Connector Appeals Program January 15 2009 Jamie Katz
- Slides: 16
Connector Appeals Program January 15, 2009 Jamie Katz
Overview • Mandate Penalty Appeals • MCC Determinations • Commonwealth Care Appeals 2 January 15, 2009
Overview • Appeals Unit volume grew dramatically between 2007 and 2008 due to Mandate Appeals and Commonwealth Care Appeals • Numbers are approximate due to complications in counting 3 January 15, 2009
Mandate Appeals Process • Mandate Appeals process a hidden success in 2008 – Brand new process involving different state agencies with no legal precedent – Modest consumer confusion or resistance – General compliance--most penalized individuals paid and most appellants who pursued appeal prevailed – Virtually all appeals resolved within 2008 – Hearings operated smoothly and in a userfriendly manner 4 January 15, 2009
Mandate Appeals Process • Number of DOR filers— 3. 9 million in 2007 – Approx. 195, 000 uninsured (5%) – Approx. 118, 000 deemed able to afford health insurance and subject to penalty • Approx. 51, 000 with No Tax Status or Limited Income Credits, so no taxes paid and no penalty of personal exemption in 2007 – Approx. 67, 000 subject to penalty • Of these taxpayers, 7, 160 filed intent to appeal with DOR 5 January 15, 2009
Mandate Appeals Process Of the 7, 160 who appealed (as of 12/31/08) • 2, 460 appeals reviewed by Connector • • 2, 070 appeals reviewed on paper, 390 through hearings Approved 1, 780 appeals on paper (72%) Denied 450 Dismissed 200 (failure to provide documents, failure to show up for a hearing) • In process 30 • 4, 700 taxpayers failed to follow through with appeals, after their initial appeal requests • Small number came late in year and still under review 6 January 15, 2009
Mandate Appeals Process Cases decided in hearings: • Hearings were primarily telephonic • Connector provides and pays for trained attorneys as hearing officers and, if necessary, interpreters • 389 hearings scheduled: • 160 dismissed for failing to appear (primarily for telephonic hearings) January 15, 2009 • Of the 229+ hearings held, 75% of appellants prevailed (173 approved, 56 denied) 7
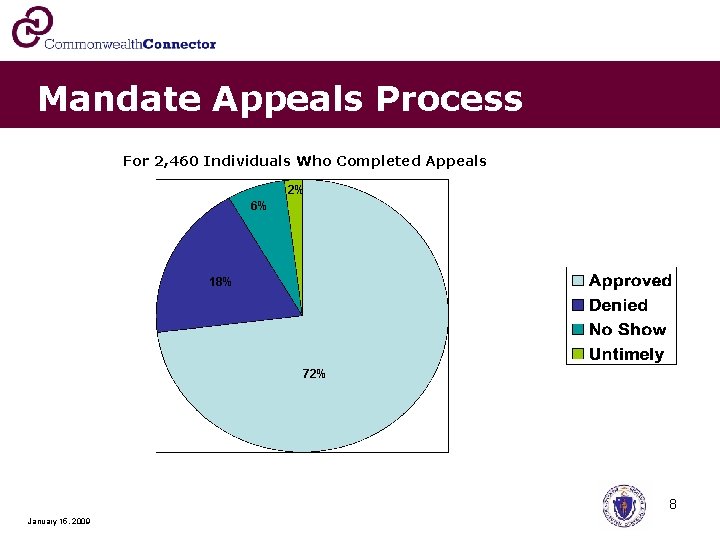
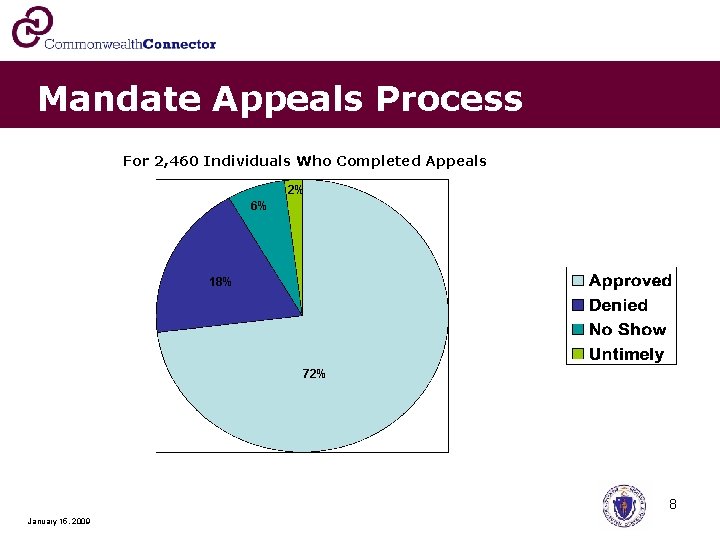
Mandate Appeals Process For 2, 460 Individuals Who Completed Appeals 2% 6% 18% 72% 8 January 15, 2009
Mandate Appeals Process Looking Forward to 2009: – Continued great assistance from DOR – Some taxpayers recognized penalty late in the year --unlikely they had a chance to remedy their situation for 2008 taxes – Added complexity due to penalty calculation based on insurance participation by individual months – Potential for much larger penalties, which may have an impact on penalty appeals volume 9 January 15, 2009
MCC Determinations • Applications for MCC Determinations – Single applications may request determinations for multiple plans, resulting in both approvals and denials (one application covers 109 plans) • 74 applications received as of 01/08/09, covering many more plans – 45 plans reviewed in full as of 01/08/09 – 39 plans approved, 3 denied, 3 determined to have no MCC deviation (no Connector action necessary) – 12 of the approved plans submitted actuarial attestations – 2 Connector FTEs currently required for MCC determinations January 15, 2009 10
