CRITICAL CARE VICTORIA STANDARDISED INOTROPES VASOPRESSORS IMPLEMENTATION PROJECT


- Slides: 12
CRITICAL CARE VICTORIA STANDARDISED INOTROPES & VASOPRESSORS IMPLEMENTATION PROJECT MR SHAUN VESEY – AUM INTENSIVE CARE UNIT SOUTH WEST HEALTHCARE, WARRNAMBOOL.
STANDARDISED INOTROPES & VASOPRESSORS IMPLEMENTATION PROJECT: OVERVIEW OF PILOT PROGRAMME The Critical Care Network (CCCN) work with critical care clinicians to improve the quality of care/patient experiences in Vic ICU/HD units. 41 public & private critical care units across regional/metropolitan areas. Work with numerous groups (Better/ Safer Care Victoria, Dept. of Human Services, ‘consumers’/communities – To provide coordinated, quality, supported care initiatives. )
STANDARDISED INOTROPES & VASOPRESSORS IMPLEMENTATION PROJECT In 2016 the ACCCN in conjunction with a number of Vic ICUs identified the need to standardize the central administration of inotropes and vasopressors. Ultimate aim: To ‘streamline’ protocols (Limit variables - “We do this” approach) Reduce medication errors Reduce patient harm Up to date practices, evidenced based, relevant across state. STANDARDIZE PRACTICE ** Out of date info/evidence** “I have worked across various units and noticed considerable inotrope/vasporessor practice variations”. Example: Removal volumes on set up of inotropes. Transfer protocols etc.
WHY, WHY ………. . STANDARDISATION ……. . AIM IS SAFETY ACROSS Victorian ICUs/CCUs, the Critical Care Network identified the immense variation in inotrope/vasopressor practices: Examples: For 6 different inotrope medications, 16 different infusion concentrations are utilized? ? For 3 vasopressor medications, 11 different infusions concentrations are utilized? ? Numerous variations in how medications are prepared? ? Different types of fluids utilized/why? ? Different starting levels, dosage limits etc. ? ? Variations in practices b/w organisations? ? (ARV transfers).
STANDARDISED INOTROPES & VASOPRESSORS IMPLEMENTATION PROJECT Intensive care at SWH is a chosen pilot hospital that has been working with multi disciplinary groups/healthcare organisations and the BCV network to implement a pilot program centered around standardizing our inotrope/vasopressor guidelines. Numerous hospital and stakeholders involved in pilot: SWH (AE, theatre, Camperdown), University Hospital Geelong ICU, Austin ICU, Epworth eastern ICU, Peninsula Health, Werribee (new ICU), ARV. * SWH Inclusive: Theatre, AE, AV not al sites etc. Team Members/stakeholders: Executive board Director Med/Nursing Craig Fraser, Julianne Clift Mark Page ICU Director SWH Tina Johnstone NUM ICU SWH Sue Bagg ANUM ICU SWH Shaun Vesey ANUM ICU SWH Suzanne Staude Pharmacist/Project manager BCV

STANDARDISED INOTROPES & VASOPRESSORS IMPLEMENTATION PROJECT Similarly to majority of projects ‘behind the scenes’ planning and implementation has been occurring: Initial acceptance into pilot program Acceptance/support from board/Hospital directors Formation of stakeholders/Pilot program group Administrative planning, What, Where, When, Who, How approach Pre Data collection/findings Network pilot planning meeting (Involving numerous pilot groups) Implementation phase (change in protocols, change in clinical practice, staff education ) Implementation/Post data collection, findings collected and evaluated (Audit bedside data/admin, examination issues etc. ) Implement changes safely across Victoria.
SO GIVE ME THE FACTS Go LIVE MONDAY 6 th AUGUST PRIMARILY INVOLVES X 9 MEDICATIONS Relevantly straight forward changes, overall smaller patient groups than tertiary centers, smaller numbers of pts requiring inotropes/vasopressors etc. Recognised that our current practices are overall solid. However, relatively small changes to be noted. Example: Dobutamine and Aramine were main 2 medications that we had significant differences over pilot recommendations. Example: Variant with our solution uses (sometimes sodium chloride 0. 9% Vs dextrose 5%).
SO GIVE ME THE FACTS Majority of staff please get involved: (No major admin jobs!!). Communication of info/presentation on pilot so all staff aware. BCV expects 80% staff informed. Alaris Networks updated: Changes of dosages, Volumes, soft/hard limits as required. Pilot protocols have been formalized/be available to go live (a lot work). Refer to Pilot study notice board info on project. Be aware of info sent via email. Primary stakeholders available to refer too. Developed cheat sheet/clinical Lanyard with primary information. Pilot Learning package will be available (refresher info if required). Open to all ideas to spread info widely and accurately.
