Community Care Update 2019 AAHAM Spring Conference 2019
- Slides: 17
Community Care Update 2019 AAHAM Spring Conference © 2019 Community Care Behavioral Health Organization
Agenda • • Introduction What is a BH-MCO? Timely File Guidelines Eligibility Contacts Billing Requirements Reminders © 2019 Community Care Behavioral Health Organization 2
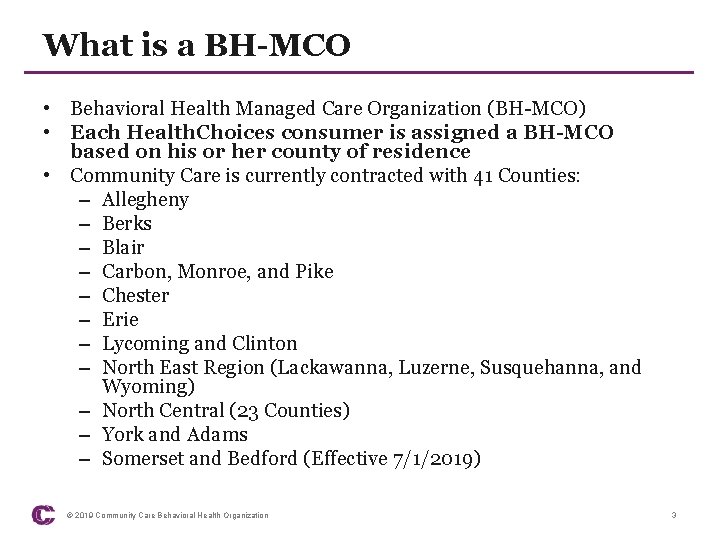
What is a BH-MCO • Behavioral Health Managed Care Organization (BH-MCO) • Each Health. Choices consumer is assigned a BH-MCO based on his or her county of residence • Community Care is currently contracted with 41 Counties: – Allegheny – Berks – Blair – Carbon, Monroe, and Pike – Chester – Erie – Lycoming and Clinton – North East Region (Lackawanna, Luzerne, Susquehanna, and Wyoming) – North Central (23 Counties) – York and Adams – Somerset and Bedford (Effective 7/1/2019) © 2019 Community Care Behavioral Health Organization 3
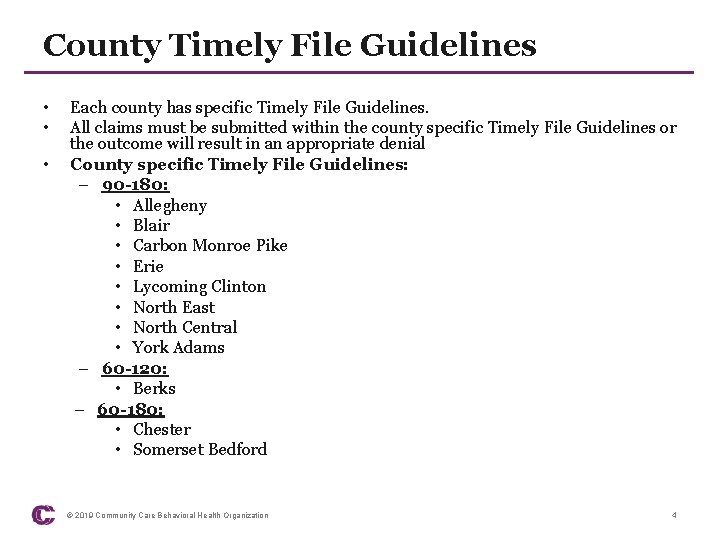
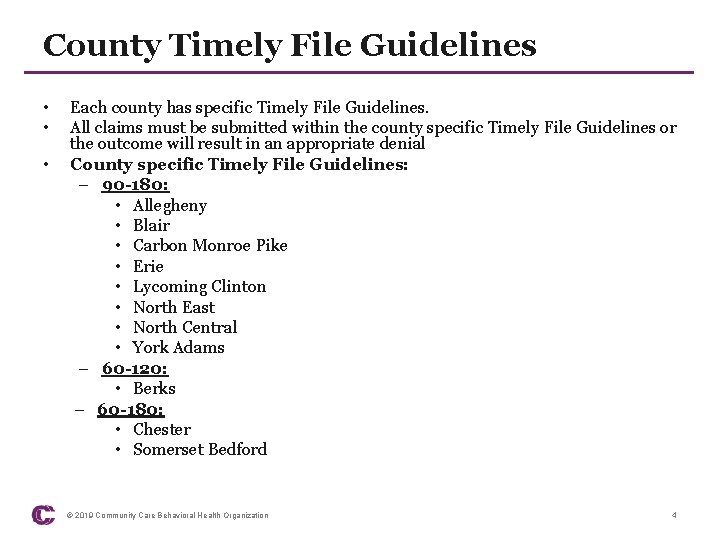
County Timely File Guidelines • • • Each county has specific Timely File Guidelines. All claims must be submitted within the county specific Timely File Guidelines or the outcome will result in an appropriate denial County specific Timely File Guidelines: – 90 -180: • Allegheny • Blair • Carbon Monroe Pike • Erie • Lycoming Clinton • North East • North Central • York Adams – 60 -120: • Berks – 60 -180: • Chester • Somerset Bedford © 2019 Community Care Behavioral Health Organization 4
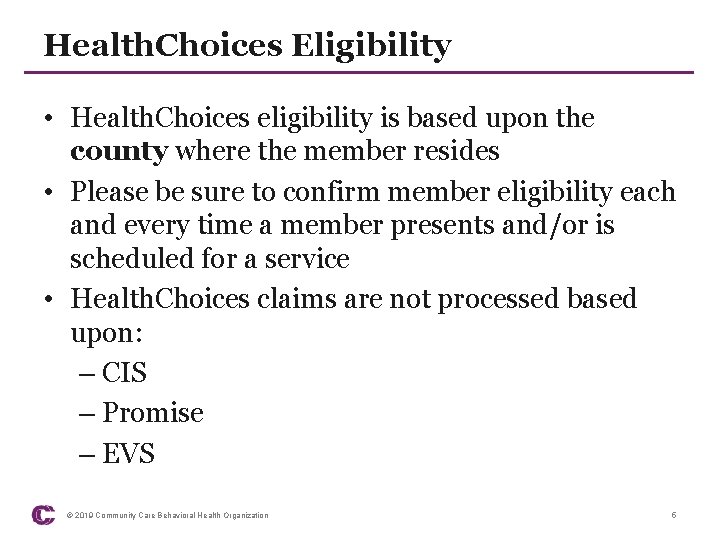
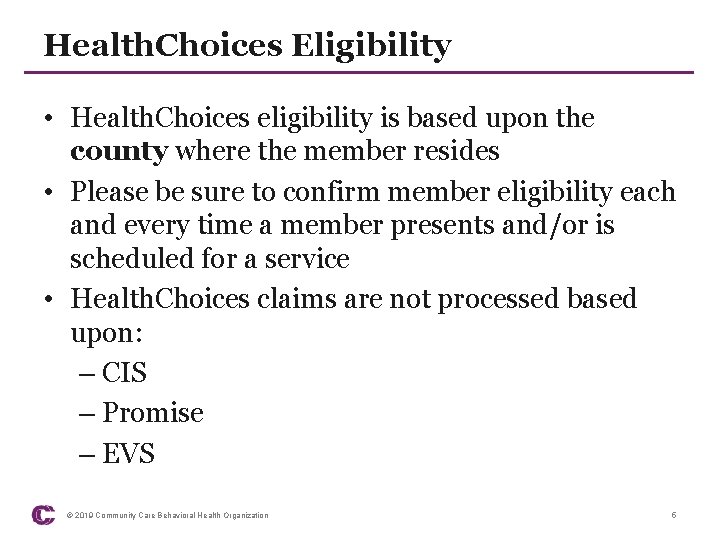
Health. Choices Eligibility • Health. Choices eligibility is based upon the county where the member resides • Please be sure to confirm member eligibility each and every time a member presents and/or is scheduled for a service • Health. Choices claims are not processed based upon: – CIS – Promise – EVS © 2019 Community Care Behavioral Health Organization 5
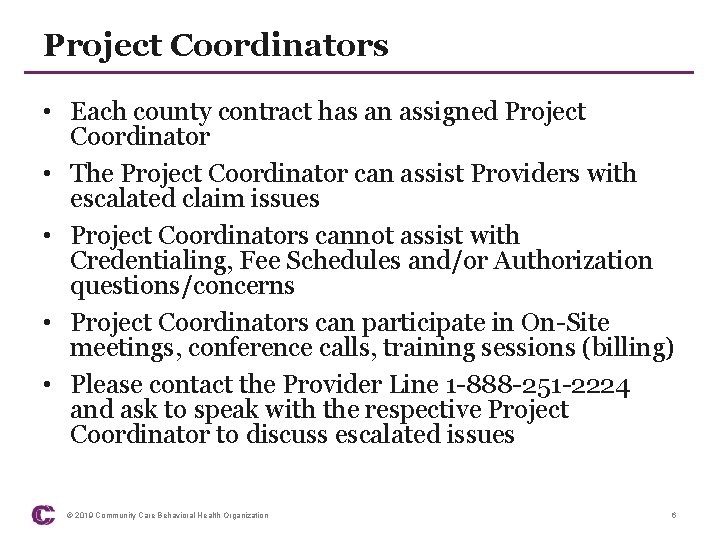
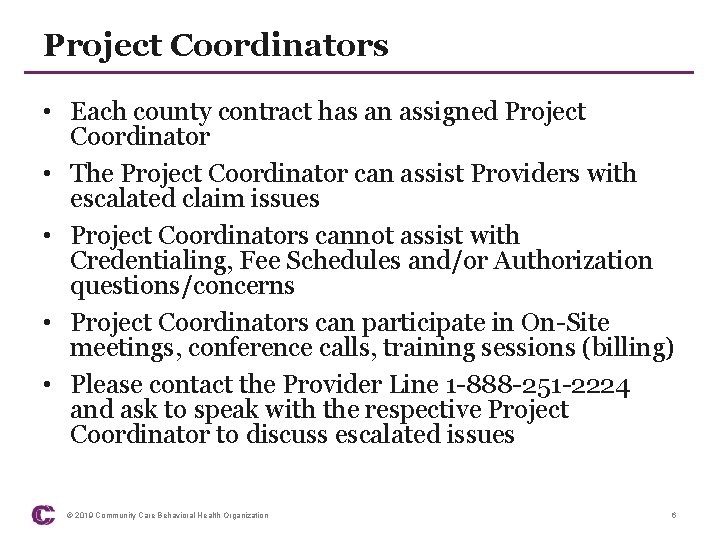
Project Coordinators • Each county contract has an assigned Project Coordinator • The Project Coordinator can assist Providers with escalated claim issues • Project Coordinators cannot assist with Credentialing, Fee Schedules and/or Authorization questions/concerns • Project Coordinators can participate in On-Site meetings, conference calls, training sessions (billing) • Please contact the Provider Line 1 -888 -251 -2224 and ask to speak with the respective Project Coordinator to discuss escalated issues © 2019 Community Care Behavioral Health Organization 6
