Appropriate and Inappropriate ADH Secretion in the Postoperative
- Slides: 19
Appropriate and Inappropriate ADH Secretion in the Post-operative Patient
Objectives • Discuss normal ADH production and activity • Describe inappropriate ADH secretion • Review causes and treatment of SIADH
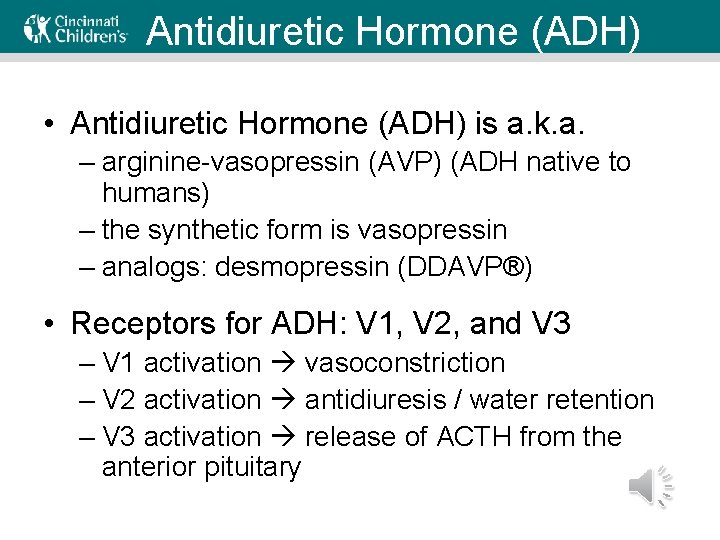
Antidiuretic Hormone (ADH) • Antidiuretic Hormone (ADH) is a. k. a. – arginine-vasopressin (AVP) (ADH native to humans) – the synthetic form is vasopressin – analogs: desmopressin (DDAVP®) • Receptors for ADH: V 1, V 2, and V 3 – V 1 activation vasoconstriction – V 2 activation antidiuresis / water retention – V 3 activation release of ACTH from the anterior pituitary
Antidiuretic Hormone (ADH) Effects and uses of ADH include • Antidiuresis • Vasoconstriction • Platelet aggregation • Regulation of the ACTH-adrenal axis
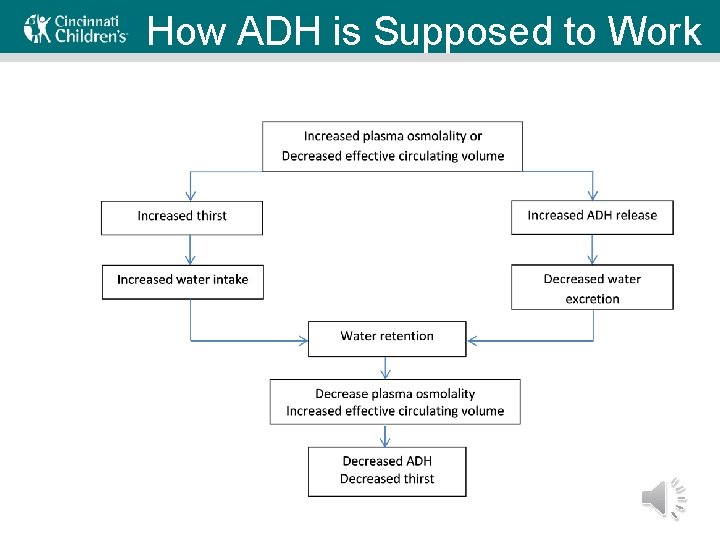
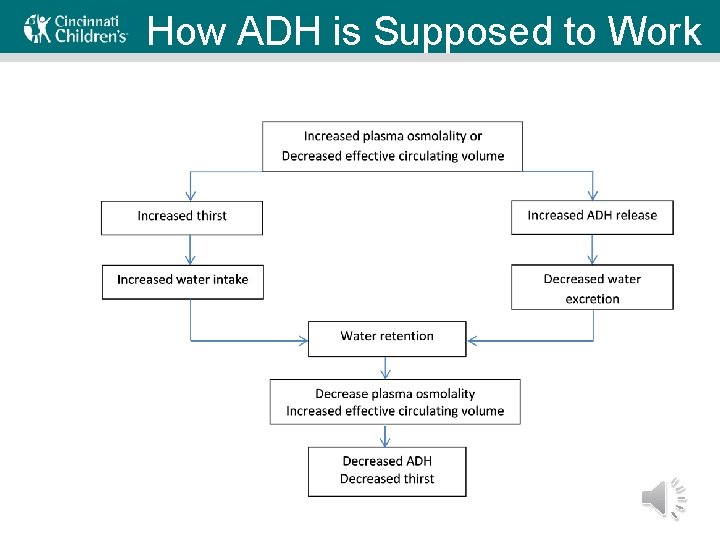
How ADH is Supposed to Work
ADH FYI • Half-life of ADH in the circulation is 15 -20 minutes • A small amount of ADH can be released directly from the hypothalamus. • As a result, posterior pituitary lesions don’t automatically lead to complete ADH deficiency • Hypovolemia (> 5 -10% depletion) can also stimulate ADH secretion
Case • You are called to evaluate a patient who is POD #2 from a VP shunt revision. She is more sleepy than normal, and per parental report she is getting more sleepy today than she was yesterday. She is still not eating well and is on IV fluids. – She had a head CT this morning that showed improvement. She has weaned down on her medications. The team would like your help regarding her increased sleepiness.
