Cryptococcosis Management of Raised Intracranial Pressure Prof David
![Association between therapeutic LP & acute mortality Only 1 LP [Diagnostic LP] Rolfes et Association between therapeutic LP & acute mortality Only 1 LP [Diagnostic LP] Rolfes et](https://slidetodoc.com/presentation_image_h2/e795a22e439fad179c0a70c389c1e047/image-7.jpg)

- Slides: 11
Cryptococcosis: Management of Raised Intracranial Pressure Prof. David W. Denning The University of Manchester, UK
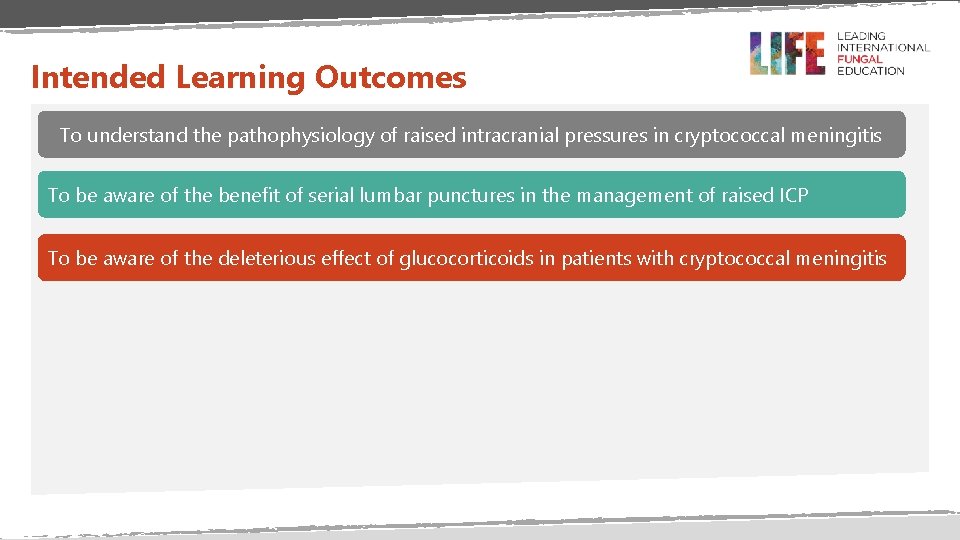
Intended Learning Outcomes To understand the pathophysiology of raised intracranial pressures in cryptococcal meningitis To be aware of the benefit of serial lumbar punctures in the management of raised ICP To be aware of the deleterious effect of glucocorticoids in patients with cryptococcal meningitis
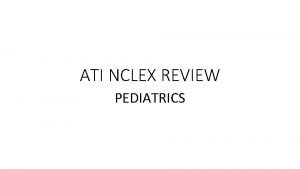
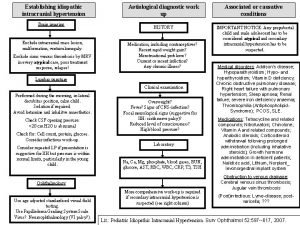
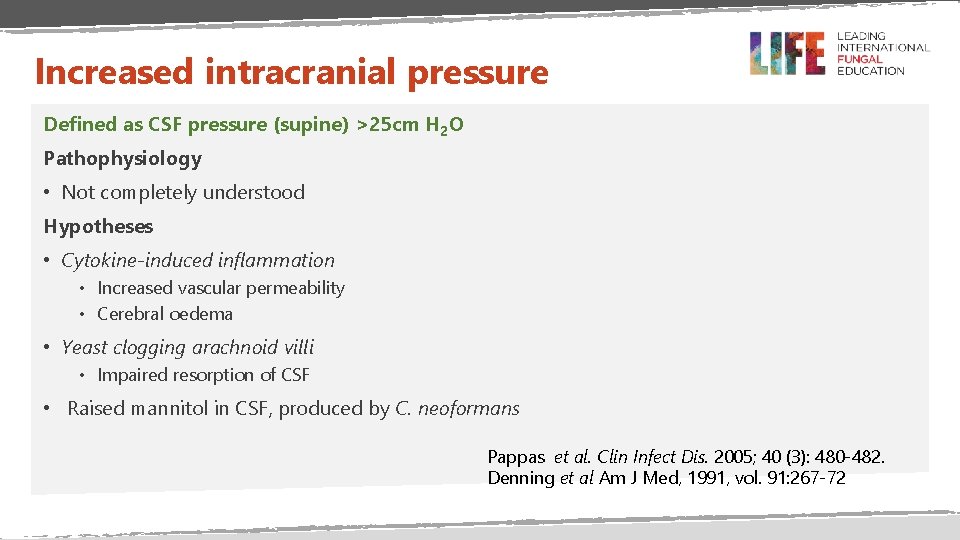
