Adequate 3 D Treatment Volume in Preoperative Radiotherapy

- Slides: 21
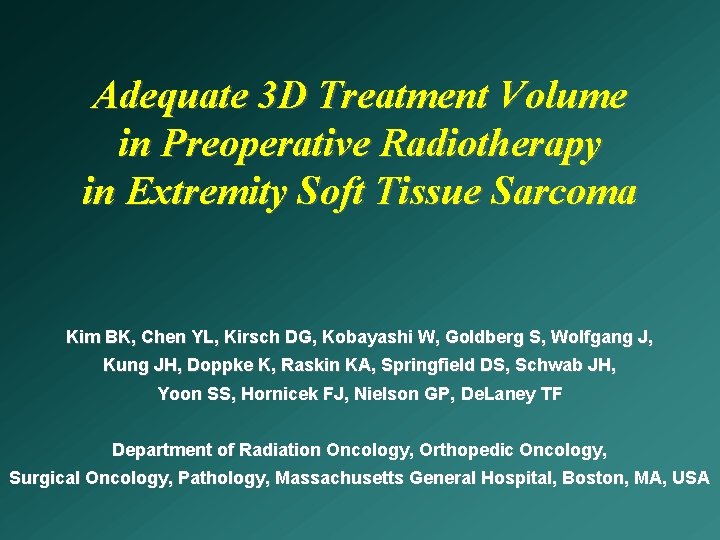
Adequate 3 D Treatment Volume in Preoperative Radiotherapy in Extremity Soft Tissue Sarcoma Kim BK, Chen YL, Kirsch DG, Kobayashi W, Goldberg S, Wolfgang J, Kung JH, Doppke K, Raskin KA, Springfield DS, Schwab JH, Yoon SS, Hornicek FJ, Nielson GP, De. Laney TF Department of Radiation Oncology, Orthopedic Oncology, Surgical Oncology, Pathology, Massachusetts General Hospital, Boston, MA, USA
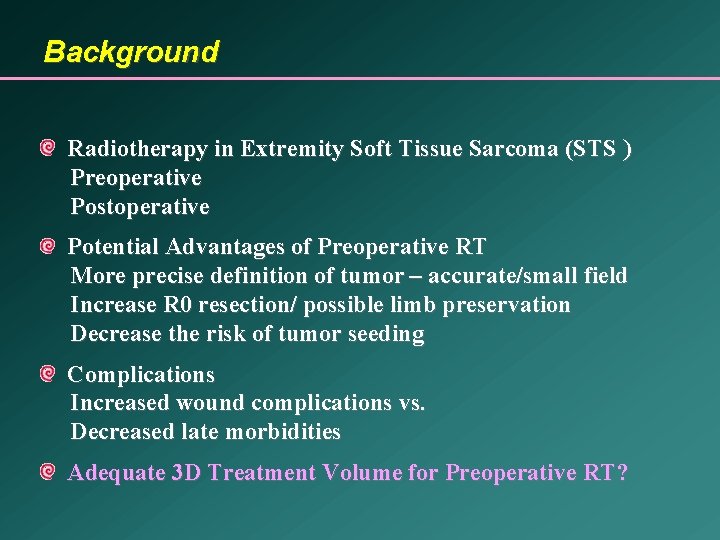
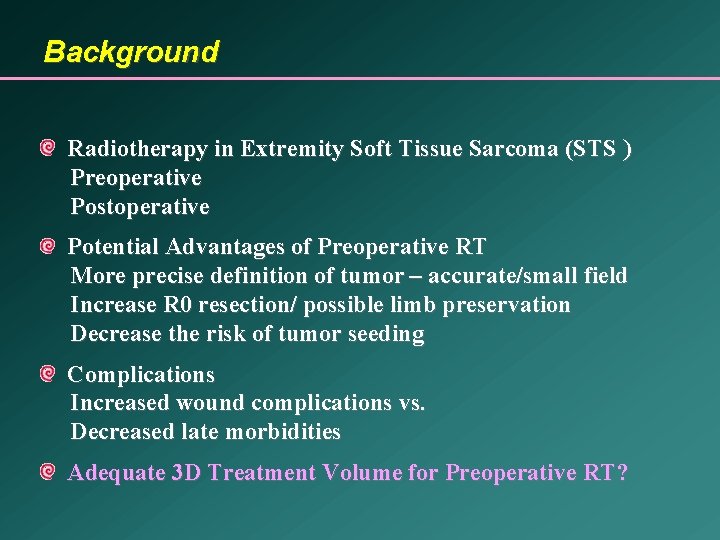
Background Radiotherapy in Extremity Soft Tissue Sarcoma (STS ) Preoperative Postoperative Potential Advantages of Preoperative RT More precise definition of tumor – accurate/small field Increase R 0 resection/ possible limb preservation Decrease the risk of tumor seeding Complications Increased wound complications vs. Decreased late morbidities Adequate 3 D Treatment Volume for Preoperative RT?
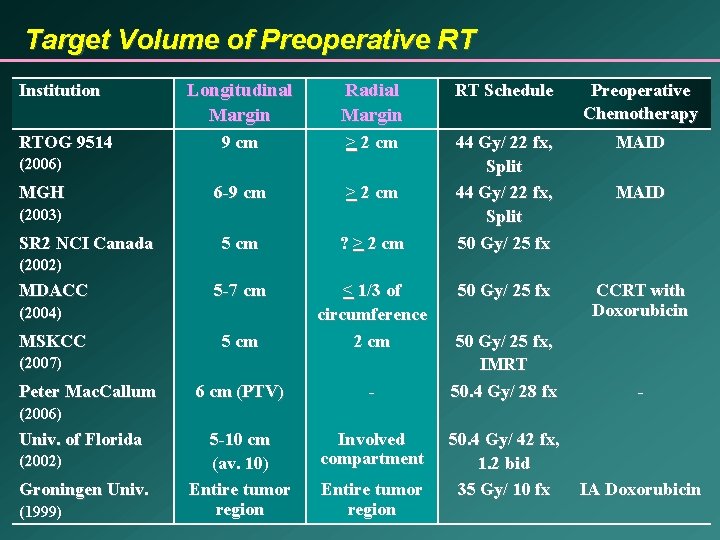
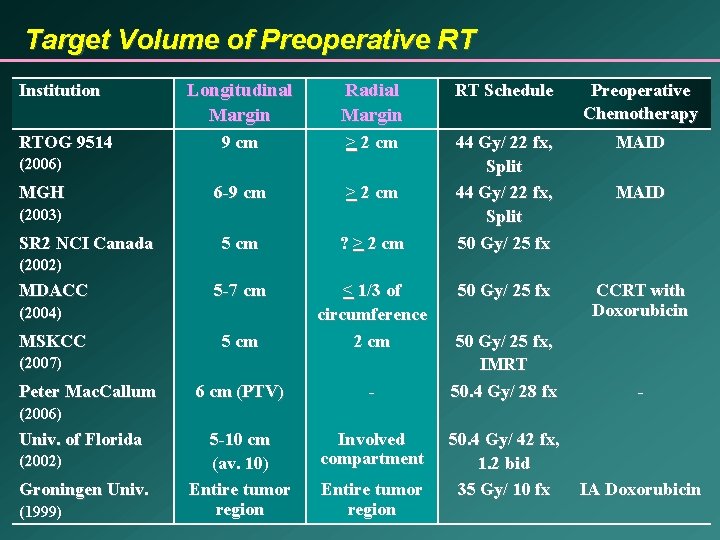
Target Volume of Preoperative RT Institution RTOG 9514 Longitudinal Margin Radial Margin RT Schedule Preoperative Chemotherapy 9 cm > 2 cm MAID 6 -9 cm > 2 cm 5 cm ? > 2 cm 44 Gy/ 22 fx, Split 50 Gy/ 25 fx 5 -7 cm 50 Gy/ 25 fx CCRT with Doxorubicin 5 cm < 1/3 of circumference 2 cm 6 cm (PTV) - 5 -10 cm (av. 10) Entire tumor region Involved compartment (2006) MGH (2003) SR 2 NCI Canada MAID (2002) MDACC (2004) MSKCC (2007) Peter Mac. Callum 50 Gy/ 25 fx, IMRT 50. 