CARING FOR THE FRAIL ELDERLY CHAPTER OUTLINE Family
- Slides: 26
CARING FOR THE FRAIL ELDERLY
CHAPTER OUTLINE • Family care • Home care • Nursing home care
FAMILY CARE - A PROFILE OF CAREGIVING One-third of men and women over the age of 65 have some type of disability Require help with activities of daily living (ADLs) and instrumental activities of daily living (IADLs) ADLs: Eating, bathing, getting dressed, getting to and from the bathroom, getting in and out of bed, and walking IADLs: Keeping track of money, doing household tasks, taking medicine, and running errands The term long-term care refers to a range of services designed to help people with chronic conditions compensate for limitations in their ability to function independently. Family members are now preforming more complex tasks that were once the roles of trained caregivers. Family members bot only provide service for ADL / IADL needs but also manage medical even without training and up to 69% stating that their family member received no home visits from a a health care professional
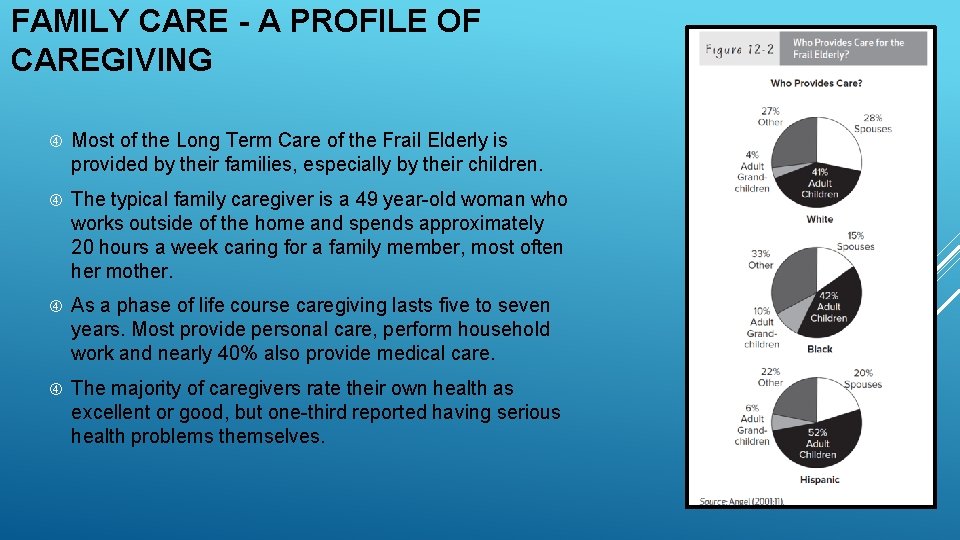
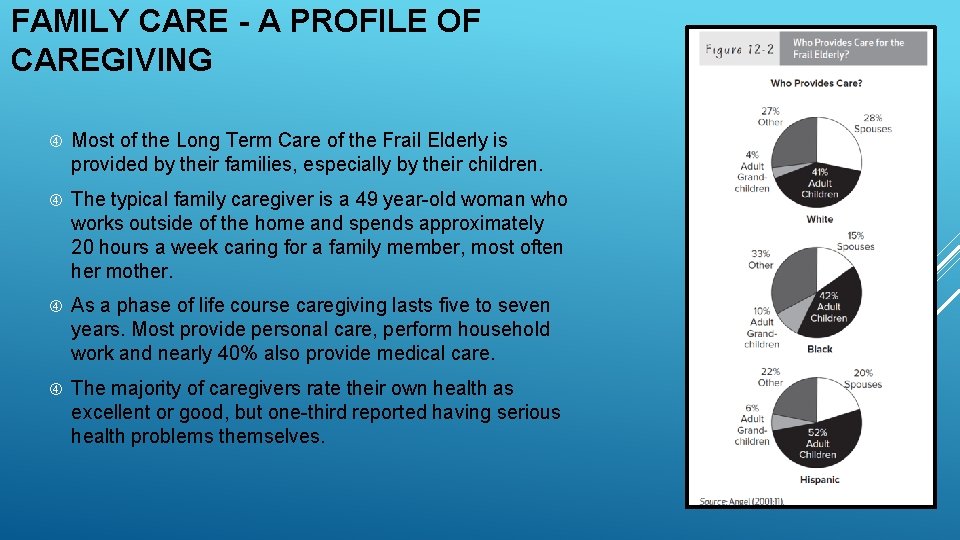
FAMILY CARE - A PROFILE OF CAREGIVING Most of the Long Term Care of the Frail Elderly is provided by their families, especially by their children. The typical family caregiver is a 49 year-old woman who works outside of the home and spends approximately 20 hours a week caring for a family member, most often her mother. As a phase of life course caregiving lasts five to seven years. Most provide personal care, perform household work and nearly 40% also provide medical care. The majority of caregivers rate their own health as excellent or good, but one-third reported having serious health problems themselves.