Increased intracranial pressure Defined as CSF pressure (supine) >25 cm H 2 O Pathophysiology • Not completely understood Hypotheses • Cytokine-induced inflammation • Increased vascular permeability • Cerebral oedema • Yeast clogging arachnoid villi • Impaired resorption of CSF • Raised mannitol in CSF, produced by C. neoformans Pappas et al. Clin Infect Dis. 2005; 40 (3): 480 -482. Denning et al Am J Med, 1991, vol. 91: 267 -72
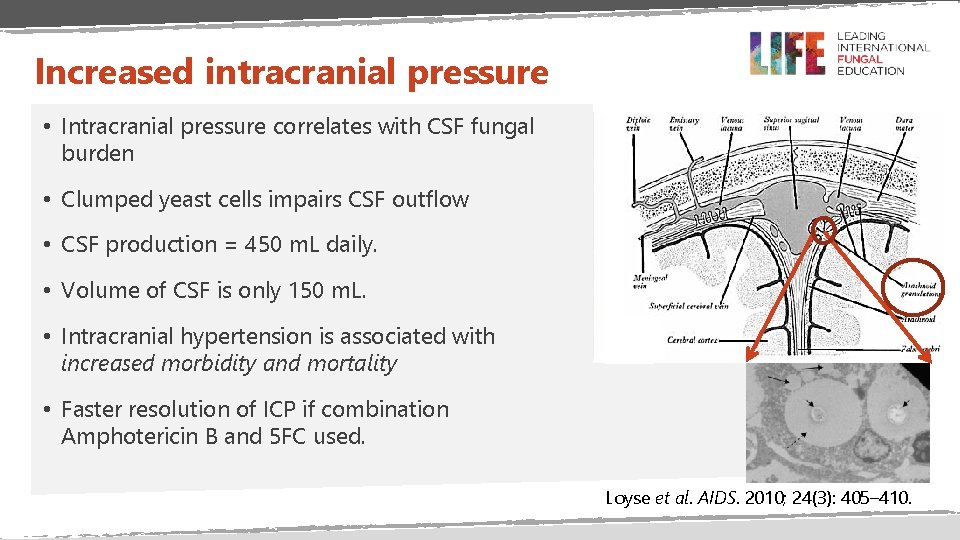
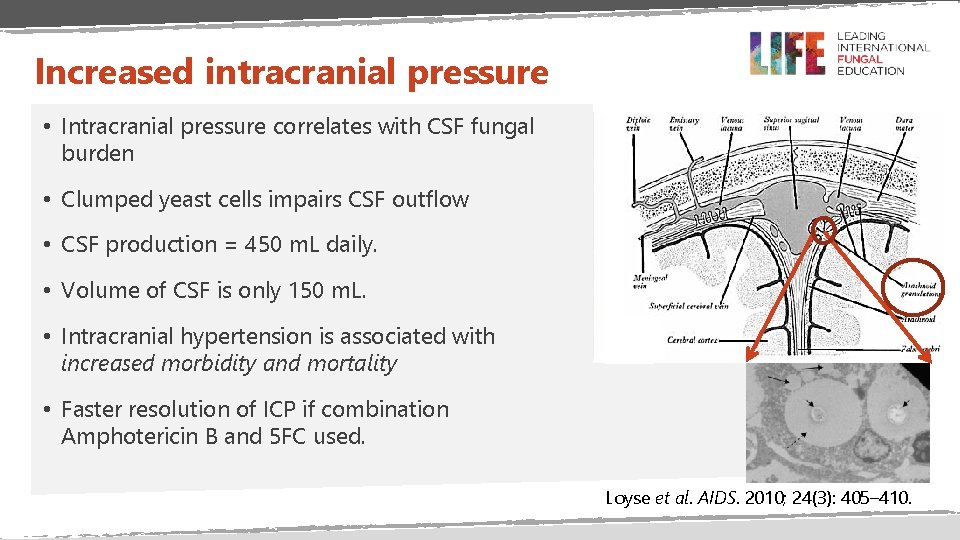
Increased intracranial pressure • Intracranial pressure correlates with CSF fungal burden • Clumped yeast cells impairs CSF outflow • CSF production = 450 m. L daily. • Volume of CSF is only 150 m. L. • Intracranial hypertension is associated with increased morbidity and mortality • Faster resolution of ICP if combination Amphotericin B and 5 FC used. Loyse et al. AIDS. 2010; 24(3): 405– 410.
