50% 90% 80% 45% 73% 70% 41% 60% 50% 30% 40% 22% 20% 22% 30% 20% 18% 10% 9% 0% 0% 0% Unhappy 0% OK Survey 1 31 10% Good 6 mo survey Great 0% 0% Unhappy 9% 10% 0% OK Good Survey 1 6 mo survey Great 31
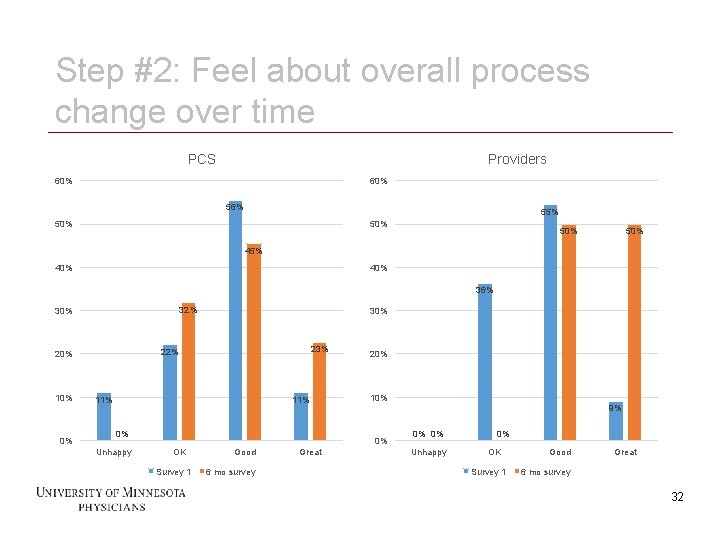
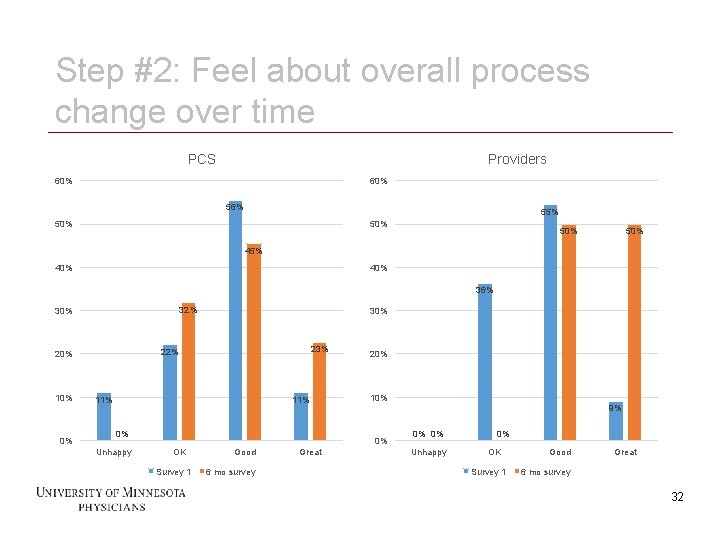
Step #2: Feel about overall process change over time PCS Providers 60% 56% 55% 50% 50% 45% 40% 36% 32% 30% 0% 11% 0% Unhappy 20% 10% 9% 0% OK Survey 1 32 23% 22% 20% 10% 30% Good 6 mo survey Great 0% 0% Unhappy 0% OK Survey 1 Good Great 6 mo survey 32
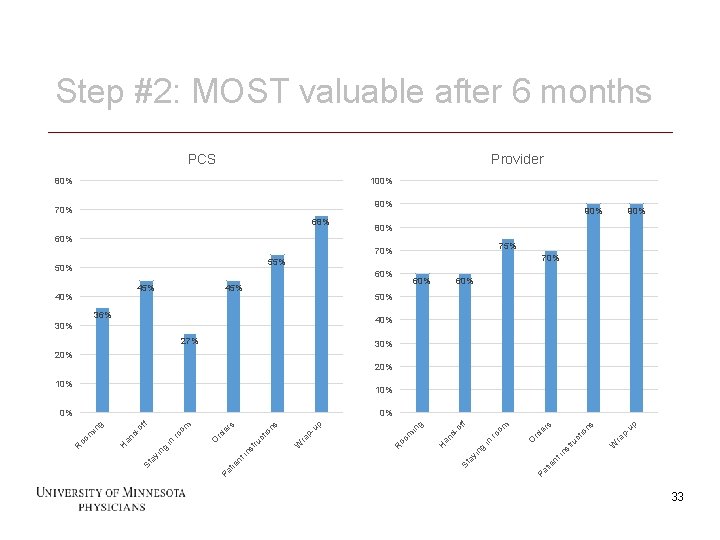
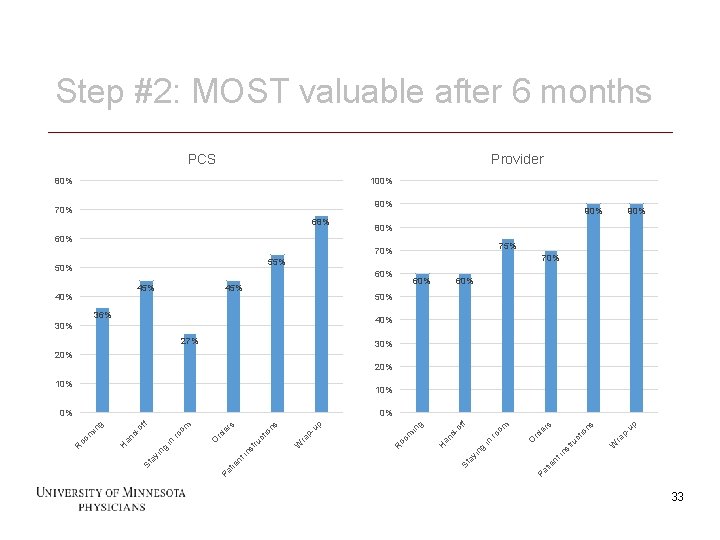
Step #2: MOST valuable after 6 months PCS Provider 80% 100% 90% 70% 68% 90% 80% 60% 75% 70% 55% 50% 60% 45% 40% 45% 90% 60% 50% 36% 40% 30% 27% 30% 20% 10% up in W io ct ru st ra p- ns s er O rd ro in ng Pa tie nt yi St a H an d- of om f g R oo m in up W ct ru in nt Pa tie ra p- ns io er st ro St a yi ng in O rd om f of an d. H in m oo R 33 s 0% g 0% 33
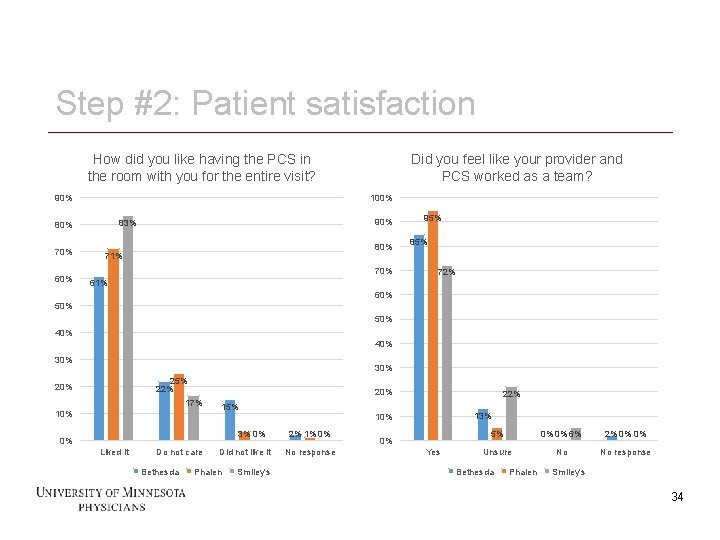
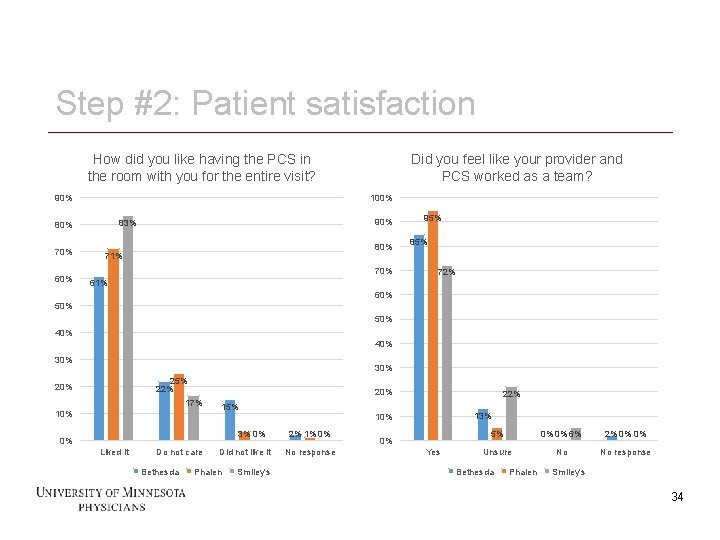