FAMILY CARE – GENDER DIFFERENCES IN CAREGIVING Nearly all studies of caregivers have found that women typically are the primary caregivers of ill and disabled family members. 88% of adult caregivers were daughters and daughter-in-law 76% of the spouses were wives In some cases divorced women care give for ex-husbands (love, or concerns about children’s feelings) The primary caregiver of the aging parents tends to be the daughter who has the least competing obligations, usually the one not working or is unmarried; however many daughters take on the role regardless of their responsibilities. Women tend to shoulder the burden of care because of traditional gendered roles, and past practice of unpaid domestic work responsibilities
FAMILY CARE – GENDER DIFFERENCES IN CAREGIVING Sons who are caregivers tend to perform different tasks from daughters where the division of labor is similar to the traditional labor division. Daughters are more likely to provide hands on personal care whereas sons are more likely to arrange transportation and perform house repairs, yard work, and managing finances Yet both sons and daughters feel obligated to help their parents. Even though both sons and daughters experience emotional strain, daughters tend to experience higher levels of stress and more guilt than sons. The division of labor breaks down when husbands and wives are caring for each other. Husbands who care for their wives perform all forms of personal care, and adopt strategies to do so
FAMILY CARE – CAREGIVER BURDEN Researchers distinguish between caregiver burden and caregiver stress. Burden typically refers to management of the tasks. Stress refers to the strain felt by the caregiver. A substantial source of caregiver stress also arises as caregivers try to negotiate the complex network of health care services for a frail, elderly individual. Social gerontologists refer to this as structural burden. In the US, structural burden is often caused by the confusing rules concerning service coverage and payment allocations for Medicare and Medicaid, and other ancillary insurance coverage. Family members who provide to frail and disabled older parents are at greater risk of physical exhaustion, poorer immune responses (elevated levels of cortisol), and deterioration of their own health status. There is also a greater risk of long term depression, greater risk of hypertension. Spousal caregivers experience even higher levels of stress and report more depressive symptoms than adult child caregivers
FAMILY CARE – CAREGIVER BURDEN When caregiver stress is high, the risk of respiratory infections increases as does the risk of psychiatric disturbances and cardiovascular disease. The scientific term for this process is allostatic load. Caregivers have a higher allostatic load that translates into health problems. To cope with the strain associated with caregiving, husbands rely more on family or care-giving services, whereas wives simply provide higher levels of care and seek friends and family for emotional support.