4 Gy/ 28 fx - 50. 4 Gy/ 42 fx, 1. 2 bid 35 Gy/ 10 fx IA Doxorubicin (2006) Univ. of Florida (2002) Groningen Univ. (1999) Entire tumor region
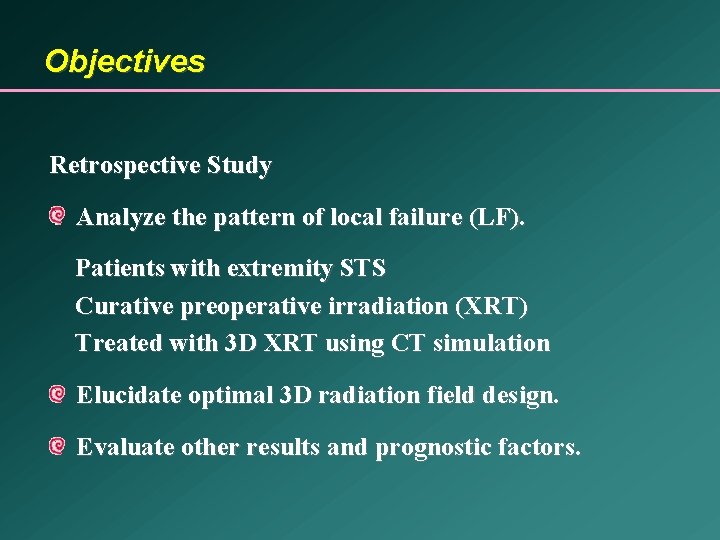
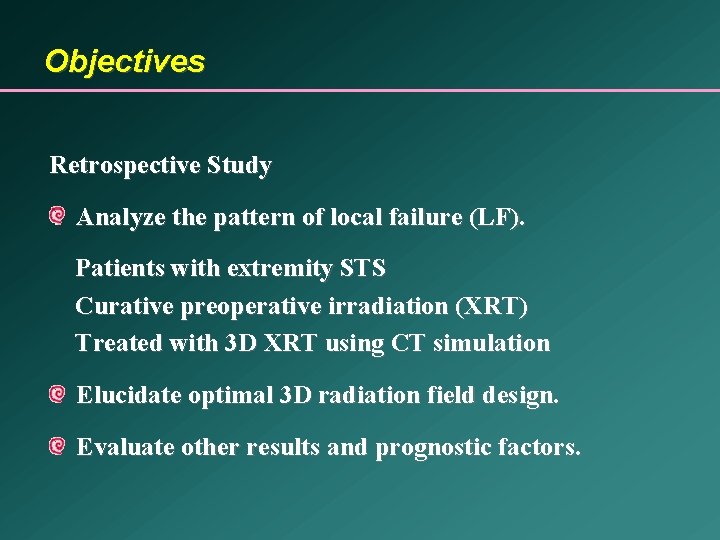
Objectives Retrospective Study Analyze the pattern of local failure (LF). Patients with extremity STS Curative preoperative irradiation (XRT) Treated with 3 D XRT using CT simulation Elucidate optimal 3 D radiation field design. Evaluate other results and prognostic factors.
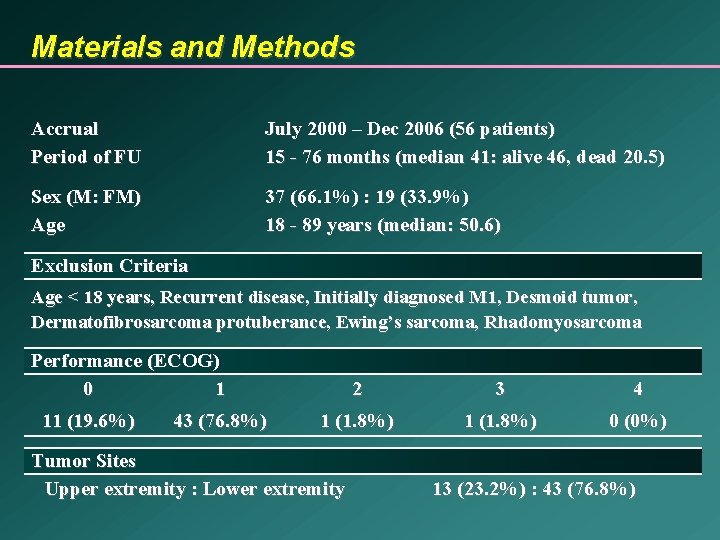
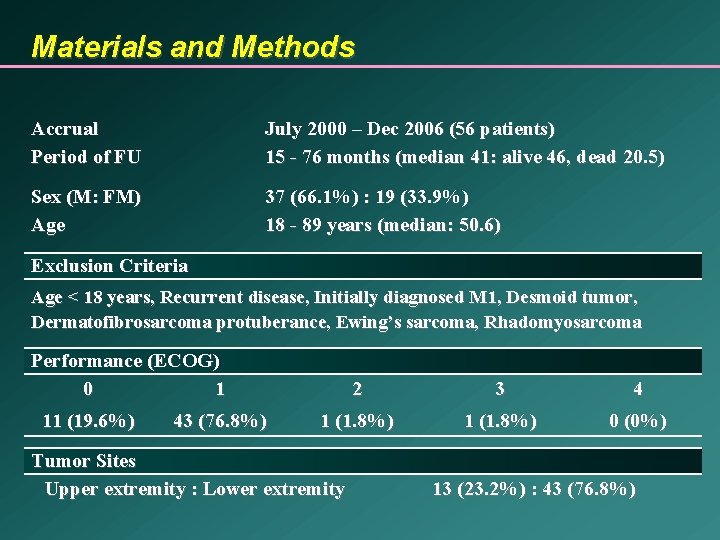
Materials and Methods Accrual Period of FU July 2000 – Dec 2006 (56 patients) 15 - 76 months (median 41: alive 46, dead 20. 5) Sex (M: FM) Age 37 (66. 1%) : 19 (33. 9%) 18 - 89 years (median: 50. 6) Exclusion Criteria Age < 18 years, Recurrent disease, Initially diagnosed M 1, Desmoid tumor, Dermatofibrosarcoma protuberance, Ewing’s sarcoma, Rhadomyosarcoma Performance (ECOG) 0 1 11 (19. 6%) 43 (76. 8%) 2 3 4 1 (1. 8%) 0 (0%) Tumor Sites Upper extremity : Lower extremity 13 (23. 2%) : 43 (76. 8%)
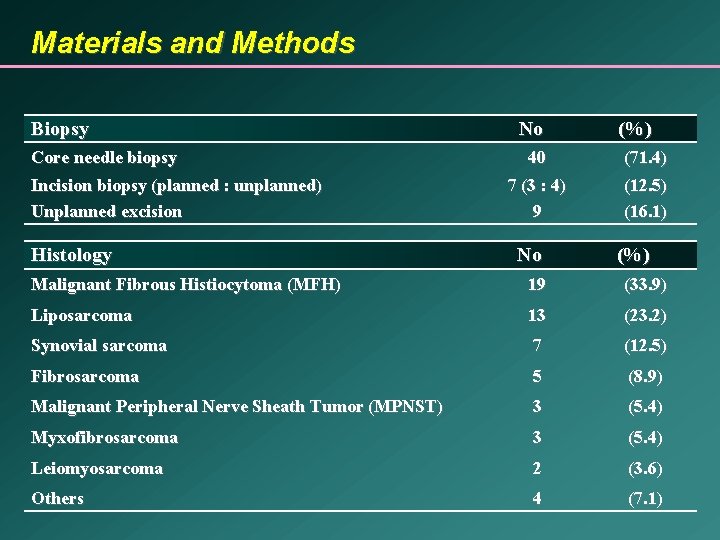
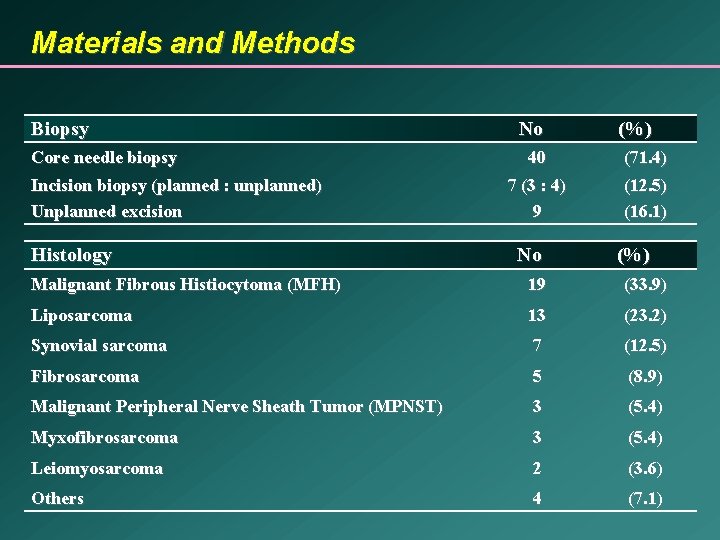
