Developmental Progression of Practice Competencies Across Four Levels
- Slides: 25
Developmental Progression of Practice Competencies Across Four Levels of Clinical Advancement (not for distribution) May 26, 2016 Tonya Johnson, DNP, RN, CCRN-K, NEA-BC Clinical Director, Pennsylvania Hospital CAPP Co-Chair Chris Sites, MSN RN Professional Development Specialist CAPP Co-Chair Kathleen Burke, Ph. D, RN, CENP, FAAN Corporate Director, Nursing Professional Development and Innovation CAPP Executive Sponsor
Objectives: 1. Describe the importance of competency domains in driving contemporary practice 2. Describe the methodology and results of the Delphi study 3. Discuss the implications of the Delphi study for professional nursing practice 2
Why Look at Competency Domains? w More than a decade after the landmark reports To Err Is Human: Building a Safer Health System, and the follow-up report, Crossing the Quality Chasm, there are significant problem with quality and safety in healthcare w Nearly 400, 000 people are still dying per year in hospitals in the USA w Quality, Safety and Education for Nurses(QSEN) competencies (developed in phases from 2005 -2012) have influenced Nursing Education curriculum (undergraduate and graduate) since 2012 but these evidenced-based domain competencies have not been incorporated into contemporary clinical practice w No longer is an Individual approach to care effective to improved quality and patient outcomes, a system’s approach is needed to accelerate improvement in quality and patient outcomes w The competency domains that frame nursing practice at Penn Medicine have not been updated in over 16 years (1999) • • Clinical Judgment and Decision Making Nurse Patient/Family Relationship Clinical Leadership Clinical Scholarship 3
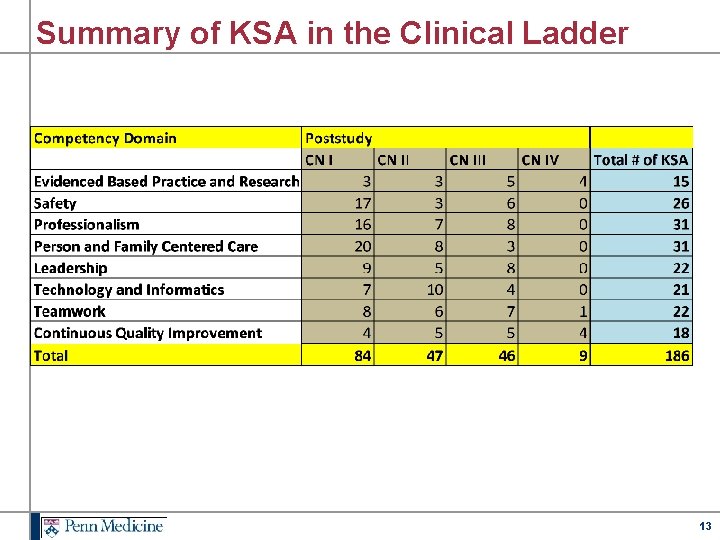
