Cryptococcosis Antifungal therapy management Prof Thomas S Harrison

- Slides: 16
Cryptococcosis: Antifungal therapy management Prof. Thomas S. Harrison Centre for Global Health, Institute of Infection and Immunity St. George’s, University of London; St George's University Hospitals NHS Foundation Trust
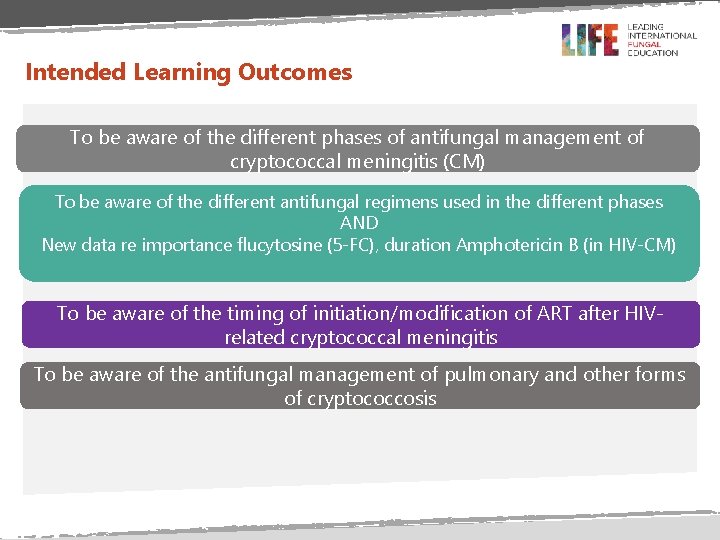
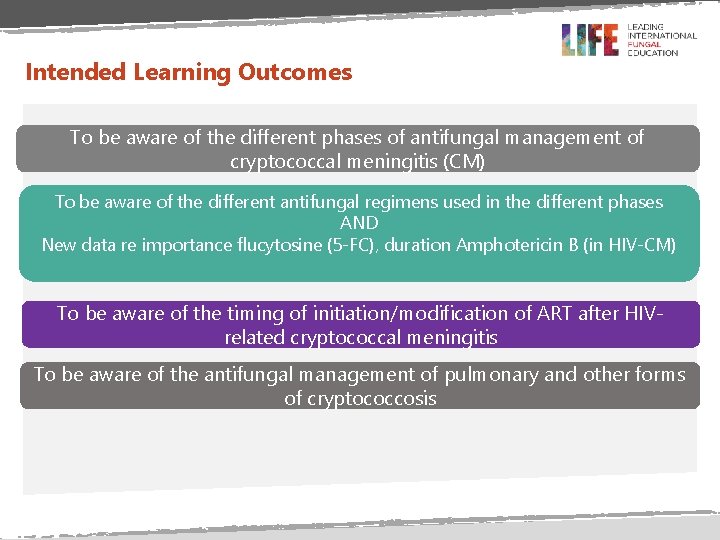
Intended Learning Outcomes To be aware of the different phases of antifungal management of cryptococcal meningitis (CM) To be aware of the different antifungal regimens used in the different phases AND New data re importance flucytosine (5 -FC), duration Amphotericin B (in HIV-CM) To be aware of the timing of initiation/modification of ART after HIVrelated cryptococcal meningitis To be aware of the antifungal management of pulmonary and other forms of cryptococcosis
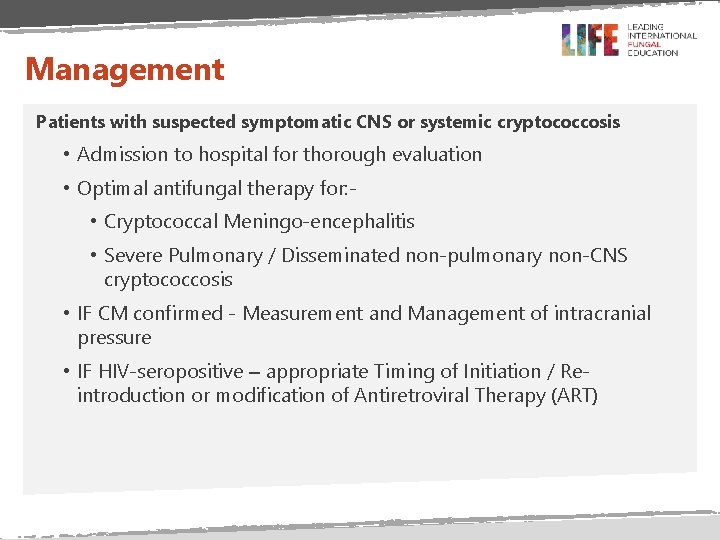