Materials and Methods Biopsy Core needle biopsy Incision biopsy (planned : unplanned) Unplanned excision Histology No (%) 40 (71. 4) 7 (3 : 4) 9 (12. 5) (16. 1) No (%) Malignant Fibrous Histiocytoma (MFH) 19 (33. 9) Liposarcoma 13 (23. 2) Synovial sarcoma 7 (12. 5) Fibrosarcoma 5 (8. 9) Malignant Peripheral Nerve Sheath Tumor (MPNST) 3 (5. 4) Myxofibrosarcoma 3 (5. 4) Leiomyosarcoma 2 (3. 6) Others 4 (7. 1)
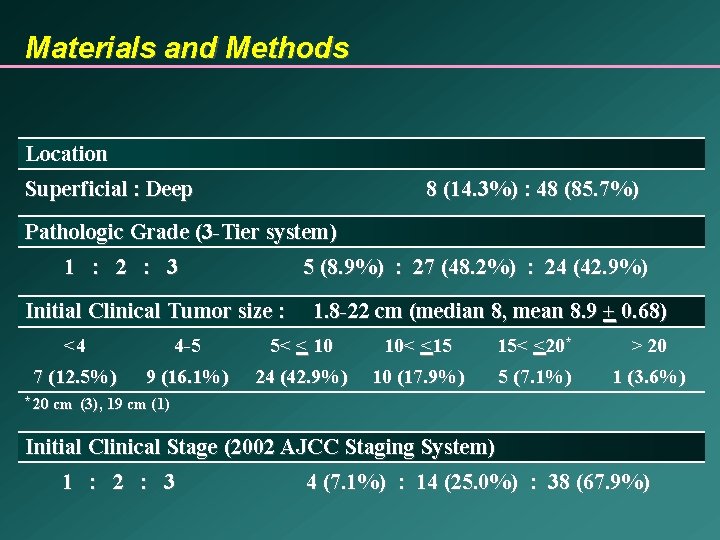
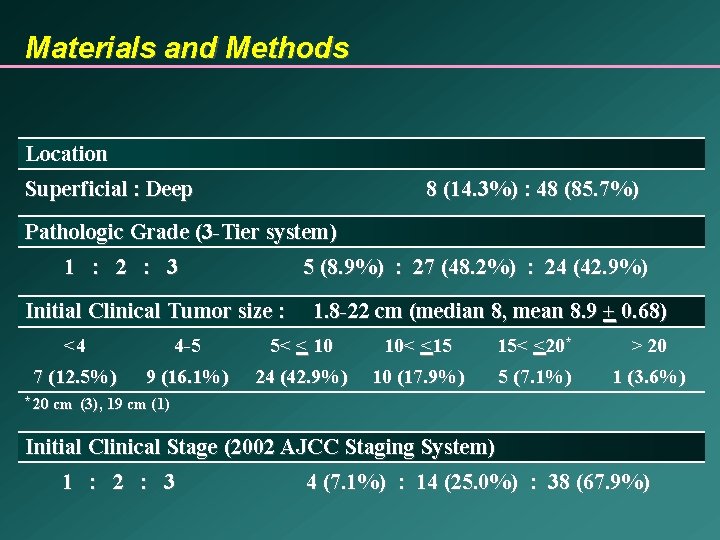
Materials and Methods Location Superficial : Deep 8 (14. 3%) : 48 (85. 7%) Pathologic Grade (3 -Tier system) 1 : 2 : 3 5 (8. 9%) : 27 (48. 2%) : 24 (42. 9%) Initial Clinical Tumor size : 1. 8 -22 cm (median 8, mean 8. 9 + 0. 68) <4 4 -5 5< < 10 10< <15 15< <20* > 20 7 (12. 5%) 9 (16. 1%) 24 (42. 9%) 10 (17. 9%) 5 (7. 1%) 1 (3. 6%) * 20 cm (3), 19 cm (1) Initial Clinical Stage (2002 AJCC Staging System) 1 : 2 : 3 4 (7. 1%) : 14 (25. 0%) : 38 (67. 9%)
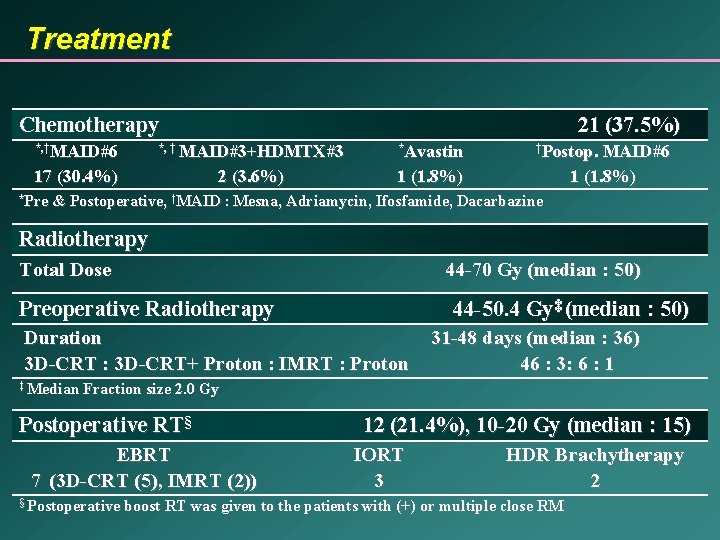
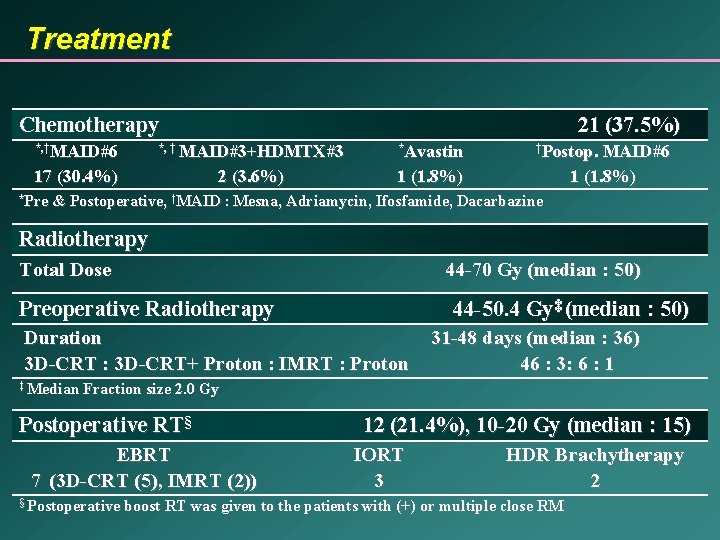
Treatment Chemotherapy 21 (37. 5%) *, †MAID#6 *, † MAID#3+HDMTX#3 *Avastin 17 (30. 4%) 2 (3. 6%) 1 (1. 8%) *Pre †Postop. MAID#6 1 (1. 8%) & Postoperative, †MAID : Mesna, Adriamycin, Ifosfamide, Dacarbazine Radiotherapy Total Dose 44 -70 Gy (median : 50) Preoperative Radiotherapy 44 -50. 4 Gy‡ (median : 50) Duration 3 D-CRT : 3 D-CRT+ Proton : IMRT : Proton ‡ Median 31 -48 days (median : 36) 46 : 3: 6 : 1 Fraction size 2. 0 Gy Postoperative RT§ EBRT 7 (3 D-CRT (5), IMRT (2)) § Postoperative 12 (21. 4%), 10 -20 Gy (median : 15) IORT 3 HDR Brachytherapy 2 boost RT was given to the patients with (+) or multiple close RM
