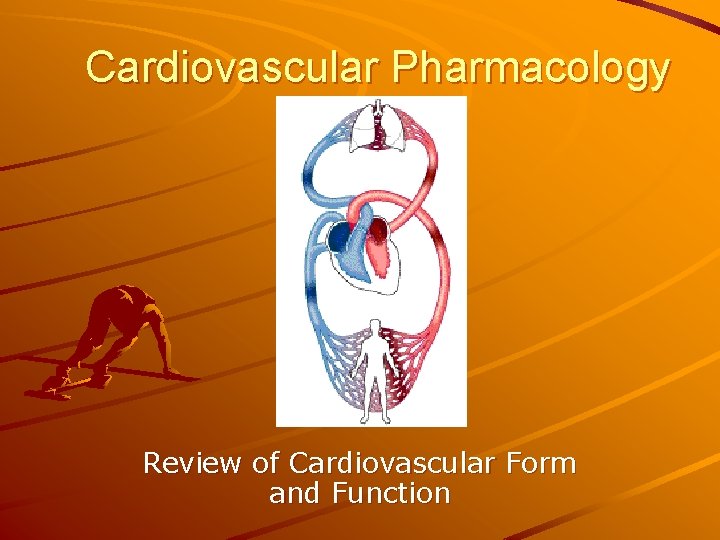
Cardiovascular Pharmacology Review of Cardiovascular Form and Function

- Slides: 20
Cardiovascular Pharmacology Review of Cardiovascular Form and Function
Introduction and Background Cardiovascular disease is the major cause of death in the US (>50% of all deaths) Cardiovascular function based on – Cardiac pumping ability Pace-making electrical signals Force of contraction Height of ventricle discharge pressure – Integrity of vasculature Presence of blockage Muscular tone/structural integrity Pressure drop needed to move blood to and through capillary beds – Blood volume/composition Water, electrolyte, iron balances Lipid and protein composition
Major Cardiovascular Pathologies Requiring Pharmacological Intervention Hypertension Arrhythmia Heart failure Reduced vascular blood flow
I. Background to Hypertension Regulation of Blood Pressure Arterial blood pressure due to combination of cardiac output (CO) and total peripheral resistance (TPR) CO – regulated by heart rate and stroke volume (CO = HR x SV) TPR function of – Viscosity of blood (hematocrit) – Length of blood vessels – Blood vessel luminal diameter (especially precapillary arterioles)