Management Patients with suspected symptomatic CNS or systemic cryptococcosis • Admission to hospital for thorough evaluation • Optimal antifungal therapy for: • Cryptococcal Meningo-encephalitis • Severe Pulmonary / Disseminated non-pulmonary non-CNS cryptococcosis • IF CM confirmed - Measurement and Management of intracranial pressure • IF HIV-seropositive – appropriate Timing of Initiation / Reintroduction or modification of Antiretroviral Therapy (ART)
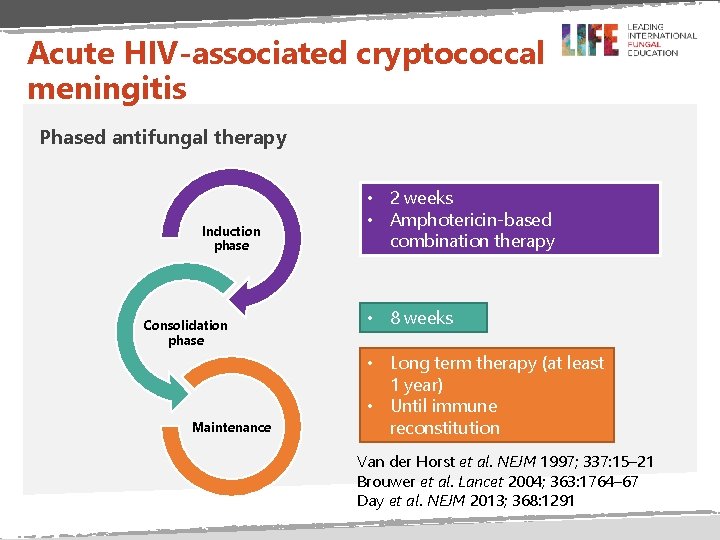
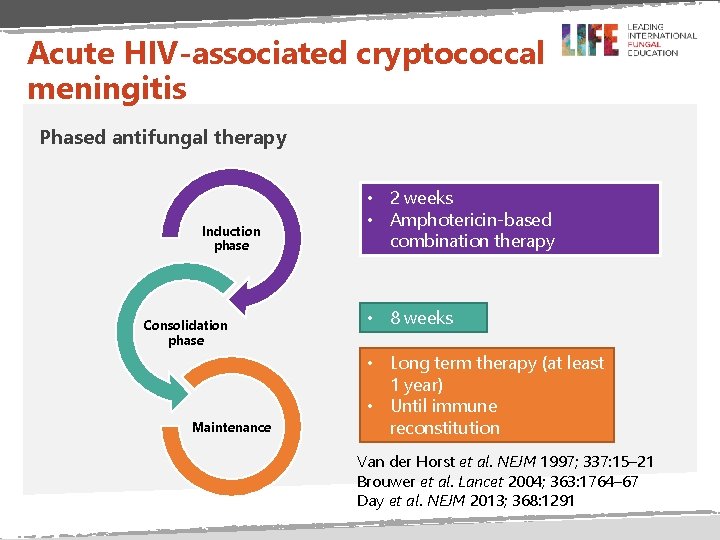
Acute HIV-associated cryptococcal meningitis Phased antifungal therapy Induction phase Consolidation phase Maintenance • 2 weeks • Amphotericin-based combination therapy • 8 weeks • Long term therapy (at least 1 year) • Until immune reconstitution Van der Horst et al. NEJM 1997; 337: 15– 21 Brouwer et al. Lancet 2004; 363: 1764– 67 Day et al. NEJM 2013; 368: 1291
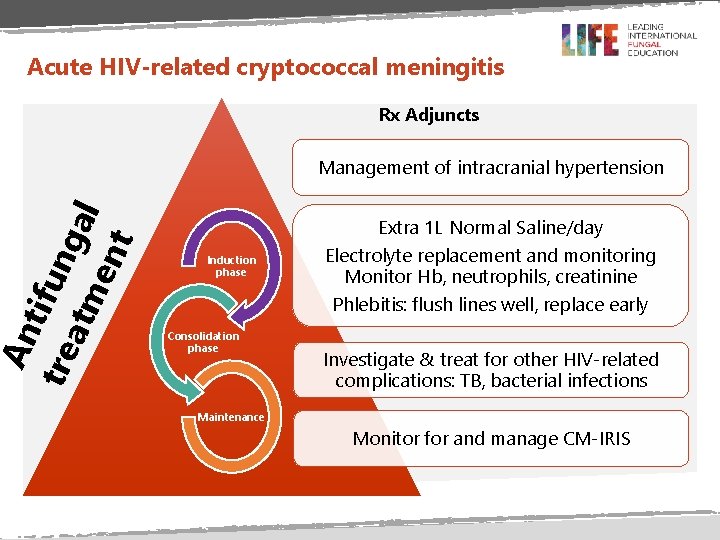
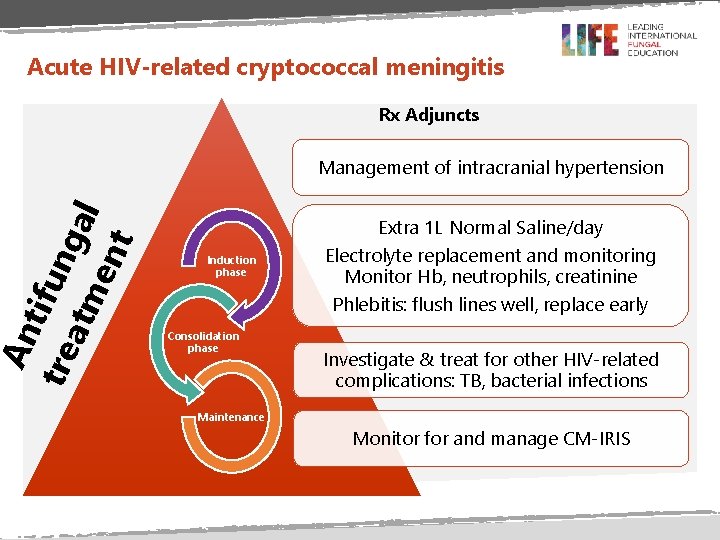