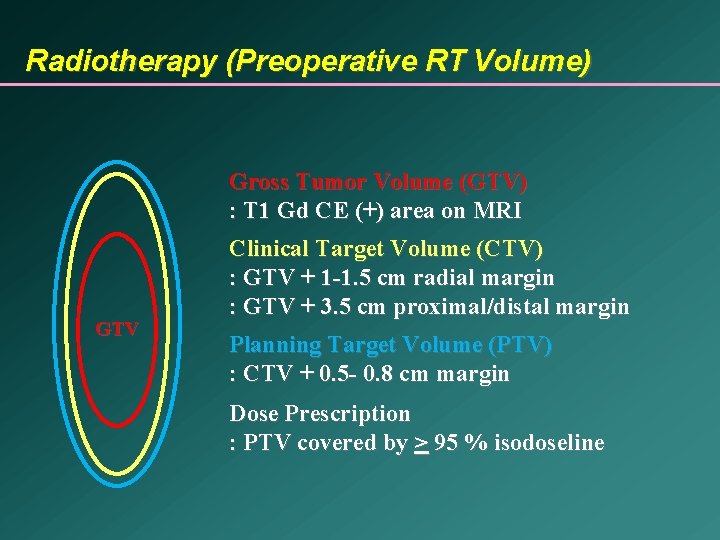
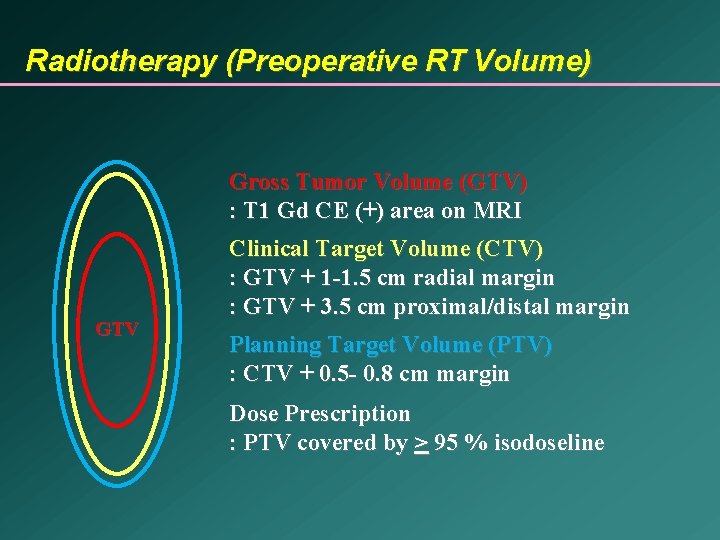
Radiotherapy (Preoperative RT Volume) Gross Tumor Volume (GTV) : T 1 Gd CE (+) area on MRI GTV Clinical Target Volume (CTV) : GTV + 1 -1. 5 cm radial margin : GTV + 3. 5 cm proximal/distal margin Planning Target Volume (PTV) : CTV + 0. 5 - 0. 8 cm margin Dose Prescription : PTV covered by > 95 % isodoseline
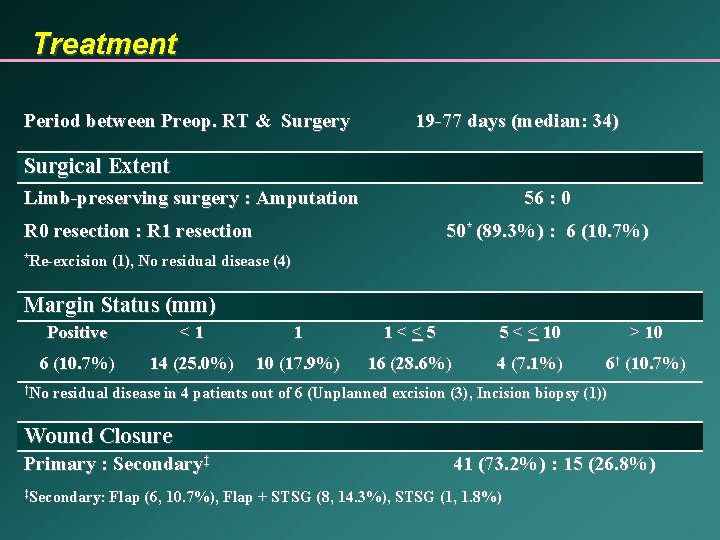
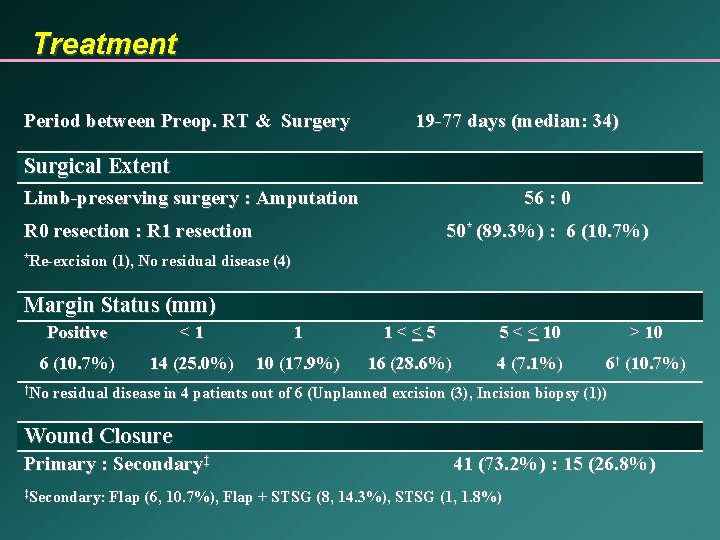
Treatment Period between Preop. RT & Surgery 19 -77 days (median: 34) Surgical Extent Limb-preserving surgery : Amputation 56 : 0 R 0 resection : R 1 resection *Re-excision 50* (89. 3%) : 6 (10. 7%) (1), No residual disease (4) Margin Status (mm) Positive <1 1 1<<5 5 < < 10 > 10 6 (10. 7%) 14 (25. 0%) 10 (17. 9%) 16 (28. 6%) 4 (7. 1%) 6† (10. 7%) †No residual disease in 4 patients out of 6 (Unplanned excision (3), Incision biopsy (1)) Wound Closure Primary : Secondary‡ ‡Secondary: Flap 41 (73. 2%) : 15 (26. 8%) (6, 10. 7%), Flap + STSG (8, 14. 3%), STSG (1, 1. 8%)
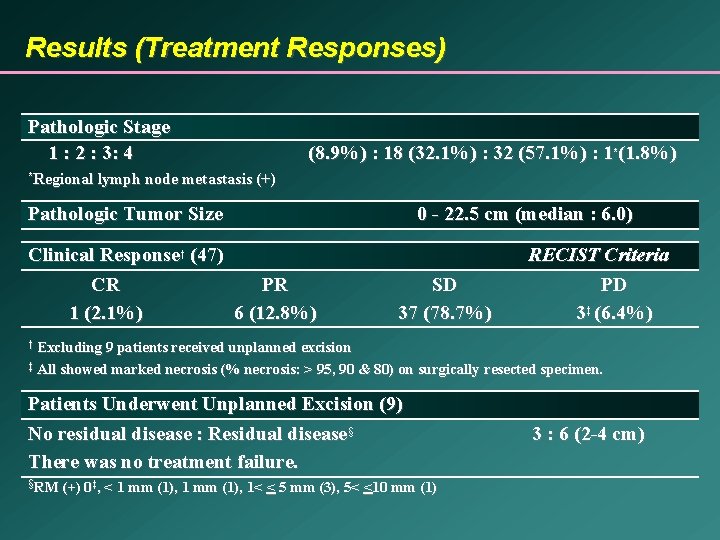
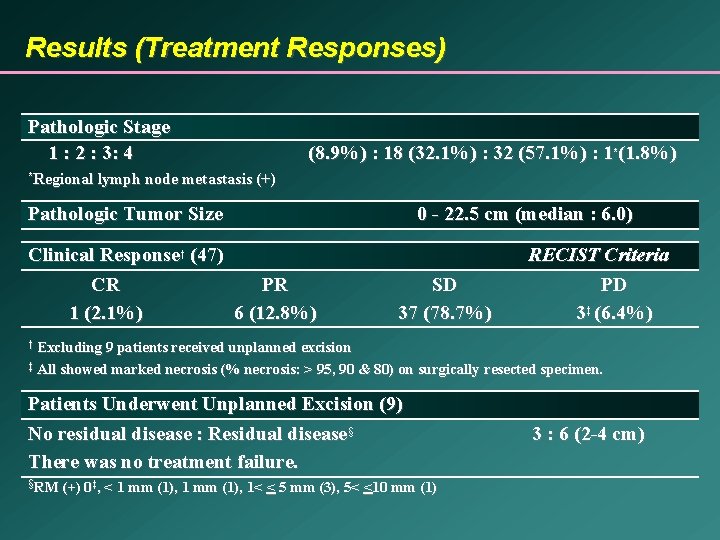
Results (Treatment Responses) Pathologic Stage 1 : 2 : 3: 4 (8. 9%) : 18 (32. 1%) : 32 (57. 1%) : 1*(1. 8%) Regional lymph node metastasis (+) * Pathologic Tumor Size Clinical Response† (47) CR PR 1 (2. 1%) 6 (12. 8%) 0 - 22. 5 cm (median : 6. 0) SD 37 (78. 7%) RECIST Criteria PD 3‡ (6. 