MCC Determinations • Many phone calls and e-mails with carriers, employers, and brokers • Guidance given on application process and standards • Organizations told not to apply if plans will not meet MCC • Examples of denials – No RX – No mental health coverage – Union submitted plan for part-time employees; Connector would not certify it due to significant deficiencies, so plan reportedly dropped 11 January 15, 2009
MCC Determinations Central issue: Will potential financial exposure for most covered individuals exceed Bronze potential exposure? • Examples of robust plans with deviations deemed MCC compliant: – Preventive care, but not before deductible in plans with low deductibles and low or no OOPs maximums – Caps on preventive care ($200 -$500) but plans with low or no deductibles and low or no OOP maximums – Mental health/substance abuse co-insurance not counted toward OOP maximums (2009 issue) – Co-pays exceed $100 and not counted toward OOP maximums (often a separate cap on these co-pays) – Infrequent: $1 million annual maximums that reset each year (plans exceed Bronze level benefits and more generous than plans with $1 million lifetime maximums) 12 January 15, 2009
MCC Determinations MCC Consumer responses • Many individuals voicing disapproval – they have insurance that does not meet MCC and they do not want to pay more • One particular sub-group – individuals who had previously purchased plans without RX – Individuals can buy prescription drugs through the VA, through pharmacies, or do not use prescription drugs – They cannot find MA plans without prescription drug coverage 13 January 15, 2009
Commonwealth Care Appeals • Approximately 3, 800 appeals filed in 2008 – Subjects of appeals: • Eligibility denials and disenrollments primarily due to access to other insurance (appeal process intertwined with exception letter process) – Approximately 70% or more of appeals were for eligibility denials or disenrollments • Denials of requests for premium or co-pay waivers • Denials of requests for plan type changes 14 January 15, 2009
Commonwealth Care Appeals • Connector closed over 2, 700 appeals in 2008 – Remaining cases—many cases require additional information, many filed late in year (approx. 1, 000 in Nov/Dec. 2008), others in the process of review – Also dealing with system changes as the program moves to Perot Systems 15 January 15, 2009
Commonwealth Care Appeals Of the approximately 2, 700 appeals closed: • 1, 350 +/- appeals dismissed as moot (large majority got into Comm Care or Mass. Health) • Approximately 400 appeals went to hearing officers – 259 appeals dismissed due to no-shows (64%) – Number of decisions issued---61 (58 pending) • 16 appeals allowed, 42 denied • Remaining cases: 850 dismissed (not Connector cases, untimely), 80 transferred to Mass. Health, others withdrawn • Efforts underway to simplify processes so that appeals and exception letter process are not occurring simultaneously 16 January 15, 2009