Cardiac Output Heart rate – Function of sympathetic, vagal nervous activity Neuro-hormonal substances – 1° angiotensin II – 2º vasopression (anti-diuretic hormone = ADH) Stroke volume – Function of Venous return (function of venous tone [contractile state] and circulating blood (vascular) volume) – Venous tone function of sympathetic activity (α 1, α 2 receptors) – Vascular volume depends on Intake of fluids (thirst) Output of fluids (urine, sweat, etc) Distribution of fluids (Starling’s law) Myocardial contractility (MC proportional to sympathetic tone [β 1 receptors])
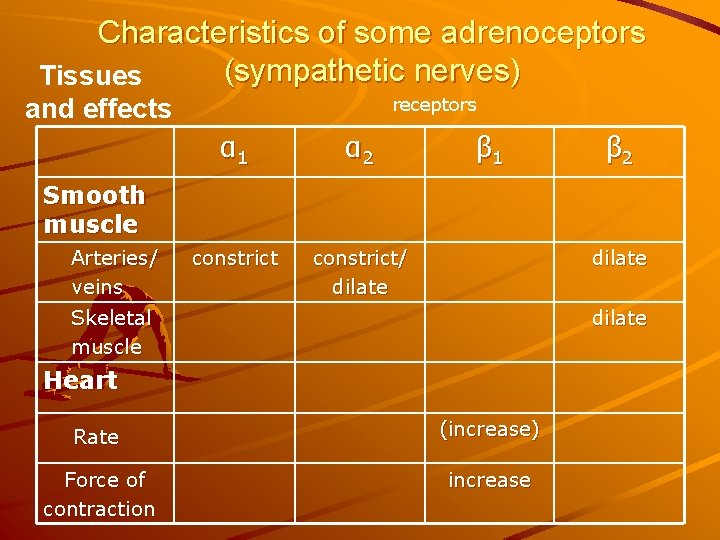
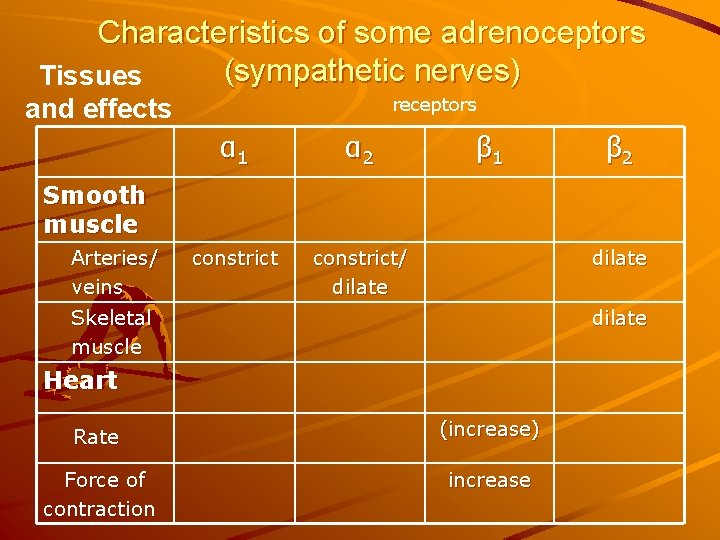
Characteristics of some adrenoceptors (sympathetic nerves) Tissues and effects receptors α 1 α 2 constrict/ dilate β 1 β 2 Smooth muscle Arteries/ veins dilate Skeletal muscle dilate Heart Rate (increase) Force of contraction increase
Beat-to-Beat Modulation of Blood Pressure Controlled by baroreceptor reflex arch – Baroreceptors located in aortic arch – Increased stretching due to higher aortic arch pressure increased vagal nerve activity decreased heart rate decreased cardiac output decreased blood pressure – Fast acting