Development of Competency Domains w Developed in 2013 by Penn Medicine Council for the Advancement of Professional Practice (CAPP) w 8 competency domains w 186 knowledge, skills, attitudes (KSAs) w Evidence – based • Landmark reports • High quality evidence • Recommendations of professional organizations • Clinical expertise • An extensive literature review • Professional Consultation – Jane Barnsteiner Ph. D, RN, FAAN – Donna Wright MS, RN 4
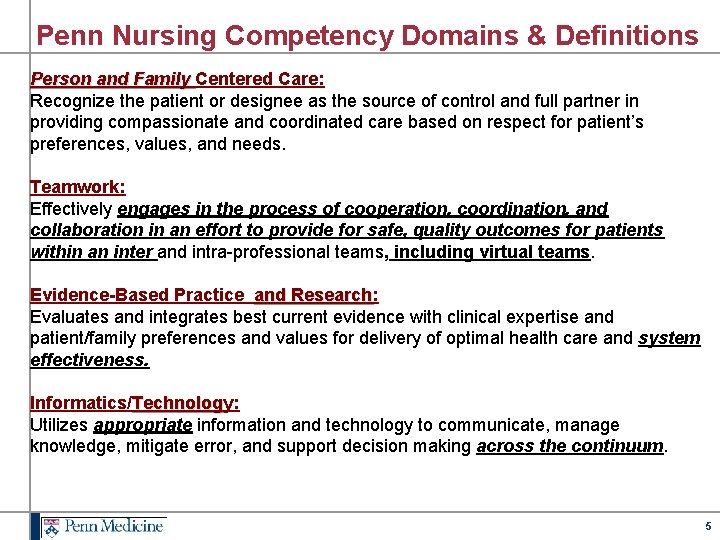
Penn Nursing Competency Domains & Definitions Person and Family Centered Care: Recognize the patient or designee as the source of control and full partner in providing compassionate and coordinated care based on respect for patient’s preferences, values, and needs. Teamwork: Effectively engages in the process of cooperation, coordination, and collaboration in an effort to provide for safe, quality outcomes for patients within an inter and intra-professional teams, including virtual teams. Evidence-Based Practice and Research: and Research Evaluates and integrates best current evidence with clinical expertise and patient/family preferences and values for delivery of optimal health care and system effectiveness. Informatics/Technology: Technolog Utilizes appropriate information and technology to communicate, manage knowledge, mitigate error, and support decision making across the continuum. 5
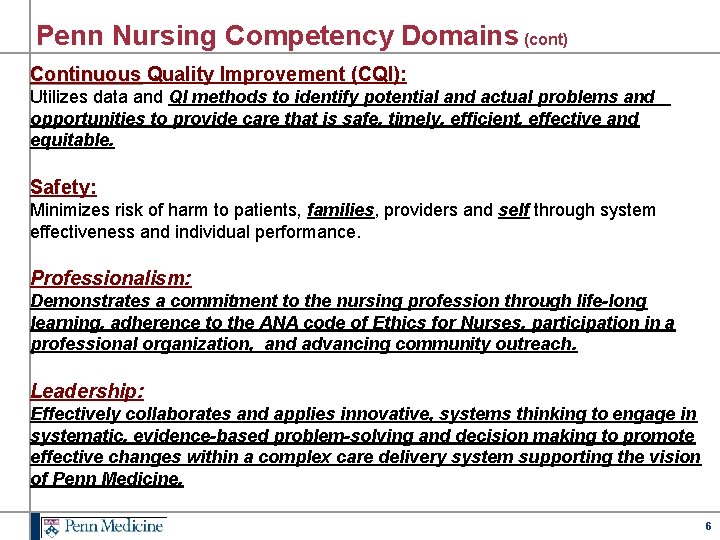
Penn Nursing Competency Domains (cont) Continuous Quality Improvement (CQI): Continuous Utilizes data and QI methods to identify potential and actual problems and opportunities to provide care that is safe, timely, efficient, effective and equitable. Safety: Minimizes risk of harm to patients, families, providers and self through system effectiveness and individual performance. Professionalism: Demonstrates a commitment to the nursing profession through life-long learning, adherence to the ANA code of Ethics for Nurses, participation in a professional organization, and advancing community outreach. Leadership: Effectively collaborates and applies innovative, systems thinking to engage in systematic, evidence-based problem-solving and decision making to promote effective changes within a complex care delivery system supporting the vision of Penn Medicine. 6