FAMILY CARE – WORK AND CAREGIVING Approximately one-third of caregiving women leave their jobs and pay a penalty in lost wages. Caregiving reduces the number of employment hours worked Reduces annual earnings. Caregivers who stop working are more likely an non-caregivers to living in poverty Employer policies play an important role. Some employers have introduced special programs to reduce stress and turnover and ease the burden for their workers. Employees commonly wish for flexible working hours, and some firms provide this option. Discrimination occurs when employers treat caregivers favorably than other employees due to the mistaken belief that their family obligations may mean that they are less committed to their jobs. The Family Medical Leave Act of 1993 (50 or more employees) allows employees to take up to 12 weeks of paid or unpaid leave for family-related reasons, including taking care of a parent with a serious medical condition
FAMILY CARE – CAREGIVING AND FAMILY RELATIONSHIPS Research suggests that caregiving not only affects the emotional well-being of the caregiver but reverberates across other family relationships. Though caregiving can cause stress in family relationships, caregiving can also be a positive influence on family relationships by bringing kin together to accomplish a shared goal The Effect of Parent-Child Relationships Relationship between the caregiver and an elderly parent can take many forms: Mutuality - Both mother and daughter describe a rewarding relationship characterized by joint activities and minimal conflicts Ambivalent - Mothers and daughters have relationships where there are rewards and costs and the relationships are sometimes tense Conflicted - There are few rewards and frequent costs
FAMILY CARE – CAREGIVING AND FAMILY RELATIONSHIPS The Effect of Parent-Child Relationships (continued)… Some abused children resolve their feelings of ambivalence toward their abuser by avoiding contact when they grow up, but others continue to maintain relationships. Ironically, the “dysfunctional parent–child relationship can switch to a recipients caregiver relationship later in life” One study attempted to measure the emotional consequences of this role reversal on the caregiver. Researchers compared caregivers who were abused as children with caregivers who had no history or abuse or neglect. Not surprisingly, they found that formerly abused caregivers had more symptoms of depression compared to caregivers who had no history or abuse or neglect. Adult survivors have weaker coping skills because of the traumatic childhood Aging parents may still be abusive towards the adult survivor Caregiving is more stressful under a sense of obligation
FAMILY CARE – CAREGIVING AND FAMILY RELATIONSHIPS The Effect on Sibling Relationships Caregiving also can generate tension between primary caregivers and their siblings. Beliefs that burdens are unequally shares Beliefs that the caregiver’s efforts are unappreciated Perceived burden can promote several emotions and emotive states, including depression and anger One study found that the greatest source of stress for women caring for parent with Alzheimer’s was their siblings Perceived burden can generate resentment and hostility between the caregiver and siblings Caregiving may also increase closeness between siblings
FAMILY CARE – CAREGIVING AND FAMILY RELATIONSHIPS The Effect on Marital Relationships Marriage can also be affected by caregiving responsibilities. On the negative side, caregiving can reduce the time husbands and wives have for each other. Women may be too worn out from performing caregiving duties to spend quality time with their husbands and may worry about whether caregiving demands are harming their marriage On the positive side, daughters and daughters-in-law who felt they were doing an adequate job as a caregiver reported higher levels of marital satisfaction. Wear and tear hypothesis - longer term caregivers have less marital satisfaction, greater marital role inequality, and greater hostility than those who recently began caregiving. This effect seems to only be buffered by the inherent quality of the marriage.
FAMILY CARE – CAREGIVING AND FAMILY RELATIONSHIPS The Effect on Grandchildren When adult children care for their aged parents, their own children often become part of the caregiving nexus. Children may have to compete with their grandparents for their parents’ attention. They may also be forced to make financial sacrifices or endure a more crowded household if their grandparents move in to their home. Family caregiving may also have positive consequences Most grandchildren felt the caregiving situation had a positive influence on family relationships Made the young people more empathetic toward the elderly as well as their grandparents Adolescents felt closer to their mothers, who were nearly always the primary caregivers. They felt rewarded when their mothers praised them for the help provided.
DISCUSSION What kind of social support would be helpful to stressedout sandwich-generation caregivers?