An tifu tre atm ngal ent Acute HIV-related cryptococcal meningitis Rx Adjuncts Management of intracranial hypertension Extra 1 L Normal Saline/day Induction phase Consolidation phase Electrolyte replacement and monitoring Monitor Hb, neutrophils, creatinine Phlebitis: flush lines well, replace early Investigate & treat for other HIV-related complications: TB, bacterial infections Maintenance Monitor for and manage CM-IRIS
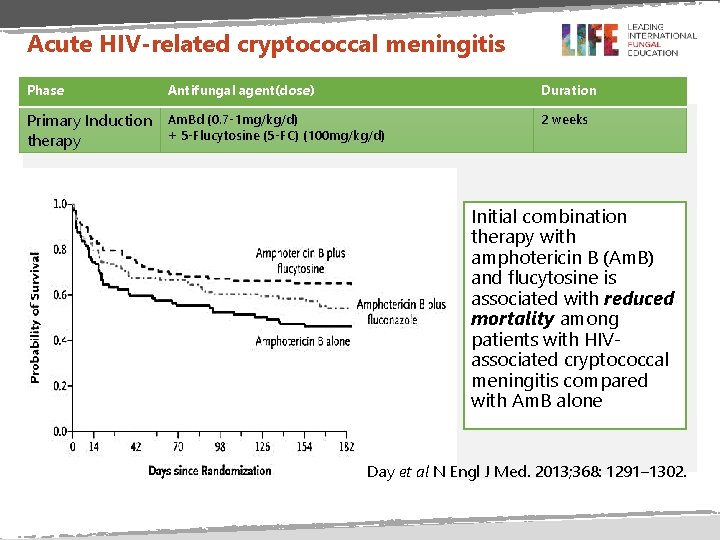
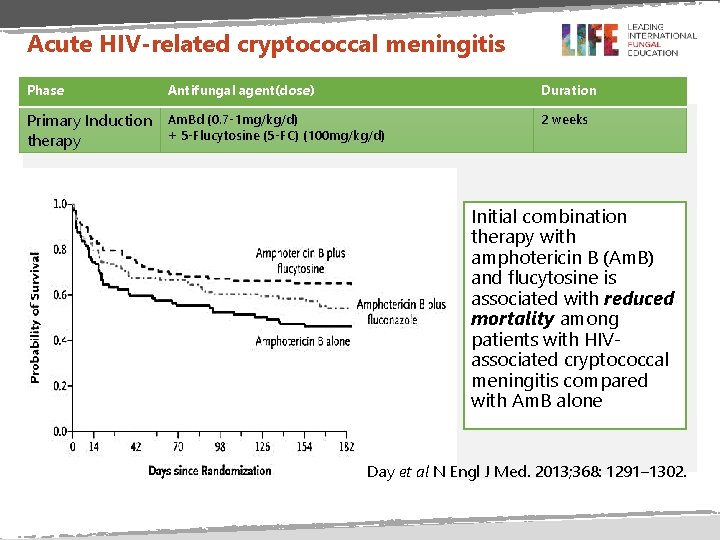
Acute HIV-related cryptococcal meningitis Phase Antifungal agent(dose) Duration Primary Induction therapy Am. Bd (0. 7 -1 mg/kg/d) + 5 -Flucytosine (5 -FC) (100 mg/kg/d) 2 weeks Initial combination therapy with amphotericin B (Am. B) and flucytosine is associated with reduced mortality among patients with HIVassociated cryptococcal meningitis compared with Am. B alone Day et al N Engl J Med. 2013; 368: 1291– 1302.
