DRAFT Campus Closure Decision Points Campus Restart Project
- Slides: 10
DRAFT Campus Closure Decision Points Campus Restart Project Management Services July 2020
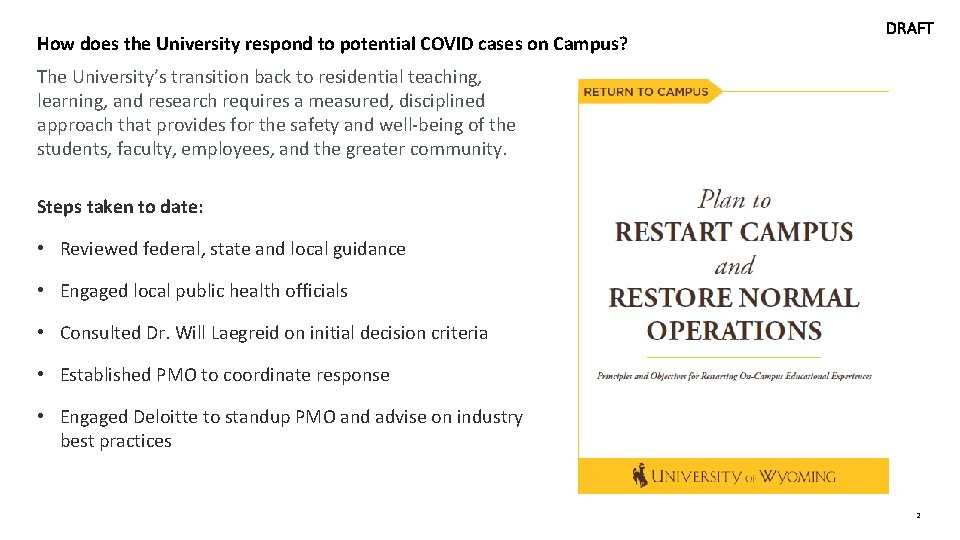
How does the University respond to potential COVID cases on Campus? DRAFT The University’s transition back to residential teaching, learning, and research requires a measured, disciplined approach that provides for the safety and well-being of the students, faculty, employees, and the greater community. Steps taken to date: • Reviewed federal, state and local guidance • Engaged local public health officials • Consulted Dr. Will Laegreid on initial decision criteria • Established PMO to coordinate response • Engaged Deloitte to standup PMO and advise on industry best practices 2
Closing Considerations Working Group Status Update | First Meeting 7/14 DRAFT The following document is shared with the Board as an approved draft that will evolve over the next several weeks. The Closing Considerations Working group has begun meeting to discuss: • • Possible, nuanced short and long-term closure options, and the phases of operation Triggers for implementing the short and long-term closure options In this discussion, the group has begun to identify critical enablers that intersect with other working groups including: • • • The Health Department/University’s ability to trace positive COVID-19 cases in an expeditious manner The University’s capacity to conduct sufficient testing upon student, faculty, and staff return to campus The University’s ability to require compliance with CDC guidelines The group will convene daily to define the conditions under which different operating models will exist. 3
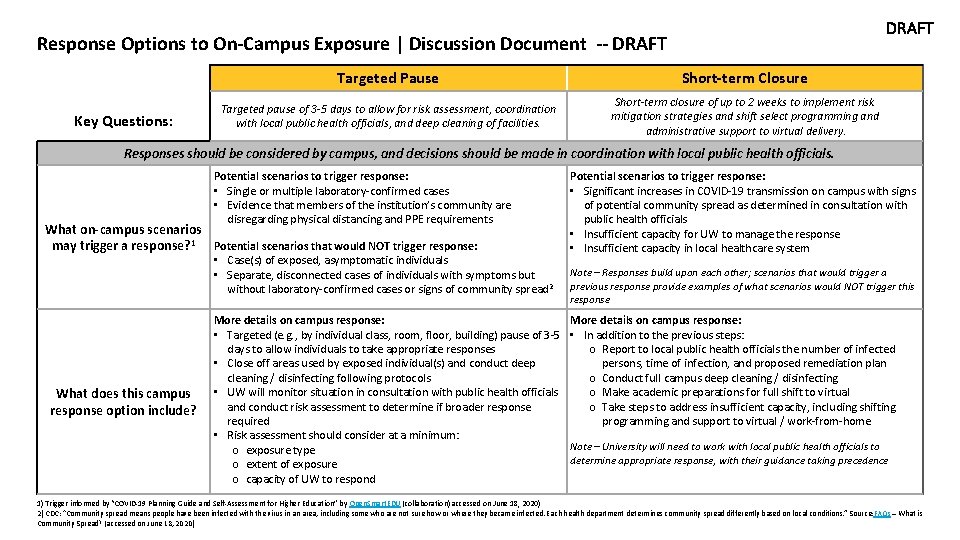
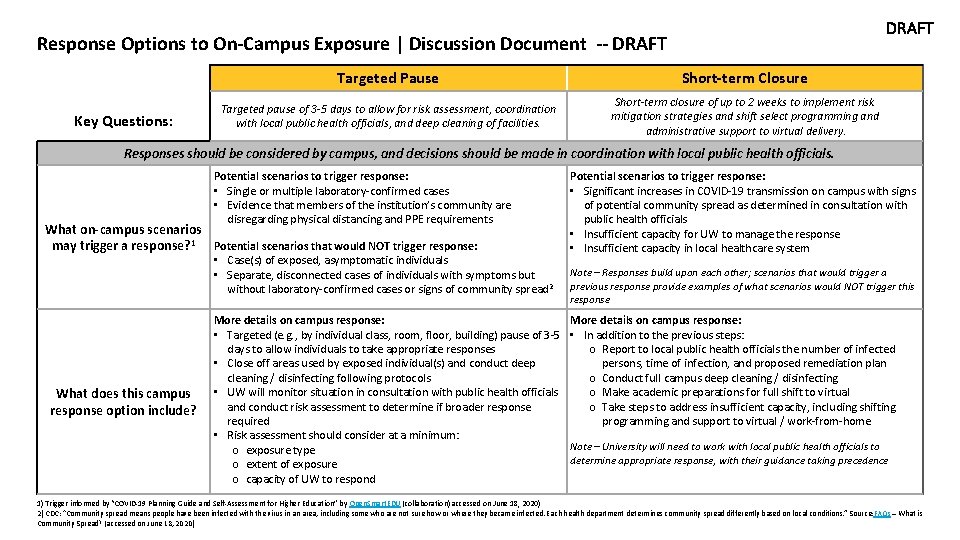