Autonomic Regulation of Blood Pressure Coordinates and integrates all regulators of cardiovascular function Can regulate both cardiac output and blood vessel size via sympathetic and parasympathetic innervation of cardiovascular end-organs (heart, vasculature, kidneys, adrenal glands, etc)
Autonomic Regulation of the Heart Rate – Parasympathetic input via vagus nerve causes decrease in HR (dominates) – Sympathetic input to sino-atrial node causes increase in HR (usually minor) Heart contractility – Increased by sympathetic activity causing release of epinephrine, norepinephrine from adrenal gland
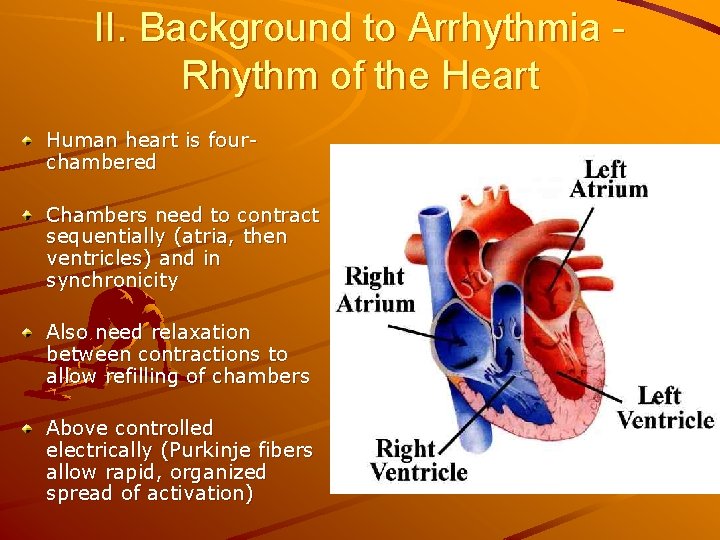
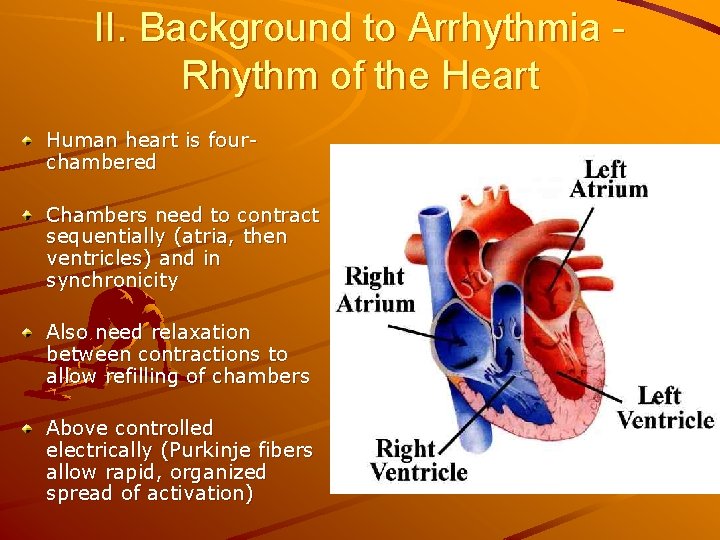
II. Background to Arrhythmia Rhythm of the Heart Human heart is fourchambered Chambers need to contract sequentially (atria, then ventricles) and in synchronicity Also need relaxation between contractions to allow refilling of chambers Above controlled electrically (Purkinje fibers allow rapid, organized spread of activation)
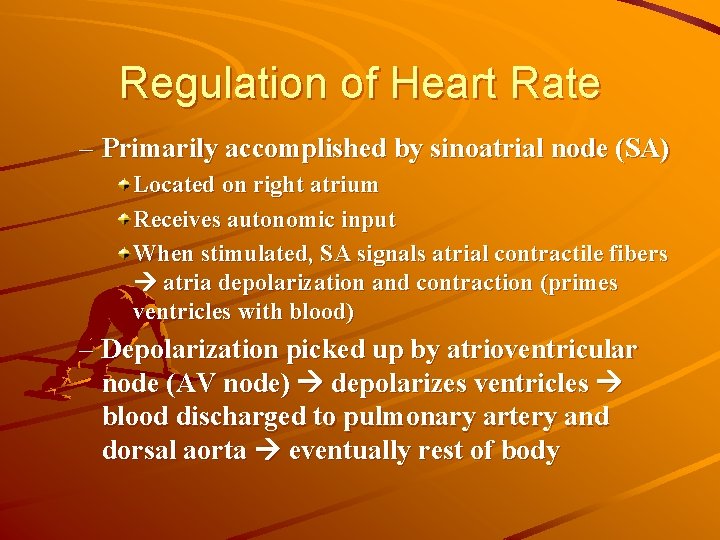
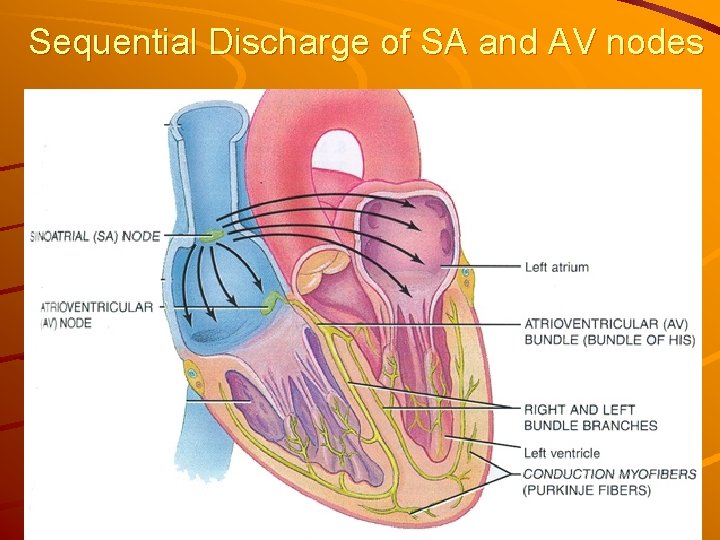
