Asthma Overview Asthma is the most common chronic


- Slides: 41
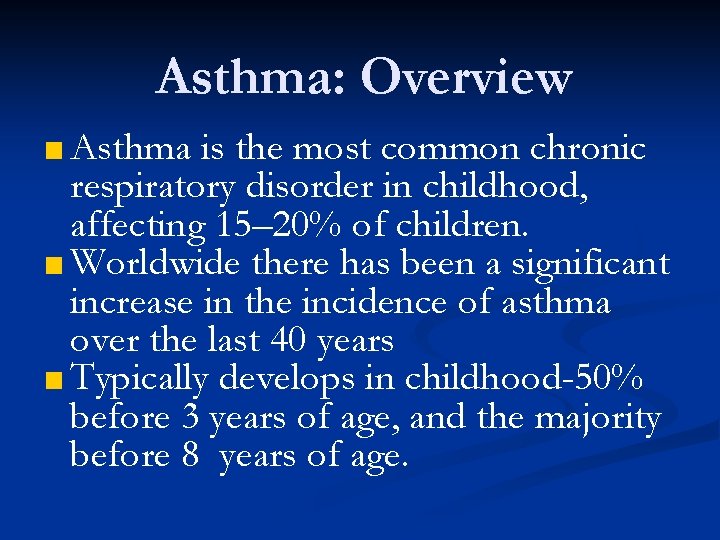
Asthma: Overview ■ Asthma is the most common chronic respiratory disorder in childhood, affecting 15– 20% of children. ■ Worldwide there has been a significant increase in the incidence of asthma over the last 40 years ■ Typically develops in childhood-50% before 3 years of age, and the majority before 8 years of age.
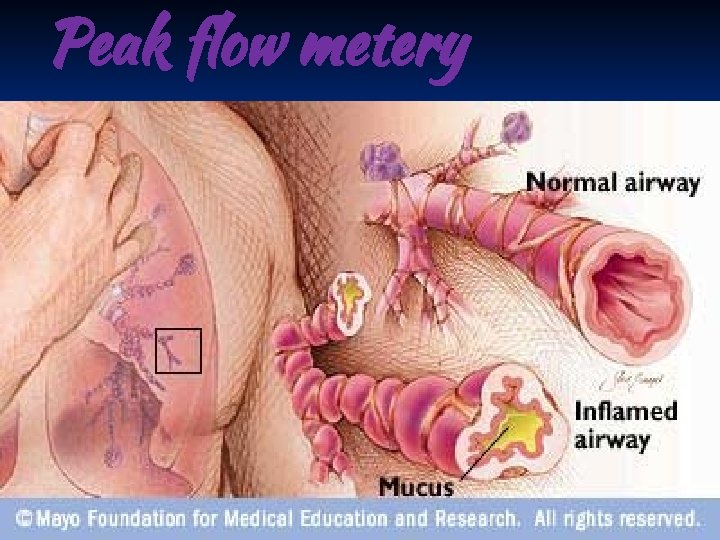
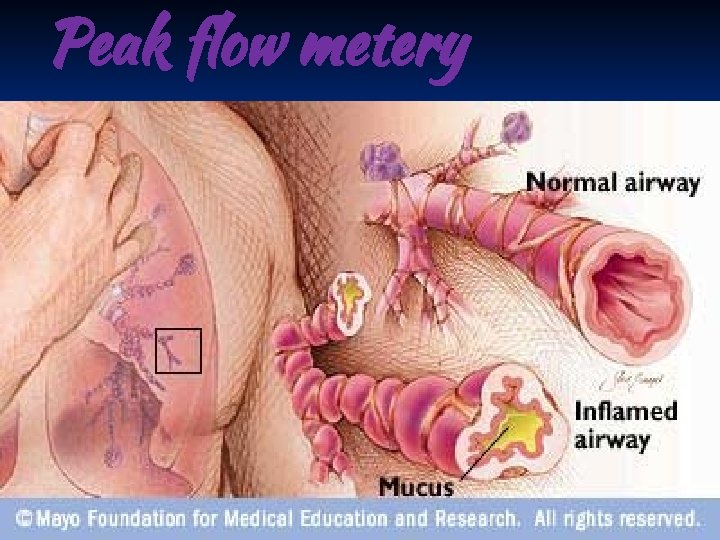
Peak flow metery
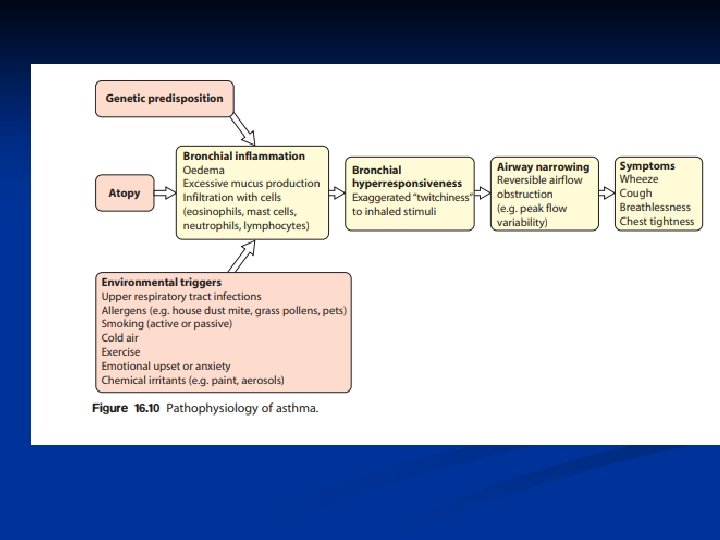
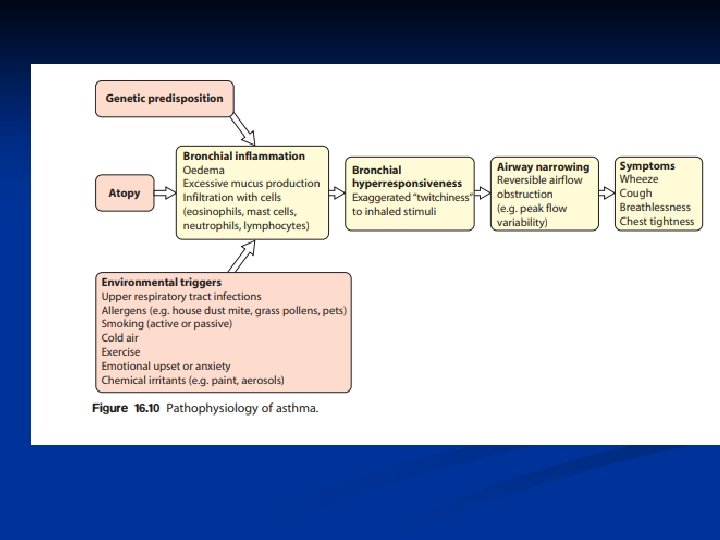
Pathogenesis ■ Airway inflammation also contributes to airflow limitation, which includes: • Bronchoconstriction • Edema • Chronic mucus plugging • Airway wall remodeling ■ All this leads to bronchial obstruction