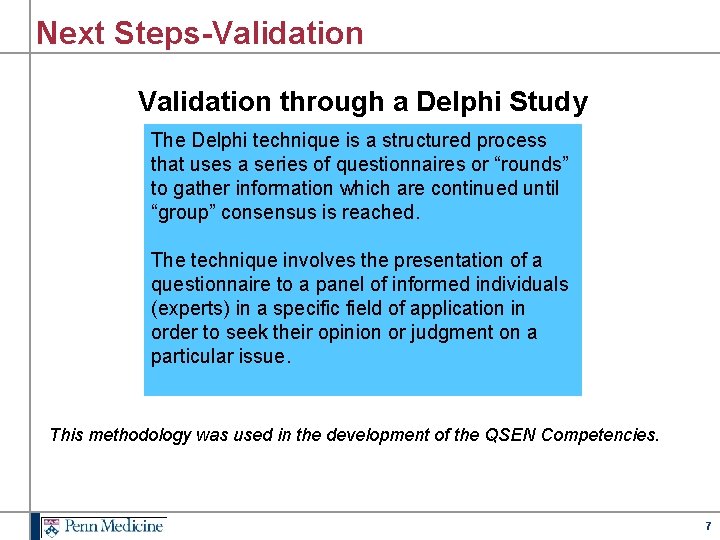
Next Steps-Validation through a Delphi Study The Delphi technique is a structured process that uses a series of questionnaires or “rounds” to gather information which are continued until “group” consensus is reached. The technique involves the presentation of a questionnaire to a panel of informed individuals (experts) in a specific field of application in order to seek their opinion or judgment on a particular issue. This methodology was used in the development of the QSEN Competencies. 7
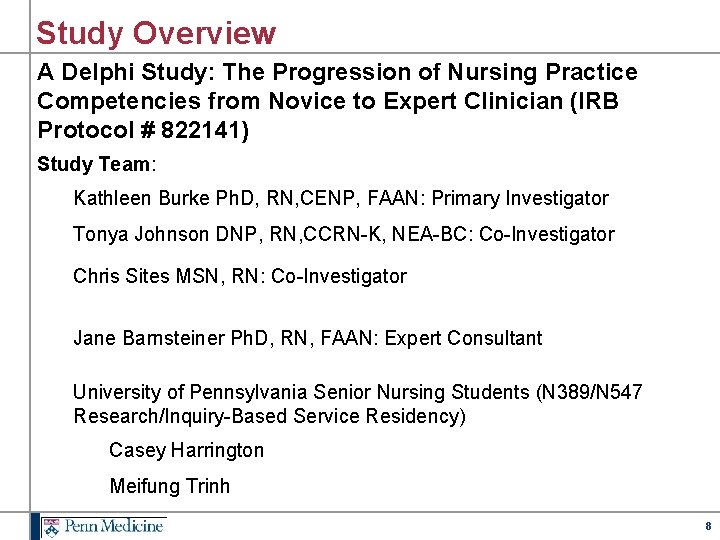
Study Overview A Delphi Study: The Progression of Nursing Practice Competencies from Novice to Expert Clinician (IRB Protocol # 822141) Study Team: Kathleen Burke Ph. D, RN, CENP, FAAN: Primary Investigator Tonya Johnson DNP, RN, CCRN-K, NEA-BC: Co-Investigator Chris Sites MSN, RN: Co-Investigator Jane Barnsteiner Ph. D, RN, FAAN: Expert Consultant University of Pennsylvania Senior Nursing Students (N 389/N 547 Research/Inquiry-Based Service Residency) Casey Harrington Meifung Trinh 8
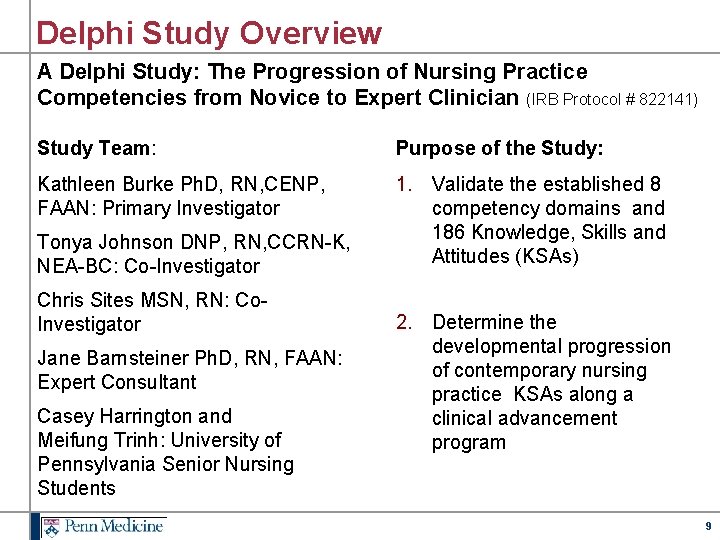
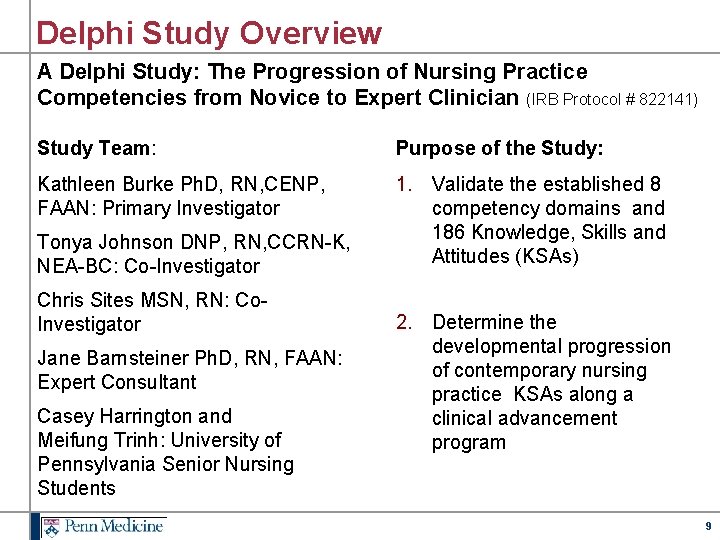
Delphi Study Overview A Delphi Study: The Progression of Nursing Practice Competencies from Novice to Expert Clinician (IRB Protocol # 822141) Study Team: Purpose of the Study: Kathleen Burke Ph. D, RN, CENP, FAAN: Primary Investigator 1. Validate the established 8 competency domains and 186 Knowledge, Skills and Attitudes (KSAs) Tonya Johnson DNP, RN, CCRN-K, NEA-BC: Co-Investigator Chris Sites MSN, RN: Co. Investigator Jane Barnsteiner Ph. D, RN, FAAN: Expert Consultant Casey Harrington and Meifung Trinh: University of Pennsylvania Senior Nursing Students 2. Determine the developmental progression of contemporary nursing practice KSAs along a clinical advancement program 9
