Asthma Definition key points Asthma is a chronic


- Slides: 20

Asthma
Definition & key points Asthma is a chronic inflammatory disorder of the airways. It is an intermittent and reversible airflow obstruction that affects the bronchioles. Obstruction may be caused by: inflammation of airway (edema/swelling) hyper-responsiveness (increased mucus production), or Bronchoconstriction

Diagnoses; Signs & Symptoms Four categories of Asthma: Mild intermittent: Symptoms occur less than twice a week. Mild persistent: Symptoms occur more than twice a week, week but not daily. Moderate persistent: Daily symptoms occur in conjunction with exacerbations twice a week. Severe persistent: Symptoms occur continually, along with frequent exacerbations that limit the client’s physical activity and quality of life
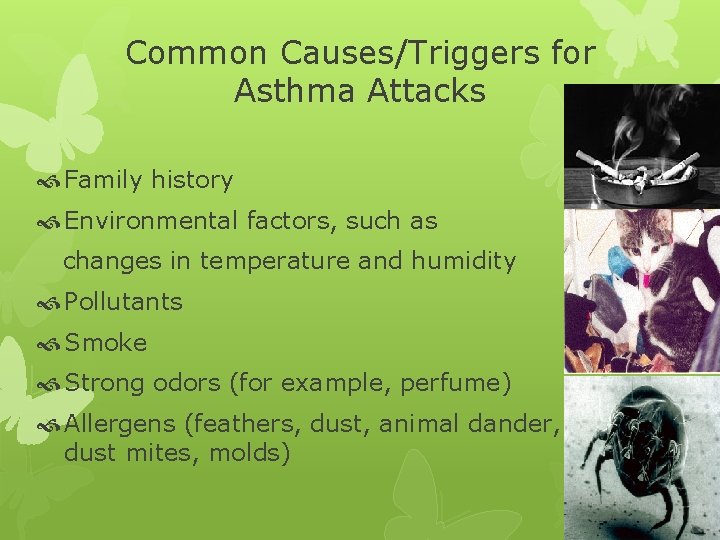
Common Causes/Triggers for Asthma Attacks Family history Environmental factors, such as changes in temperature and humidity Pollutants Smoke Strong odors (for example, perfume) Allergens (feathers, dust, animal dander, dust mites, molds)
Goals of Asthma Management Improve airflow. Relieve symptoms. Prevent acute attacks. Reducing asthma morbidity is a goal of Healthy People 2010.
Common Triggers for Asthma Attacks Exercises Stress (emotionally upset) Medications (aspirin, NSAIDS, beta-blockers, cholinergic drugs) Enzymes, including those in laundry detergents Chemicals (for example, household cleaners)
Common Triggers for Asthma Attacks Weather changes Upper respiratory infections Cold air Rhinosinusitis Gastroesophageal reflux
Diagnostic Procedures and Nursing Interventions Pulmonary function tests are the most accurate tests Forced vital capacity (FVC) is the volume of air exhaled from full inhalation to full exhalation. Forced expiratory volume in the first second (FEV 1) is the volume of air blown out as hard and fast as possible during the first second of the most forceful exhalation after the greatest full inhalation. Peak expiratory rate flow (PERF) is the fastest airflow rate reached during exhalation. A decrease in FEV 1 or PERF by 15 to 20% below the expected value is common in clients with asthma. An increase in these values by 12% following the administration of bronchodilators is diagnostic for asthma.
Diagnostic Procedures and Nursing Interventions Arterial Blood Gases (ABGs) Decreased Pa. O 2 Pa. CO 2 may be decreased in early stages of an attack due to the client’s increased work of breathing. It will rise as fatigue sets in. Chest x-ray is used to diagnose changes in chest structure over time.
Assessment Clients with mild to moderate asthma may experience few or no symptoms between asthma attacks. During attacks, monitor for signs and symptoms. Dyspnea Chest tightness Coughing Wheezing Mucus production Use of accessory muscles Poor oxygen saturation (low Sa. O 2) diaphoresis, tachycardia, and widened pulse pressure.
Assess/Monitor Client’s respiratory status (airway, RR, use of accessory muscles, oxygenation status) before and after intervention Client’s history regarding current and previous asthma exacerbations Onset and duration Precipitating factors Changes in medication regimen Medications that relieve symptoms Other medications taken Self-care methods used to relieve symptoms General appearance (chest diameter) Laboratory findings (ABGs, sputum culture results)
NANDA Nursing Diagnoses Impaired gas exchange Ineffective airway clearance Ineffective breathing pattern Anxiety
Nursing Interventions Administer oxygen therapy as prescribed. Place the client in high-Fowler’s position Monitor pulse & RR during an acute attack. Initiate and maintain IV access. Administer medications as prescribed: Bronchodilators Short-acting beta 2 agonists, such as albuterol (Ventolin) provide rapid reliefs
Nursing Interventions Anticholinergic drugs (Atrovent), block the parasympathetic nervous system, allowing for bronchodilation & decreased pulmonary secretions. Methylxanthines (theophylline), require close monitoring of serum medication levels Anti-inflammatories decrease airway inflammation. Corticosteroids; if given systemically, monitor for serious SE Monoclonal antibodies, such as Xolair
Nursing Interventions Combination agents (bronchodilator and antiinflammatory) Ipratropium and albuterol (Combivent) Fluticasone and salmeterol (Advair) If prescribed separately for inhalation administration at the same time, administer the bronchodilator first in order to increase the absorption of the anti-inflammatory agent. Maintain a calm and reassuring behavior.
Client Education Instruct the client how to recognize and avoid triggering agents Instruct the client how to properly self-administer medications (nebulizers and inhalers). Educate the client regarding infection prevention techniques. Encourage the client to get a pneumonia vaccine. Promote good nutrition. Reinforce importance of good hand hygiene. If the client smokes, discuss the effects of smoking on asthma and possible smoking cessation strategies. Encourage regular exercise as part of asthma therapy. Promotes ventilation and perfusion. Maintains cardiac health Enhances skeletal muscle strength. Clients may require pre-medication. Provide referral to support groups as needed.
Complications and Nursing Implications Respiratory Failure Persistent hypoxemia Monitor oxygenation levels and acid-base balance. Prepare for intubation and mechanical ventilation as indicated. Status Asthmaticus Life-threatening episode of airway obstruction that is often unresponsive to common treatment. Extreme wheezing, labored breathing, use of accessory muscles, distended neck veins, and risk for cardiac and/or respiratory arrest.
Status Asthmaticus Causes: Infection, anxiety, nebulizer abuse, dehydration, increased adrenergic blockage, and nonspecific irritants may contribute to these episodes
Management of status asthmaticus Prepare for emergency intubation. As prescribed, administer potent systemic bronchodilators, such as epinephrine, and initiate systemic steroid therapy. Respiratory and cardiac rhythm should be monitored continuously during the acute phase and until the patient stabilizes and responds to therapy. Assess the patient’s skin turgor for signs of dehydration; fluid intake is essential to combat dehydration, to loosen secretions, and to facilitate expectoration. • Administer IV fluids as prescribed, up to 3 to 4 L/day, unless contraindicated. Encourage the patient to conserve energy. Ensure patient’s room is quiet and free of respiratory irritants (eg, flowers, tobacco smoke, perfumes, or odors of cleaning agents); nonallergenic pillows should be used.