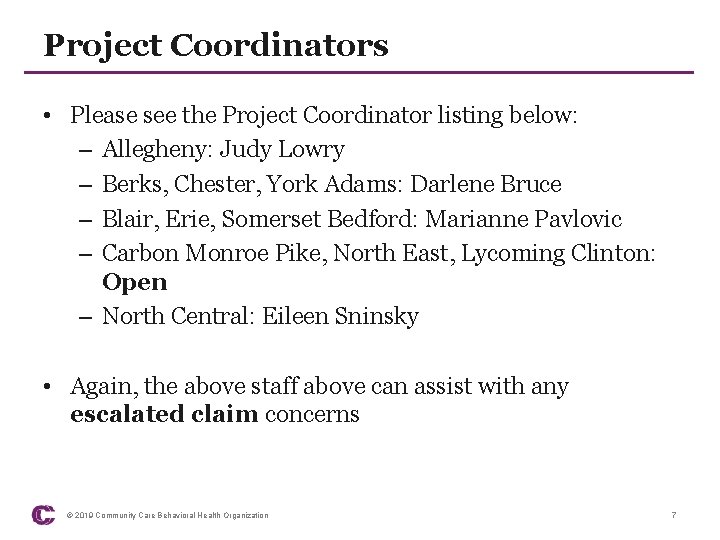
Project Coordinators • Please see the Project Coordinator listing below: – Allegheny: Judy Lowry – Berks, Chester, York Adams: Darlene Bruce – Blair, Erie, Somerset Bedford: Marianne Pavlovic – Carbon Monroe Pike, North East, Lycoming Clinton: Open – North Central: Eileen Sninsky • Again, the above staff above can assist with any escalated claim concerns © 2019 Community Care Behavioral Health Organization 7
Provider Reimbursement Claim Line • All claim related questions must be directed to the following telephone number: • 1 -888 -251 -2224, Prompt #1 • Please do not contact a Network representative or Care Manager to discuss ‘claims’. • Be prepared to provide the following: – 10 Digit Medicaid Number or 7 Digit ALDA Member Number – Your name – Your employer name – Date of service – Please be sure to have the claim you are calling to discuss in front of you © 2019 Community Care Behavioral Health Organization 8
Provider Reimbursement Claim Line • Provider Line staff are unable to complete a claim search by: – Name – Social Security Number – Primary Insurance Group or Id number. • Most Importantly: – Please review Provider On. Line prior to placing a call to the Provider Line. – Do not place a call to the Provider Line if a claim is not finalized meaning: • There is not a check number, check date or payment amount populated in Provider On. Line © 2019 Community Care Behavioral Health Organization 9
Provider Online • Provider On. Line (POL) is a web-based product created for providers to submit claims, view claim status, access weekly EOP’s, manage staff permissions related to POL, 837/835 transactions • Community Care strongly suggests Providers use POL as a TOOL to confirm claim status, payment and/or denial as well as BILL claims either manually or as an 837 direct submitter • There is no charge associated with POL • Please be sure that ‘all’ staff have access as a PRIORITY © 2019 Community Care Behavioral Health Organization 10