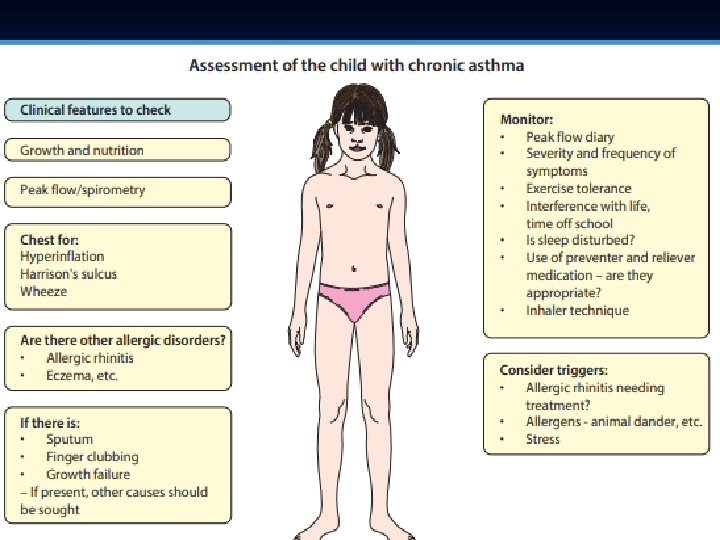
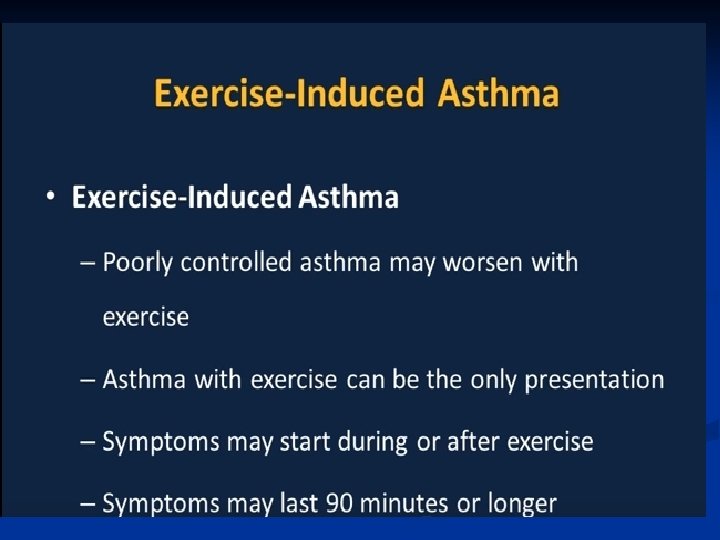
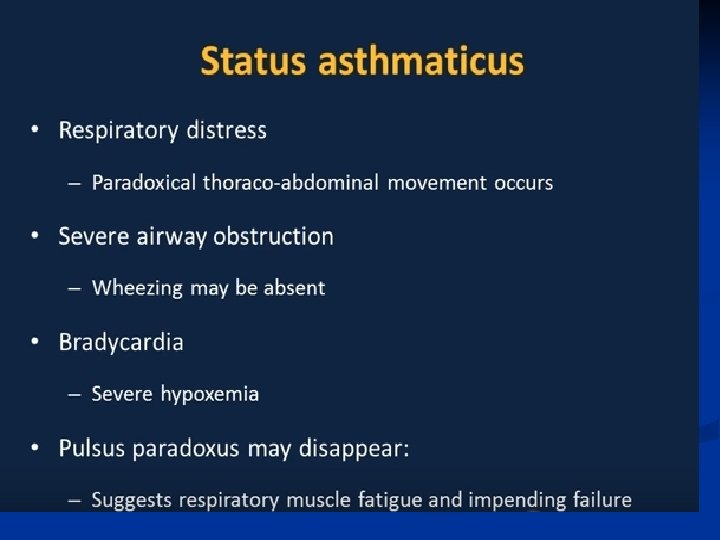
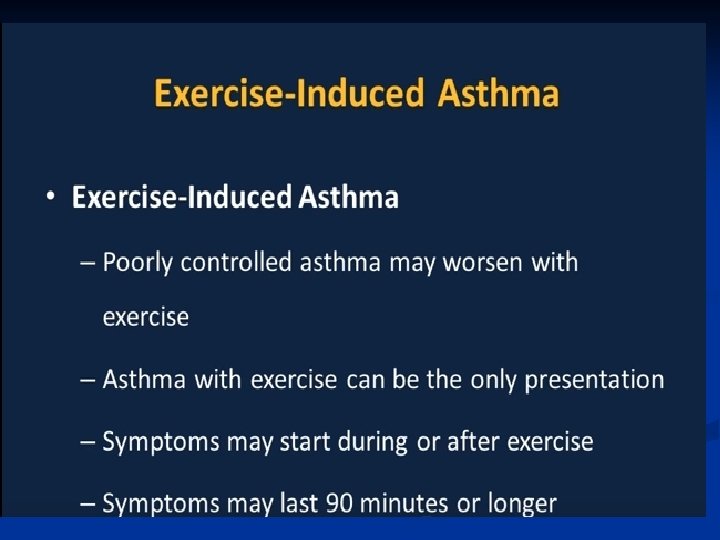
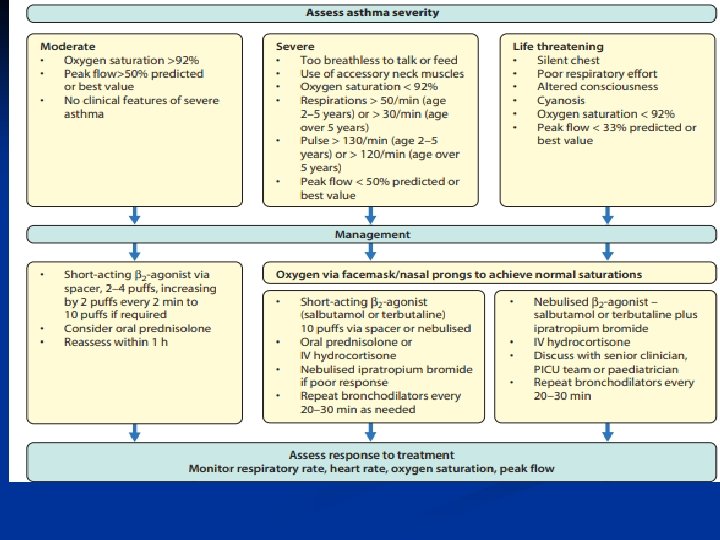
Clinical features Asthma should be suspected in any child with wheezing on more than one occasion. Other key features associated child having asthma include: ■ • Symptoms worse at night and in the early morning ■ • Symptoms that have triggers (e. g. exercise, pets, dust, cold air, emotions. ■ • Interval symptoms, i. e. symptoms between acute exacerbation. ■ • Personal or family history of an atopic disease ■ • Positive response to asthma therapy. ■
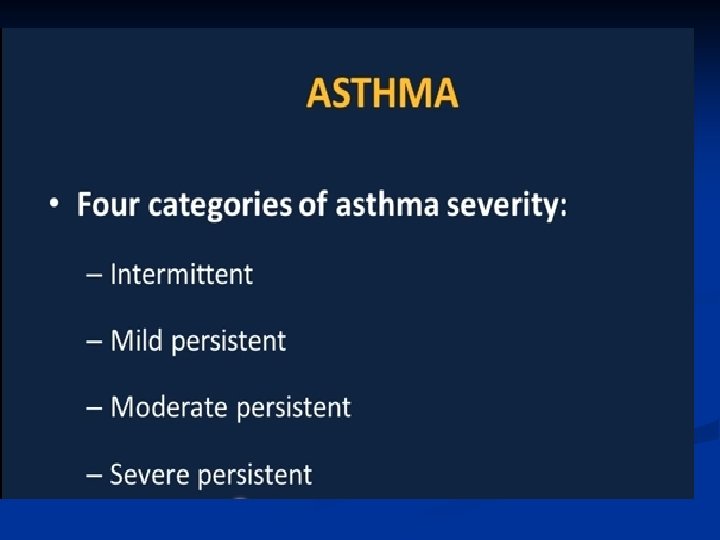