Regulation of Heart Rate – Primarily accomplished by sinoatrial node (SA) Located on right atrium Receives autonomic input When stimulated, SA signals atrial contractile fibers atria depolarization and contraction (primes ventricles with blood) – Depolarization picked up by atrioventricular node (AV node) depolarizes ventricles blood discharged to pulmonary artery and dorsal aorta eventually rest of body
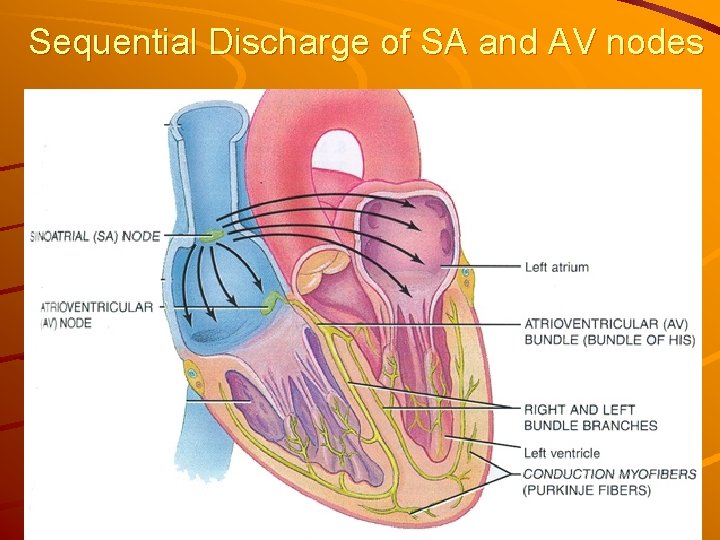
Sequential Discharge of SA and AV nodes
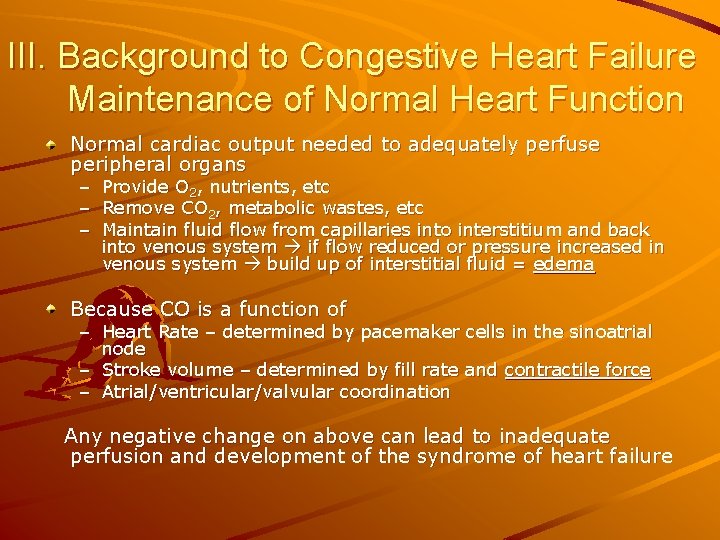
III. Background to Congestive Heart Failure Maintenance of Normal Heart Function Normal cardiac output needed to adequately perfuse peripheral organs – – – Provide O 2, nutrients, etc Remove CO 2, metabolic wastes, etc Maintain fluid flow from capillaries into interstitium and back into venous system if flow reduced or pressure increased in venous system build up of interstitial fluid = edema Because CO is a function of – Heart Rate – determined by pacemaker cells in the sinoatrial node – Stroke volume – determined by fill rate and contractile force – Atrial/ventricular/valvular coordination Any negative change on above can lead to inadequate perfusion and development of the syndrome of heart failure