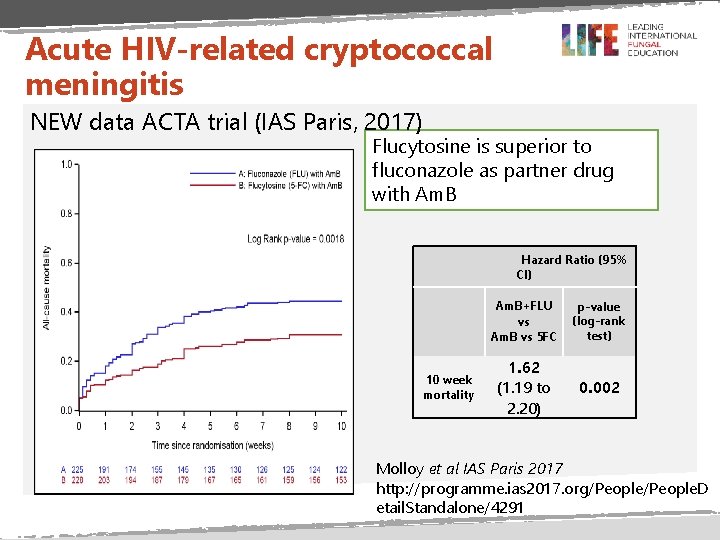
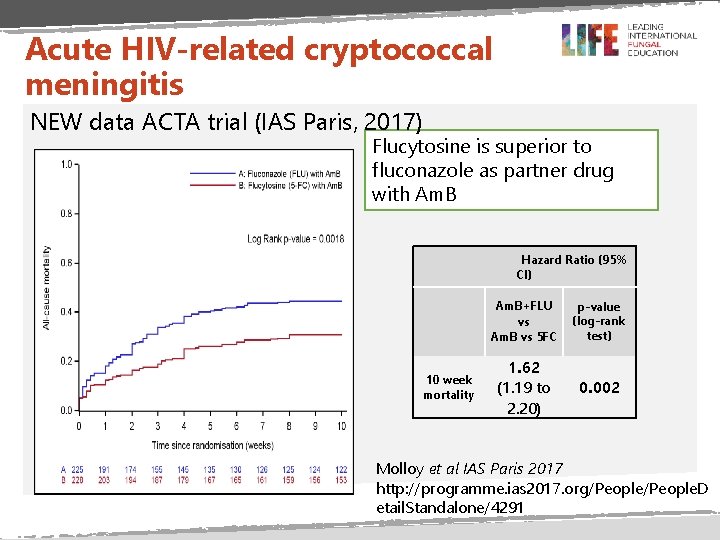
Acute HIV-related cryptococcal meningitis NEW data ACTA trial (IAS Paris, 2017) Flucytosine is superior to fluconazole as partner drug with Am. B Hazard Ratio (95% CI) 10 week mortality Am. B+FLU vs Am. B vs 5 FC p-value (log-rank test) 1. 62 (1. 19 to 2. 20) 0. 002 Molloy et al IAS Paris 2017 http: //programme. ias 2017. org/People. D etail. Standalone/4291
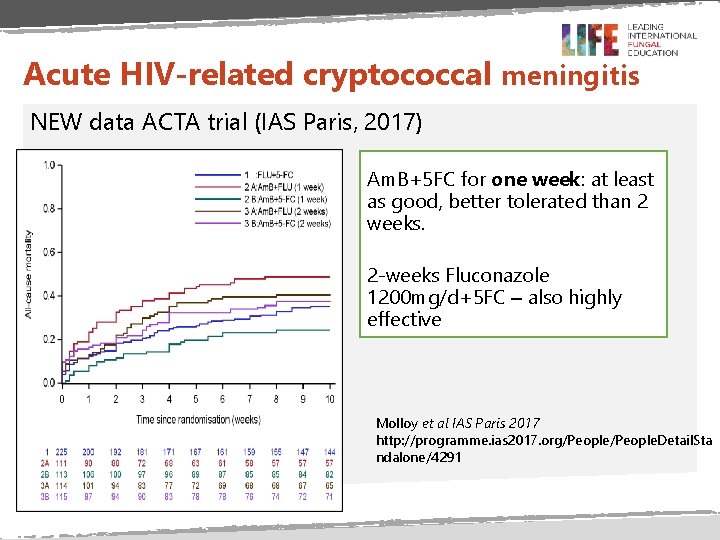
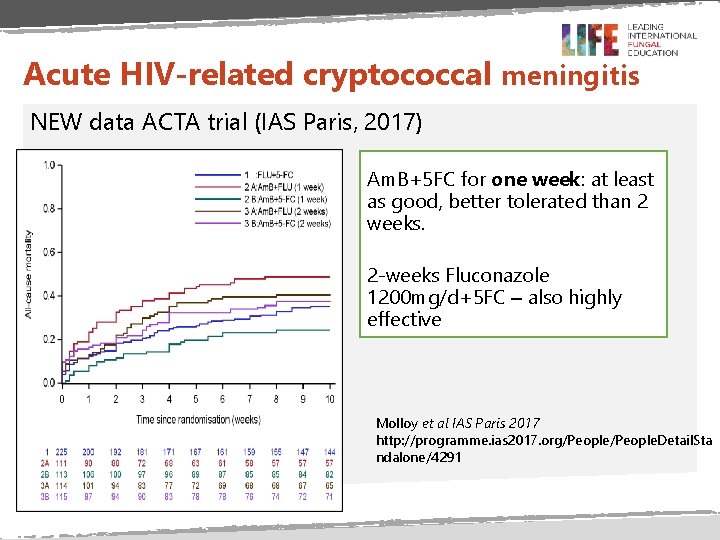
Acute HIV-related cryptococcal meningitis NEW data ACTA trial (IAS Paris, 2017) Am. B+5 FC for one week: at least as good, better tolerated than 2 weeks. 2 -weeks Fluconazole 1200 mg/d+5 FC – also highly effective Molloy et al IAS Paris 2017 http: //programme. ias 2017. org/People. Detail. Sta ndalone/4291