DRAFT Response Options to On-Campus Exposure | Discussion Document -- DRAFT Key Questions: Targeted Pause Short-term Closure Targeted pause of 3 -5 days to allow for risk assessment, coordination with local public health officials, and deep cleaning of facilities. Short-term closure of up to 2 weeks to implement risk mitigation strategies and shift select programming and administrative support to virtual delivery. Responses should be considered by campus, and decisions should be made in coordination with local public health officials. Potential scenarios to trigger response: • Single or multiple laboratory-confirmed cases • Evidence that members of the institution’s community are disregarding physical distancing and PPE requirements What on-campus scenarios may trigger a response? 1 Potential scenarios that would NOT trigger response: • Case(s) of exposed, asymptomatic individuals • Separate, disconnected cases of individuals with symptoms but without laboratory-confirmed cases or signs of community spread 2 What does this campus response option include? More details on campus response: • Targeted (e. g. , by individual class, room, floor, building) pause of 3 -5 days to allow individuals to take appropriate responses • Close off areas used by exposed individual(s) and conduct deep cleaning / disinfecting following protocols • UW will monitor situation in consultation with public health officials and conduct risk assessment to determine if broader response required • Risk assessment should consider at a minimum: o exposure type o extent of exposure o capacity of UW to respond Potential scenarios to trigger response: • Significant increases in COVID-19 transmission on campus with signs of potential community spread as determined in consultation with public health officials • Insufficient capacity for UW to manage the response • Insufficient capacity in local healthcare system Note – Responses build upon each other; scenarios that would trigger a