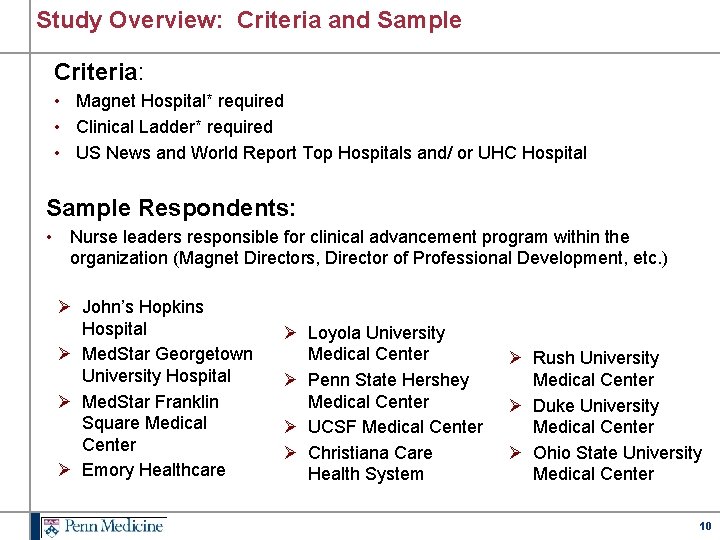
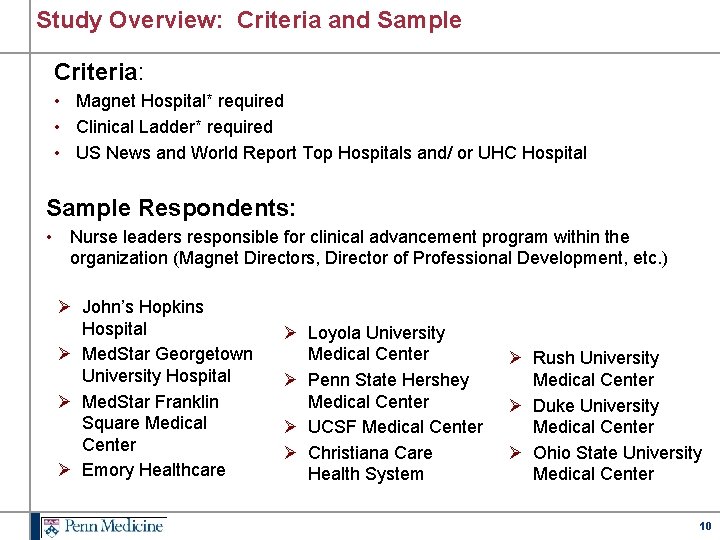
Study Overview: Criteria and Sample Criteria: • Magnet Hospital* required • Clinical Ladder* required • US News and World Report Top Hospitals and/ or UHC Hospital Sample Respondents: • Nurse leaders responsible for clinical advancement program within the organization (Magnet Directors, Director of Professional Development, etc. ) Ø John’s Hopkins Hospital Ø Med. Star Georgetown University Hospital Ø Med. Star Franklin Square Medical Center Ø Emory Healthcare Ø Loyola University Medical Center Ø Penn State Hershey Medical Center Ø UCSF Medical Center Ø Christiana Care Health System Ø Rush University Medical Center Ø Duke University Medical Center Ø Ohio State University Medical Center 10
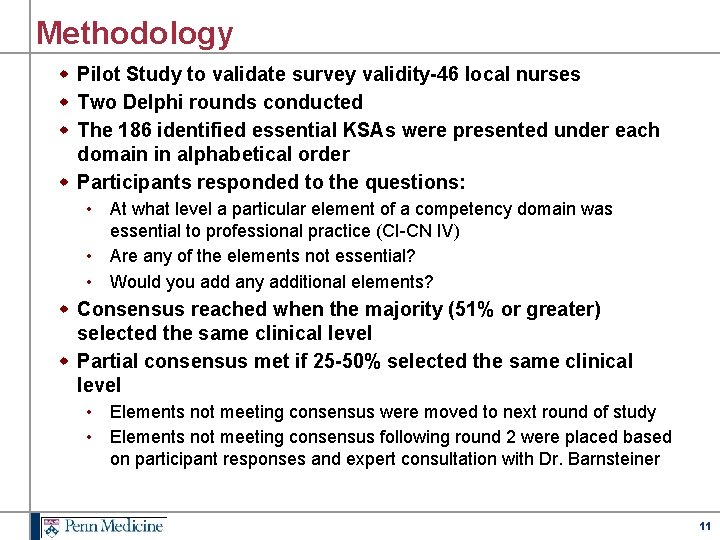
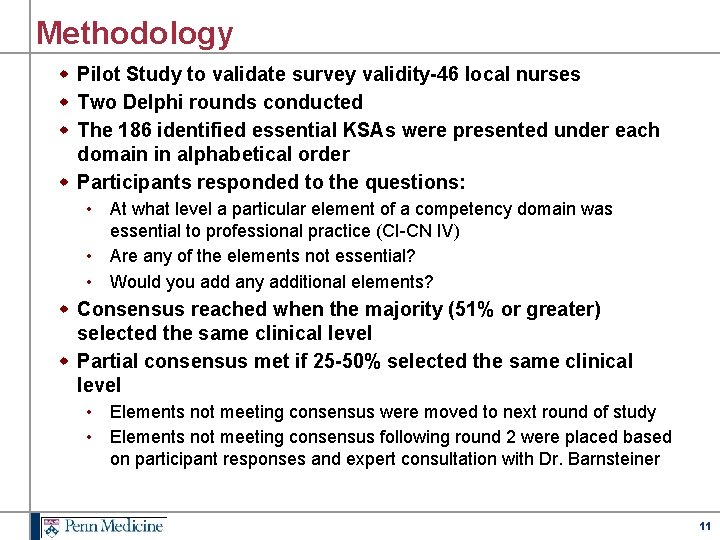
Methodology w Pilot Study to validate survey validity-46 local nurses w Two Delphi rounds conducted w The 186 identified essential KSAs were presented under each domain in alphabetical order w Participants responded to the questions: • At what level a particular element of a competency domain was essential to professional practice (CI-CN IV) • Are any of the elements not essential? • Would you add any additional elements? w Consensus reached when the majority (51% or greater) selected the same clinical level w Partial consensus met if 25 -50% selected the same clinical level • Elements not meeting consensus were moved to next round of study • Elements not meeting consensus following round 2 were placed based on participant responses and expert consultation with Dr. Barnsteiner 11
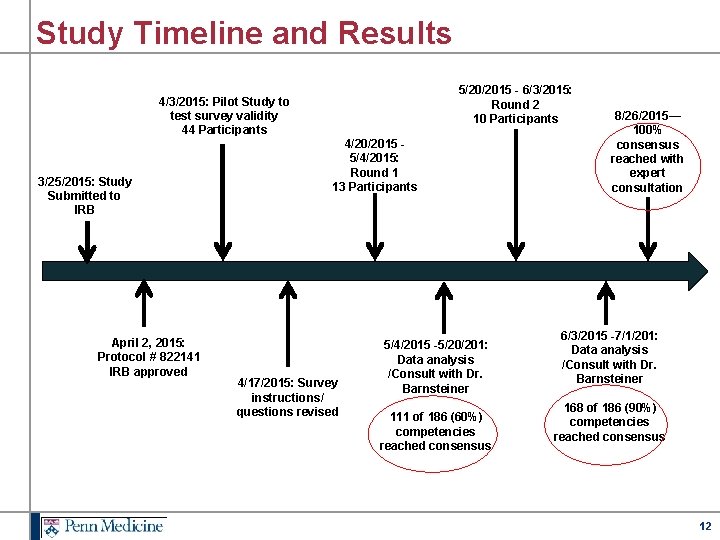
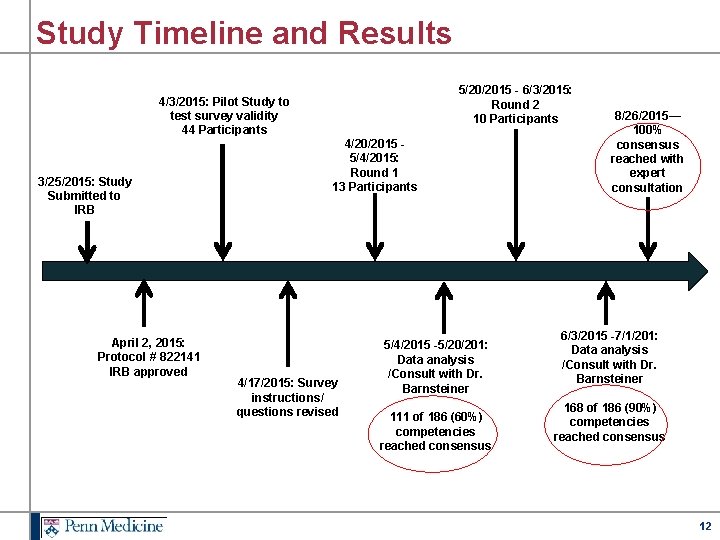