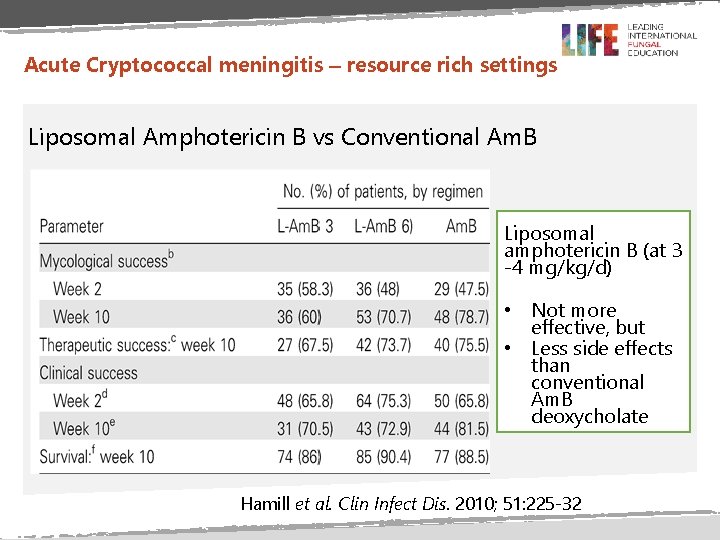
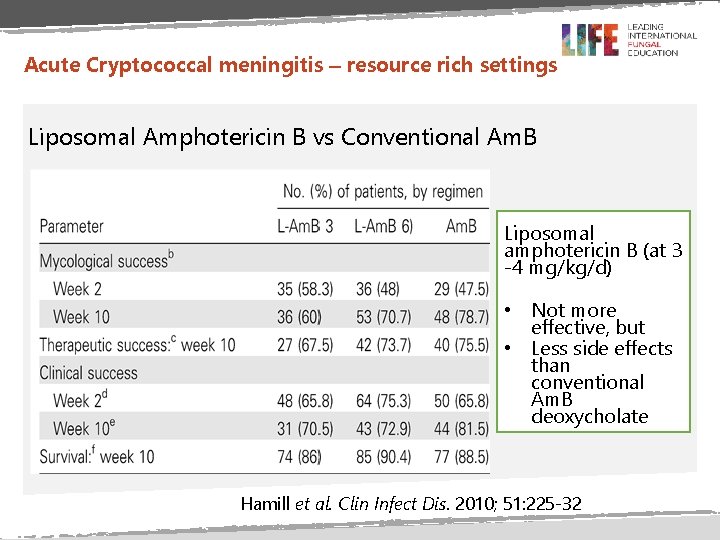
Acute Cryptococcal meningitis – resource rich settings Liposomal Amphotericin B vs Conventional Am. B Liposomal amphotericin B (at 3 -4 mg/kg/d) • Not more effective, but • Less side effects than conventional Am. B deoxycholate Hamill et al. Clin Infect Dis. 2010; 51: 225 -32
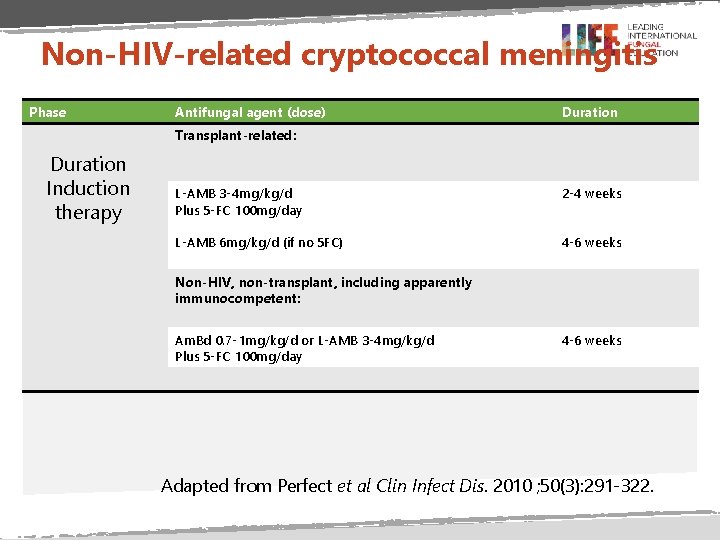
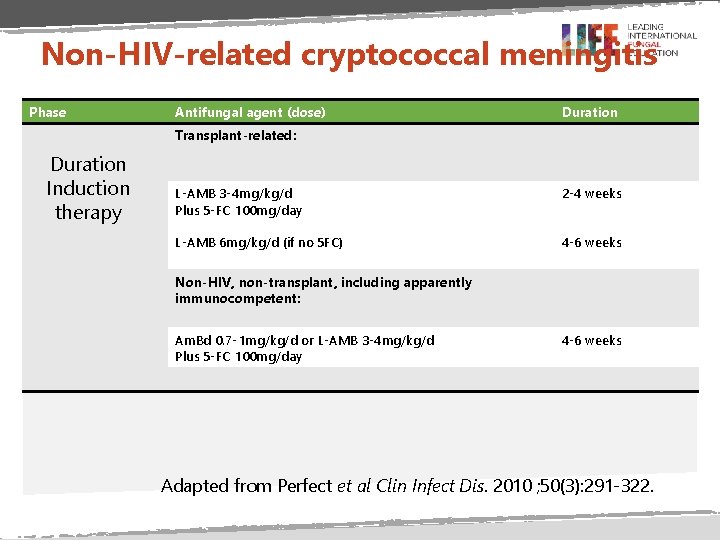
Non-HIV-related cryptococcal meningitis Phase Antifungal agent (dose) Duration Transplant-related: Duration Induction therapy L-AMB 3 -4 mg/kg/d Plus 5 -FC 100 mg/day 2 -4 weeks L-AMB 6 mg/kg/d (if no 5 FC) 4 -6 weeks Non-HIV, non-transplant, including apparently immunocompetent: Am. Bd 0. 7 -1 mg/kg/d or L-AMB 3 -4 mg/kg/d Plus 5 -FC 100 mg/day 4 -6 weeks Adapted from Perfect et al Clin Infect Dis. 2010 ; 50(3): 291 -322.