previous response provide examples of what scenarios would NOT trigger this response More details on campus response: • In addition to the previous steps: o Report to local public health officials the number of infected persons, time of infection, and proposed remediation plan o Conduct full campus deep cleaning / disinfecting o Make academic preparations for full shift to virtual o Take steps to address insufficient capacity, including shifting programming and support to virtual / work-from-home Note – University will need to work with local public health officials to determine appropriate response, with their guidance taking precedence 1) Trigger informed by “COVID-19 Planning Guide and Self-Assessment for Higher Education” by Open. Smart. EDU (collaboration) accessed on June 18, 2020) 2) CDC: “Community spread means people have been infected with the virus in an area, including some who are not sure how or where they became infected. Each health department determines community spread differently based on local conditions. ” Source: FAQs – What 4 is Community Spread? (accessed on June 18, 2020)
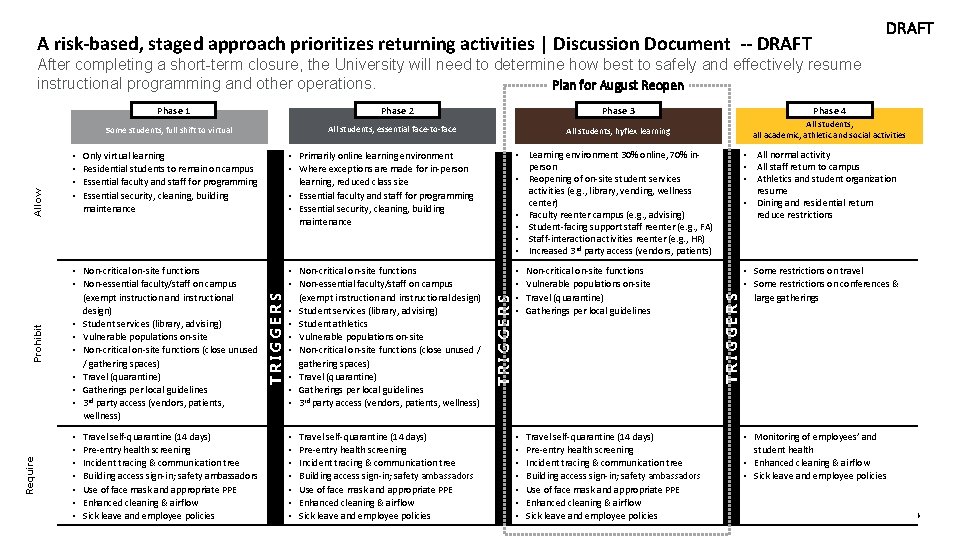
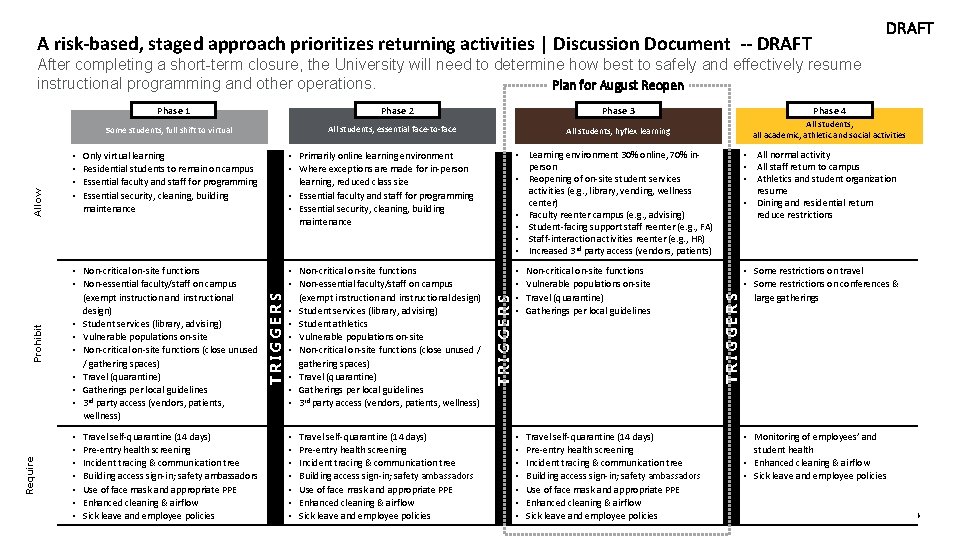
DRAFT A risk-based, staged approach prioritizes returning activities | Discussion Document -- DRAFT After completing a short-term closure, the University will need to determine how best to safely and effectively resume instructional programming and other operations. Plan for August Reopen Phase 2 All students, essential face-to-face Require Only virtual learning Residential students to remain on campus Essential faculty and staff for programming Essential security, cleaning, building maintenance • Non-critical on-site functions • Non-essential faculty/staff on campus (exempt instruction and instructional design) • Student services (library, advising) • Vulnerable populations on-site • Non-critical on-site functions (close unused / gathering spaces) • Travel (quarantine) • Gatherings per local guidelines • 3 rd party access (vendors, patients, wellness) • • Travel self-quarantine (14 days) Pre-entry health screening Incident tracing & communication tree Building access sign-in; safety ambassadors Use of face mask and appropriate PPE Enhanced cleaning & airflow Sick leave and employee policies Phase 4 All students, hyflex learning All students, all academic, athletic and social activities • Primarily online learning environment • Where exceptions are made for in-person learning, reduced class size • Essential faculty and staff for programming • Essential security, cleaning, building maintenance • Learning environment 30% online, 70% inperson • Reopening of on-site student services activities (e. g. , library, vending, wellness center) • Faculty reenter campus (e. g. , advising) • Student-facing support staff reenter (e. g. , FA) • Staff-interaction activities reenter (e. g. , HR) • Increased 3 rd party access (vendors, patients) • Non-critical on-site functions • Non-essential faculty/staff on campus (exempt instruction and instructional design) • Student services (library, advising) • Student athletics • Vulnerable populations on-site • Non-critical on-site functions (close unused / gathering spaces) • Travel (quarantine) • Gatherings per local guidelines • 3 rd party access (vendors, patients, wellness) • • Non-critical on-site functions Vulnerable populations on-site Travel (quarantine) Gatherings per local guidelines • • • • Travel self-quarantine (14 days) Pre-entry health screening Incident tracing & communication tree Building access sign-in; safety ambassadors Use of face mask and appropriate PPE Enhanced cleaning & airflow Sick leave and employee policies TRIGGERS • • TRIGGERS Prohibit Allow Some students, full shift to virtual Phase 