Provider Online • Access to Provider On. Line (POL) can be completed by accessing the Community Care website: – CCBH. com – Provider Resources – Secure Sites – Provider Online Claims • If you require assistance, please contact the Provider Line 1 -888 -251 -2224, Prompt #1 • Request POL assistance and/or a training session at any time © 2019 Community Care Behavioral Health Organization 11
Billing Reminders • The Provider Billing Manual is posted: – CCBH. com website – Provider Resources – Provider Manual • If you require assistance, please contact the Provider Line: 1 -888 -251 -2224 • Billing assistance, including training can be scheduled at any time © 2019 Community Care Behavioral Health Organization 12
Billing Reminders • ORP-Ordering, Referring and Prescribing-Required – Please review the Provider Alert and the attachment posted to the CCBH. com website • Inpatient facilities-Please be sure the units billed equals the number of days indicated in your date span • Do not bill OP services on a UB-04 -EVER. • Include the Community Care Form Number when submitting ‘Corrected Claims’ • Bill procedure codes/revenue codes according to your Community Care Fee Schedule-ONLY. © 2019 Community Care Behavioral Health Organization 13
TPL/COB Reminders • Community Care is the Payer of LAST RESORT-ALWAYS • Providers are responsible to confirm if a member has primary insurance and bill accordingly • A Provider nor a Member can elect to avoid the primary payer requirements • Do not bill Community Care at the same time you bill a primary insurance • Include the primary Explanation of Payment along with the LEGEND with each and every claim submitted • Do not FAX a Claim or an EOB • Bill procedure codes/revenue codes according to your Community Care Fee Schedule-ONLY © 2019 Community Care Behavioral Health Organization 14
TPL/COB Reminders • If you receive a Medical Necessity denial from a primary insurance carrier, you must exhaust the appeal process • If a Provider is NOT CONTRACTED with a Member’s primary insurance, Community Care will not reimburse the services • A Provider nor a Member can elect to avoid the primary payer requirements • Community Care will process and pay the Patient Responsibility (PR) indicated on an EOB if both the Community Care Clinical and Billing processes are completed correctly (authorization on file/clean claim submitted) • Do not mail claim(s) to Community Care’s P. O. Box which require a Signature © 2019 Community Care Behavioral Health Organization 15