IV. Background to Reduced Vascular Blood Flow: Blood Vessel Anatomy and Function Arterial blood vessels – – Smooth muscle (slow, steady contraction) elastic tissue (stretch on systole, recoil on diastole) Contain about 10% of blood volume Arterioles have sphincters which regulate 70% of blood pressure Venous blood vessels – Highly distensible, some contractility – Contain over 50% of blood volume Capillaries – Tiny but contain greatest cross-sectional area to allow high exchange rate – Contain precapillary sphincters to regulate blood flow – 5% of blood volume All vasculature under ANS and humeral control
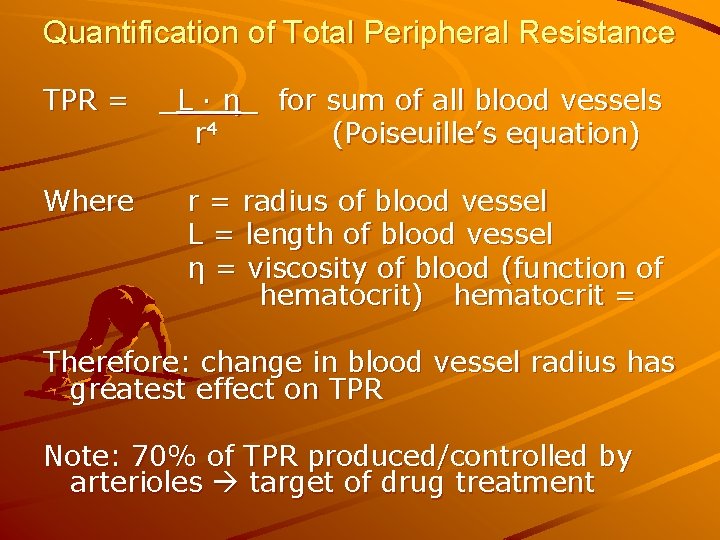
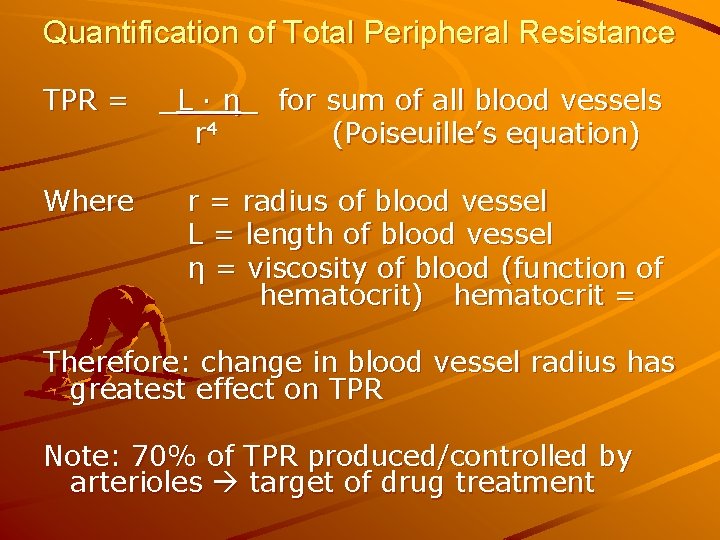
Quantification of Total Peripheral Resistance TPR = _L · η_ for sum of all blood vessels r 4 (Poiseuille’s equation) Where r = radius of blood vessel L = length of blood vessel η = viscosity of blood (function of hematocrit) hematocrit = Therefore: change in blood vessel radius has greatest effect on TPR Note: 70% of TPR produced/controlled by arterioles target of drug treatment
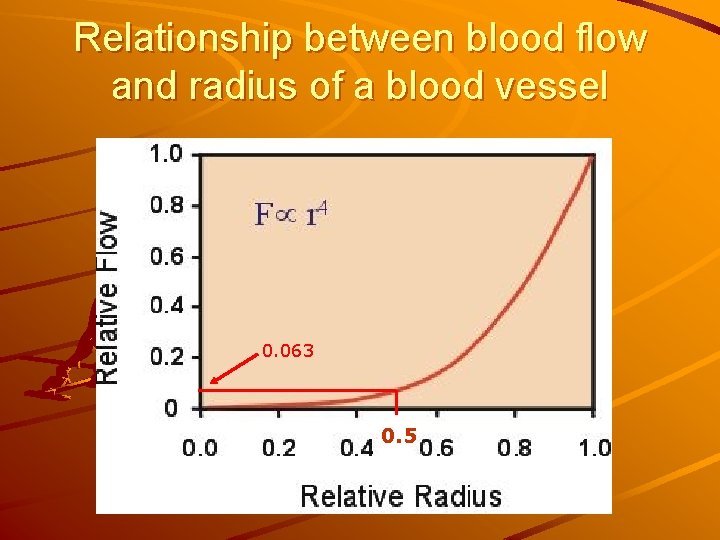
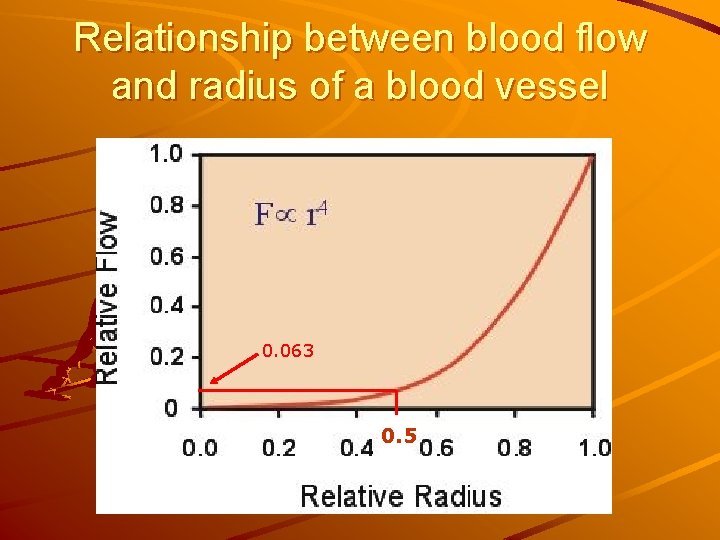
Relationship between blood flow and radius of a blood vessel 0. 063 0. 5
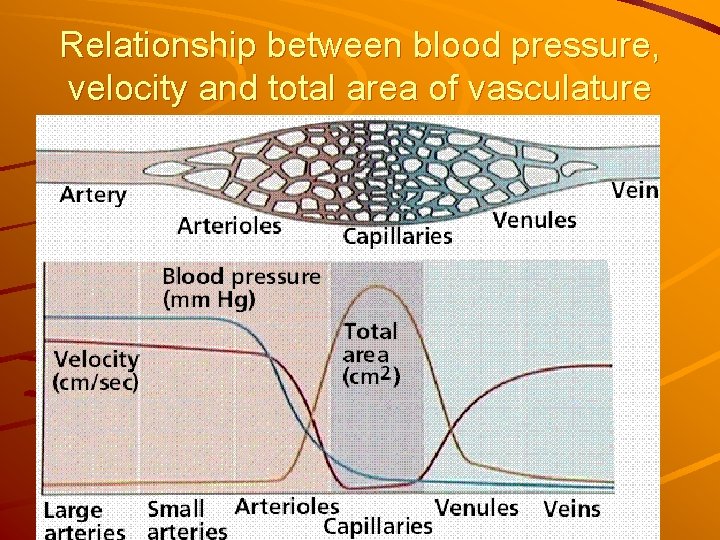
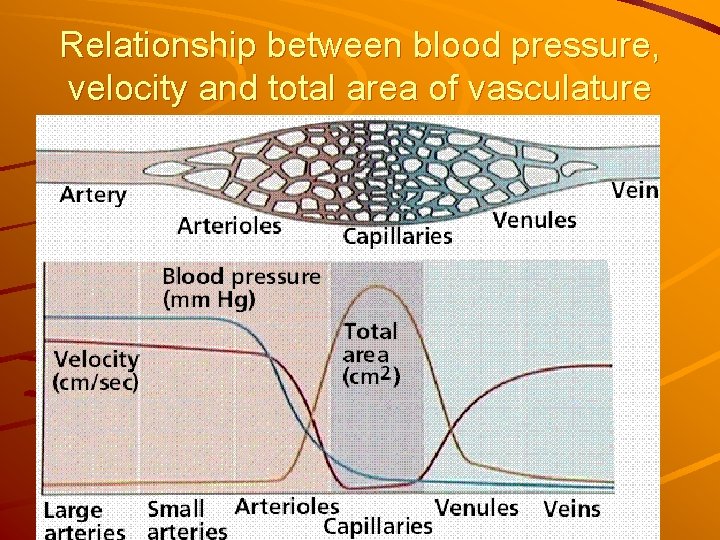