3 • All normal activity • All staff return to campus • Athletics and student organization resume • Dining and residential return reduce restrictions TRIGGERS Phase 1 • Some restrictions on travel • Some restrictions on conferences & large gatherings • Monitoring of employees’ and student health • Enhanced cleaning & airflow • Sick leave and employee policies 5
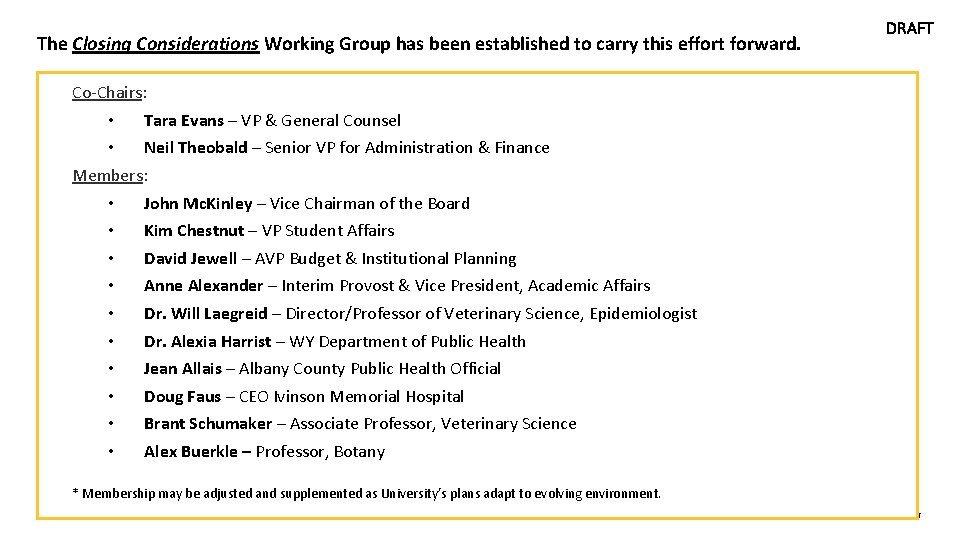
The Closing Considerations Working Group has been established to carry this effort forward. DRAFT Co-Chairs: • Tara Evans – VP & General Counsel • Neil Theobald – Senior VP for Administration & Finance Members: • John Mc. Kinley – Vice Chairman of the Board • Kim Chestnut – VP Student Affairs • David Jewell – AVP Budget & Institutional Planning • Anne Alexander – Interim Provost & Vice President, Academic Affairs • Dr. Will Laegreid – Director/Professor of Veterinary Science, Epidemiologist • Dr. Alexia Harrist – WY Department of Public Health • Jean Allais – Albany County Public Health Official • Doug Faus – CEO Ivinson Memorial Hospital • Brant Schumaker – Associate Professor, Veterinary Science • Alex Buerkle – Professor, Botany * Membership may be adjusted and supplemented as University’s plans adapt to evolving environment. 6
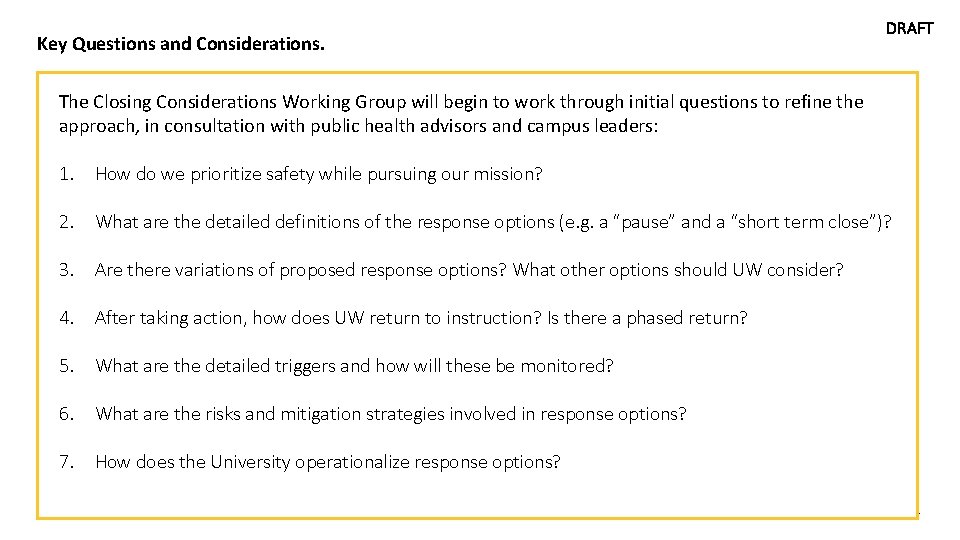
Key Questions and Considerations. DRAFT The Closing Considerations Working Group will begin to work through initial questions to refine the approach, in consultation with public health advisors and campus leaders: 1. How do we prioritize safety while pursuing our mission? 2. What are the detailed definitions of the response options (e. g. a “pause” and a “short term close”)? 3. Are there variations of proposed response options? What other options should UW consider? 4. After taking action, how does UW return to instruction? Is there a phased return? 5. What are the detailed triggers and how will these be monitored? 6. What are the risks and mitigation strategies involved in response options? 7. How does the University operationalize response options? 7