4%) Excluding 9 patients received unplanned excision ‡ All showed marked necrosis (% necrosis: > 95, 90 & 80) on surgically resected specimen. † Patients Underwent Unplanned Excision (9) No residual disease : Residual disease§ There was no treatment failure. §RM (+) 0‡, < 1 mm (1), 1< < 5 mm (3), 5< <10 mm (1) 3 : 6 (2 -4 cm)
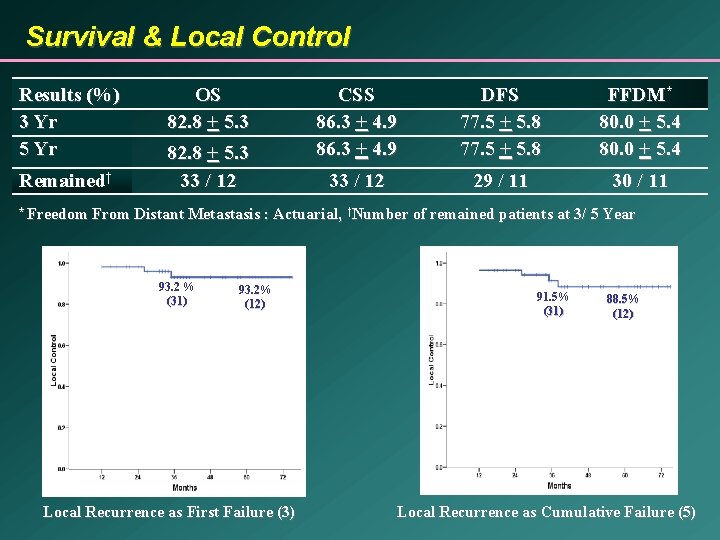
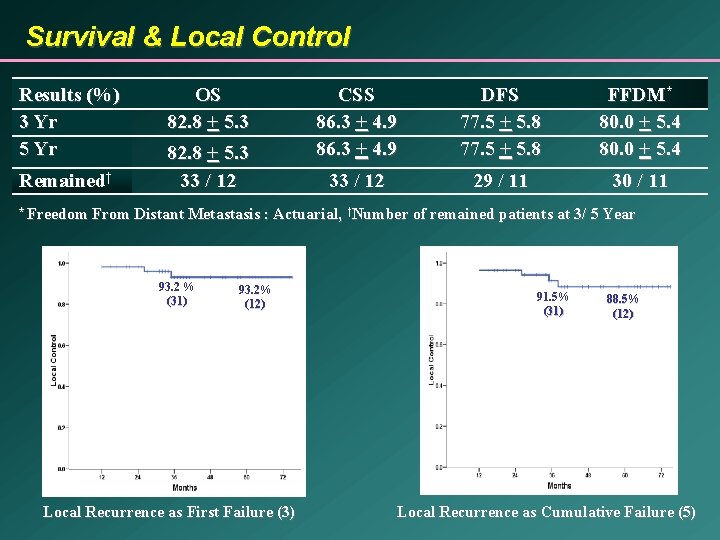
Survival & Local Control Results (%) 3 Yr 5 Yr Remained† * Freedom OS 82. 8 + 5. 3 33 / 12 CSS 86. 3 + 4. 9 DFS 77. 5 + 5. 8 FFDM* 80. 0 + 5. 4 33 / 12 29 / 11 30 / 11 From Distant Metastasis : Actuarial, †Number of remained patients at 3/ 5 Year 93. 2 % (31) 93. 2% (12) Local Recurrence as First Failure (3) 91. 5% (31) 88. 5% (12) Local Recurrence as Cumulative Failure (5)
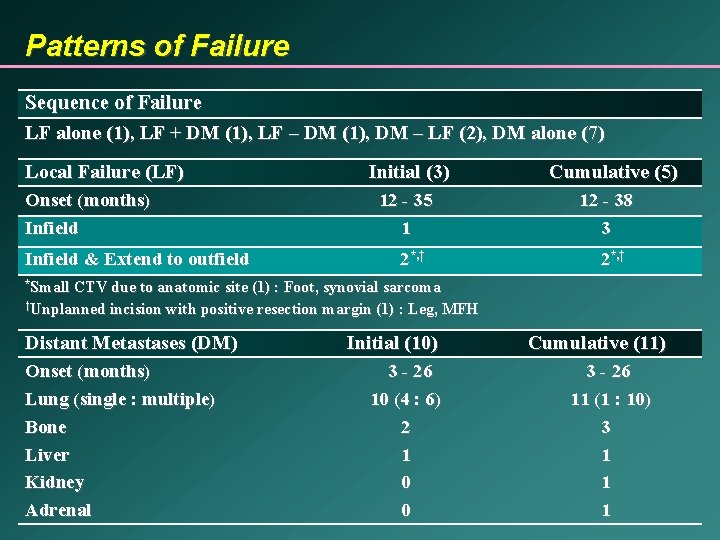
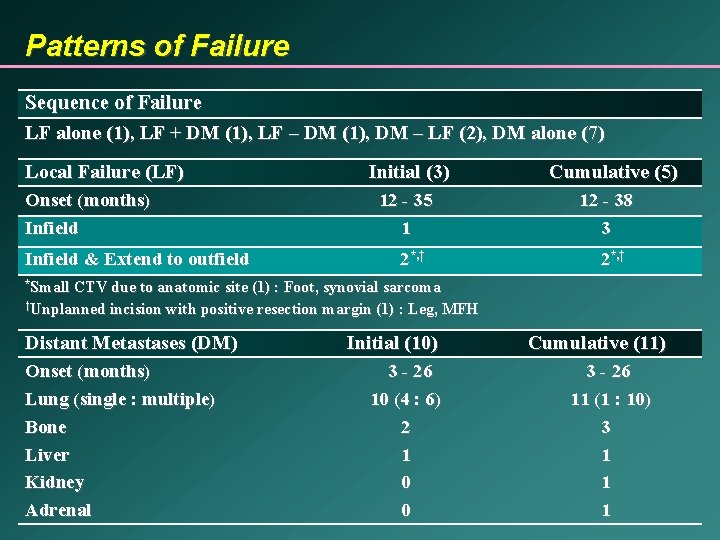
Patterns of Failure Sequence of Failure LF alone (1), LF + DM (1), LF – DM (1), DM – LF (2), DM alone (7) Local Failure (LF) Onset (months) Infield & Extend to outfield Initial (3) 12 - 35 1 2*, † Cumulative (5) 12 - 38 3 2*, † *Small CTV due to anatomic site (1) : Foot, synovial sarcoma †Unplanned incision with positive resection margin (1) : Leg, MFH Distant Metastases (DM) Onset (months) Lung (single : multiple) Bone Liver Kidney Adrenal Initial (10) 3 - 26 10 (4 : 6) 2 1 0 0 Cumulative (11) 3 - 26 11 (1 : 10) 3 1 1 1
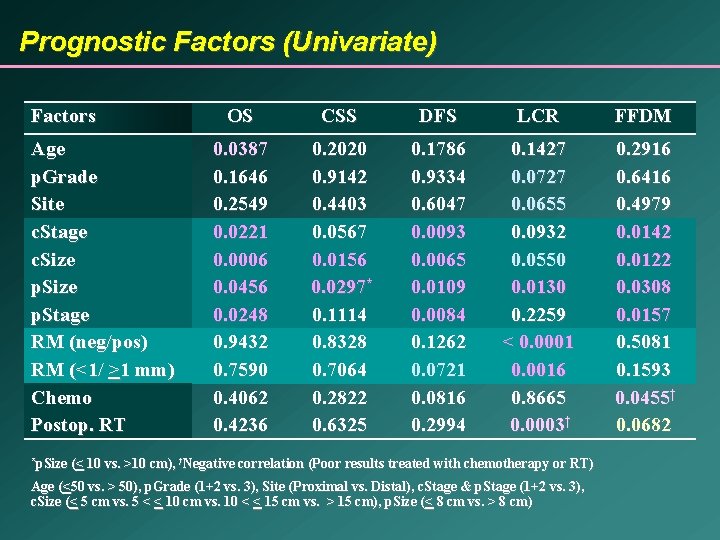
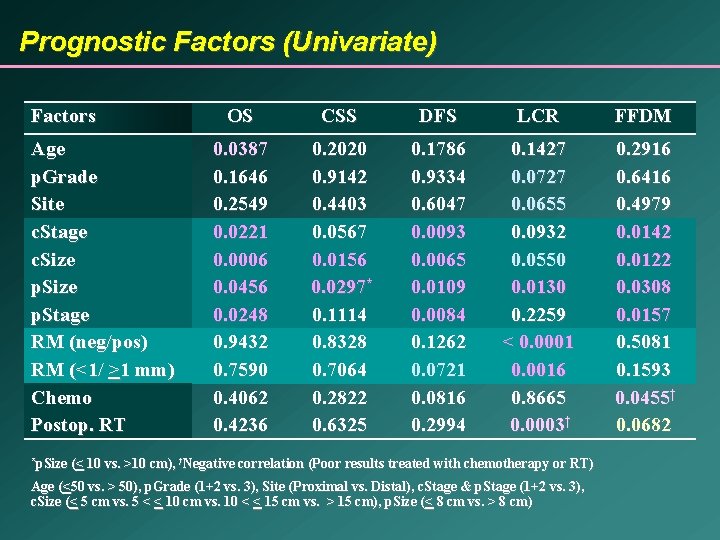