Study Timeline and Results 4/3/2015: Pilot Study to test survey validity 44 Participants 3/25/2015: Study Submitted to IRB April 2, 2015: Protocol # 822141 IRB approved 5/20/2015 - 6/3/2015: Round 2 10 Participants 4/20/2015 - 5/4/2015: Round 1 13 Participants 4/17/2015: Survey instructions/ questions revised 5/4/2015 -5/20/201: Data analysis /Consult with Dr. Barnsteiner 111 of 186 (60%) competencies reached consensus 8/26/2015— 100% consensus reached with expert consultation 6/3/2015 -7/1/201: Data analysis /Consult with Dr. Barnsteiner 168 of 186 (90%) competencies reached consensus 12
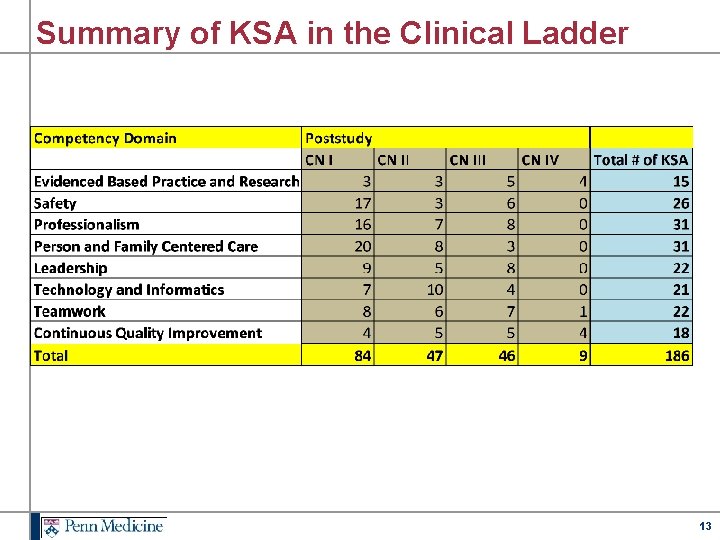
Summary of KSA in the Clinical Ladder 13
Benefits of Applying the Empirical Evidence to Practice w As a result of the evidence generated from the Delphi study, Penn Medicine has the unique opportunity to apply this evidence to: • Drive quality and clinical outcomes as it supports the Penn Medicine Blueprint for Quality and Safety • Clearly define role expectations through redesign of the performance appraisals • Enhance accountability in our clinical advancement program • Recognize and promote the contemporary practice of our nurses • Elevate professional nursing practice 14
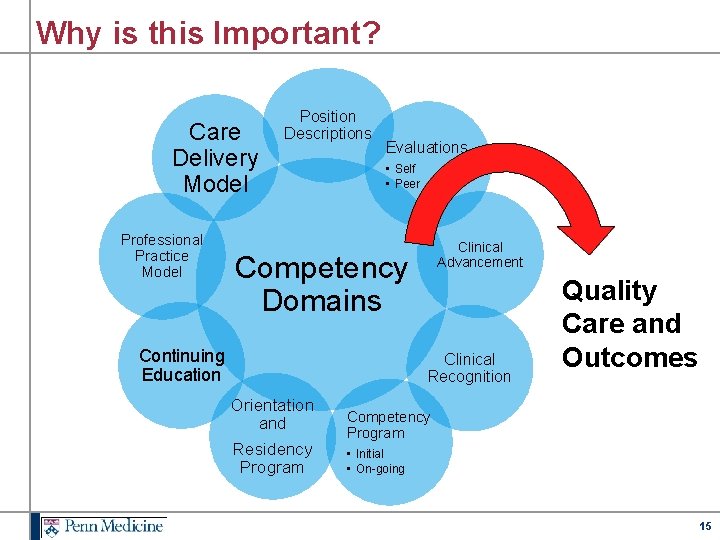
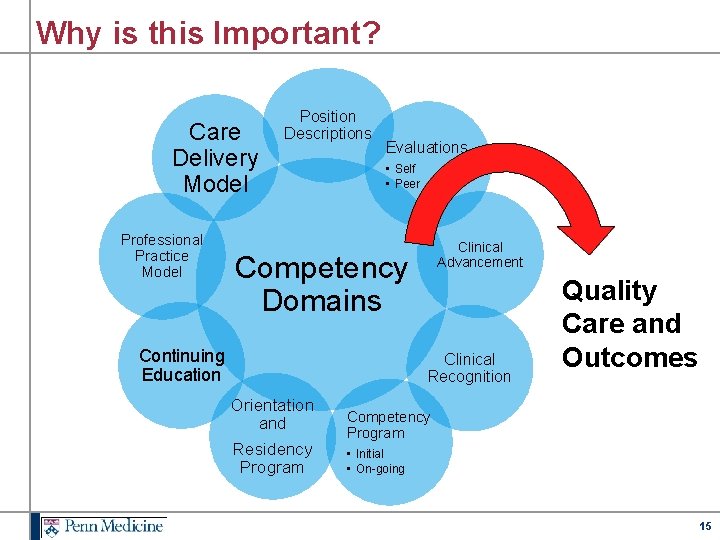
Why is this Important? Care Delivery Model Professional Practice Model Position Descriptions Evaluations • Self • Peer Clinical Advancement Competency Domains Continuing Education Clinical Recognition Orientation and Residency Program Quality Care and Outcomes Competency Program • Initial • On-going 15
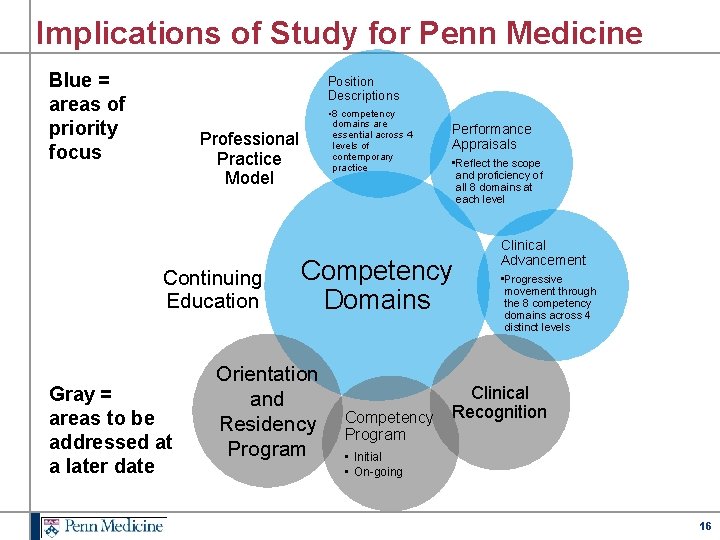
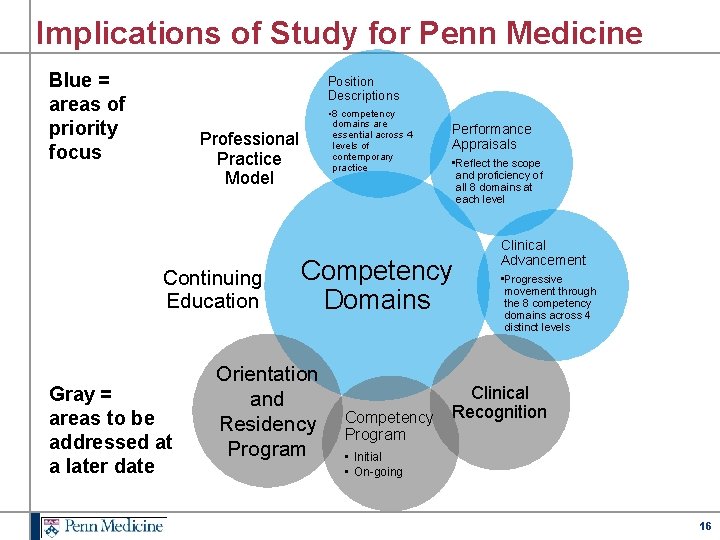
Implications of Study for Penn Medicine Blue = areas of priority focus Position Descriptions • 8 competency domains are essential across 4 levels of contemporary practice Professional Practice Model Continuing Education Gray = areas to be addressed at a later date Performance Appraisals • Reflect the scope and proficiency of all 8 domains at each level Competency Domains Orientation and Residency Program Competency Program Clinical Advancement • Progressive movement through the 8 competency domains across 4 distinct levels Clinical Recognition • Initial • On-going 16