HOME CARE – HOME AND COMMUNITY-BASED SERVICES Home and Community-Based Services A recent effort to reduce unnecessary institutionalization is the Program of All-Inclusive Care for the Elderly (PACE). PACE is an optional benefit for older people who meet their state's standards for nursing home care. It features comprehensive medical and social services in a variety of settings so the elder can receive services in the home rather than a nursing home. Much of the interest in expanding HCBS stems from a desire to reduce nursing home costs Policymakers fear that if paid HCBS is expanded, family and friends may stop providing care There is no evidence that HCBS reduce costs or nursing home use Most research shows that families do not withdraw support when home and community-based services are provided but rather that the disabled elderly receive more care Quality is another important issue. Evidence suggests that home and community-based services are not always adequate. Most home care workers are middle-aged women. Low wages and poor working conditions create high turnover rate among home health aides
HOME CARE – HOME AND COMMUNITY-BASED SERVICES Home and Community-Based Services Many frail elderly who might otherwise have to enter institutions are able to remain in their own homes if they have access to home and community based services (HCBS). The most common home and community-based services are (1) personal care, such as bathing, dressing, feeding, and grooming, (2) housekeeping, including meal preparation and planning, grocery shopping, transportation to medical services, and bill paying, and (3) case management. Case management is provided by a social worker who assists frail elderly people and their families in obtaining medical, social, and personal services These services may include: Respite care, adult day care, social stimulation, and sometimes medical or rehabilitative care, and hospice service
HOME CARE – HOME AND COMMUNITY-BASED SERVICES Race, Ethnicity, and Long-Term Care Minorities are less likely than the white elderly to receive home and community-based services or to enter nursing homes Some people argue that cultural preferences are the reason for these differences. Among some minority groups, cultural norms dictate that children should care for their aged parents Food choices and language barriers Black and Latino Elders may be more concerned about the racial and ethnic background of the caregivers Lack of access is another reason members of minority groups receive nursing home care less frequently than whites Minority elderly may not be willing to move to a nursing home that is far from their families
HOME CARE – HOME AND COMMUNITY-BASED SERVICES Private Long-Term-Care Insurance Today, neither Medicare nor Medicaid pays much for home care services. One option is private financing through long-term care insurance Initially began in the 1980’s to help cover the cost of nursing home care, but expanded to gradually cover assisted living and in-home care. By 2003 sales peaked, but growth abruptly stopped and many companies stopped offering policies because insurers underestimated costs and could not pay for the promised care. This drop in sales was compounded with a reduction in services covered, and criminal activity. Long term care insurance does pay for some benefits, but it is very expensive, and no more than 520% of the population has policies.
NURSING HOME CARE In the past the nursing home was the most common site for care of the frail elderly, but that has changed considerably in the past few decades. Between 2000 and 2010 the share of the 65 and older population residing in a nursing home dropped from 4. 6 percent to 3. 1 percent. The reasons for the decline are numerous and include the availability of alternative forms of care, especially assisted living facilities, changes in how care for the elderly is funded, and the preference of older people to live independently.
NURSING HOME CARE – STAFF TURNOVER The starting salary for nursing home aides is usually the minimum wage, and they receive few fringe benefits such as health insurance or pensions. Average annual wage in 2015 was $21, 820 ( slightly higher than home health aides salaries) Care is needed on a 24 -hour basis, so many of these aides work nights, weekends, and holidays. Patients are dependent on employees for the most basic ADL’s Management and employee relationships are poor, many nursing homes are understaffed and prompt the employee to rush through caregiving tasks. The work frequently requires aides to manually lift patients, which often results in back injuries. Care workers are more likely to be injured that construction workers and coal miners Thus, there are many factors that promote absenteeism and high worker turnover Only 46% of nursing homes provide basic levels of care, one-fourth have deficiencies that could promote injury and death. Many nursing homes are constrained by the amount of funding that they receive though government funding (Medicare/Medicaid).