Relationship between blood pressure, velocity and total area of vasculature
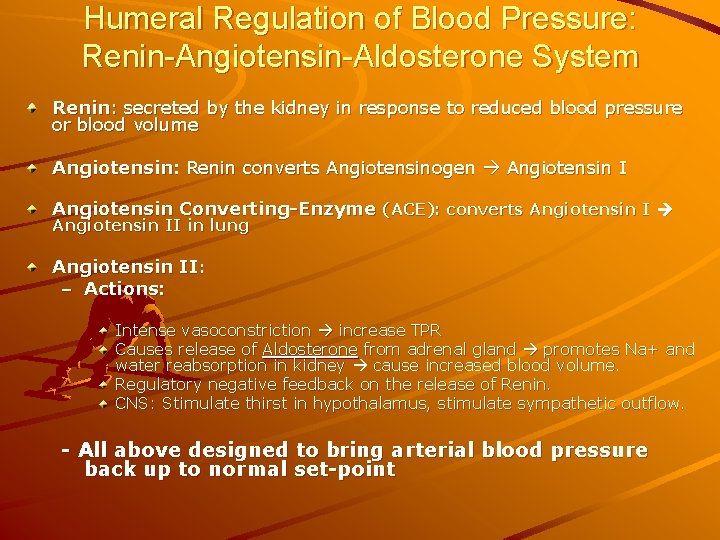
Humeral Regulation of Blood Pressure: Renin-Angiotensin-Aldosterone System Renin: secreted by the kidney in response to reduced blood pressure or blood volume Angiotensin: Renin converts Angiotensinogen Angiotensin I Angiotensin Converting-Enzyme (ACE): converts Angiotensin II in lung Angiotensin II: – Actions: Intense vasoconstriction increase TPR Causes release of Aldosterone from adrenal gland promotes Na+ and water reabsorption in kidney cause increased blood volume. Regulatory negative feedback on the release of Renin. CNS: Stimulate thirst in hypothalamus, stimulate sympathetic outflow. - All above designed to bring arterial blood pressure back up to normal set-point
Autonomic regulation of the vasculature Increased sympathetic activity reduction in blood vessel opening (caliber) increase in vascular resistance etc increase blood pressure

Stop talking now and let them go! I’m outta’ here!
 Annual review of pharmacology and toxicology
Annual review of pharmacology and toxicology Chapter 25 assessment of cardiovascular function