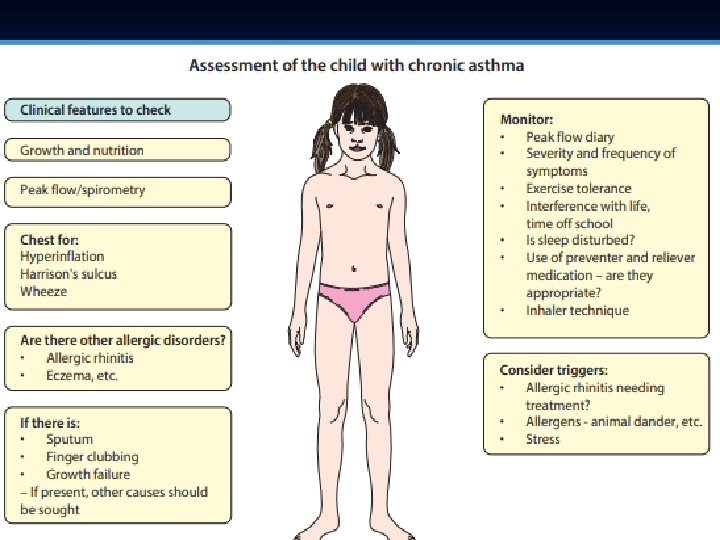
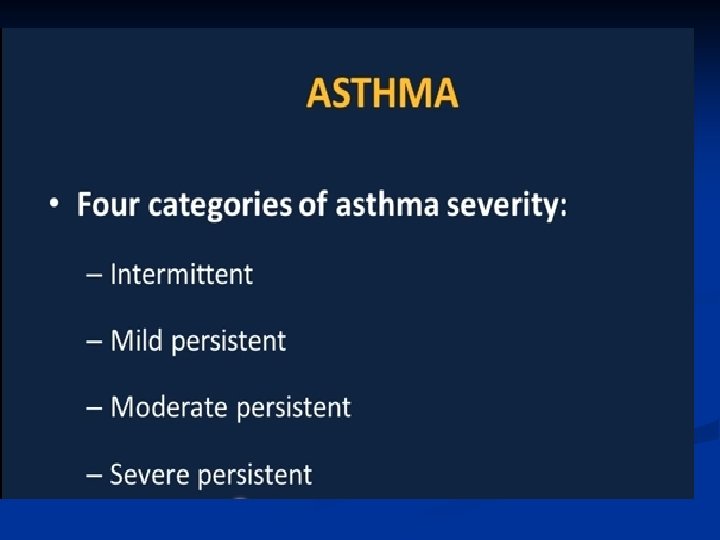
Patterns of Asthma According to ■ ■ ■ • How frequent are the symptoms? • What triggers the symptoms? Specifically, are sport and general activities affected by the asthma? • How often is sleep disturbed by asthma? • How severe are the interval symptoms between exacerbations? • How much school has been missed due to asthma?
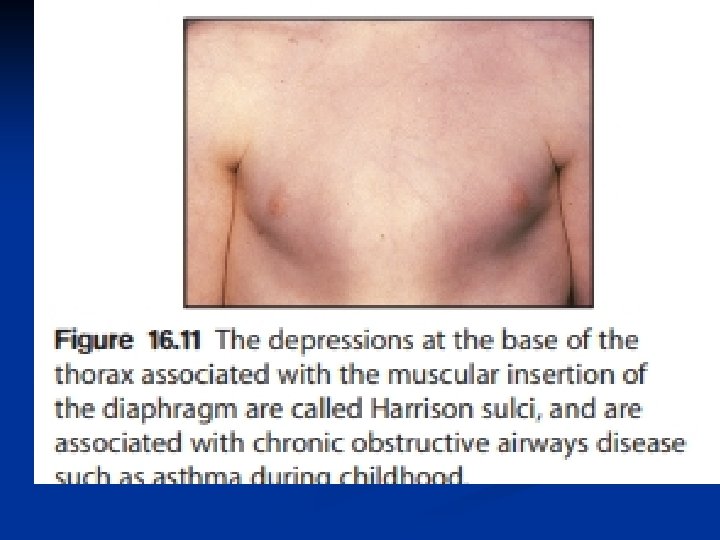
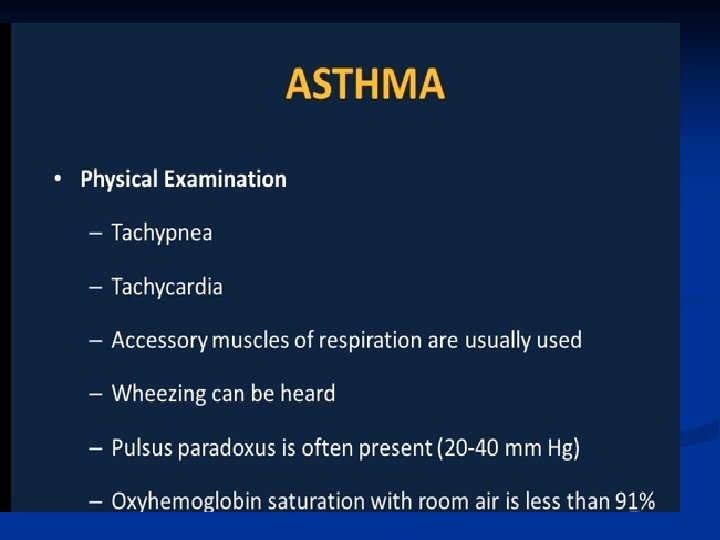
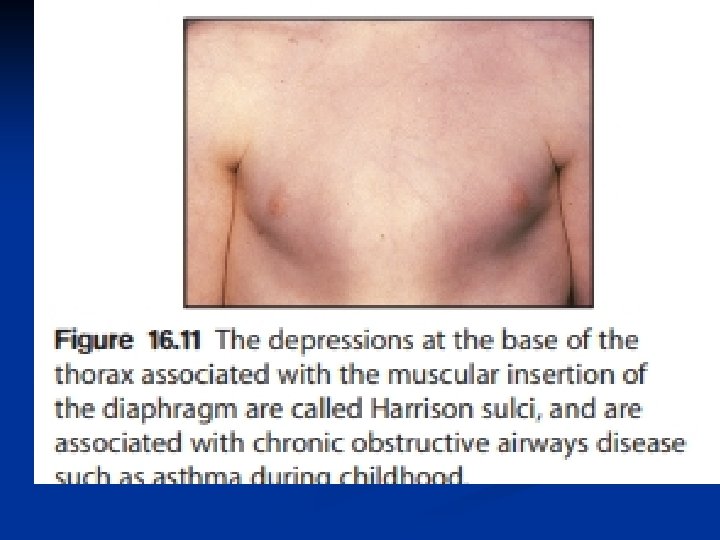
Examination of the chest is usually normal between attacks. ■ In long-standing asthma there may be hyperinflation of the chest. ■ generalised polyphonic expiratory wheeze and a prolonged expiratory phase. ■ Onset of the disease in early