Approval and Socialization w Penn Medicine Chief Nursing Officer Council - Approval to move forward w Nursing Leadership Meetings at each entity within Penn Medicine • Target audience-CDs, NM, ANM, CNS, CNE/NPDS, Shared Governance Chairs w Human Resources w Nursing Recruitment w Professional Development, Education, and Advisory Council 17
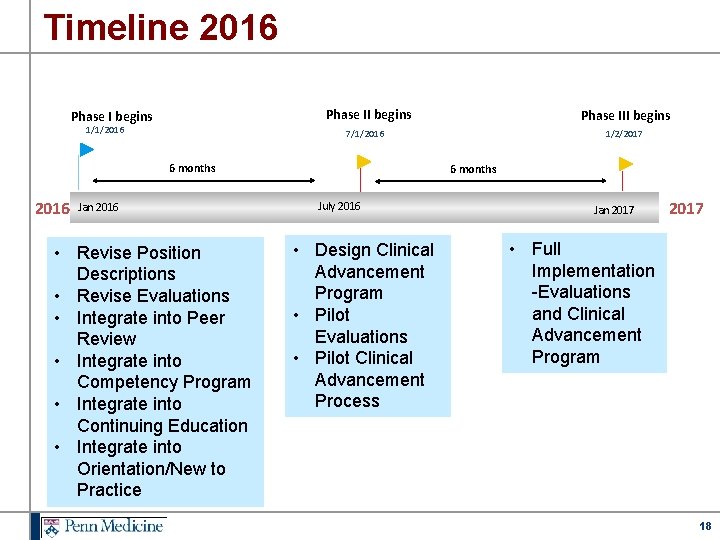
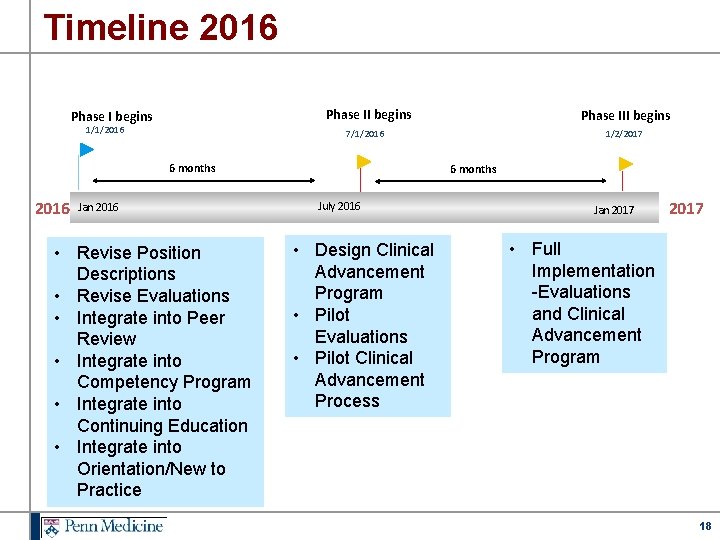
Timeline 2016 Phase II begins Phase I begins 1/1/2016 1/2/2017 7/1/2016 6 months 2016 Phase III begins Jan 2016 • Revise Position Descriptions • Revise Evaluations • Integrate into Peer Review • Integrate into Competency Program • Integrate into Continuing Education • Integrate into Orientation/New to Practice 6 months July 2016 • Design Clinical Advancement Program • Pilot Evaluations • Pilot Clinical Advancement Process Jan 2017 • Full Implementation -Evaluations and Clinical Advancement Program 18
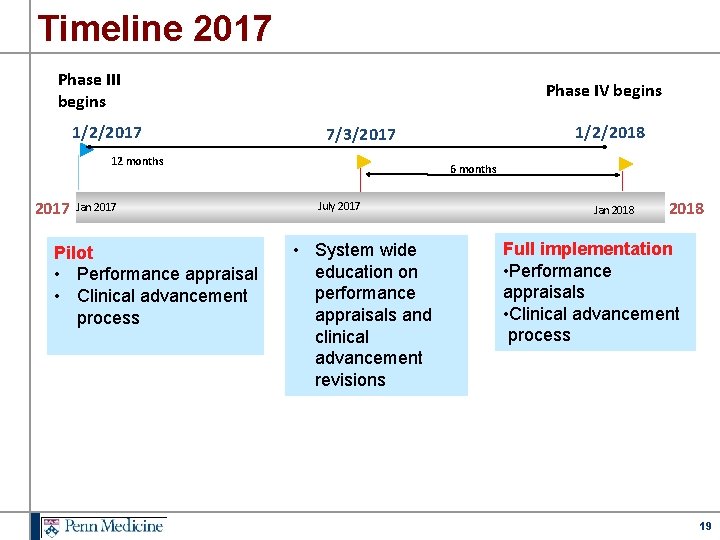
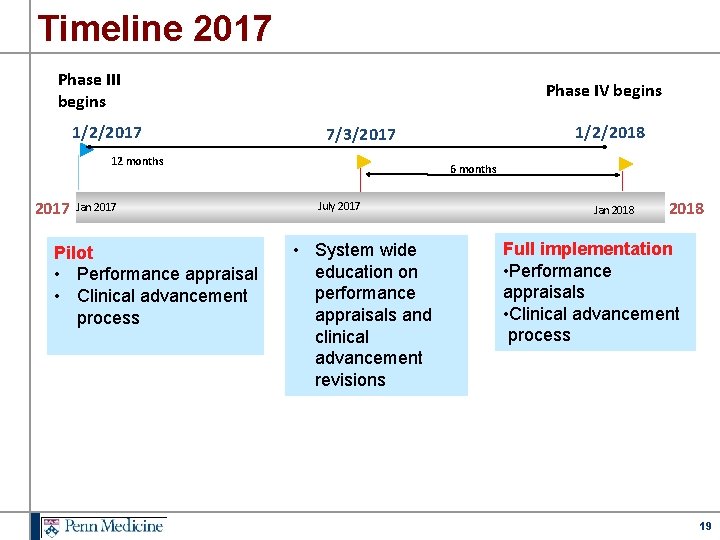
Timeline 2017 Phase III begins 1/2/2017 Phase IV begins 12 months 2017 Jan 2017 Pilot • Performance appraisal • Clinical advancement process 1/2/2018 7/3/2017 6 months July 2017 • System wide education on performance appraisals and clinical advancement revisions Jan 2018 Full implementation • Performance appraisals • Clinical advancement process 19
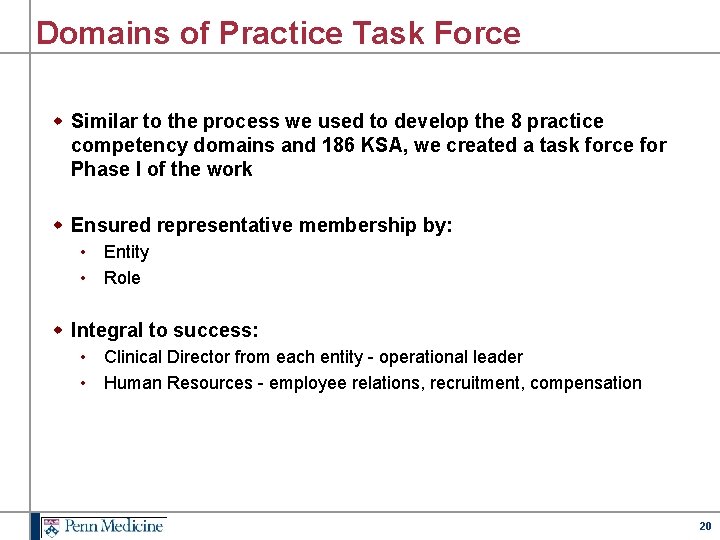
Domains of Practice Task Force w Similar to the process we used to develop the 8 practice competency domains and 186 KSA, we created a task force for Phase I of the work w Ensured representative membership by: • Entity • Role w Integral to success: • Clinical Director from each entity - operational leader • Human Resources - employee relations, recruitment, compensation 20
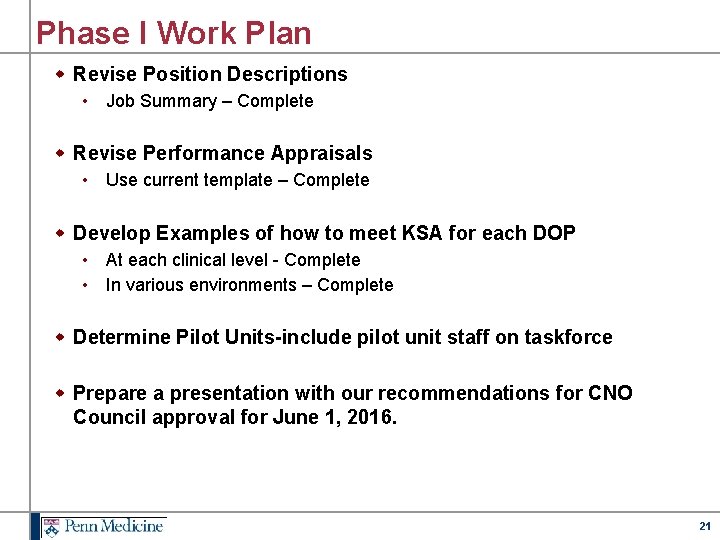
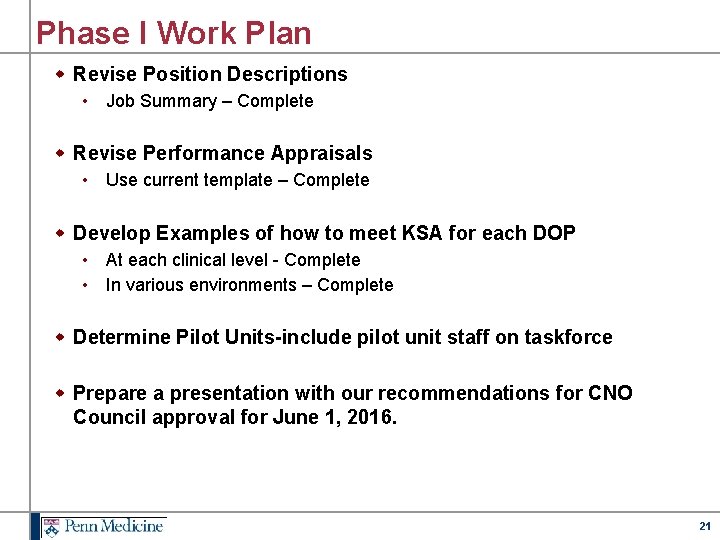