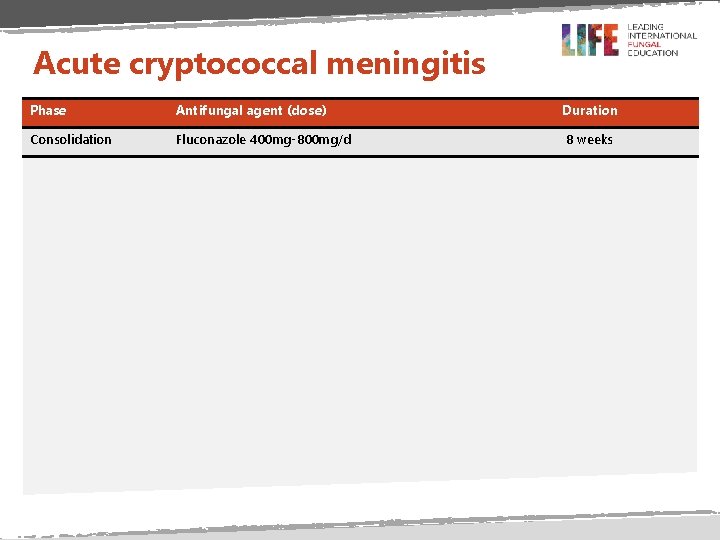
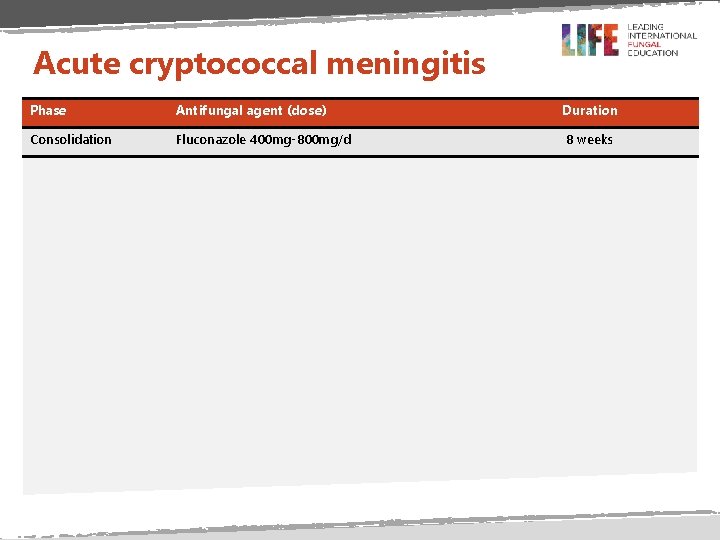
Acute cryptococcal meningitis Phase Antifungal agent (dose) Duration Consolidation Fluconazole 400 mg-800 mg/d 8 weeks
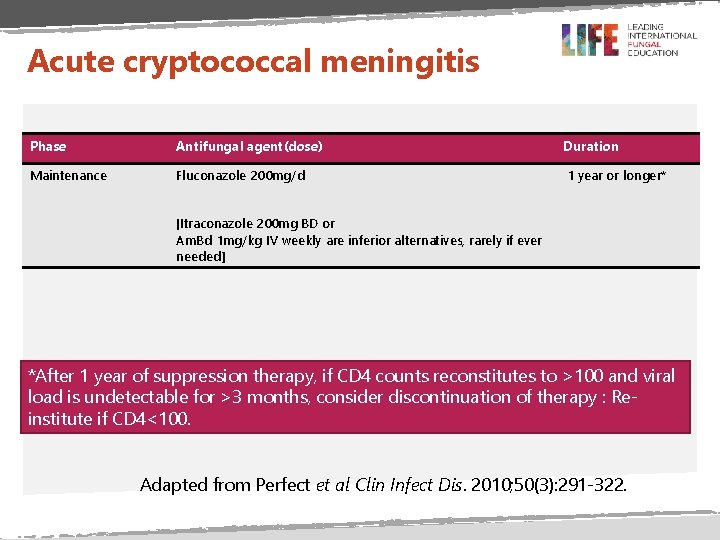
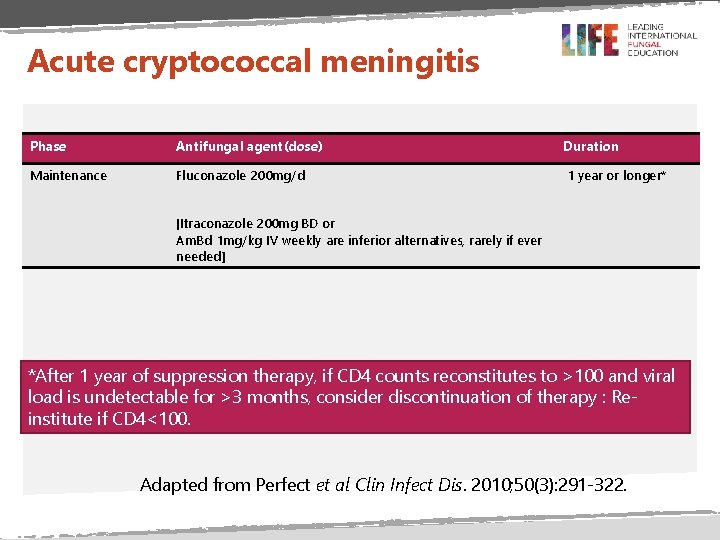
Acute cryptococcal meningitis Phase Antifungal agent(dose) Duration Maintenance Fluconazole 200 mg/d 1 year or longer* [Itraconazole 200 mg BD or Am. Bd 1 mg/kg IV weekly are inferior alternatives, rarely if ever needed] *After 1 year of suppression therapy, if CD 4 counts reconstitutes to >100 and viral load is undetectable for >3 months, consider discontinuation of therapy : Reinstitute if CD 4<100. Adapted from Perfect et al Clin Infect Dis. 2010; 50(3): 291 -322.
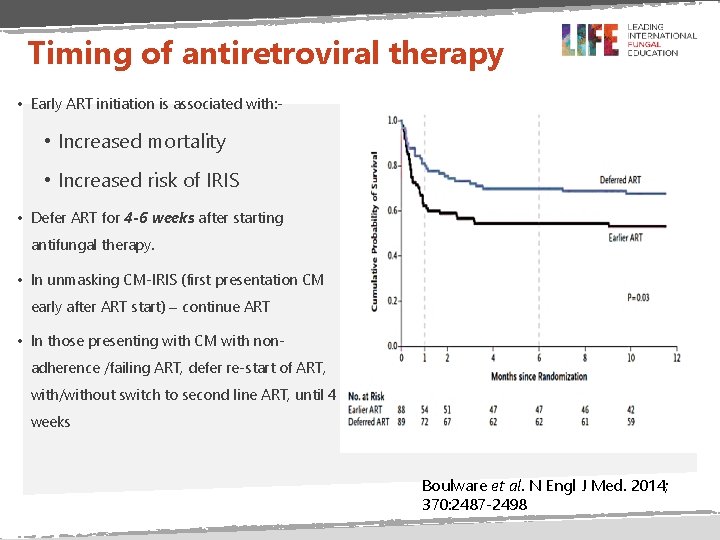
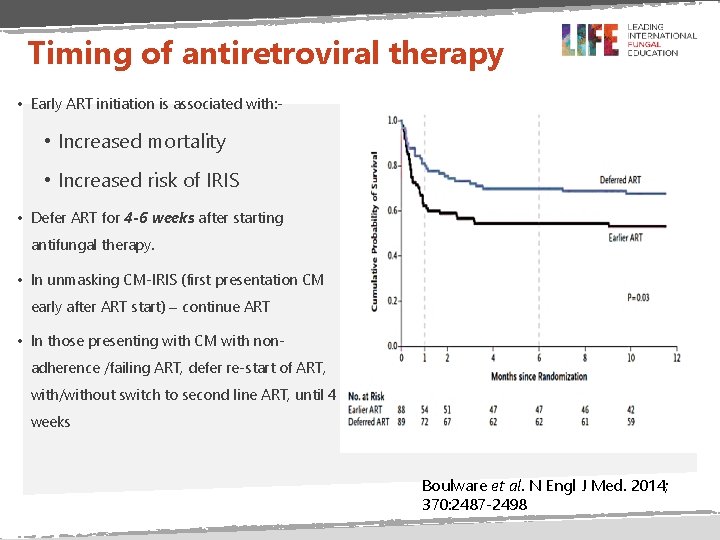
Timing of antiretroviral therapy • Early ART initiation is associated with: - • Increased mortality • Increased risk of IRIS • Defer ART for 4 -6 weeks after starting antifungal therapy. • In unmasking CM-IRIS (first presentation CM early after ART start) – continue ART • In those presenting with CM with nonadherence /failing ART, defer re-start of ART, with/without switch to second line ART, until 4 weeks Boulware et al. N Engl J Med. 2014; 370: 2487 -2498