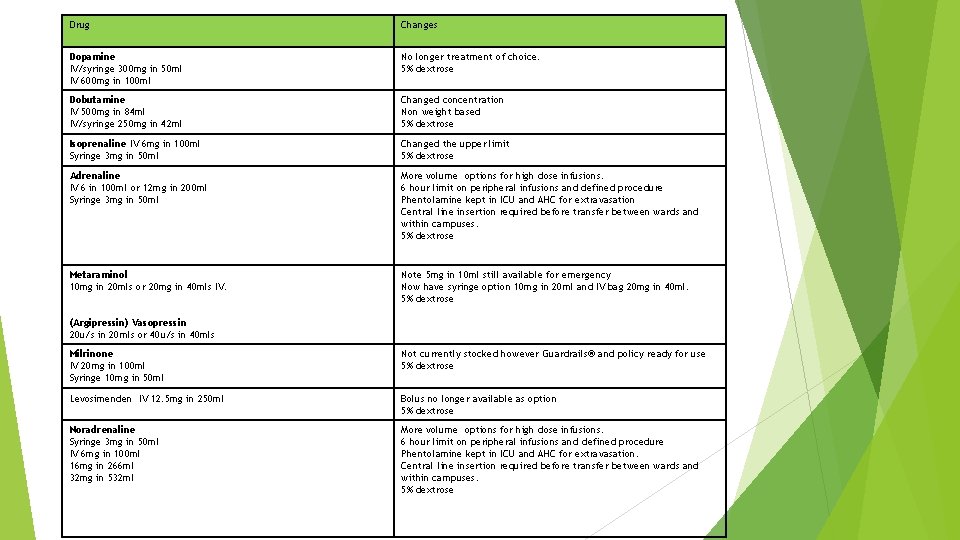
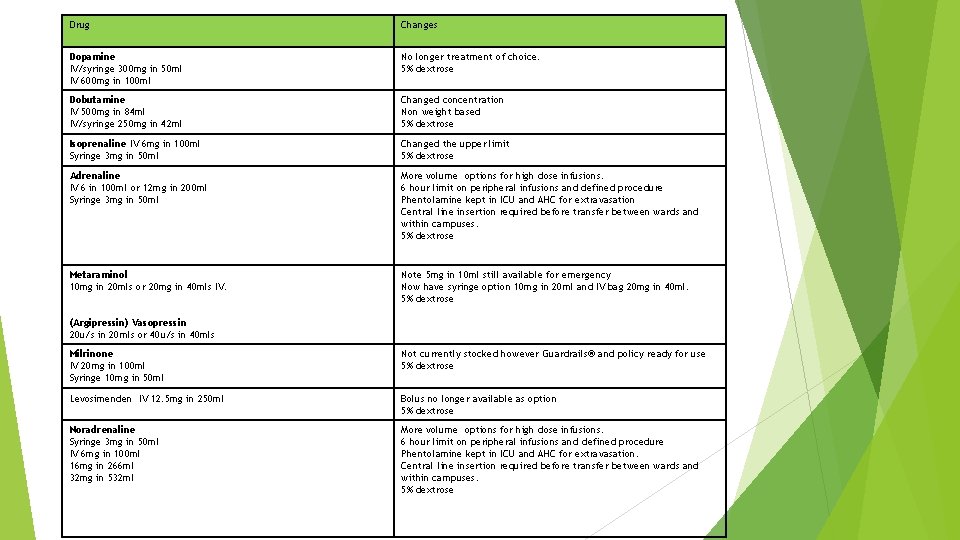
Drug Changes Dopamine IV/syringe 300 mg in 50 ml IV 600 mg in 100 ml No longer treatment of choice. 5% dextrose Dobutamine IV 500 mg in 84 ml IV/syringe 250 mg in 42 ml Changed concentration Non weight based 5% dextrose Isoprenaline IV 6 mg in 100 ml Syringe 3 mg in 50 ml Changed the upper limit 5% dextrose Adrenaline IV 6 in 100 ml or 12 mg in 200 ml Syringe 3 mg in 50 ml More volume options for high dose infusions. 6 hour limit on peripheral infusions and defined procedure Phentolamine kept in ICU and AHC for extravasation Central line insertion required before transfer between wards and within campuses. 5% dextrose Metaraminol 10 mg in 20 mls or 20 mg in 40 mls IV. Note 5 mg in 10 ml still available for emergency Now have syringe option 10 mg in 20 ml and IV bag 20 mg in 40 ml. 5% dextrose (Argipressin) Vasopressin 20 u/s in 20 mls or 40 u/s in 40 mls Milrinone IV 20 mg in 100 ml Syringe 10 mg in 50 ml Not currently stocked however Guardrails® and policy ready for use 5% dextrose Levosimenden IV 12. 5 mg in 250 ml Bolus no longer available as option 5% dextrose Noradrenaline Syringe 3 mg in 50 ml IV 6 mg in 100 ml 16 mg in 266 ml 32 mg in 532 ml More volume options for high dose infusions. 6 hour limit on peripheral infusions and defined procedure Phentolamine kept in ICU and AHC for extravasation. Central line insertion required before transfer between wards and within campuses. 5% dextrose
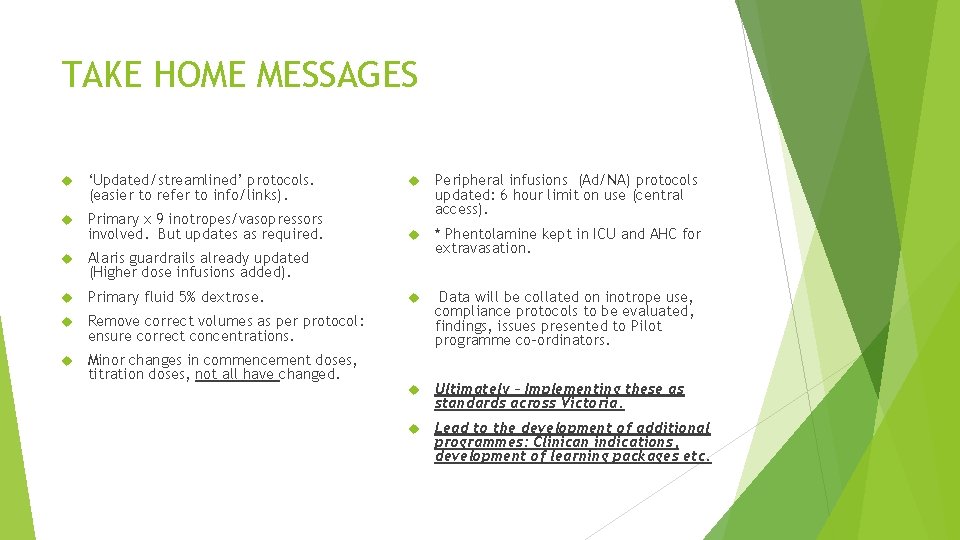