Syndrome of Inappropriate ADH • ADH is released regardless of plasma osmolality • ADH promotes water reabsorption in the collecting tubules • This increases TBW, which dilutes plasma (lower Na and osmolality) & increases blood volume • Increased blood volume triggers solute/Na+ excretion • This causes even greater decreases in plasma sodium and osmolality
Causes of SIADH (Part 1 of 3) • CNS disturbances – stroke, hemorrhage, infection, trauma, and psychosis • Pulmonary processes – most notably pneumonia (viral, bacterial, or TB) – asthma, atelectasis, acute respiratory failure, and pneumothorax • • Ectopic production of ADH by a tumor Hypopituitarism Hypothyroidism Hereditary SIADH
Causes of SIADH (Part 2 of 3) Iatrogenic or medication induced: • Desmopressin or oxytocin • Psych meds: SSRIs, amitriptyline, MAO inhibitors, haloperidol • Anti-epileptics: carbamazepine, oxcarbazepine, and valproate • Pain relievers: opiates, NSAIDs • Nicotine • Heme-Onc meds: cyclophospamide, vincristine, vinblastine, cisplatin, ifosfamide, methotrexate, interferon -alpha, interferon-gamma, bromocriptine
Causes of SIADH (Part 3 of 3) • Factors that STIMULATE Release of ADH – Surgery – Stress / Pain – Nausea – Pregnancy – Hypoglycemia
Findings in SIADH Historical or exam features that raise concern: • Signs of causes of SIADH • Anorexia, nausea in milder hyponatremia • Confusion, lethargy, tremor, other abnormal neurologic findings in more significant hyponatremia Main laboratory findings in SIADH are: • Hyponatremia (<135 mmol/L) • Hypoosmolality • Urine osmolality > 100 mosmol/kg • Urine sodium usually > 40 meq/L • Normal serum potassium, creatinine and acid-base status • Normal adrenal and thyroid function
Severe Complication of SIADH • Severe neurologic symptoms, typically seizures, can occur (usually Na <120 meq/L) – Require rapid initial correction with hypertonic saline. – Overly rapid correction can lead to osmotic demyelination • Increasing sodium by ≤ 9 meq/L over 24 hours is recommended • Moderate hyponatremia (Na 120 to 129 meq/L) – Usually asymptomatic – Slow correction of the hyponatremia
Treatment: Step 1 Treat the underlying disease, if possible • Treat infections – E. g. meningitis, pneumonia, tuberculosis • Stop contributing drugs, if possible – DDAVP, SSRIs, AEDs – Opiates, NSAIDs • Replace hormones – Replace cautiously in adrenal insufficiency – Per usual in hypothyroidism
Treatment: Step 2 Increase the serum sodium • Fluid restriction – Beware of cerebral salt wasting in the setting of subarachnoid hemorrhage or signs of volume depletion • IV Fluids – concentration of IVF must exceed the electrolyte concentration of the urine not just the plasma • Enteral sodium +/- a loop diuretic • Vasopressin receptor antagonists
Key Points • ADH serves a needed function to regulate volume and solute status • Hospitalized patients are at high risk for SIADH, particularly those who also undergo surgery • Identification of the cause of SIADH is key to treatment
Questions for Review • List 3 risk factors for SIADH that postoperative patients are at high risk for. • Explain how SIADH results in hyponatremia.
Further Discussion • You are about to go see your new consult. With a improving head CT and decreased pain medications, you think that her sleepiness is less likely due to acute surgical issue or over-sedation from narcotics. You suspect she may have SIADH. What are the key parts of your physical exam? What laboratory data do you want to order?
References 1. Dunn FL, Brennan TJ, Nelson AE, Robertson GL. The role of blood osmolality and volume in regulating vasopressin secretion in the rat. The Journal of clinical investigation. Dec 1973; 52(12): 3212 -3219. 2. Robertson GL, Aycinena P, Zerbe RL. Neurogenic disorders of osmoregulation. The American journal of medicine. Feb 1982; 72(2): 339 -353. Rose BD, Post TW. Chapter 6 B: Antidiuretic hormone and water balance. www. uptodate. com. 2000. 4. Steele A, Gowrishankar M, Abrahamson S, Mazer CD, Feldman RD, Halperin ML. Postoperative hyponatremia despite near-isotonic saline infusion: a phenomenon of desalination. Annals of internal medicine. Jan 1 1997; 126(1): 20 -25. Sterns RH. Pathophysiology and etiology of the syndrome of inappropriate antidiuretic hormone secretion (SIADH). www. uptodate. com. 2012. 6. Sterns RH. Evaluation of the patient with hyponatremia. www. uptodate. com. 2013. 7. Sterns RH. Treatment of hyponatremia: Syndrome of inappropriate antidiuretic hormone secretion (SIADH) and reset osmostat. www. uptodate. com. 2013. 8. Sterns RH. Overview of the treatment of hyponatremia. www. uptodate. com. 2013.