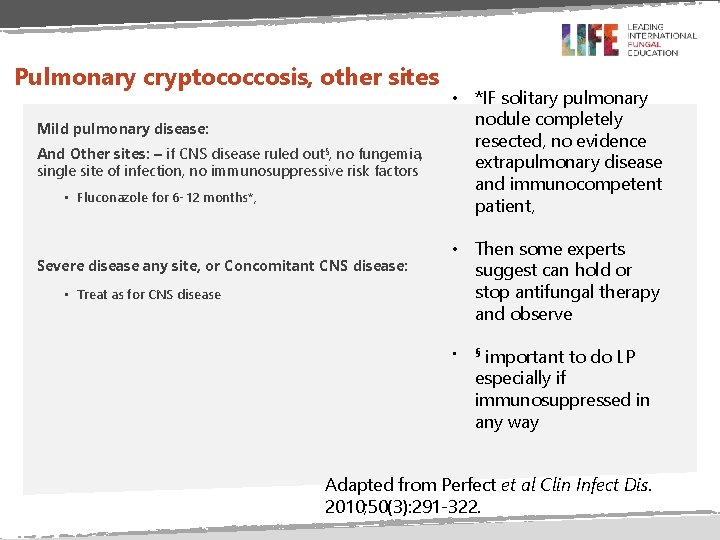
Pulmonary cryptococcosis, other sites Mild pulmonary disease: And Other sites: – if CNS disease ruled out§, no fungemia, single site of infection, no immunosuppressive risk factors • Fluconazole for 6 -12 months*, Severe disease any site, or Concomitant CNS disease: • Treat as for CNS disease • *IF solitary pulmonary nodule completely resected, no evidence extrapulmonary disease and immunocompetent patient, • Then some experts suggest can hold or stop antifungal therapy and observe • important to do LP especially if immunosuppressed in any way § Adapted from Perfect et al Clin Infect Dis. 2010; 50(3): 291 -322.
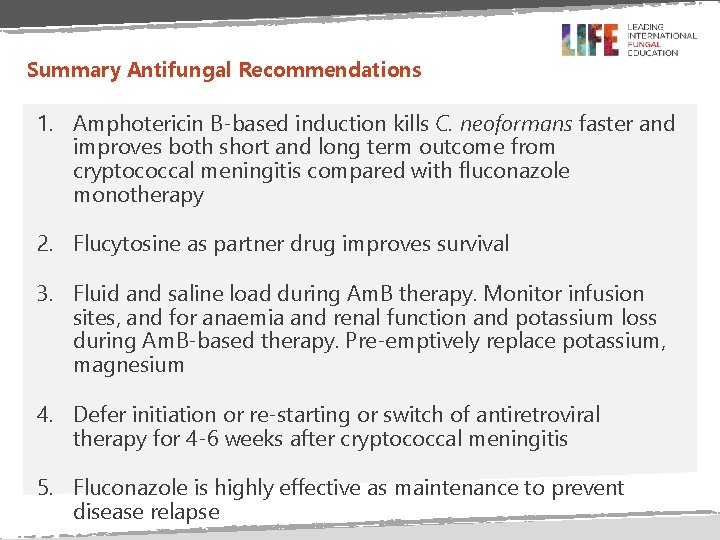
Summary Antifungal Recommendations 1. Amphotericin B-based induction kills C. neoformans faster and improves both short and long term outcome from cryptococcal meningitis compared with fluconazole monotherapy 2. Flucytosine as partner drug improves survival 3. Fluid and saline load during Am. B therapy. Monitor infusion sites, and for anaemia and renal function and potassium loss during Am. B-based therapy. Pre-emptively replace potassium, magnesium 4. Defer initiation or re-starting or switch of antiretroviral therapy for 4 -6 weeks after cryptococcal meningitis 5. Fluconazole is highly effective as maintenance to prevent disease relapse

END
 Theme of harrison bergeron
Theme of harrison bergeron Antifungal drugs classification
Antifungal drugs classification Types of antifungal drugs
Types of antifungal drugs Capsofungin
Capsofungin Dr.saeed ahmed
Dr.saeed ahmed Antifungal sensitivity test
Antifungal sensitivity test Thrush creams boots
Thrush creams boots Both psychoanalysis and humanistic therapy stress
Both psychoanalysis and humanistic therapy stress Bioness bits cost
Bioness bits cost Psychoanalytic therapy is to as humanistic therapy is to
Psychoanalytic therapy is to as humanistic therapy is to Thomas mocker and thomas stewart
Thomas mocker and thomas stewart Drug therapy management
Drug therapy management Leiderschapsstijlen
Leiderschapsstijlen Reuven harrison
Reuven harrison Ted harrison northern lights
Ted harrison northern lights Harrison benedict formula
Harrison benedict formula Harrisons sulci
Harrisons sulci