Prognostic Factors (Univariate) Factors Age p. Grade Site c. Stage c. Size p. Stage RM (neg/pos) RM (<1/ >1 mm) Chemo Postop. RT *p. Size OS CSS DFS LCR FFDM 0. 0387 0. 1646 0. 2549 0. 0221 0. 0006 0. 0456 0. 0248 0. 9432 0. 7590 0. 4062 0. 4236 0. 2020 0. 9142 0. 4403 0. 0567 0. 0156 0. 0297* 0. 1114 0. 8328 0. 7064 0. 2822 0. 6325 0. 1786 0. 9334 0. 6047 0. 0093 0. 0065 0. 0109 0. 0084 0. 1262 0. 0721 0. 0816 0. 2994 0. 1427 0. 0727 0. 0655 0. 0932 0. 0550 0. 0130 0. 2259 < 0. 0001 0. 0016 0. 8665 0. 0003† 0. 2916 0. 6416 0. 4979 0. 0142 0. 0122 0. 0308 0. 0157 0. 5081 0. 1593 0. 0455† 0. 0682 (< 10 vs. >10 cm), †Negative correlation (Poor results treated with chemotherapy or RT) Age (<50 vs. > 50), p. Grade (1+2 vs. 3), Site (Proximal vs. Distal), c. Stage & p. Stage (1+2 vs. 3), c. Size (< 5 cm vs. 5 < < 10 cm vs. 10 < < 15 cm vs. > 15 cm), p. Size (< 8 cm vs. > 8 cm)
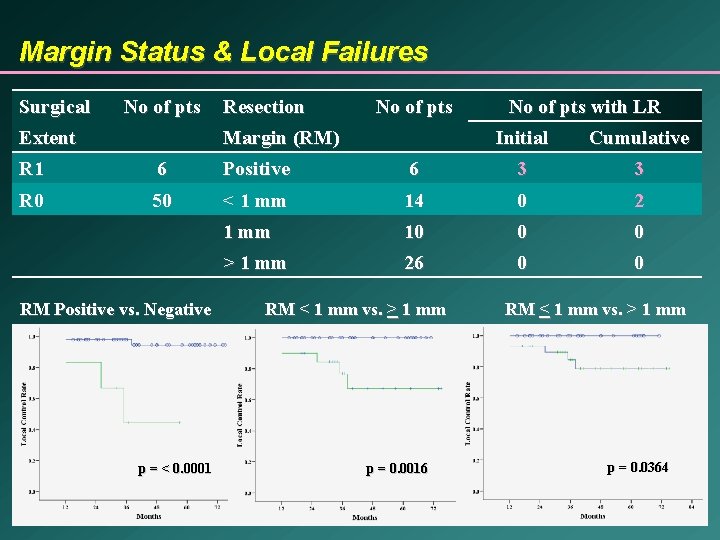
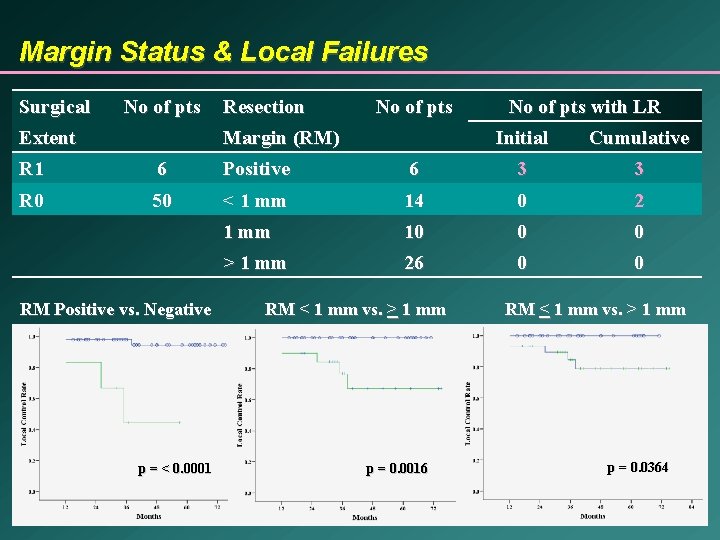
Margin Status & Local Failures Surgical No of pts Extent Resection No of pts Margin (RM) No of pts with LR Initial Cumulative R 1 6 Positive 6 3 3 R 0 50 < 1 mm 14 0 2 1 mm 10 0 0 > 1 mm 26 0 0 RM Positive vs. Negative p = < 0. 0001 RM < 1 mm vs. > 1 mm p = 0. 0016 RM < 1 mm vs. > 1 mm p = 0. 0364
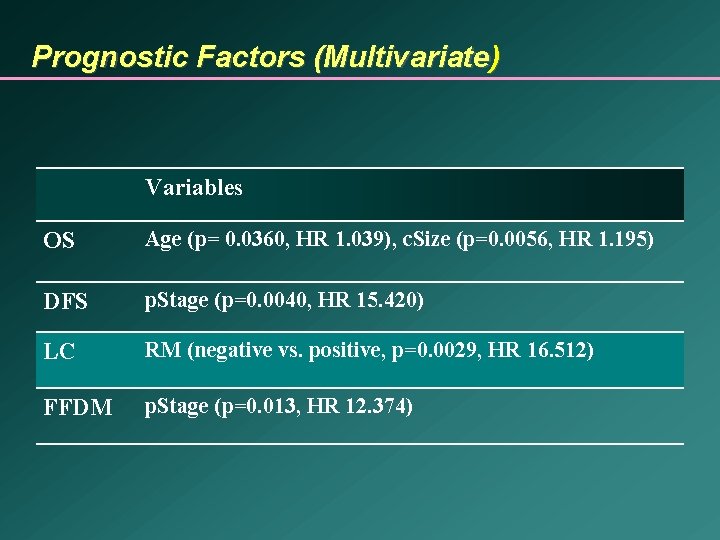
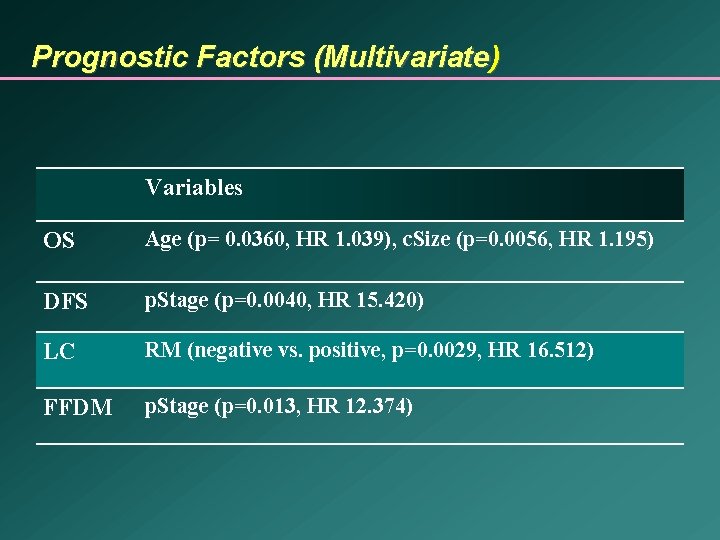
Prognostic Factors (Multivariate) Variables OS Age (p= 0. 0360, HR 1. 039), c. Size (p=0. 0056, HR 1. 195) DFS p. Stage (p=0. 0040, HR 15. 420) LC RM (negative vs. positive, p=0. 0029, HR 16. 512) FFDM p. Stage (p=0. 013, HR 12. 374)