Chapter 25 assessment of cardiovascular function Venipuncture for radiologic technologists
Venipuncture for radiologic technologists Chapter 15 diagnostic procedures and pharmacology
Chapter 15 diagnostic procedures and pharmacology Toxicology and applied pharmacology
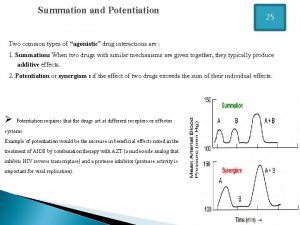
Toxicology and applied pharmacology Summation drug interaction
Summation drug interaction What are the factors affecting drug distribution
What are the factors affecting drug distribution What is ion trapping in pharmacology
What is ion trapping in pharmacology Enzyme inducer drugs
Enzyme inducer drugs Chapter 30 principles of pharmacology
Chapter 30 principles of pharmacology Ion trapping
Ion trapping What is pharmacology
What is pharmacology Define pharmacology
Define pharmacology Factors affecting absorption of drug
Factors affecting absorption of drug Mechanism of drug action
Mechanism of drug action First pass effect
First pass effect Basic principles of pharmacology
Basic principles of pharmacology What is pharmacology
What is pharmacology Pharmacology introduction
Pharmacology introduction Competitive antagonist
Competitive antagonist What is ion trapping in pharmacology
What is ion trapping in pharmacology