Step #2: Patient satisfaction How did you like having the PCS in the room with you for the entire visit? 90% 100% 60% 90% 83% 80% 70% Did you feel like your provider and PCS worked as a team? 80% 71% 70% 95% 85% 72% 61% 60% 50% 40% 30% 25% 22% 20% 17% 10% 15% 3% 0% 0% Liked it Do not care Bethesda 34 Did not like it Phalen Smiley's 22% 13% 10% 2% 1% 0% No response 0% Yes 5% 0% 0% 6% 2% 0% 0% Unsure No No response Bethesda Phalen Smiley's 34
Step #2: Outcome measures Turn-around time (TAT) More visits/finances – not yet able to measure 35 35
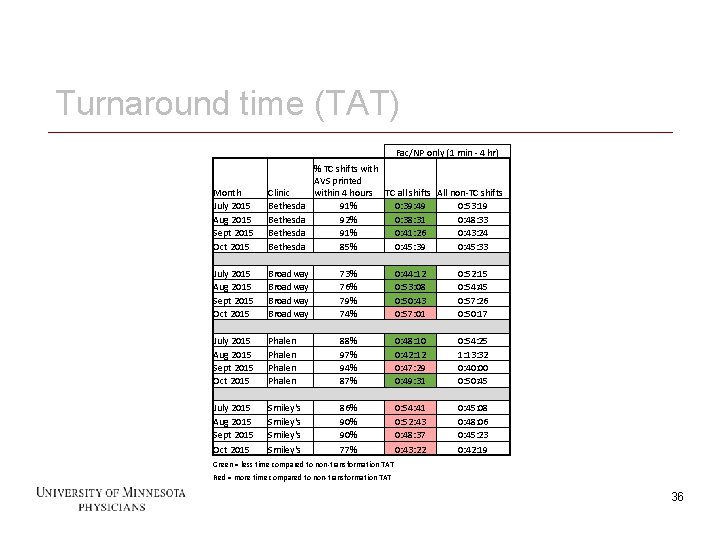
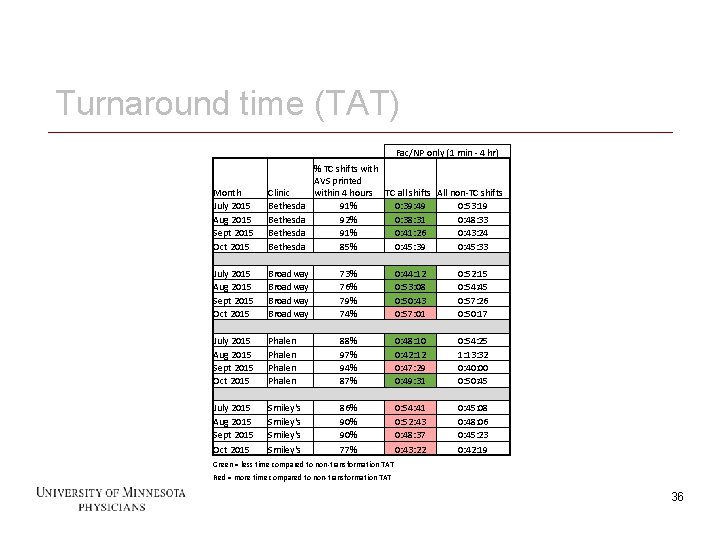
Turnaround time (TAT) Fac/NP only (1 min - 4 hr) % TC shifts with AVS printed within 4 hours TC all shifts All non-TC shifts 91% 0: 39: 49 0: 53: 19 92% 0: 38: 31 0: 48: 33 91% 0: 41: 26 0: 43: 24 85% 0: 45: 39 0: 45: 33 Month July 2015 Aug 2015 Sept 2015 Oct 2015 Clinic Bethesda July 2015 Aug 2015 Sept 2015 Oct 2015 Broadway 73% 76% 79% 74% 0: 44: 12 0: 53: 08 0: 50: 43 0: 57: 01 0: 52: 15 0: 54: 45 0: 57: 26 0: 50: 17 July 2015 Aug 2015 Sept 2015 Oct 2015 Phalen 88% 97% 94% 87% 0: 48: 10 0: 42: 12 0: 47: 29 0: 49: 31 0: 54: 25 1: 13: 32 0: 40: 00 0: 50: 45 July 2015 Aug 2015 Sept 2015 Oct 2015 Smiley's 86% 90% 77% 0: 54: 41 0: 52: 43 0: 48: 37 0: 43: 22 0: 45: 08 0: 48: 06 0: 45: 23 0: 42: 19 Green = less time compared to non-transformation TAT Red = more time compared to non-transformation TAT 36 36
LESSONS LEARNED 37 37
Lessons Learned - PCS can do this and they like it General tide vs local few Vulnerability Listened Understand vulnerability when training Needed to train MD/DO on PCS vulnerability 38 Quicker to see value Continuity Doing it more than docs Get better quicker More resilient Stuck with it Found the value Moving into scribing 38
Lessons Learned - Physicians Deconstruction of visits Autonomy vs Standard Work Owning the note Whole note Assessment and Plan Overt communication Who doesn’t work well Highly invested in AVS Highly invested in beautiful notes High psychosocial complexity 39 39
Lessons Learned - Leadership Build followership / clear direction Worth the time before starting Authorship vs “Build it for me” Straw dog vs blank sheet of paper Small group to pre-build Time vs pressure to change Let process mature before changing Train MD/DO about PCS vulnerability 40 40
Sticky wickets Level loading Hiring Financials – more visits 41 41
Questions/discussion Should this model (Step #2) move onto residents? What are the operational positives? What are the educational negatives? Do you have a similar model? What can you share to help us all learn? 42 42
THANK YOU! 43 43