Phase I Work Plan w Revise Position Descriptions • Job Summary – Complete w Revise Performance Appraisals • Use current template – Complete w Develop Examples of how to meet KSA for each DOP • At each clinical level - Complete • In various environments – Complete w Determine Pilot Units-include pilot unit staff on taskforce w Prepare a presentation with our recommendations for CNO Council approval for June 1, 2016. 21
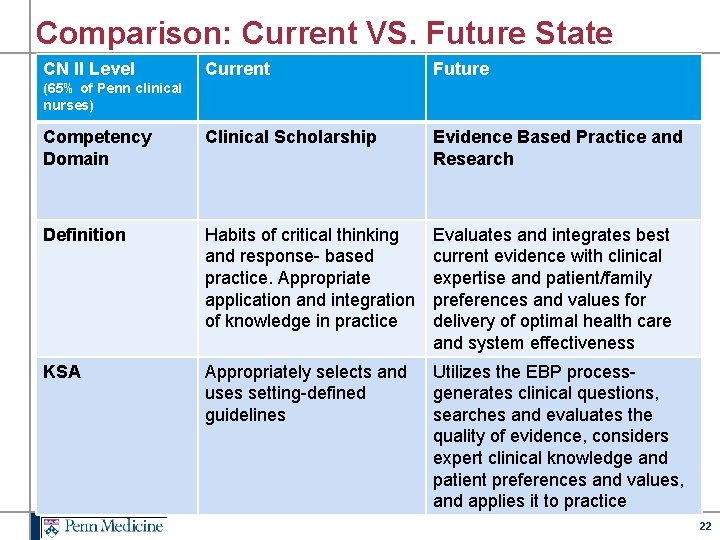
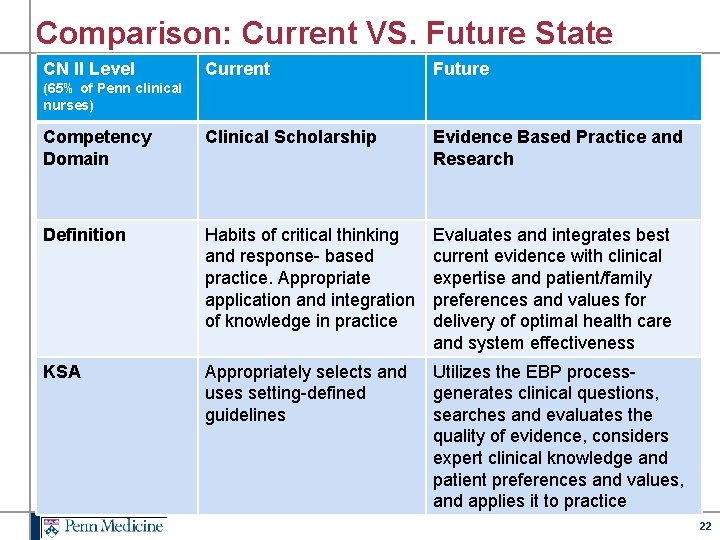
Comparison: Current VS. Future State CN II Level Current Future Competency Domain Clinical Scholarship Evidence Based Practice and Research Definition Habits of critical thinking and response- based practice. Appropriate application and integration of knowledge in practice Evaluates and integrates best current evidence with clinical expertise and patient/family preferences and values for delivery of optimal health care and system effectiveness KSA Appropriately selects and uses setting-defined guidelines Utilizes the EBP processgenerates clinical questions, searches and evaluates the quality of evidence, considers expert clinical knowledge and patient preferences and values, and applies it to practice (65% of Penn clinical nurses) 22
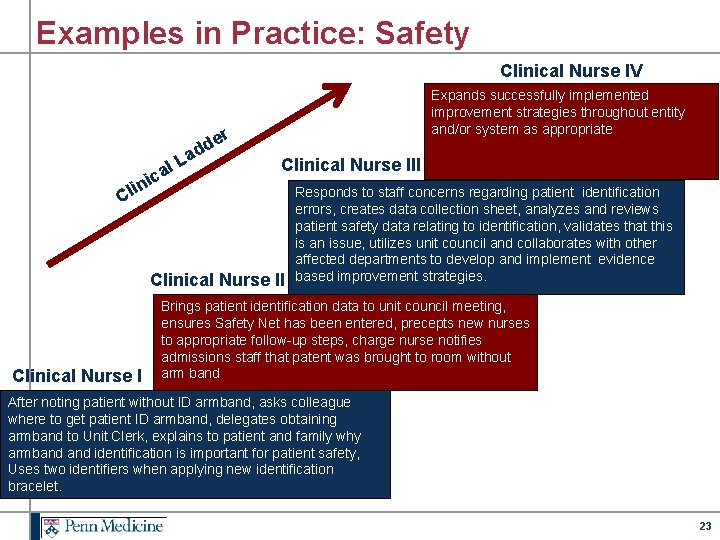
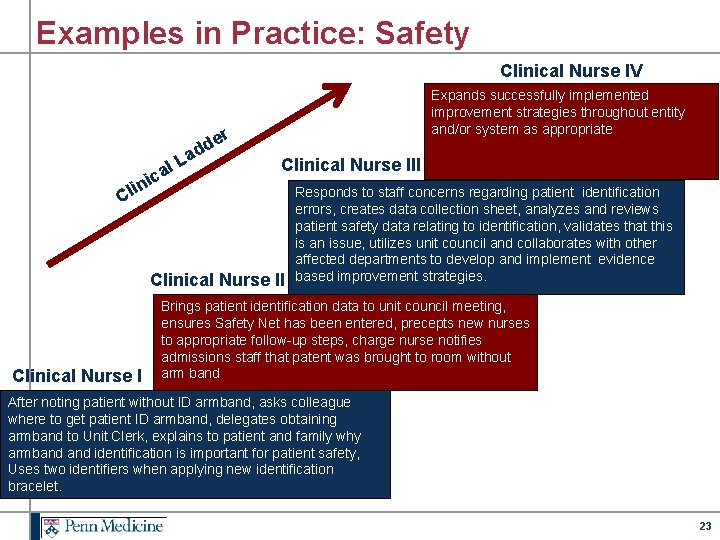
Examples in Practice: Safety Clinical Nurse IV Expands successfully implemented improvement strategies throughout entity and/or system as appropriate r de d La al c i n Clinical Nurse III i Cl Clinical Nurse II Clinical Nurse I Responds to staff concerns regarding patient identification errors, creates data collection sheet, analyzes and reviews patient safety data relating to identification, validates that this is an issue, utilizes unit council and collaborates with other affected departments to develop and implement evidence based improvement strategies. Brings patient identification data to unit council meeting, ensures Safety Net has been