NURSING HOME CARE – ACCESS TO NURSING HOME CARE In 2012, the average annual cost for a semi-private room in a nursing home was $81, 000 with costs exceeding $100, 000 in some cities. Medicare pays only a small fraction of nursing home care costs. Paid only when an older person is released from a hospital to a skilled nursing facility Medicare currently pays almost three times as much as Medicaid for patient care in many states. As a result, nursing homes have attempted to increase the number of residents whose care is paid by Medicare, leaving fewer beds available for Medicaid patients. As a result of such policies, Medicaid recipients are denied access to many nursing homes. They wait longer to gain admission to a nursing home and end up in less desirable homes. Many patients who pay for private care rapidly deplete their assets and thus become poor through spending down to the $2000 of their life savings before they can receive Medicaid funding. Many of those who experience these difficulties are racial and ethnic minorities. Yet all racial groups are likely to be affected, given the high cost of care. Medicaid has a “look back” period of five years to see whether assets were improperly transferred.
NURSING HOME CARE Adjusting to a Nursing Home People who live independently in a community find the transition to institutional life difficult Loss of independence is the most important concern Daily Life In a Nursing Home Perhaps the most difficult aspect of life in a total institution is the monotonous daily routine. The routine results from pressure on nursing home aides to meet the basic needs of the residents. Residents must be fed, dressed, bathed, and prepared for bed. Quality Of Care Poor quality care in nursing homes becomes abuse Nursing homes that have high levels of turnover among their nursing aides generally provide poorer care than those with low turnover Concerns about quality of care in nursing homes are widespread among family members, the public, and policymakers
NURSING HOME CARE Families of the Institutionalized Elderly Caregiver stress often does not end after an aging parent or spouse is admitted to a nursing home Conflict with the staff adds to the stress, as caregivers who formerly attended to every need of their loved ones now find they are at the mercy of strangers
DISCUSSION Many people fear ending their lives in a nursing home. In your view, what is the worst aspect of life in a total institution?
ADDITIONAL INTERNET RESOURCES 1. Administration on Aging (http: //www. aoa. gov/ ) 2. Agency for Health Care Policy and Research (https: //www. ahrq. gov/research/findings/factsheets/medicaremedicaid/mednote/index. html ) 3. The Eden Alternative (http: //www. edenalternative. com ) 4. National Institute on Aging (https: //www. nia. nih. gov ) 5. Caregiver Alliance (http: //www. caregiver. org/caregiver/jsp/home. jsp )
 Caring occasion/caring moment
Caring occasion/caring moment Calbala
Calbala Fract root word
Fract root word At grass philip larkin
At grass philip larkin He is quite short
He is quite short Chapter 10:4 confusion and disorientation in the elderly
Chapter 10:4 confusion and disorientation in the elderly Chapter 10:4 confusion and disorientation in the elderly
Chapter 10:4 confusion and disorientation in the elderly Chapter 21 caring for head and spine injuries
Chapter 21 caring for head and spine injuries Chapter 31 caring for your career and yourself
Chapter 31 caring for your career and yourself Cna chapter 10 caring for yourself
Cna chapter 10 caring for yourself Chapter 24 caring for your career and yourself
Chapter 24 caring for your career and yourself Milwaukee elderly neglect
Milwaukee elderly neglect Objectives of geriatric nursing
Objectives of geriatric nursing Nphce launch date
Nphce launch date Elderly mobility scale
Elderly mobility scale Bp goal for elderly
Bp goal for elderly Communication with the elderly
Communication with the elderly Anticipatory guidance for adults
Anticipatory guidance for adults Clay county transit for elderly
Clay county transit for elderly Psychosocial needs of the elderly
Psychosocial needs of the elderly Dependency ratio geography
Dependency ratio geography Pijnmodel loeser
Pijnmodel loeser '+elderly +ensure
'+elderly +ensure Common psychosocial care problems of the elderly
Common psychosocial care problems of the elderly Nausea and vomiting in the elderly
Nausea and vomiting in the elderly Low sodium levels in the elderly
Low sodium levels in the elderly National programme for health care of elderly
National programme for health care of elderly