Appendix Exposure Types and Guidance on How Individuals Should Respond
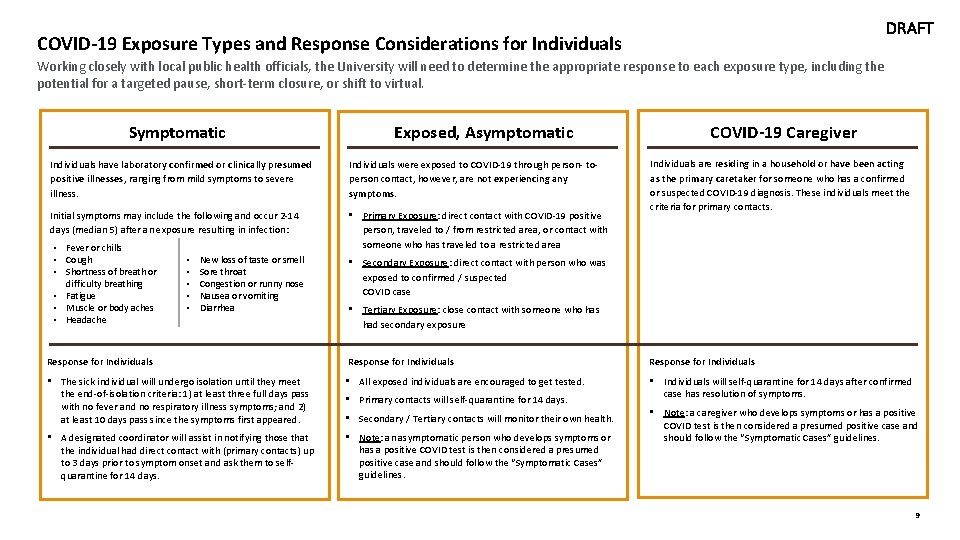
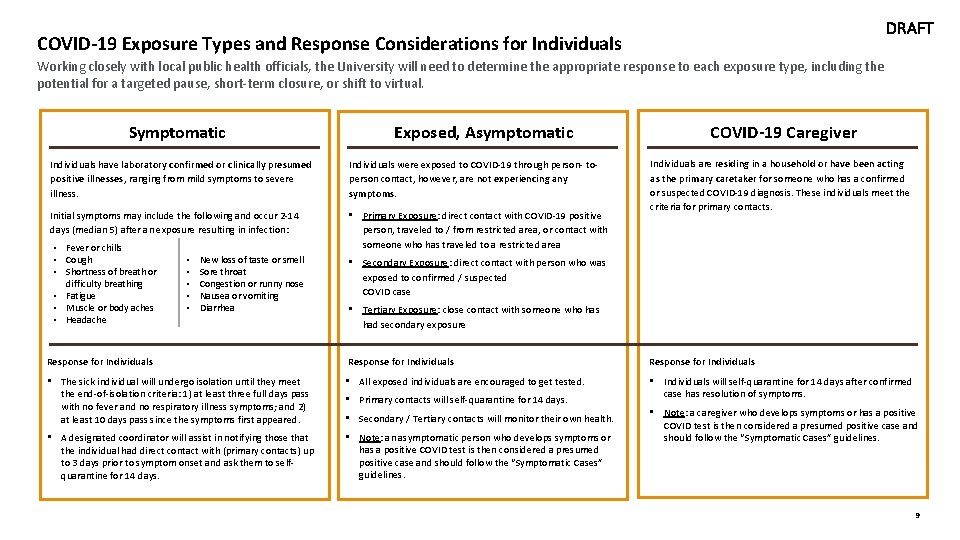
DRAFT COVID-19 Exposure Types and Response Considerations for Individuals Working closely with local public health officials, the University will need to determine the appropriate response to each exposure type, including the potential for a targeted pause, short-term closure, or shift to virtual. Symptomatic Exposed, Asymptomatic Individuals have laboratory confirmed or clinically presumed positive illnesses, ranging from mild symptoms to severe illness. Individuals were exposed to COVID-19 through person- toperson contact, however, are not experiencing any symptoms. Initial symptoms may include the following and occur 2 -14 days (median 5) after an exposure resulting in infection: • Primary Exposure: direct contact with COVID-19 positive person, traveled to / from restricted area, or contact with someone who has traveled to a restricted area • Fever or chills • Cough • Shortness of breath or difficulty breathing • Fatigue • Muscle or body aches • Headache • • • New loss of taste or smell Sore throat Congestion or runny nose Nausea or vomiting Diarrhea COVID-19 Caregiver Individuals are residing in a household or have been acting as the primary caretaker for someone who has a confirmed or suspected COVID-19 diagnosis. These individuals meet the criteria for primary contacts. • Secondary Exposure: direct contact with person who was exposed to confirmed / suspected COVID case • Tertiary Exposure: close contact with someone who has had secondary exposure Response for Individuals • The sick individual will undergo isolation until they meet the