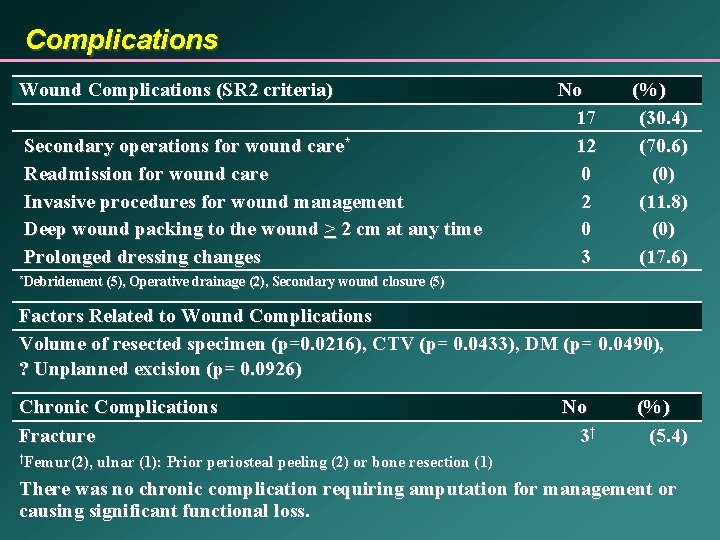
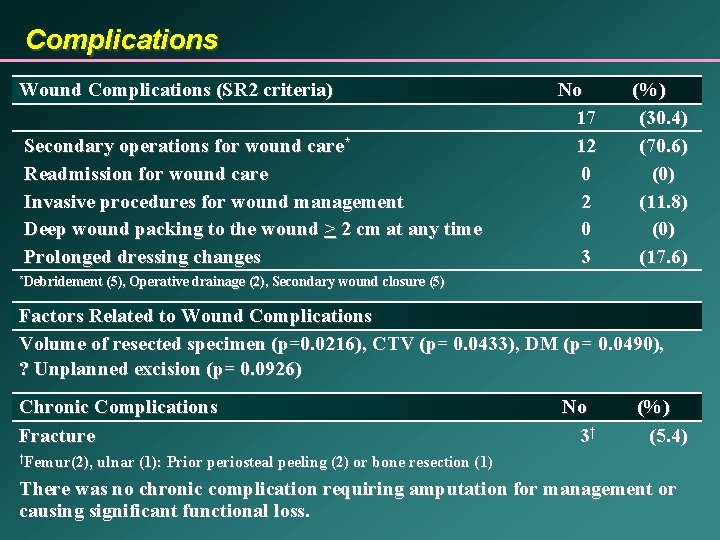
Complications Wound Complications (SR 2 criteria) Secondary operations for wound care* Readmission for wound care Invasive procedures for wound management Deep wound packing to the wound > 2 cm at any time Prolonged dressing changes *Debridement No 17 12 0 3 (%) (30. 4) (70. 6) (0) (11. 8) (0) (17. 6) (5), Operative drainage (2), Secondary wound closure (5) Factors Related to Wound Complications Volume of resected specimen (p=0. 0216), CTV (p= 0. 0433), DM (p= 0. 0490), ? Unplanned excision (p= 0. 0926) Chronic Complications Fracture †Femur(2), No 3† (%) (5. 4) ulnar (1): Prior periosteal peeling (2) or bone resection (1) There was no chronic complication requiring amputation for management or causing significant functional loss.
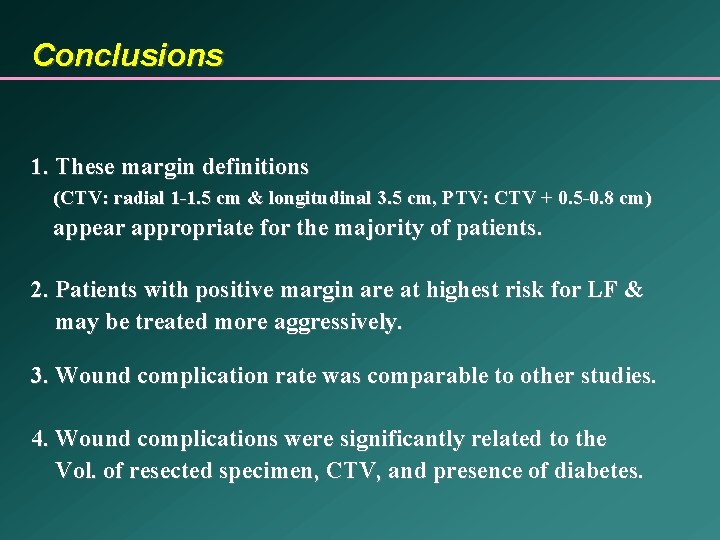
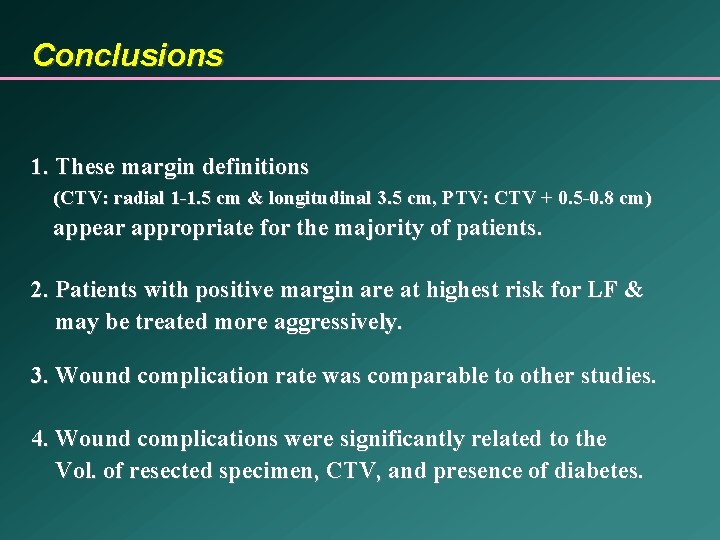
Conclusions 1. These margin definitions (CTV: radial 1 -1. 5 cm & longitudinal 3. 5 cm, PTV: CTV + 0. 5 -0. 8 cm) appear appropriate for the majority of patients. 2. Patients with positive margin are at highest risk for LF & may be treated more aggressively. 3. Wound complication rate was comparable to other studies. 4. Wound complications were significantly related to the Vol. of resected specimen, CTV, and presence of diabetes.