childhood may result in Harrison sulci. ■ Evidence of eczema and allergic rhinitid should be sought, ■. Growth should be plotted but is normal unless the asthma is extremely severe. ■

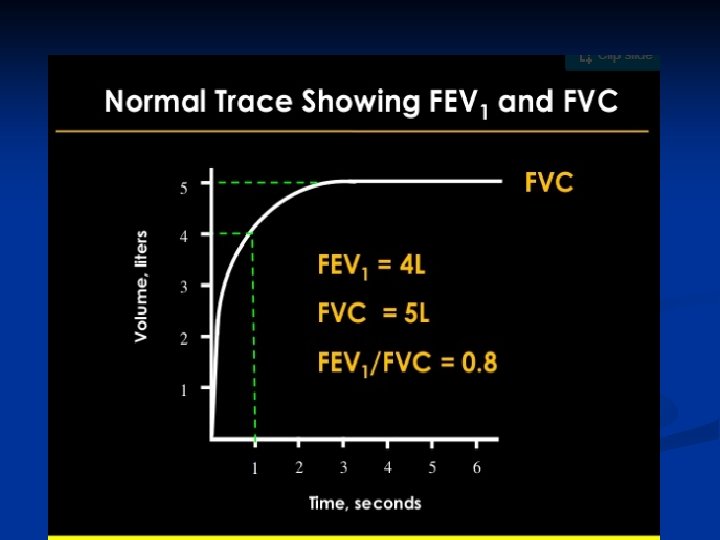
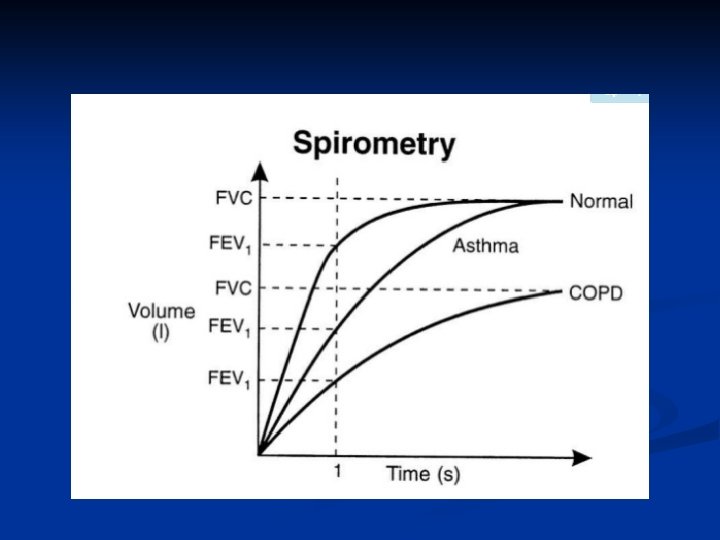
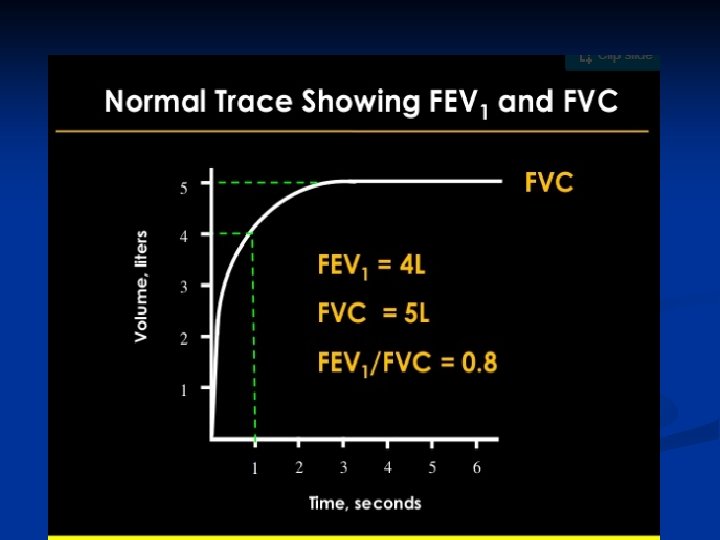
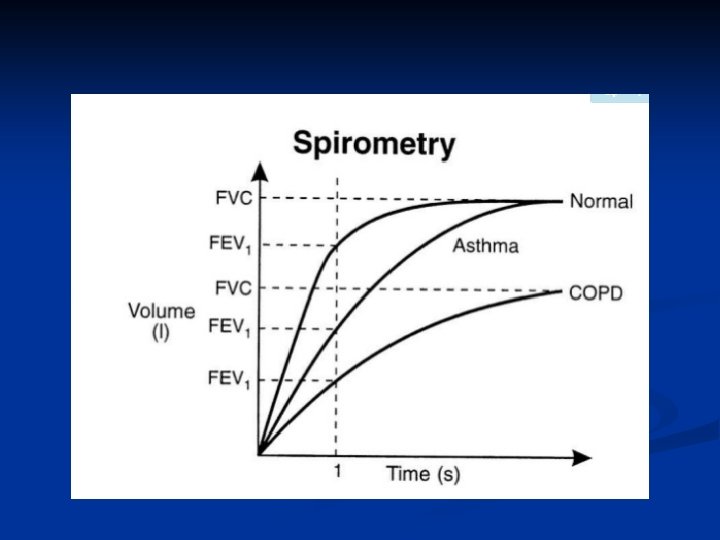
Function Testing ■ Determines ■ Degree of airway obstruction ■ Other lung disorders
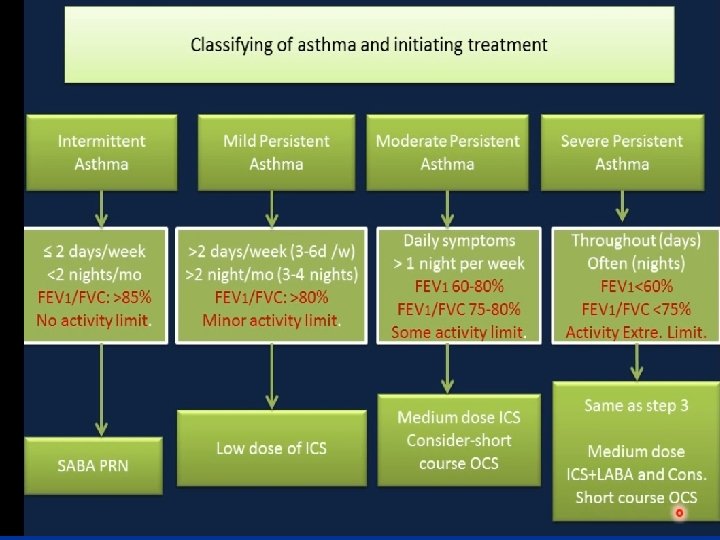
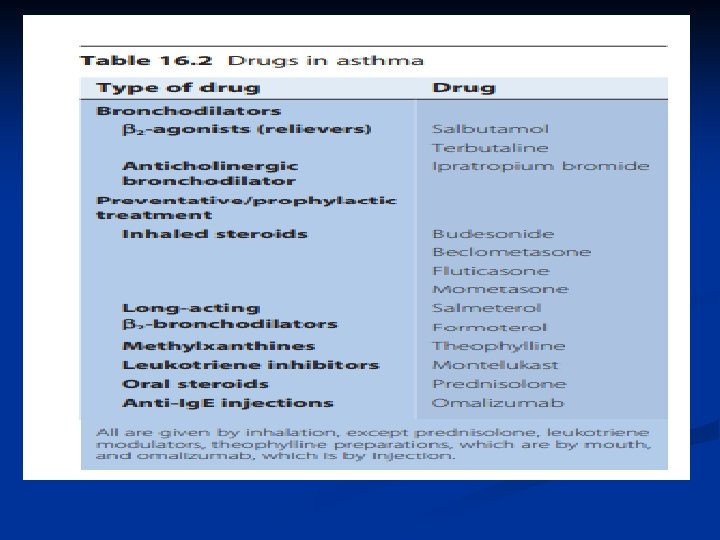
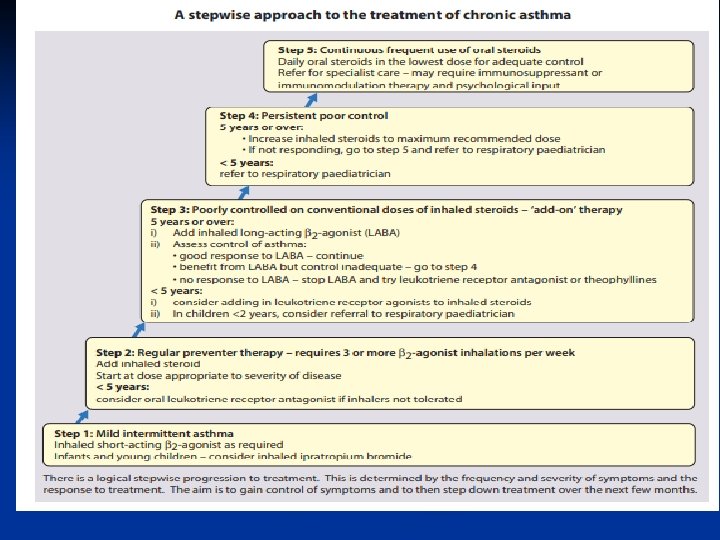
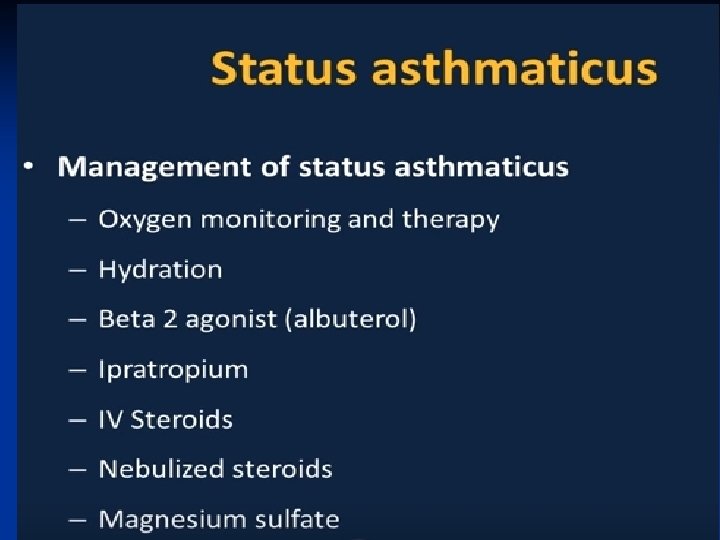
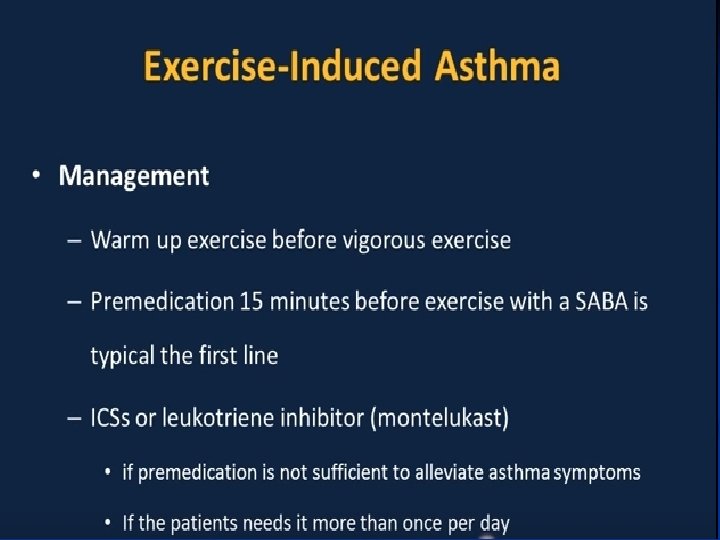
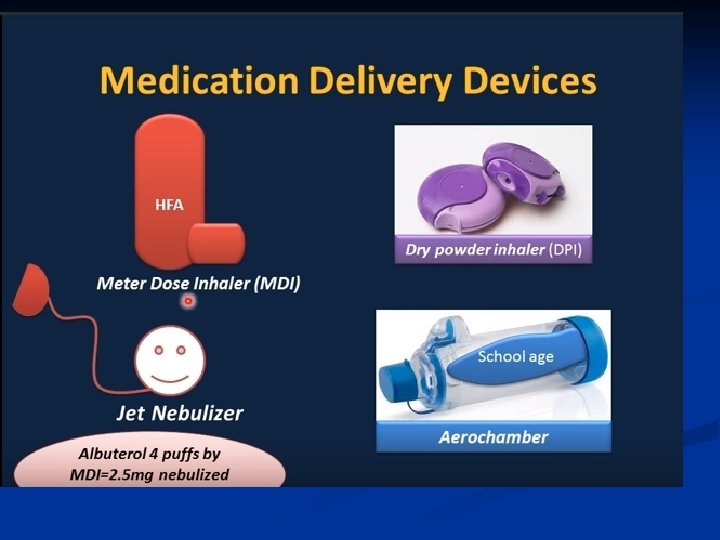
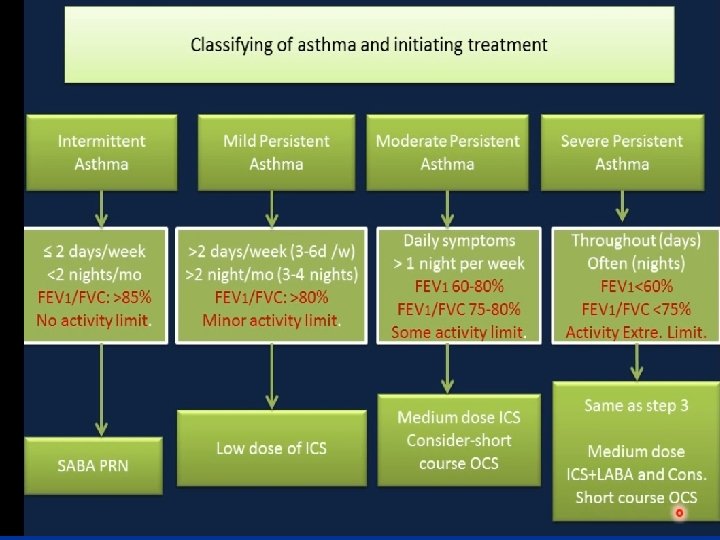
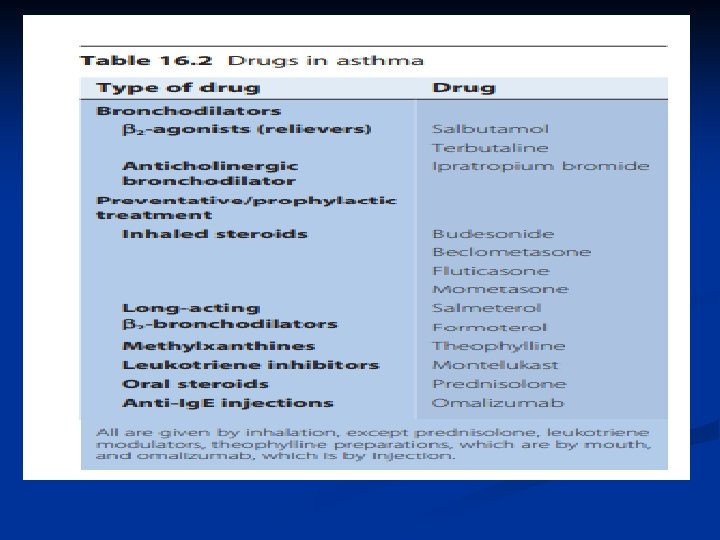