Complications of raised ICP • Reduced consciousness - increasing risk from aspiration, low calorie and fluid intake • Early (and sometimes delayed) death • Visual loss (16 -32%) • Due to persistent papilledema • ? Direct invasion by Cryptococcus • Hearing loss (7 -17%) Bicanic & Harrison. British Medical Bulletin. 2004; 72 (1): 99– 118 Okun & Butler. Arch Ophthalmol. 1964; 71(1): 52 -57
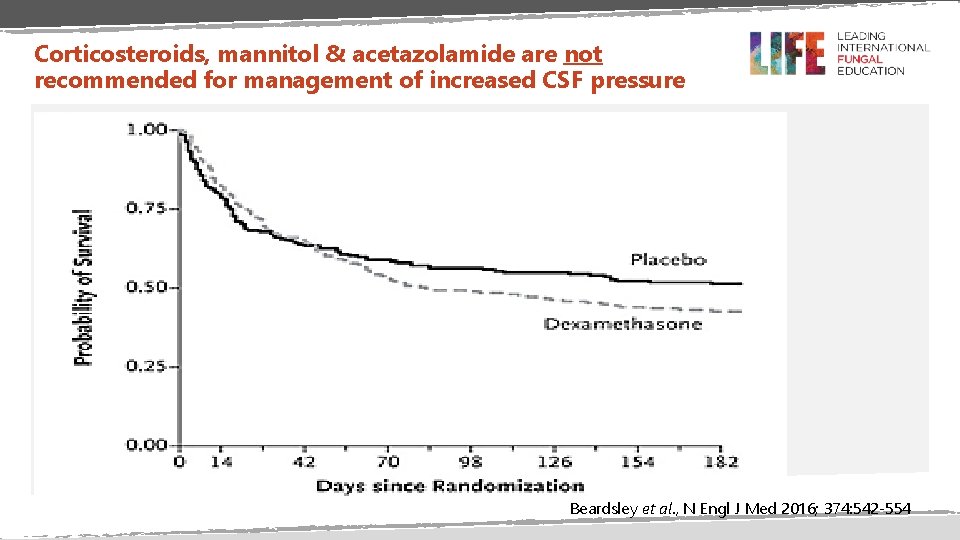
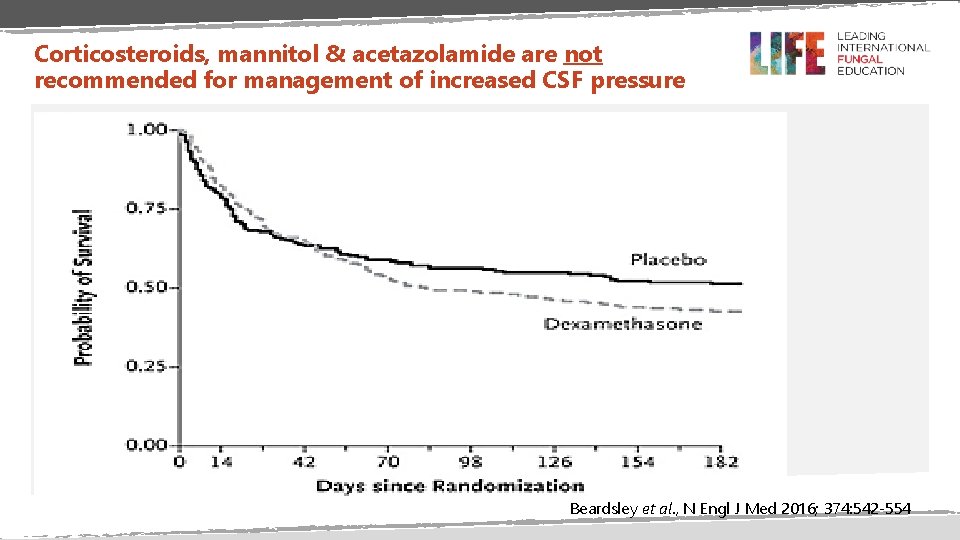
Corticosteroids, mannitol & acetazolamide are not recommended for management of increased CSF pressure Beardsley et al. , N Engl J Med 2016; 374: 542 -554
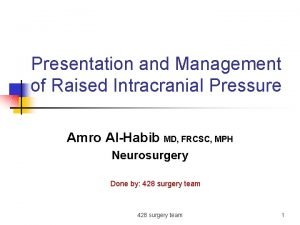