Overview • Confirm eligibility each/every time a member presents or schedules a service • Bill according to the correct County Fee Schedule, Member’s County Residence, County Affiliation • Submit clean claims timely, according to the County specific Timely File Guidelines • Confirm claim receipt, status, payment/denial via Provider On. Line (POL) • Complete timely follow-up via Provider On. Line (POL) • A Provider nor a Member can elect to avoid the primary payer requirements • Community Care will process and pay the Patient Responsibility (PR) indicated on an EOB if both the Community Care Clinical and Billing processes are completed correctly. (authorization on file/clean claim submitted) • Take the time to review the CCBH. com website on a regular basis to confirm if there are Provider Alerts posted related to Billing/Clinical requirements © 2019 Community Care Behavioral Health Organization 16
Thank you! © 2019 Community Care Behavioral Health Organization
 What is an alternative of log based recovery
What is an alternative of log based recovery Primary secondary tertiary care
Primary secondary tertiary care Spring, summer, fall, winter... and spring cast
Spring, summer, fall, winter... and spring cast Spring summer fall winter and spring months
Spring summer fall winter and spring months University community plan update
University community plan update Acwa spring conference
Acwa spring conference Spring io conference 2020
Spring io conference 2020 Stfm conference
Stfm conference Ba conference 2019
Ba conference 2019 Iala conference 2019
Iala conference 2019 Fasfaa conference 2019
Fasfaa conference 2019 Esop conference 2019 las vegas
Esop conference 2019 las vegas Nmls resource center
Nmls resource center Third party risk management conference 2019 new york
Third party risk management conference 2019 new york Executive assistant conference 2019
Executive assistant conference 2019 2019 dod allied nations technical corrosion conference
2019 dod allied nations technical corrosion conference Fsna conference 2019
Fsna conference 2019 Mil std 7179
Mil std 7179