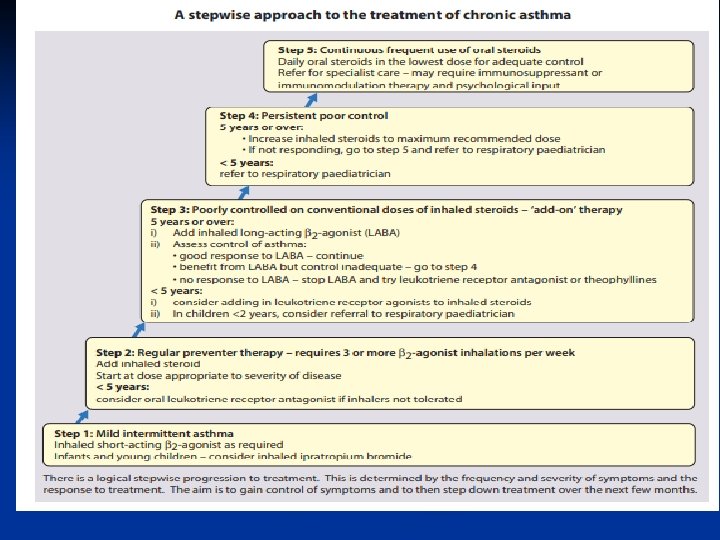
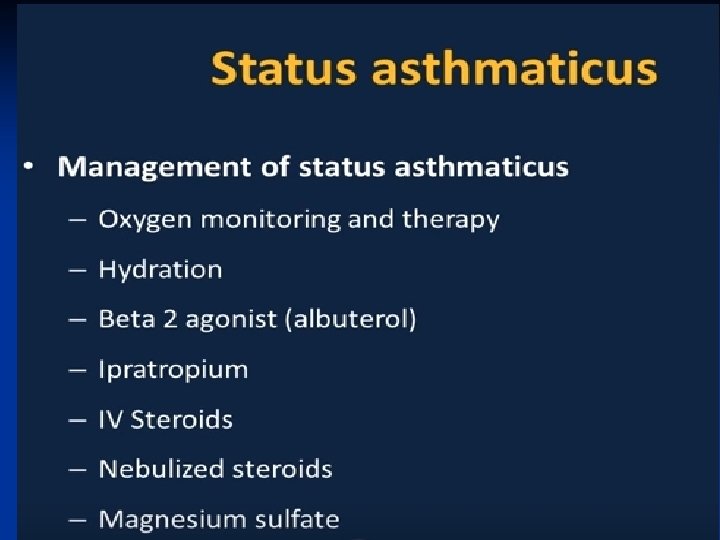
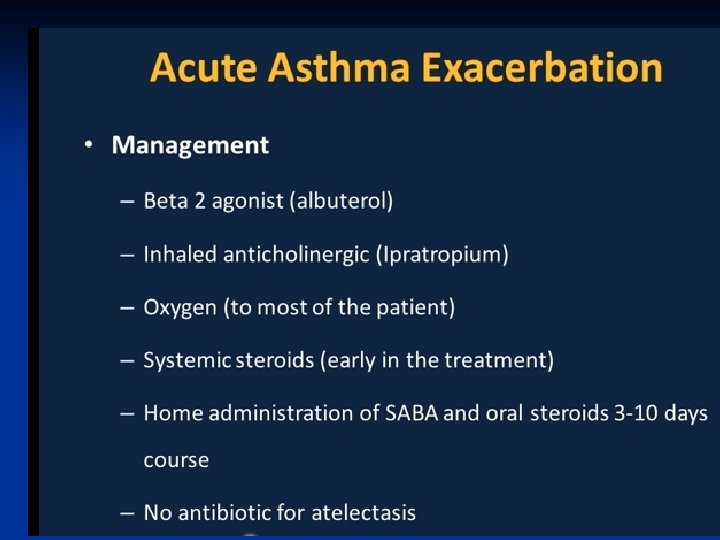
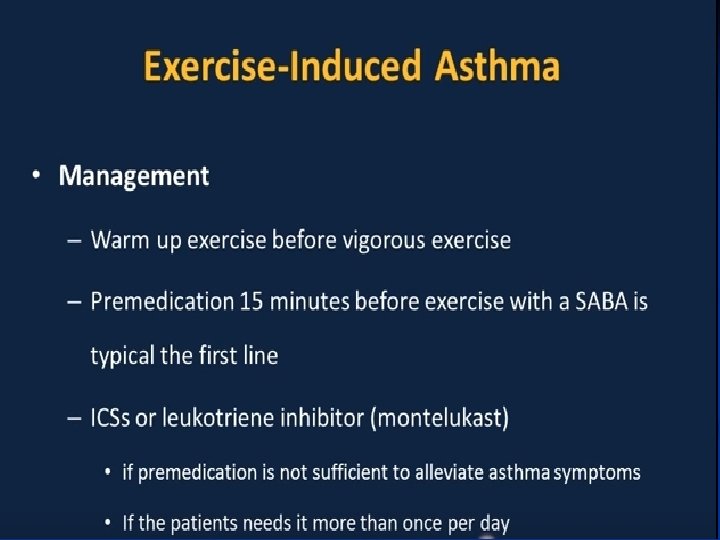
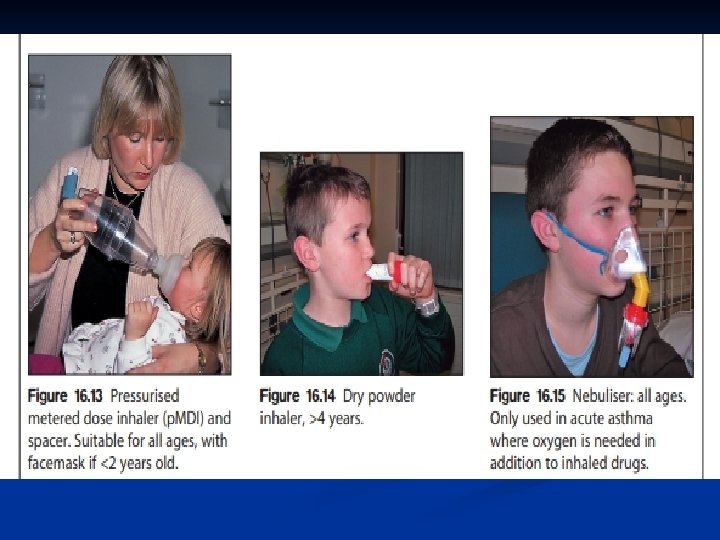
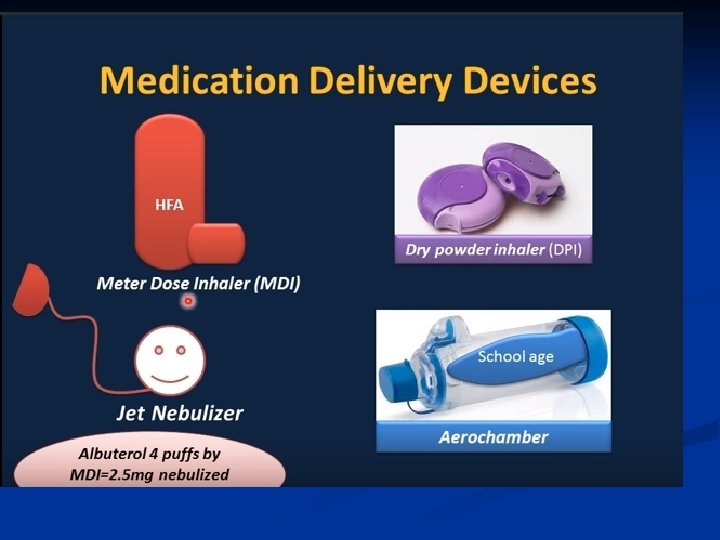
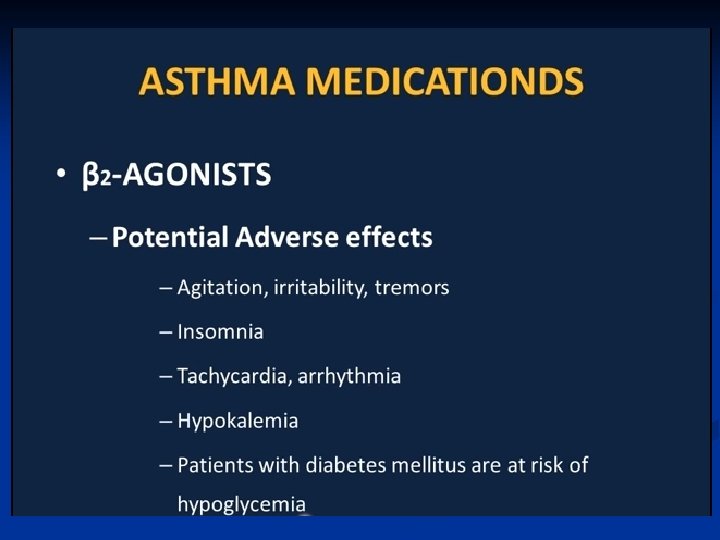
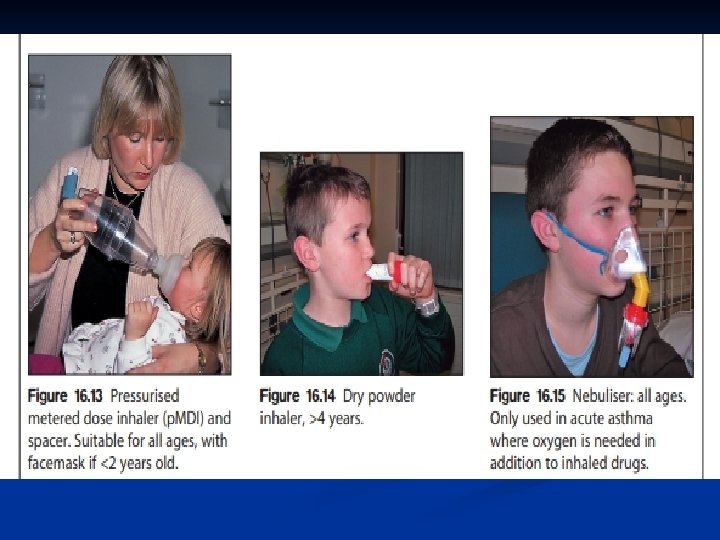
Bronchodilator therapy Inhaled β 2 -agonists are the most commonly used and most effective bronchodilators. Short-actingβ 2 -agonists ■ have a rapid onset of action, effective for 2– 4 h ■ have few side-effects. ■ They are used as required for increased symptoms, and in high doses for acute asthma attacks. long-actingβ 2 -agonists (LABAs)such as salmeterol or formoterol are effective for 12 h. ■ They are not used in acute asthma, and ■ should not be used without an inhaled cortico. ■ LABAs are useful in exercise-induced asthma. ■