TAKE HOME MESSAGES ‘Updated/streamlined’ protocols. (easier to refer to info/links). Primary x 9 inotropes/vasopressors involved. But updates as required. Alaris guardrails already updated (Higher dose infusions added). Primary fluid 5% dextrose. Remove correct volumes as per protocol: ensure correct concentrations. Minor changes in commencement doses, titration doses, not all have changed. Peripheral infusions (Ad/NA) protocols updated: 6 hour limit on use (central access). * Phentolamine kept in ICU and AHC for extravasation. Data will be collated on inotrope use, compliance protocols to be evaluated, findings, issues presented to Pilot programme co-ordinators. Ultimately – Implementing these as standards across Victoria. Lead to the development of additional programmes: Clinican indications, development of learning packages etc.

DEVELOPMENT OF LANYARD CARD/SUMMARY WHAT ARE YOUR VIEWS? IT IS VALUED? ? WHAT INFO DO YOU WANT? ? HOW SHOULD IT BE STRUCTURED/PRESENTED? ?
QUESTIONS? ?
 Type of vasopressors
Type of vasopressors Inotropes examples
Inotropes examples Negative inotropic drugs
Negative inotropic drugs Inotropes drugs
Inotropes drugs Critical semi critical and non critical instruments
Critical semi critical and non critical instruments Critical semi critical and non critical instruments
Critical semi critical and non critical instruments Habitos de la victoria privada
Habitos de la victoria privada Standardised inotrope and vasopressor guidelines
Standardised inotrope and vasopressor guidelines Sera rules
Sera rules Molecular response
Molecular response Pmcv cv template
Pmcv cv template Primary secondary tertiary care
Primary secondary tertiary care Safer care victoria
Safer care victoria