Thank you for your attention!
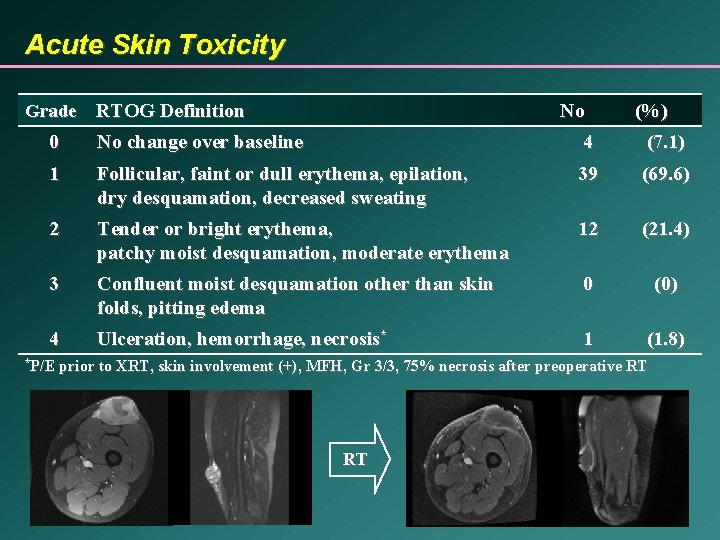
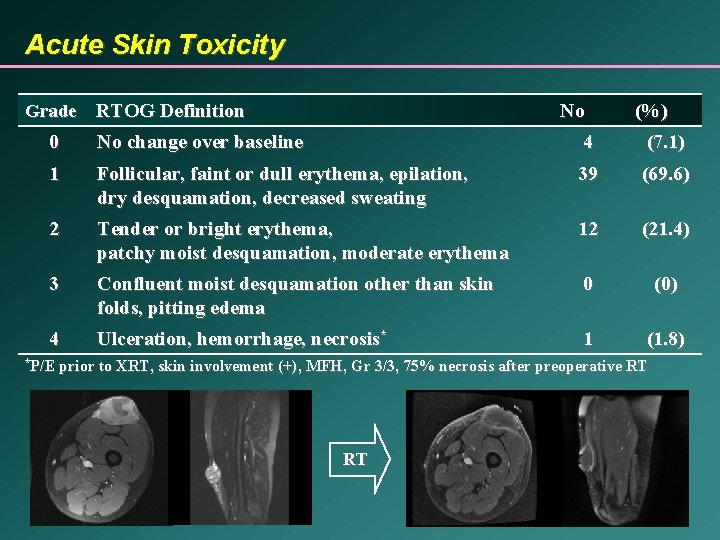
Acute Skin Toxicity Grade RTOG Definition No (%) 0 No change over baseline 4 (7. 1) 1 Follicular, faint or dull erythema, epilation, dry desquamation, decreased sweating 39 (69. 6) 2 Tender or bright erythema, patchy moist desquamation, moderate erythema 12 (21. 4) 3 Confluent moist desquamation other than skin folds, pitting edema 0 (0) 4 Ulceration, hemorrhage, necrosis* 1 (1. 8) *P/E prior to XRT, skin involvement (+), MFH, Gr 3/3, 75% necrosis after preoperative RT RT
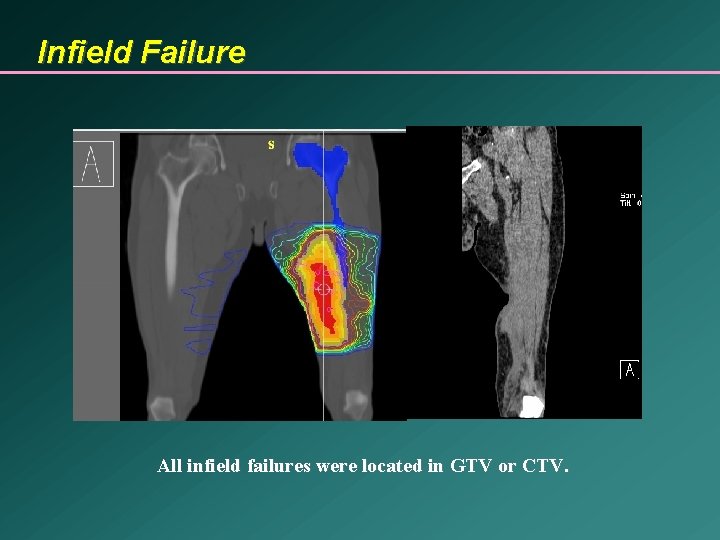
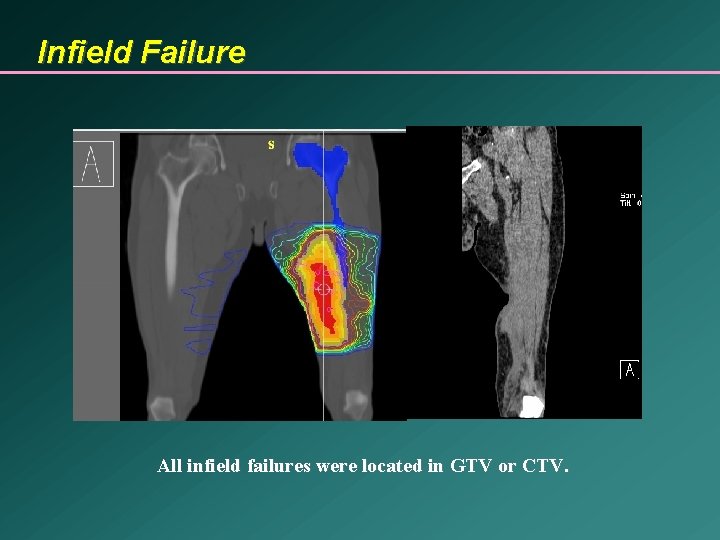
Infield Failure All infield failures were located in GTV or CTV.
 Pterigiums
Pterigiums Wedge factor radiotherapy
Wedge factor radiotherapy Radiotherapy
Radiotherapy Ssd and sad technique in radiotherapy
Ssd and sad technique in radiotherapy Siemens radiotherapy
Siemens radiotherapy Radiotherapy
Radiotherapy Post operative nursing care of cataract
Post operative nursing care of cataract Post operative nursing management
Post operative nursing management Cushing's triad
Cushing's triad Preoperative patient education ppt
Preoperative patient education ppt Nursing management preoperative care
Nursing management preoperative care Preoperative care ppt
Preoperative care ppt Perioperative care phases
Perioperative care phases Glaucoma nursing management
Glaucoma nursing management Perioperative definition nursing
Perioperative definition nursing Preoperative medical evaluation of the healthy patient
Preoperative medical evaluation of the healthy patient Serving size examples
Serving size examples Enduring service intensifiers
Enduring service intensifiers Adequate platelets
Adequate platelets Right to adequate food
Right to adequate food Proposal for a directive on adequate minimum wages
Proposal for a directive on adequate minimum wages Adequate meaning
Adequate meaning