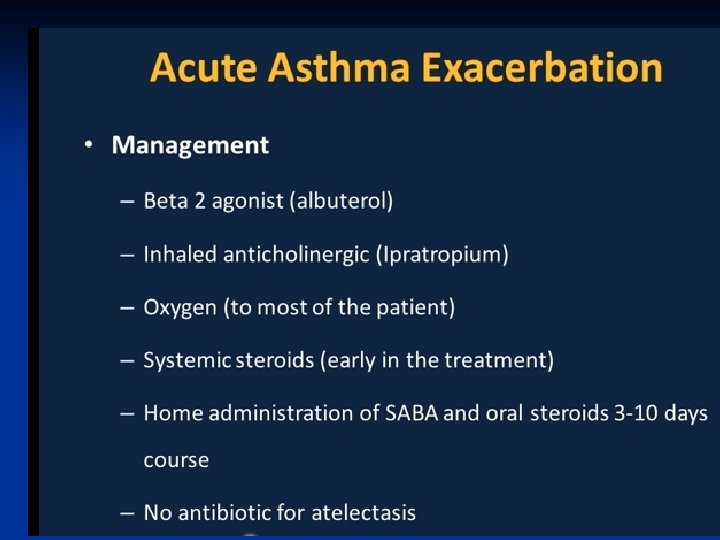
Ipratropium bromide ■ ■ an anticholinergic bronchodilator, is sometimes given to young infants when other bronchodilators are found to be ineffective, or in the treatment of severe acute asthma.
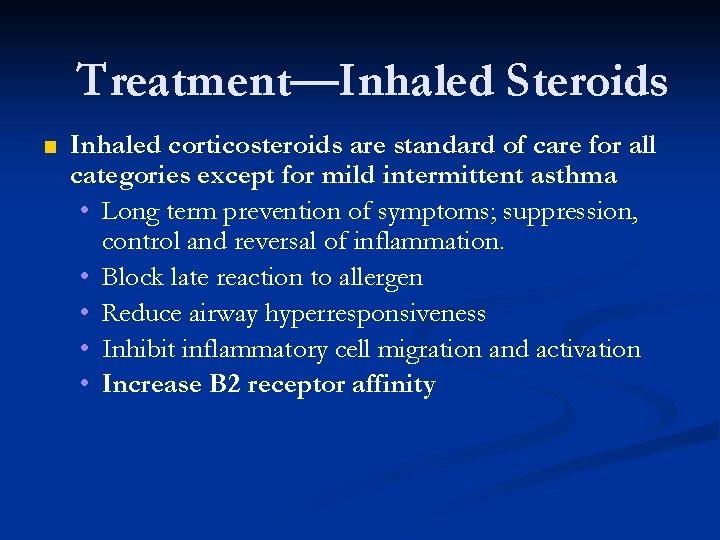
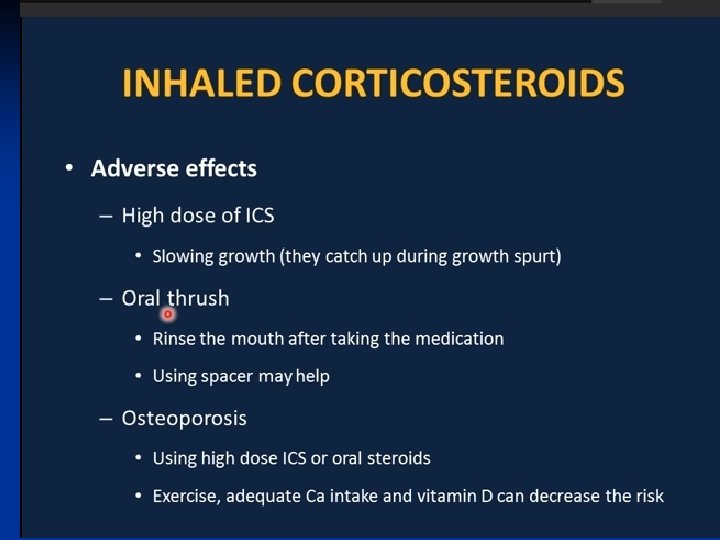
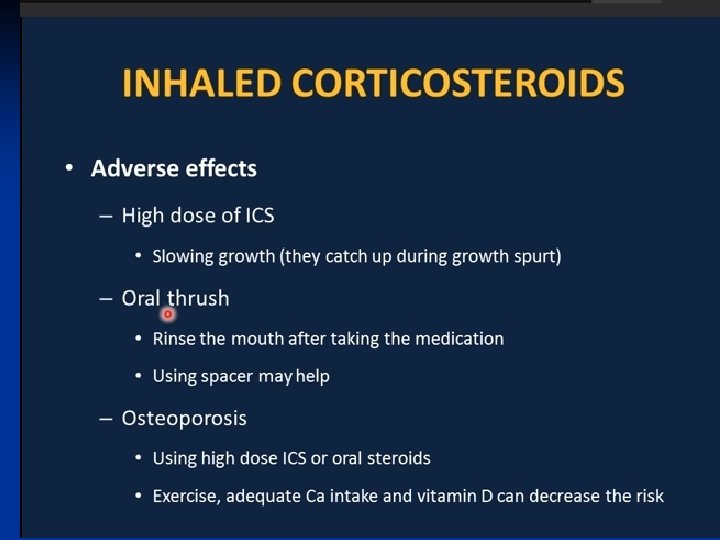
Treatment—Inhaled Steroids ■ Inhaled corticosteroids are standard of care for all categories except for mild intermittent asthma • Long term prevention of symptoms; suppression, control and reversal of inflammation. • Block late reaction to allergen • Reduce airway hyperresponsiveness • Inhibit inflammatory cell migration and activation • Increase B 2 receptor affinity