end-of-isolation criteria: 1) at least three full days pass with no fever and no respiratory illness symptoms; and 2) at least 10 days pass since the symptoms first appeared. • All exposed individuals are encouraged to get tested. • Individuals will self-quarantine for 14 days after confirmed case has resolution of symptoms. • A designated coordinator will assist in notifying those that the individual had direct contact with (primary contacts) up to 3 days prior to symptom onset and ask them to selfquarantine for 14 days. • Note: an asymptomatic person who develops symptoms or has a positive COVID test is then considered a presumed positive case and should follow the “Symptomatic Cases” guidelines. • Primary contacts will self-quarantine for 14 days. • Secondary / Tertiary contacts will monitor their own health. • Note: a caregiver who develops symptoms or has a positive COVID test is then considered a presumed positive case and should follow the “Symptomatic Cases” guidelines. 9
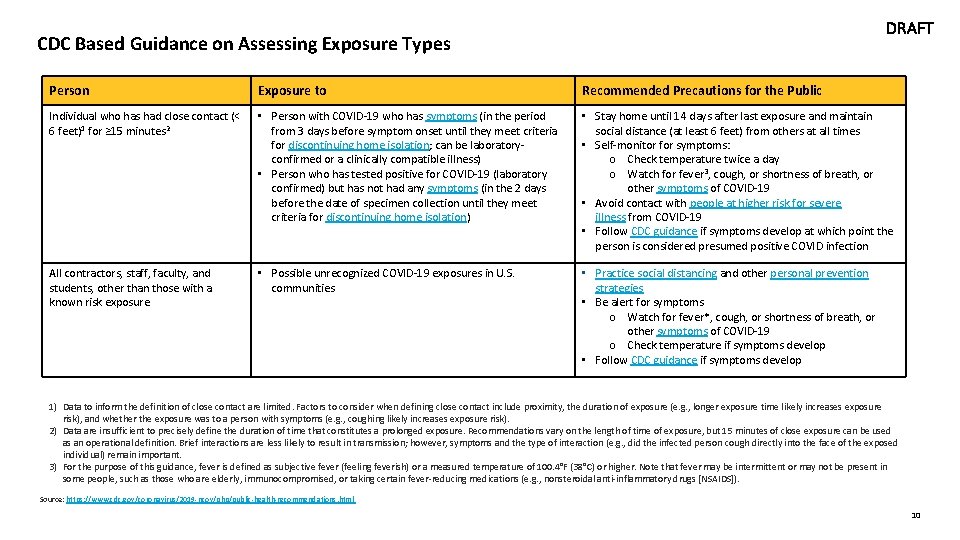
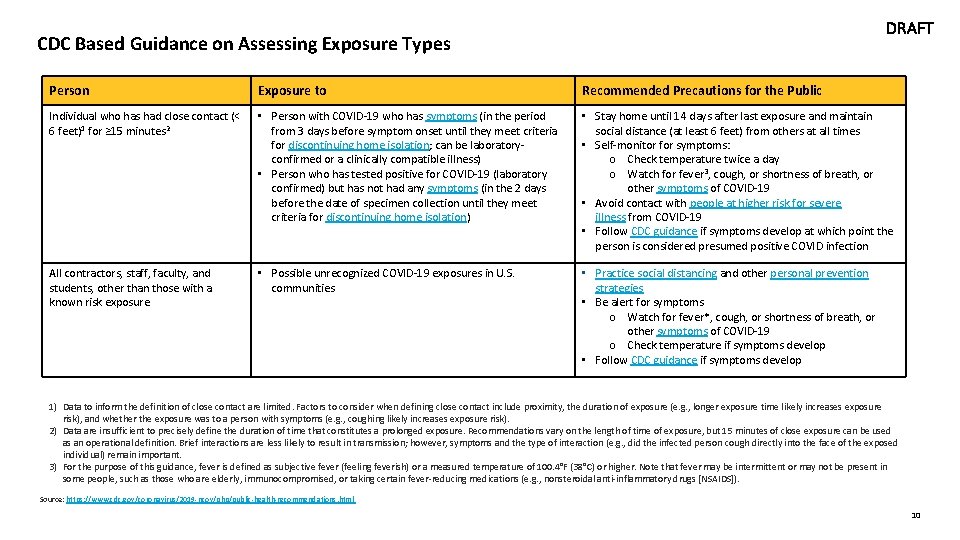
DRAFT CDC Based Guidance on Assessing Exposure Types Person Exposure to Recommended Precautions for the Public Individual who has had close contact (< 6 feet)1 for ≥ 15 minutes 2 • Person with COVID-19 who has symptoms (in the period from 3 days before symptom onset until they meet criteria for discontinuing home isolation; can be laboratoryconfirmed or a clinically compatible illness) • Person who has tested positive for COVID-19 (laboratory confirmed) but has not had any symptoms (in the 2 days before the date of specimen collection until they meet criteria for discontinuing home isolation) • Stay home until 14 days after last exposure and maintain social distance (at least 6 feet) from others at all times • Self-monitor for symptoms: o Check temperature twice a day o Watch for fever 3, cough, or shortness