![Association between therapeutic LP acute mortality Only 1 LP Diagnostic LP Rolfes et Association between therapeutic LP & acute mortality Only 1 LP [Diagnostic LP] Rolfes et](https://slidetodoc.com/presentation_image_h2/e795a22e439fad179c0a70c389c1e047/image-7.jpg)
Association between therapeutic LP & acute mortality Only 1 LP [Diagnostic LP] Rolfes et al. Clin Infect Dis 2014; 58 (11); 1607 -1614
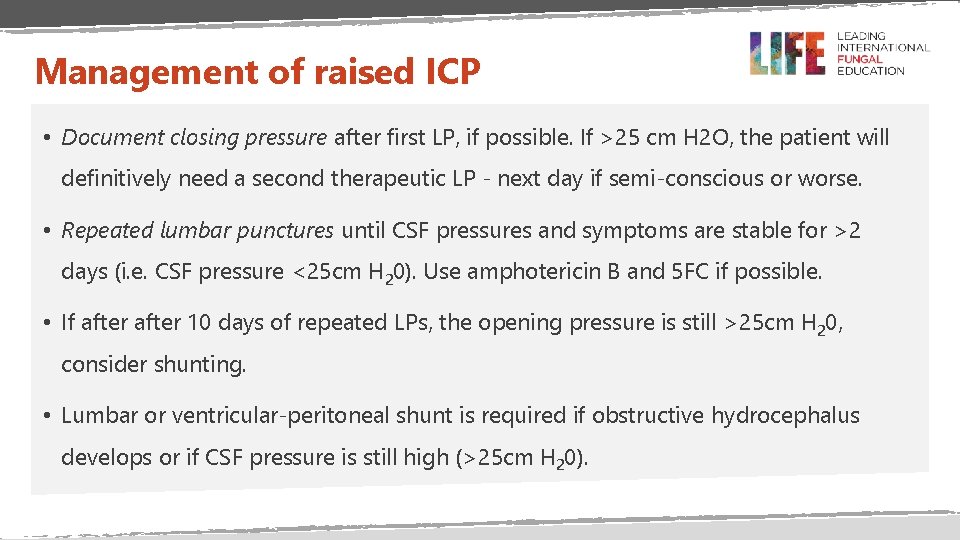
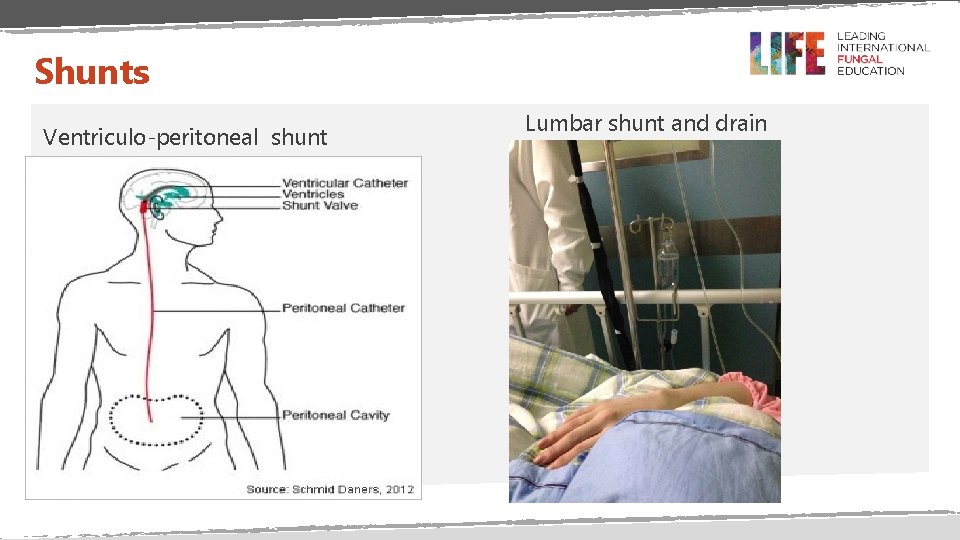
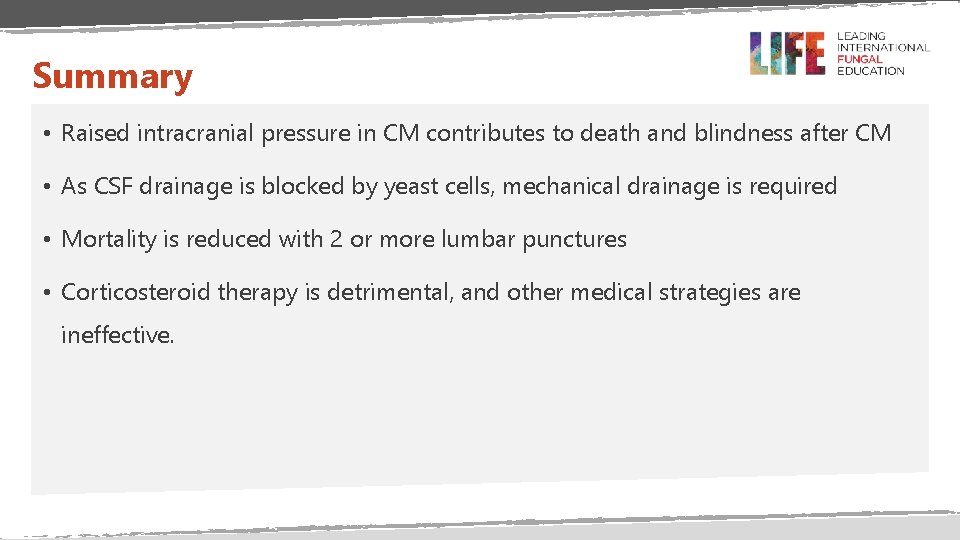
Management of raised ICP • Document closing pressure after first LP, if possible. If >25 cm H 2 O, the patient will definitively need a second therapeutic LP - next day if semi-conscious or worse. • Repeated lumbar punctures until CSF pressures and symptoms are stable for >2 days (i. e. CSF pressure <25 cm H 20). Use amphotericin B and 5 FC if possible. • If after 10 days of repeated LPs, the opening pressure is still >25 cm H 20, consider shunting. • Lumbar or ventricular-peritoneal shunt is required if obstructive hydrocephalus develops or if CSF pressure is still high (>25 cm H 20).
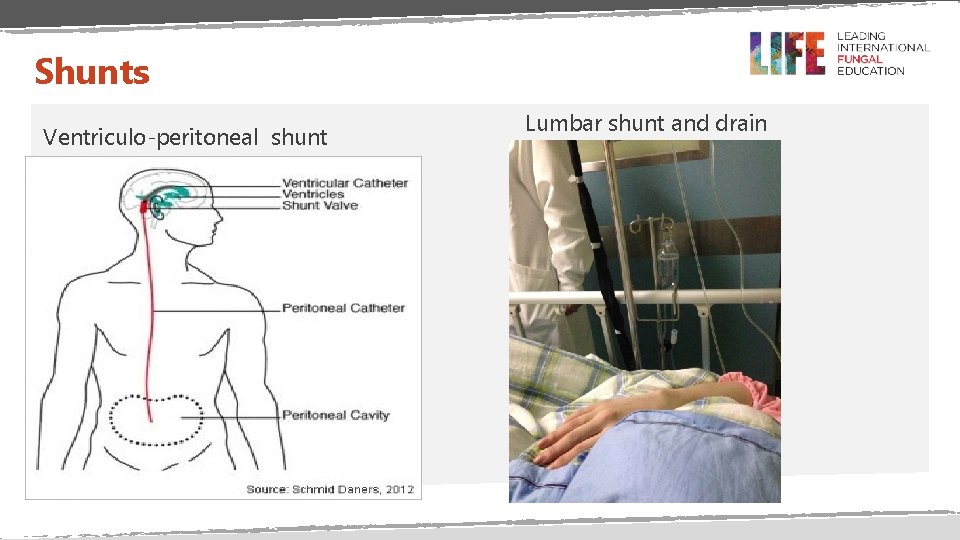
Shunts Ventriculo-peritoneal shunt Lumbar shunt and drain
Summary • Raised intracranial pressure in CM contributes to death and blindness after CM • As CSF drainage is blocked by yeast cells, mechanical drainage is required • Mortality is reduced with 2 or more lumbar punctures • Corticosteroid therapy is detrimental, and other medical strategies are ineffective.

END