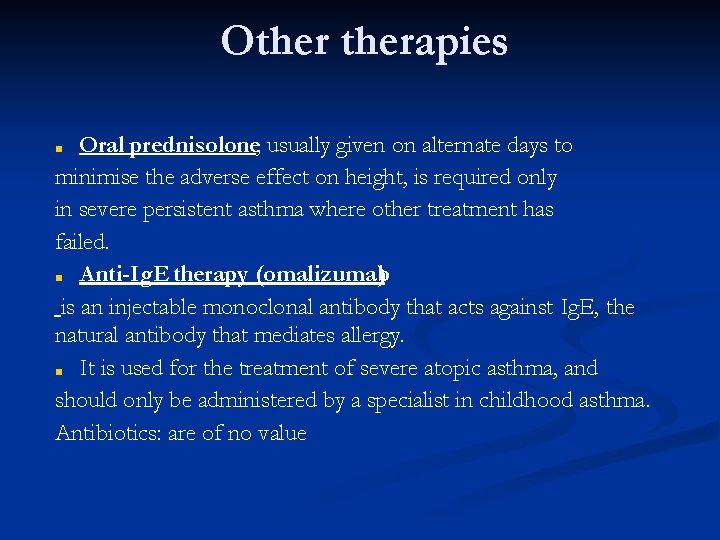
Otherapies Oral prednisolone, usually given on alternate days to minimise the adverse effect on height, is required only in severe persistent asthma where other treatment has failed. ■ Anti-Ig. E therapy (omalizumab ) is an injectable monoclonal antibody that acts against Ig. E, the natural antibody that mediates allergy. ■ It is used for the treatment of severe atopic asthma, and should only be administered by a specialist in childhood asthma. Antibiotics: are of no value ■
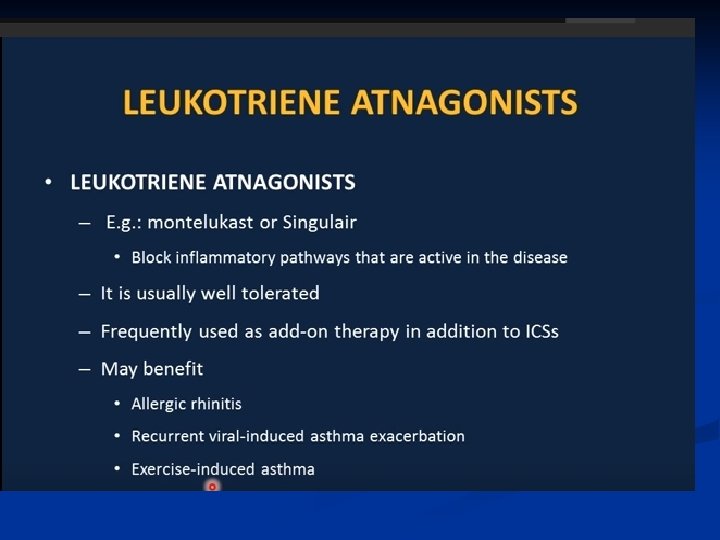
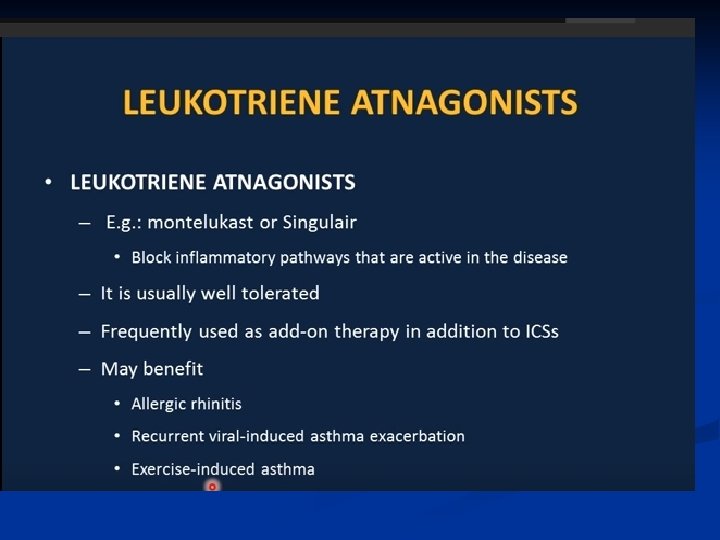