entered, precepts new nurses to appropriate follow-up steps, charge nurse notifies admissions staff that patent was brought to room without arm band After noting patient without ID armband, asks colleague where to get patient ID armband, delegates obtaining armband to Unit Clerk, explains to patient and family why armband identification is important for patient safety, Uses two identifiers when applying new identification bracelet. 23
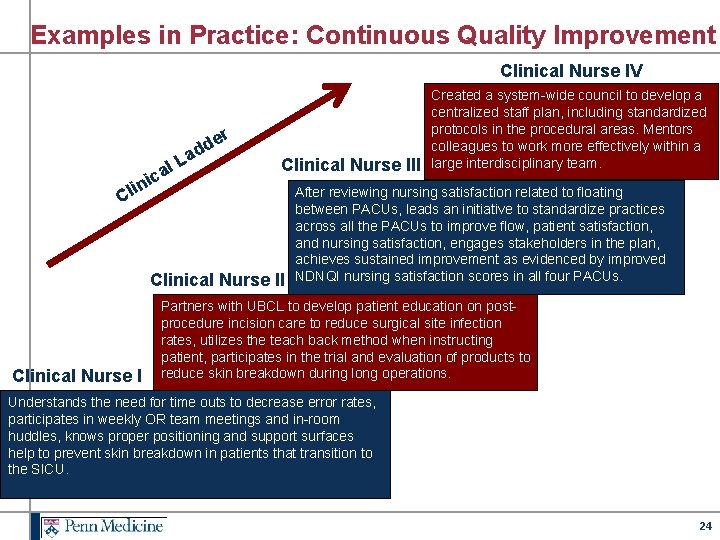
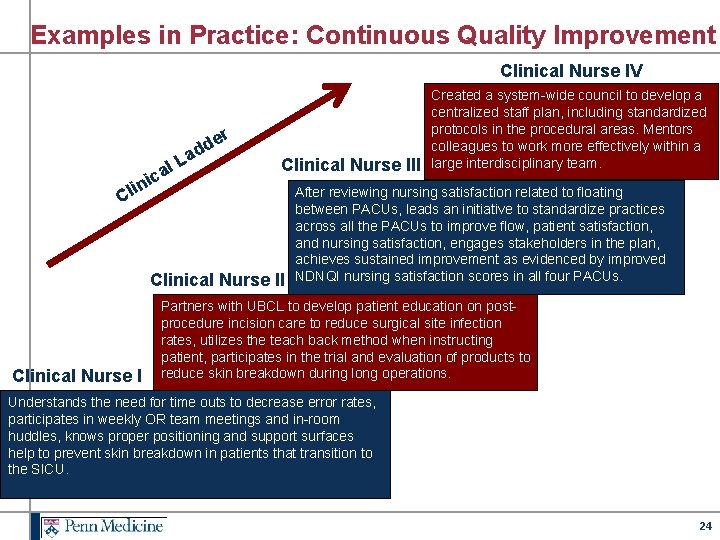
Examples in Practice: Continuous Quality Improvement Clinical Nurse IV r de d La al c i n Clinical Nurse III i Cl Clinical Nurse II Clinical Nurse I Created a system-wide council to develop a centralized staff plan, including standardized protocols in the procedural areas. Mentors colleagues to work more effectively within a large interdisciplinary team. After reviewing nursing satisfaction related to floating between PACUs, leads an initiative to standardize practices across all the PACUs to improve flow, patient satisfaction, and nursing satisfaction, engages stakeholders in the plan, achieves sustained improvement as evidenced by improved NDNQI nursing satisfaction scores in all four PACUs. Partners with UBCL to develop patient education on postprocedure incision care to reduce surgical site infection rates, utilizes the teach back method when instructing patient, participates in the trial and evaluation of products to reduce skin breakdown during long operations. Understands the need for time outs to decrease error rates, participates in weekly OR team meetings and in-room huddles, knows proper positioning and support surfaces help to prevent skin breakdown in patients that transition to the SICU. 24
Questions? A Special Thank You to the Penn Medicine Chief Nursing Officer Council for Supporting this Work Contact Information: Tonya. johnson@uphs. upenn. edu Christine. sites@uphs. upenn. edu Kathleen. burke@uphs. upenn. edu 25