of breath, or other symptoms of COVID-19 • Avoid contact with people at higher risk for severe illness from COVID-19 • Follow CDC guidance if symptoms develop at which point the person is considered presumed positive COVID infection All contractors, staff, faculty, and students, other than those with a known risk exposure • Possible unrecognized COVID-19 exposures in U. S. communities • Practice social distancing and other personal prevention strategies • Be alert for symptoms o Watch for fever*, cough, or shortness of breath, or other symptoms of COVID-19 o Check temperature if symptoms develop • Follow CDC guidance if symptoms develop 1) Data to inform the definition of close contact are limited. Factors to consider when defining close contact include proximity, the duration of exposure (e. g. , longer exposure time likely increases exposure risk), and whether the exposure was to a person with symptoms (e. g. , coughing likely increases exposure risk). 2) Data are insufficient to precisely define the duration of time that constitutes a prolonged exposure. Recommendations vary on the length of time of exposure, but 15 minutes of close exposure can be used as an operational definition. Brief interactions are less likely to result in transmission; however, symptoms and the type of interaction (e. g. , did the infected person cough directly into the face of the exposed individual) remain important. 3) For the purpose of this guidance, fever is defined as subjective fever (feeling feverish) or a measured temperature of 100. 4°F (38°C) or higher. Note that fever may be intermittent or may not be present in some people, such as those who are elderly, immunocompromised, or taking certain fever-reducing medications (e. g. , nonsteroidal anti-inflammatory drugs [NSAIDS]). Source: https: //www. cdc. gov/coronavirus/2019 -ncov/php/public-health-recommendations. html 10