Add-on therapy LABA: ■ The first choice of add-on therapy in a child over 5 years ■ leukotriene receptor antagonist such as montelukast is Recommended in children under 5 years. Also used when LABA fails to control symptoms. ■ Slow-release oral theophyllineis an alternative; however, it has a high incidence of sideeffects (vomiting, insomnia, headaches, poor concentration), so it is not commonly used in children. ■
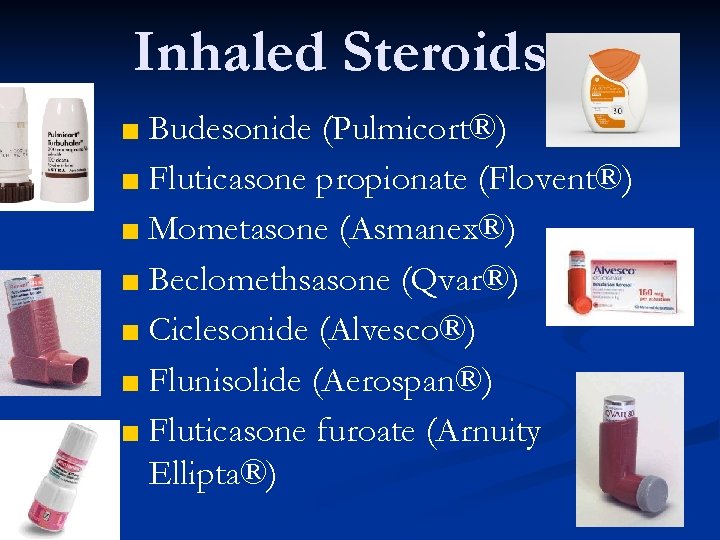
Inhaled Steroids ■ Budesonide (Pulmicort®) ■ Fluticasone propionate (Flovent®) ■ Mometasone (Asmanex®) ■ Beclomethsasone (Qvar®) ■ Ciclesonide (Alvesco®) ■ Flunisolide (Aerospan®) ■ Fluticasone furoate (Arnuity Ellipta®)

Combination Therapy ■ Fluticasone + Salmeterol (Advair®) ■ Budesonide +Formoterol (Symbicort®) ■ Mometasone +Formoterol (Dulera®) ■ Fluticasone +Salmeterol (Air. Duo Respiclick®)